Why is phlebectomy prescribed?
The purpose of this operation is to normalize blood circulation in the legs and prevent further damage to the veins.
Phlebectomy is prescribed when conservative treatment methods do not bring results. Surgical intervention is decided upon after treatment with medications, massage courses, and therapeutic exercises.
Photos - before and after
A doctor from Switzerland, R. Muller, became the founder of the miniphlebectomy method. Its essence is that a needle was used to penetrate a vein. At the final stage of the operation, the puncture sites along the edges were tightened with adhesive tape without additional sutures.
Müller phlebectomy is performed both in the system of the small saphenous vein and in large main vessels. This method of removing varicose veins has gained recognition due to its safety and cosmetic effect.
Today, this operation is performed by phlebologists using specialized equipment and modern techniques. The general principles of the procedure remain the same, but the approaches have become safer and less traumatic for patients.
Phlebectomy is performed on an outpatient or inpatient basis, depending on the severity of the disease and the chosen surgical technique.
Recovery periods after surgery
The average duration of the postoperative period is 7-10 days. This period may vary depending on the progress of the operation and the general condition of the patient. If there are any additional pathologies, the doctor sets an individual rehabilitation period.
The recovery period after surgery is divided into two stages - early and late. The early period begins immediately after the operation and lasts two days. The patient then undergoes basic recovery, which can take up to three months after surgery.
Indications and contraindications
The indication for phlebectomy of the lower extremities is varicose veins (ICD code – I83 “Varicose veins of the lower extremities”).
This pathology in a mild form can be corrected by drug treatment, but if the following symptoms are present, surgical intervention is indicated:
- pain in the legs and a burning sensation in the veins;
- swelling of the lower extremities and their chronic fatigue;
- the presence of ulcers that cannot be treated and do not heal over time;
- spread of the disease to the area up to the knee and above;
- venous nodes are swollen and protrude through the skin;
- blood stagnation in the extremities.
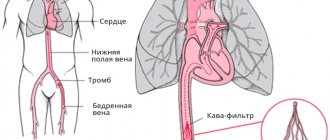
In addition, venectomy is indicated for varicothrombophlebitis. It occurs as a result of varicose veins and is characterized by the development of thrombosis of the saphenous veins of the lower extremities. The resulting blood clot prevents normal blood flow. Because of this, a blood clot forms inside the vein; when palpated, a lump-shaped compaction is felt. When the clot increases significantly in size and reaches a deep vein, the risk of developing pulmonary embolism increases. This condition is life-threatening and can cause sudden death.
Despite its safety, phlebectomy of the veins of the lower extremities has a number of contraindications:
- hypertonic disease;
- decreased immunity;
- cardiac ischemia;
- infectious and inflammatory diseases of the skin of the legs (erysipelas, eczema, boils in the operated area);
- infectious diseases in the acute stage;
- advanced age;
- pregnancy (2 - 4 trimesters) and lactation period;
- menstruation in women (high risk of bleeding);
- atherosclerosis of the lower extremities;
- acute deep vein thrombosis;
- diabetes.
What is phlebectomy? The essence of the operation
Phlebectomy (synonymous with venectomy) is one of the oldest methods of surgically eliminating varicose veins on the legs through holes in the skin. Modern medicine has several methods of phlebectomy of the veins of the lower extremities, named after their creators: according to Madelung, Muller, Babkot and Narat. Regardless of the name of the operation to remove sections of veins in the legs, the expected result is the same - exclusion of the vessel from the general blood flow and normalization of blood supply to tissues in which trophic changes are observed.
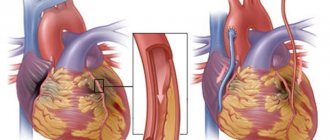
During surgery to remove varicose veins, specialists redirect blood flow through deep veins. The affected vessels are cut off from the bloodstream, separated from surrounding tissue and pulled out through incisions in the skin. Despite the complexity of the procedure, this vein operation is as safe and effective as minimally invasive procedures in the initial stage of varicose veins - sclerotherapy or laser coagulation. Doctors often combine these methods with surgical treatment of varicose veins to achieve better results.
