In older people, heart failure (HF) appears as a result of pathological changes in the organs and systems of the body. Note that in young people, disruptions in the functioning of the cardiac system occur suddenly against the background of acute pathological processes, but in older people the disease develops gradually, eventually becoming a chronic process.
This is a natural mechanism of aging of the body, however, it often indicates an exacerbation of diseases that prevailed in people in their youth. In our editorial we will talk about the symptoms of heart failure, as well as the treatment of pathology in old age.
In old age, chronic heart failure is one of the most common problems.
Causes of heart failure in old age
Heart failure should not be considered as a disease that arose independently. Experts say that this dangerous condition is caused by a malfunction of one or more body systems.
A very common factor that provokes heart failure in old age is the narrowing of the arteries that deliver oxygen to the heart muscle . Moreover, such vascular pathology can manifest itself not only in adulthood, but also at a very young and even young age.
Statistics show that, on average, 10 out of 1000 patients over the age of 70 are diagnosed with heart failure. The disease most often affects women, since older men are more likely to die from vascular disease before it leads to heart failure.
The next factor is arterial hypertension , which is characterized by an increased load on the heart. Because of this, the vital organ increases in size, the heart muscle weakens, and heart failure develops.
- Recommended articles to read:
- Social services for older people
- Diseases of old age
- Valuable tips on how to choose a boarding house
Not least among the prerequisites for the development of pathology are coronary disease, caused by blockage of the heart vessels with lipoids (fat-like substances), and heart attack , which entails partial death of heart tissue.
The development of the disease in old age can be caused by arrhythmia (irregular contraction), which disrupts the rhythm of the heart filling with blood and its release. Experts consider the most dangerous condition to be when the heart beats more than 140 beats per minute.
Other factors that can trigger the development of heart failure in old age are:
- Changes in the structure of the valves, which disrupts the process of filling the heart with blood;
- Inflammation of the heart muscle due to alcohol, infection or toxic damage;
- Hormonal imbalance (for example, with hyperthyroidism - excessive thyroid function);
- Addiction to alcohol or drugs.
Usually, when going on a well-deserved retirement, an elderly person becomes less physically active. Because of this, signs of cardiovascular disease may develop faster, but be less pronounced. It is not uncommon for patients to have two or three conditions at the same time that can lead to heart failure in old age.
In cases where it is impossible to reliably determine the cause of the pathology, doctors diagnose idiopathic heart failure.
Read the material on the topic: How to prevent a stroke
Signs of right ventricular failure
The first thing that should alert you to this pathology is the appearance of swelling in the legs, which, starting from the ankle joints and ankles, gradually spreads up the limbs. The reason for such edema is the same as for pulmonary edema - when a significant volume of blood accumulates in the vessels of the lower extremities, it leads to an increase in pressure, and in the smallest blood vessels, capillaries, transudate (the liquid part of the blood) is squeezed into the tissue.
The increase in edema will occur slowly, and it will be visually noticeable already after the loss of 4–5 liters of fluid. Before this, the patient may feel heaviness in the legs, fatigue and decreased diuresis (urination). Gradually, swelling spreads to the hips, lower back, and abdominal cavity. Pain may appear in the area of the right hypochondrium, which indicates the involvement of the liver in the process. The accumulation of transudate in the abdominal cavity will lead to an enlarged abdomen, which in appearance will resemble the belly of a frog. If fluid fills the pleural cavity, it will prevent the lung tissue from fully expanding. Then respiratory failure develops - cyanosis, severe shortness of breath will appear, and cardiac asthma will develop, which was mentioned above.
Help for a patient by relatives in this condition will be similar to that described above. Drug therapy in such conditions is determined only by a doctor.
Symptoms of heart failure in old age
Heart failure can occur in acute or chronic form. The main manifestations of the disease include:
- Slowing down of general blood flow;
- Increased pressure in the chambers of the heart;
- Decreased volume of blood “pumped” by the heart;
- Accumulation of blood that the heart cannot cope with in the abdominal cavity and in the veins of the legs.
Due to the fact that heart failure has vague symptoms, its treatment in old age becomes significantly more complicated.
Signs of the disease in older people are more similar to manifestations of natural aging:
- Fatigue;
- Weakness;
- Insomnia;
- Fast fatiguability;
- Drowsiness;
- Decreased mental abilities;
- Irritability;
- Depression.
Among experienced therapists, manifestations of heart failure in old age are usually called “masks.”
As for the congestive chronic form of the disease, its classic symptoms are shortness of breath and swelling of the legs. In older people they appear much later than in other patients. Therefore, at the time of visiting a doctor, the heart of an elderly person is usually in a very poor condition.
Symptoms of heart failure in old age are in many cases not specific and are “disguised” as signs of other diseases. The most common variants of the course of the disease are:
- Abdominal – accompanied by bloating and a feeling of heaviness in the abdomen, constipation, loss of appetite;
- Arrhythmic - an elderly patient feels rhythm interruptions and intense heartbeats, rapid heartbeat;
- Cerebral – manifested by causeless general weakness, mood swings, anxiety, drowsiness, loss of orientation;
- Pulmonary , the main symptoms of which are a cough not associated with a cold and shortness of breath. These manifestations intensify with physical activity and in a lying position;
- Renal - accompanied by low urine output, causing swelling of the legs and feet, which diuretics cannot cope with. Urinalysis shows elevated levels of red blood cells and protein.
Significant differences in the symptoms of heart failure in old age are due to which side of the heart the disease develops.
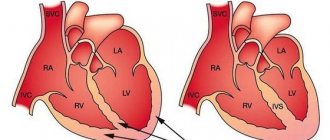
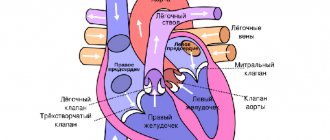
Right-sided insufficiency occurs when the outflow of blood from the right ventricle and right atrium is difficult for one reason or another (for example, due to dysfunction of the valve). The result is increased pressure and fluid accumulation in the vessels that originate in the right chambers of the heart (veins of the legs and liver). Because of this, there is an increase in liver volume and swelling of the legs.
With left-sided heart failure in older people, there is increased secretion of mucus (possibly mixed with blood) and general weakness. It is the upper chamber of the heart (left atrium) that receives oxygenated blood from the lungs and pumps it into the lower chamber (left ventricle), from where it is distributed to all organs and systems. If the left side of the heart is malfunctioning, blood flows back into the pulmonary vessels, and excess fluid penetrates through the smallest vessels and causes breathing problems.
The condition of congestive heart failure in old age is characterized by the fact that the kidneys cannot cope with large volumes of fluid, and the salt, which they normally excrete along with water, remains in the body, causing swelling. In this case, doctors diagnose kidney failure, which can be cured by eliminating the underlying cause - heart failure.
If any system does not perform its functions, the body turns on a defense mechanism to eliminate the problem. This property of our body manifests itself in heart failure in old age as follows:
- Changes in heart size . To send a sufficient volume of blood to organs and tissues, its chambers expand and begin to work more intensely;
- Increase in heart rate;
- Inclusion of the compensatory mechanism (renin-angiotensin system). In the early stages of heart failure in old age, the kidneys begin to produce the hormone renin, which prevents salt and water from being excreted in the urine, returning them to the blood. Because of this, pressure increases and the volume of circulating blood increases. In this way, the elderly patient’s body tries to provide the brain and other vital organs with sufficient oxygen. However, the heart cannot work indefinitely in an enhanced mode, so this mechanism is effective only in the early stages of the disease.
Read material on the topic: Health of older people
Signs of left ventricular failure
One day you suddenly notice that, while climbing the stairs to your floor, for some reason you involuntarily begin to breathe through your mouth. Moreover, you want to stop to rest, although just recently you were climbing the steps almost at a run. It’s just fatigue - you decide - shortness of breath always appears when exerting yourself. And indeed, after sitting in front of the TV for some time, we felt that everything had returned to normal. That’s how it is, the load always makes you breathe more often and deeper, and this is normal. But when you have to calm your breathing in a sitting position for more than ten minutes, then you need to think about heart failure, moreover, of the left side of the heart. Shortness of breath is the earliest sign of left ventricular failure.
How does this happen
We know that the left ventricle ejects blood into the aorta, from which it disperses through the vascular system throughout the body, reaching every organ. When there is not enough oxygen somewhere, the heart speeds up its rhythm in order to eliminate the resulting hypoxia (lack of oxygen). At the same time, breathing becomes more frequent to increase the flow of air into the lungs. When a weakened heart is unable to transfer blood from the lungs to the aorta and somewhere the lack of oxygen cannot be eliminated, tachycardia (rapid heart rate) and tachypnea (rapid breathing) remain for a longer time.