In addition to alleviating the general condition and restoring tissue nutrition, phlebectomy improves the aesthetic appearance of the lower extremities: the venous pattern becomes invisible.
Should I have surgery?
Classic or combined phlebectomy, like any other surgical intervention, often frightens the patient, which is why he has doubts about whether it is worth performing the operation in his case, or whether conservative methods can be used. Experts do not prescribe it if it is possible to relieve symptoms and eliminate varicose veins in other ways. If they do not lead to positive results, it is unlikely that it will be possible to avoid surgery to remove a vein in the leg.
The patient should not get hung up on fears and think that such an intervention could be dangerous. Modern methods are practically devoid of shortcomings that can lead to negative consequences.
The question of whether surgery is needed for grade 2 varicose veins in the absence of a high prevalence of pathologically altered vessels, thrombosis, and severe symptoms is not subject to discussion. It is more profitable to treat such forms and stages of the disease with minimally invasive methods. Surgeons are not inclined to use this procedure for varicose veins in children: in a child under 18 years of age, the body is quite plastic, it is more susceptible to the positive influence of conservative methods, and the operation can lead to unpredictable consequences.
Modern types of phlebectomy
Improvements in medical instruments and equipment have led to the emergence of different types of phlebectomy. Patients can choose one of the ways to perform this operation.
Types of phlebectomy:
- Combined method.
- Radiofrequency obliteration (RAO).
- Laser coagulation.
- Echosclerotherapy.
Combined method
Classic combined phlebectomy is divided into the following stages:
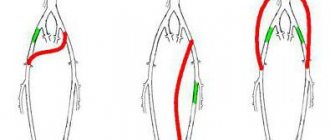
- Crossectomy (Troyanov-Trendelenburg operation) is a procedure for ligating the great saphenous vein and its subsequent intersection. The manipulation is performed at the point where the vein flows into the deep venous system. The result is a cessation of blood movement through the affected vessels. This stage may be the first, but sometimes it ends the operation. As a rule, this is done if there is a high risk of deep vein thrombosis. A crossectomy incision is made in the groin area or behind the knee.
- Stripping (Babcock operation) - removal of a vein after its intersection. This technique is a radical one, since its implementation involves complete excision of the damaged vessel using a metal probe with a hook at the end. With the short stripping technique, not the entire vein is removed, but only a small part of it.
- Ligation of perforating vessels (Narat technique) is performed after extraction of the saphenous veins. Perforating vessels perform the function of connecting deep veins with superficial ones. The procedure is necessary to prevent blood from entering the superficial system.
- Miniphlebectomy (Varadi operation or microphlebectomy) can be performed as the final stage of classic phlebectomy. It can also act as an independent operation to remove venous branches through small punctures in the skin. The operation is performed under local anesthesia, does not leave scars and gives a good cosmetic effect.
Some stages of combined phlebectomy can be replaced with more gentle minimally invasive interventions - laser or radiofrequency.
These methods do not require general anesthesia, as they do not involve the removal of veins. They are carried out in conjunction with ultrasound control in the early stages of varicose veins.
Radiofrequency obliteration (RAO)
The technique of performing the operation has a number of successive stages:
- After puncture, a special catheter with radiofrequency electrodes is inserted into the affected vein.
- A radio wave is transmitted to it, which causes it to heat up.
- The catheter moves inside the vein, heats and glues its walls.
- Then it is slowly removed from the cavity of the vessel.
- After the vessel walls are completely closed, the puncture site is disinfected, sealed with adhesive tape and an anti-embolic stocking is put on.
The procedure is performed under local anesthesia, has a short recovery period and an aesthetic result.
Laser coagulation
Laser coagulation has a similar mechanism to radiofrequency obliteration. Its distinctive feature is the use of laser radiation.
The surgeon makes a puncture on the right or left side of the knee, then inserts a catheter. A laser light guide is placed into the lumen of the vessel, which heats up and burns its walls.
As a result of a spasm of the vessel caused by temperature exposure, its walls stick together. After some time, the burn site will be overgrown with connective tissue, and the vessel will disappear forever.