But over time, shortness of breath not only does not go away, but becomes more and more pronounced and occurs even with slight exertion. Hoarse, wheezing breathing appears. This is due to the fact that from the blood stagnating in the vessels of the lungs, its liquid part (plasma) is squeezed into the tissue of the bronchi, making them rigid. Then, from a distance, you can already hear gurgling wheezes when breathing, which indicate that the plasma is beginning to sweat into the alveoli. The previously dry cough becomes wet and the lungs begin to swell.
Moreover, over time, a person begins to suffocate in a state of complete immobility and even in a lying position. In such cases, we have to talk about the occurrence of attacks of cardiac asthma. The latter can be stopped by placing pillows under the patient's back after sitting him down. And most often in the evening nothing causes alarm - such patients fall asleep quite calmly. The drama plays out at night.
- Left-sided heart failure is always accompanied by weakness and increased fatigue, which occurs as a result of decreased blood flow to the muscles.
- The patient becomes irritated by the constant need to urinate at night, and as the disease progresses, a decrease in urine output may occur.
- Reduced blood flow to the brain causes frequent headaches and memory impairment.
- Old people may experience hallucinatory phenomena.
Changes in the patient’s appearance will not linger. Sick sweating, pale skin with cyanotic fingers. A constant rapid pulse is tachycardia, with which the heart tries to compensate for the insufficient emission of blood in one contraction (systole). Blood pressure is low, but hypertension soon develops due to spasm of peripheral vessels.
Without treatment, all this will ultimately lead to an increase in pulmonary edema. The cough intensifies, and whitish, foamy sputum is released, which then turns pink due to the sweating of red blood cells - erythrocytes - into the alveoli. Breathing in this state is bubbling and can be clearly heard from a distance. The patient is in a state of excitement - fear of death from suffocation, which can occur without immediate assistance. Of course, in such advanced cases, treatment should be carried out only in a hospital.
The very first aid
However, it often happens that a person’s life literally depends on the timely assistance of relatives, who must competently provide it before the ambulance arrives. The patient should be calmed and seated with his legs down - this will reduce the flow of venous blood to the lungs. The room must be ventilated. Give a nitroglycerin tablet under the tongue. Bubbling breathing, especially accompanied by the discharge of foamy sputum, can be stopped or reduced by applying tourniquets to the thighs for fifteen to twenty minutes - this will again reduce the blood flow to the lungs.
Functional classes of heart failure in old age
To correctly assess the severity of heart failure in old age, doctors use four functional classes:
- Physical activity is not limited, the disease does not affect the patient’s quality of life;
- Physical activity is accompanied by shortness of breath, general weakness, and rapid heartbeat. During rest, these manifestations do not bother the patient;
- Performance is significantly reduced, the slightest activity provokes shortness of breath, angina attacks, and palpitations. During the rest period, the patient's condition returns to normal;
- The working capacity of an elderly patient is lost completely or partially, the disease makes itself felt even during rest.
Causes of HF
Heart failure is not an independent disease - it is a symptom that accompanies physiological situations or pathological processes associated with vasospasm and myocardial hypoxia.
| Physiological reasons | Pathological causes |
| Nervous overstrain of any nature, stress | Heart defects of various etiologies |
| Physical exercise | Tumors |
| Hereditary predisposition to heart pathologies | IHD in all manifestations from hypertension, angina to heart attack |
| Taking medications | Cardiosclerosis |
| Obesity | Infections of any etiology |
| Cachexia | Chronic bronchitis, COPD |
| Poor nutrition | Endocrine pathologies |
| Bad habits | Rheumatism, autoimmune processes |
| Pregnancy | Heart rhythm disturbances |
| Period | Anemia |
| Meteor dependence | Disturbances in the blood flow at different levels |
| Heatstroke or sunstroke, sudden temperature changes | Inflammation of the membranes of the heart |
How is heart failure diagnosed in old age?
Methods for diagnosing heart failure in elderly and young adults do not differ significantly. However, when working with a mature patient, it is especially important to slowly question and listen carefully to him, because many older people suffer from memory impairment.
To confirm the preliminary diagnosis of “heart failure in old age,” hardware and laboratory tests are used.
To assess the condition of the valve apparatus and myocardium, the following is carried out:
- Electrocardiography with minimal stress tests;
- General chest x-ray (in two projections);
- Doppler ultrasound.