The procedure is characterized by a favorable postoperative period and good cosmetic effect.
Echosclerotherapy
Echosclerotherapy is a modern, minimally invasive method in which a special drug, a foam sclerosant, is injected into a vein.
By acting on the walls of the veins, this substance sticks them together and interrupts the blood flow. The procedure is carried out on an outpatient basis, after its completion you will need to use an elastic bandage or wear compression garments. For better distribution of the substance, the patient is recommended to walk for the first hour after surgery.
The manipulation lasts up to 1.5 hours, depending on its complexity, determined by the stage of development of the disease.
History of surgical treatment of varicose veins of the lower extremities
The history of surgical treatment of varicose veins is closely related to the study of varicose veins themselves. A German doctor, Friedrich von Trendelenburg, suggested a cause-and-effect relationship between varicose veins and blood reflux in the area of the saphenofemoral junction. In 1860, Trendelenburg, based on this theory, proposed a method of surgical treatment of varicose veins by cutting and ligating the trunk of the great saphenous vein in the upper third of the thigh.
The founder of phlebectomy is Friedrich von Trendelenburg.
It is safe to say that the modern stage of phlebology as a medical science began precisely then. Next, an outstanding Russian doctor, Alexey Alekseevich Troyanov, proposed ligating the vein using a double ligature and excising a section of the great saphenous vein. In fairness, it is worth noting that none of these luminaries of their time insisted on mandatory ligation of the great saphenous vein at the level of the saphenofemoral junction. Oddly enough, the further development of phlebological science was ensured by extremely traumatic and aggressive techniques. The greatest contribution to the understanding of the anatomy of varicose great saphenous vein and the pathophysiology of reflux was probably made by the Modelung operation. The essence of the technique is to remove the great saphenous vein through a stripe incision along the entire venous vessel, from the groin to the ankle. Most sane surgeons abstained from the practical application of this operation, but they certainly made their own, quite significant, contribution to the knowledge of venous anatomy. Most importantly, it became clear that the trunk of the great saphenous vein needed to be removed. Already in 1908, V.V. Babcock proposed the option of removing the great saphenous vein using a special probe. This innovation, of course, was a breakthrough of its time and the first step towards a radical reduction in the traumatism of the intervention while maintaining all the advantages of removing the trunk of the great saphenous vein. With minor changes, mainly related to the design of the probe, the technique was successfully used for many decades. A number of specialists, mainly from government medical institutions, do not doubt the relevance of combined Babcock phlebectomy today, in the 21st century.
Preparation
Initially, in preparation for surgery, the patient is prescribed an ultrasound duplex scanning of the veins, and each affected area is marked.
The patient may also be offered phlebography, an examination using a contrast agent. This makes it possible to see the blood circulation process and determine the affected areas.
Based on the results of ultrasound and phlebography, the doctor receives a complete picture of the disease and decides on the choice of phlebectomy method. These examinations are used as the basis for the final formulation of the diagnosis.
At the next stage, the patient undergoes a standard preoperative examination:
- Fluorography, cardiogram.
- General blood and urine analysis.
- Biochemical blood test, hemostasiogram (coagulogram).
- Tests for HIV, hepatitis, syphilis.
- Analysis to determine blood group, Rhesus affiliation.
- Consultation with a therapist regarding existing contraindications to surgery.
When preparing for surgery, it is recommended:
- Before admission to the hospital, the patient, as prescribed by the phlebologist, selects compression hosiery or elastic bandages for himself.
- Before the procedure, you must shave the hair on your legs and groin area.
- On the eve of the operation, the patient must undergo a consultation with a surgeon and anesthesiologist.
- During general anesthesia, the last meal and fluid intake should be taken at least 12 hours before surgery. If spinal anesthesia or local anesthesia is used, there is no need to change your eating schedule. Avoid drinking alcoholic beverages for at least 24 hours.
Postoperative period
Once the patient's suture is removed, the following recovery procedures must be used:
- compression therapy;
- drug therapy - antibiotics, anti-inflammatory drugs, painkillers and others;
- physiotherapy.
After surgery, you must adhere to a healthy lifestyle. After surgery, it is necessary to eliminate modifiable risk factors that began to provoke the development of pathology in the veins.
Progress of the operation
The course of the operation will depend on the degree of damage to the veins and the stage of varicose veins.
If the doctor decides to perform a combined phlebectomy, the procedure will take approximately 2 hours.
This operation requires hospitalization and is performed under general or spinal anesthesia. Immediately after the manipulations, elastic bandaging of the patient’s legs is performed.
In order to prevent the occurrence of bruises and bleeding, it is necessary to bandage the limbs correctly. A faster and easier way is to use compression garments. As a rule, combined phlebectomy is prescribed for severe stages of varicose veins.
In cases of extensive varicose veins, the operation is performed using the Cockett method. Its purpose is to ligate blood vessels in the lower leg area. An incision is made along the surface of the lower leg to the upper ankle area.
For milder forms of lesions, other intervention techniques are used - miniphlebectomy, radiofrequency or laser phlebectomy. They are performed on an outpatient basis under local anesthesia and last 30-40 minutes.
Surgical treatment (combined phlebectomy) - surgical technique
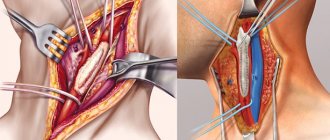
Modern combined phlebectomy is performed under general anesthesia or epidural anesthesia. After processing the surgical field, ligation and intersection of the main saphenous vein (great or small) in the area of the sapheno-femoral or saphenopopliteal anastomosis is performed, that is, crossectomy. To access these areas of the venous vessels, incisions are used along the inguinal or popliteal folds. The length of the incisions varies from one and a half to several centimeters.
Stages of classical phlebectomy
Stripping is performed, removing the trunks of the saphenous veins using a special probe, followed by removal of the tributaries of the main veins. After control of hemostasis, aseptic dressings are applied, compression garments or bandages are put on.
Postoperative rehabilitation
Full recovery, subject to the doctor’s recommendations and proper postoperative care, occurs after six months.
Rehabilitation after combined phlebectomy begins in the hospital, since the patient spends another 1-2 weeks there. One week after phlebectomy, the sutures are removed for the incision in the groin area, and after 10-12 days - in the area under the knee.
For one month after surgery, the patient must wear compression stockings or elastic bandages around the clock.
This introduces certain restrictions into the usual personal hygiene regime.
You can wet your leg only after the stitches have been removed. After a month, the doctor changes the period of wearing compression garments or the order of bandaging in accordance with individual indications. As a rule, 4 weeks after phlebectomy it is allowed to take it off at night and wash thoroughly.
For another 2-3 months, the patient continues to wear compression stockings during the day. During this period, it is prohibited to visit the sauna, bathhouse or take a hot bath.
In the first two days after surgery, pain is treated with analgesics and phlebotonics are prescribed (Phlebodia, Detralex).
During the same period, thrombosis prevention is performed with drugs that prevent increased blood clotting (Cardiomagnyl, Aspirin, Fraxiparine injections, Clopidogrel and others).
After the operation, the patient may experience a feeling of a hot flush in the legs or a feeling as if a needle is stabbing in the shin area. This may occur due to the accumulation of blood under the skin layer and the resulting swelling. If there is no redness on the skin and the body temperature remains within 37.5°C, then there is no need to worry about it. If the temperature rises above this value and signs of inflammation appear on the skin, you should immediately inform your doctor.
Recommendations after returning home:
- During the recovery period, swimming, walking and cycling will be useful.
- It is not recommended to lift heavy objects or wear uncomfortable high-heeled shoes.
- You should avoid staying in a static position for a long time (sitting or standing); every 30 minutes you should alternately stretch both legs.
- Regular and moderate physical activity (climbing stairs, performing therapeutic exercises) is necessary.
- During rest, for better blood flow, you should keep your legs elevated.
- You should give up bad habits (smoking and drinking alcohol).
Diet during rehabilitation
A narrow specialized diet is not required during rehabilitation. However, doctors formulate general nutritional recommendations that must be followed in the postoperative period.
These include:
- Abstain from fatty, salty and spicy foods. Smoked products, sweet drinks, canned food and semi-finished products are excluded.
- The diet should contain foods rich in fiber, plant fibers and pectins.
- The daily menu should include green vegetables (salad, green beans, cabbage), foods rich in polyunsaturated fatty acids (seafood, seaweed).
- It is recommended to increase the consumption of fruits and berries containing large amounts of vitamin C (black currants, cranberries, citrus fruits).
- Every day you need to drink at least 2 liters of clean water without gas.
- The menu must include products containing coumarins (onions, garlic, cherries, cherries, olive oil).
- You should control portion sizes and avoid overeating. Instead of black tea and coffee, use infusions of herbs (nettle, acacia and St. John's wort) and herbal teas (rose hips, sea buckthorn).
- Alcoholic drinks are excluded for the entire rehabilitation period and are allowed after 3 months in moderate doses (for example, a glass of dry wine with meals).
Exercise therapy and physiotherapy
The patient spends the first day after surgery in a lying position. Moreover, even on a hospital bed several hours after the procedure, he is recommended to have minimal physical activity.
You need to start with simple movements - bending and straightening your legs at the knees, turning your shins, rotating your feet. This is necessary in order to restore blood circulation in the legs and prevent stagnation.
The patient is allowed to walk on the second day, from this moment his physical activity should increase to prevent undesirable consequences. The recommended physical activity over the next 10 days is regular performance of a special set of exercises and moderate walking.
Some effective therapeutic exercises include:
- imitation of cycling while lying on your back;
- raising straight (or bent) legs and then lowering them;
- pulling the knees towards the chest;
- alternate walking on toes and heels;
- rotational movements of the ankle joint;
- scissors exercise.
Therapeutic exercises and physical activity are an effective remedy against postoperative complications.
They prevent the formation of edema, stimulate blood circulation, and promote lymph outflow.
Also during this period, a light massage is allowed, which improves blood flow and prevents the formation of blood clots.
To stimulate the healing process of sutures and tissue scarring, the doctor prescribes physiotherapeutic procedures - magnetic therapy and ultra-high-frequency therapy.
Creams and ointments
In addition to drug therapy, external agents - creams, gels and ointments - are also used during the rehabilitation period. They have an analgesic and antispasmodic effect, relieve inflammation and tone the walls of the veins.
If there are seals, bruises and hematomas, the use of these products helps them quickly resolve. The preparations should be applied to the skin 2-3 times a day until the internal seals disappear completely.
These products may be composed of:
- Natural (extracts and extracts of medicinal herbs and plants).
- Chemical (based on heparin and troxerutin).
The application of any external preparations is carried out only in the absence of open damage to the skin.
Rehabilitation
The duration of rehabilitation after varicose vein surgery depends on many factors, which include the initial condition of the patient, the length of the removed vein, the presence of concomitant diseases and others. In most cases, it lasts at least 3 months: this is exactly how long it takes the body to fully or partially restore blood flow and redirect it to the lateral blood supply system. The timing may vary depending on the method used: with a combined method, the postoperative period is always shorter, especially if sclerosants, laser and other modern technologies were used during the intervention.
To ensure that this process is successful and that problems with other veins do not arise, recovery after phlebectomy involves:
- Prevention of complications - infection of postoperative wounds, formation of blood clots and others. Immediately after the operation, the doctor conducts a conversation with the patient, in which hygiene requirements are voiced. They will depend on the method used. For example, after a phlebectomy according to Cockett, it is not recommended to wash the ankle part of the legs until the seam is closed, while after operations to remove varicose veins performed through micro-incisions, you can take a shower already on the first day. After hygiene procedures, the wounds are treated with drying antiseptics: brilliant green, iodine. To reduce the risk of thrombosis, the doctor may prescribe blood thinners, but only if there is no tendency to bleed.
- Maintaining the muscular system in the area where intervention for varicose veins in the legs was performed in sufficient tone. As you know, muscle contraction helps to more actively push venous blood upward, removing some of the load from the vascular walls. During the first week, restrictions are in place prohibiting increased activity and heavy lifting. They are relevant for any type of intervention, but you should not switch to bed rest: the sooner you start moving, the lower the risk of congestion and, accordingly, thrombosis. Starting from days 5-7, patients are shown exercise therapy, gymnastics, and physical therapy under the supervision of a specialist. After mastering the exercises, you can practice on your own.
- Acceleration of healing and tissue restoration with the help of physiotherapy: UHF therapy, quartz irradiation and others. With them, rehabilitation after phlebectomy will proceed much faster, and in combination with massage and reflexology, they will reduce the risk of trophic changes. The procedures are prescribed by the doctor on an individual basis.
In the first 7-10 days after the intervention, the patient may experience pain and discomfort in the legs. To eliminate them, the doctor prescribes painkillers. It is not recommended to select medications on your own, since some medications contribute to excessive blood thinning or, conversely, increase its viscosity.
Important! If within a week the discomfort does not subside, but intensifies, you should inform your doctor about it.
Diet
The role of rational and healthy nutrition after phlebectomy is often downplayed, although it is no less important than regimen and exercise, hygiene and medication. Firstly, a special diet and the inclusion of certain foods in the diet will help reduce blood viscosity. Secondly, eliminating certain foods that retain fluid in the body will eliminate swelling. Thirdly, during the recovery stage after leg surgery for varicose veins, the diet will curb weight gain or bring it back to normal in obese patients.
What can you eat after surgery for varicose veins:
- Soups with vegetable broth or water, stews, casseroles and salads with vegetables colored green, yellow and orange. They contain vitamin C, rutin and substances that promote blood thinning and vascular regeneration, as well as fiber that is useful during the recovery stage.
- Cereal porridge to maintain intestinal motility.
- Fruits and berries, always red or black (blueberries, raspberries, currants, blueberries, blackberries, cherries), citrus fruits - contain vitamins C, P and coumarins, which are necessary for the prevention of thrombosis. Eat fresh, in salads. You can make juices, compotes and fruit drinks from them.
- Seafood, sea fish, algae as a source of Omega-3 and Omega-6 acids, taurine, iron and iodine, necessary to maintain elasticity and restore blood vessels. It is advisable to steam the fish, and you can use the seaweed to make salads and soups.
- To restore soft tissues, replenish elastin and protein levels in the body, it is useful to consume white meat and poultry liver. It is recommended to boil them, steam them or bake them. You can prepare a dietary pate from the liver.
Regardless of the stage of recovery, post-phlebectomy patients are advised to drink more fluids. This can be non-carbonated mineral water, herbal tea (bearberry, lingonberry and rosehip), natural juices and compotes, fruit drinks.
When creating a menu, you should pay attention to the tolerance of products. Many of them can cause allergies or cause intestinal disorders (food allergies).
The list of prohibited foods after surgery for varicose veins includes:
- spicy and salty dishes, smoked meats, fast food, which contains a lot of salt;
- coffee and strong tea;
- alcohol;
- sweets, baked goods and any high-calorie food with minimal fiber and vitamins.
These products contribute to fluid retention in the body, irritate the walls of blood vessels, and provoke their spasms. In addition, against the background of limited physical activity, they can lead to weight gain, which is extremely undesirable for varicose veins.
Pros and cons of this operation
Like any other medical procedure, phlebectomy has its advantages and disadvantages.
Positive characteristics include the following:
- this is a radical and most effective way to treat varicose veins of the lower extremities;
- minimal likelihood of relapse and the appearance of new veins;
- the opportunity to receive this medical service under a compulsory health insurance policy (CHI);
- minor damage to the integrity of the skin (invisible scar, small scar);
- good tolerability among patients and cosmetic effect;
- short recovery period.
The disadvantages of the procedure include the following:
- use of anesthesia (risk of side effects and intolerance to its components);
- at first, the surgical sites may hurt and swell;
- there is a possibility of postoperative complications;
- the appearance of age spots, hematomas and bruises at the site of vein removal;
- After the operation, a scar remains at the site of the incision.
Features of the technique
Combined phlebectomy is a surgical method for treating varicose veins.
This is a classic surgical option that includes several stages. The main task is to eliminate reflux. At the same time, the doctor carefully selects ways to get rid of this problem.
The surgeon tries to restore the normal functioning of the reverse outflow of blood in the venous system of the legs. Surgery will help stop blood flow in the varicose vein and in all tributaries.
This problem can be solved by complete elimination or by using a chemical effect on the vascular endothelium.
FAQ
Vein removal surgery is in demand, since varicose veins are a disease that often occurs in the adult population.
People are concerned about what changes consent to surgery will bring to their daily lives.
Is it possible to play sports after phlebectomy?
During the first three months, only moderate physical activity is recommended.
Strength sports, aerobics, fitness, running, long walking and cycling are prohibited. During the rehabilitation period, you should not overload the lower limbs with power, dynamic and impact loads.
During the entire recovery period, only therapeutic exercises are allowed.
After successful rehabilitation, you can gradually return to preoperative activities under the supervision of a physician.
Is it possible to walk in heels?
You can walk in heels, the main thing is to choose the right heel height. High-heeled shoes are not recommended either before or after surgery.
But the heel on the shoe must be present, and its height should be from 2 to 4 centimeters.
Phlebologists do not recommend shoes with either completely flat soles or heels higher than 5 centimeters.
Duration of sick leave
A sick leave for a period of at least 7 days is given to each patient, regardless of the type of phlebectomy performed.
Medical practice shows that the rehabilitation period is not limited to a week and it is possible to extend sick leave according to individual indications.
Phlebectomy technique
Before starting the combined phlebectomy procedure, the doctor must mark the patient's varicose vessels. This is done in a vertical position using duplex ultrasound scanning.
The doctor must determine the extent of the damage to the valve apparatus of the main type veins, mark all the areas of confluence of tributaries. In addition, it is necessary to mark those tributaries that are affected by varicose veins.
As we mentioned earlier, it is carried out in stages. Let's highlight the main stages:
- Crossectomy, which can be either distal or proximal (lower and upper).
- Stripping (sometimes short type).
- Elimination of perforating discharge (vein ligation).
- Miniphlebectomy.
In rare situations (for example, in the very early stages of the disease, with a non-trunk course of the disease, when there is no need to eliminate the GSV and SSV), some stages of the operation can proceed as independent ones.
The stage of combined phlebectomy may be the replacement of classical methods with alternative minimally invasive methods. This can be either sclerotherapy or laser procedures.
What complications may arise?
Incorrect procedure technique and failure to follow postoperative recommendations can lead to various complications:
- Inflammation, infection and suppuration in the hematoma area.
- Bleeding.
- Thrombosis in deep veins.
- Thromboembolism.
- Subcutaneous lumps and bruises.
- Relapse (the appearance of new veins above the incision site or scar).
- Nerve damage and sensory disturbances, numbness of the limb in the lower leg (inner side), foot and ankle.
- Damage to the lymphatic vessels (lymphorrhea).
Possible complications
After combined phlebectomy, reviews are mostly positive. A person’s vital functions improve, he can walk without pain. However, the procedure can also cause some complications:
- Heavy bleeding during surgery. It is not always possible to stop him quickly. More often, this complication occurs in those patients who have problems with blood.
- Constant pain in the legs, the appearance of lumps, which can also be painful.
- Decreased sensitivity in the limbs. This condition is typical for those patients whose nerves were damaged during surgery,
- Suppuration. This complication occurs due to non-compliance with the rules of septic tanks and antiseptics.
Sometimes a patient develops deep vein thrombosis after the intervention. If complications occur, the patient requires drug therapy. It will help relieve postoperative symptoms faster.
Do's and don'ts after vein removal surgery
The postoperative period of phlebectomy is called the rehabilitation or recovery period. Estimated duration is about a month. After combined phlebectomy, the patient remains in the hospital for a couple of weeks. This is required to remove stitches: cosmetic ones are removed after 7 days, all this time doctors recommend:
- wear compression stockings or bandage the seams tightly with an elastic bandage;
- regularly perform a complex of exercise therapy, balanced, dosed, calculated by a doctor on an individual basis;
- adhere to an antiatherogenic diet with a predominance of vegetables and fruits;
- drink more clean water (30 ml per 1 kg of weight);
- take medications prescribed by your doctor: venotonics, anticoagulants or antiplatelet agents, painkillers (if necessary);
- to refuse from bad habits;
- control weight.
A massage course, swimming, cycling will not be superfluous. At home, you can perform simple leg movements while lying in bed. Showers, baths, saunas, and swimming pools must be avoided until a doctor's permission. Even after the stitches are completely removed, you should avoid taking hot baths. For a month, compression underwear or elastic bandages are worn around the clock (it will not be possible to fully implement hygienic procedures). After a month, compression will be required only during the day; in the evening, the bandages can be removed and hygiene procedures taken.
You need to get up and walk on the next postoperative day. This is the prevention of thrombosis. But you can’t lift heavy objects, as well as stand or sit for a long time (up to and including changing jobs, if it’s related to an office work schedule).
Consequences of phlebectomy
Complications most often can be expected after phlebectomy. Surgery to remove veins for varicose veins on the legs using the classical method can lead to:
- Severe pain along the operated vein.
- Accumulation of blood under the skin.
- The formation of extensive hematomas prone to suppuration.
During the rehabilitation period, postoperative sutures require careful treatment, and bandages are applied to them for hygienic purposes. If the rules for caring for sutures are violated (if the sutures are not treated in a timely manner and bandages are not changed), the patient may experience wound infection in the postoperative period. The accumulation of blood along the removed vein forms compactions that are painful on palpation.
If there are no hyperemic areas above the seals, indicating a bacterial infection or inflammatory process, then over time you can expect them to resolve. How long this will take depends on individual characteristics and compliance with the doctor’s recommendations.
After surgery, you need to keep the sutures clean to avoid infection.
When ligating the vein trunk, injury may occur to the nerves that pass near the saphenous and femoral veins or lymphatic vessels of the legs. When lymphatic vessels are damaged, lymph can soak into the tissue, forming swelling, or accumulate in the resulting cavity. In the latter case, a puncture is prescribed to free the cavity from accumulated fluid or open it. Rehabilitation in this case will include the use of decongestant medications.
You can walk around the ward already in the first hours, provided that the load on the legs is reduced with the help of a splint, and elastic bandages on the legs will prevent the risk of blood clots, bleeding and recurrence of varicose veins. Elastic bandages need to be worn for a long period of time (2-3 months). After phlebectomy, it is necessary to perform special physical therapy exercises and walk so that lumps and hematomas disappear on the operated legs
How long it is necessary to wear bandages should be determined by the doctor, taking into account:
- Difficulty of intervention.
- The extent of affected vessels in varicose veins.
- Risk of recurrence of varicose veins.
- Individual characteristics.
To disappear hematomas on the legs after surgery, you need to walk and do special exercises.
To avoid complications after surgery, it is necessary to follow the doctor’s recommendations in the postoperative period and a special regimen. Reviews of radical phlebectomy indicate great trauma and difficult postoperative recovery. But patient reviews also indicate the high effectiveness of the operation (see photo.
After the operation, a diet is prescribed, which should contain a large amount of vitamins, microelements, and fiber. Also, the diet should provide blood thinning. This diet allows you to reduce the risk of complications after surgery during the rehabilitation period. It is necessary to include feasible sports activities, walking, taking walks, and swimming. Dosed physical activity, a healthy lifestyle, and diet will help speed up recovery and prevent recurrence of varicose veins.
Since rehabilitation after radical phlebectomy takes a long period of time, the patient is given a sick leave certificate. How long you can stay on sick leave is determined by your doctor. If the work is not associated with increased stress and prolonged standing, then the sick leave is closed after 1-1.5 weeks. Rehabilitation involves the use of phlebotonics, which is stipulated in the phlebologist’s recommendation. You can expect a recurrence of varicose veins during the period of hormonal changes in the body.