The following laboratory parameters are extremely important:
- Complete blood count with leukocyte formula;
- Residual nitrogen and bilirubin in the blood;
- Sugar and protein content in blood and urine;
- Transaminase and lactate dehydrogenase enzymes;
- Triglycerides, lipoproteins.
To determine the presence of unusual lung sounds that occur due to fluid accumulation in the alveoli, the doctor listens to the elderly patient with a stethoscope or orders an X-ray examination.
The noises that arise in the patient’s heart when it is filled with blood and released are subject to careful study.
To assess the degree of swelling in the limbs of an elderly person, the doctor applies finger pressure to a certain area of the skin and records the time it takes for it to return to its original state.
An important sign of heart failure in old age, indicating insufficient oxygen in the blood, is cyanosis (blue discoloration of the extremities), which is often accompanied by chills.
To understand whether the disease has led to changes in heart parameters, the patient is sent for an echo and radionuclide cardiogram.
To identify sites of blockage in blood vessels and measure pressure in the heart chambers, cardiac catheterization is performed, during which a thin tube is inserted directly into the heart muscle through a vein or artery.
To determine changes in the rhythm and size of the heart, as well as the effectiveness of the prescribed treatment, the patient is prescribed an electrocardiogram (ECG).
Read material on the topic: Flu in older people: signs, treatment and prevention
The essence of pathology
The essence of the process is the loss of the ability to fully fill and empty the chambers of the heart. The result is insufficient nutrition and oxygen supply to all internal organs and tissues. The problem often occurs in elderly patients over 60 years of age. There are acute and chronic forms of pathology.
Acute heart failure is a symptom of decompensation of pre-existing heart diseases, a consequence of injuries, and large blood loss. The danger of this condition is the rapid progression of the pathological process with a fatal outcome if the patient is not provided with medical assistance in a timely manner.
Chronic HF exists for a long time, becomes overgrown with symptoms, and leads to a decrease in quality of life and disability. CHF is divided into 4 classes:
| Class | Characteristic |
| First | There are no complaints, but there are already signs of heart failure |
| Second | Complaints of fatigue appear after any exercise, a person’s motor activity decreases, and the quality of life deteriorates. |
| Third | Complaints are present even in a state of rest, shortness of breath increases, fatigue from any simple activity |
| Fourth | The discomfort is constant, minimal exercise worsens the patient’s condition |
Heart failure according to localization is divided into left ventricular (stagnation of blood in the small circle, bleeding of the large one), right ventricular (blood fills the large circle, in the small circle there is a deficiency), mixed, when both ventricles are affected.
In the elderly, it is customary to pay special attention to hemodynamics, according to which they distinguish:
- hypokinetic failure - the heart releases a minimum of blood into the bloodstream, which causes shock;
- stagnant, when venous blood stagnates in a large circle, causing pulmonary edema and asthma.
But most often in patients over 60, HF is divided according to precipitating factors into:
- overload – normal blood flow is disrupted due to high load on the heart, while contractile function is preserved;
- myocardial – the normal ability of the myocardium to contract and rest is lost due to damage to the walls of the heart muscle;
- mixed.
Different gradations of heart failure do not exclude common causes of its development.
How is heart failure treated in old age?
Modern drug therapy can effectively combat heart failure. Treatment in old age involves the use of the following groups of drugs:
- Cardiac glycosides, for the production of which the foxglove plant is used, are now actively used in the treatment of heart failure in old age. Drugs in this group increase the force of heart contractions and affect metabolic processes in heart cells, which significantly improves blood supply to the body. However, the side effects of cardiac glycosides, especially when treating elderly patients, can be much stronger than the effect of treatment with them. Therefore, you should take drugs from this group only as prescribed and under the supervision of a doctor;
- Diuretics have been used since the 1950s to stimulate the elimination of excess fluid and salt from the body through urine. Drugs in this group support the functioning of the heart, reducing the volume of circulating blood, facilitating blood flow, and lowering blood pressure;
- Vasodilators are a group of modern drugs that help dilate peripheral arteries and facilitate the passage of blood through the vessels, which, in turn, significantly facilitates the work of the heart. This class of drugs includes nitrates, calcium channel blockers, etc.
In emergency situations, for example, when disorders of the heart valves lead to heart failure, treatment in old age is carried out using surgical methods. In some cases, only a heart transplant can save the patient's life.
Treatment of heart failure in old age is associated with the following difficulties:
- The presence of one or more concomitant diseases, taking multiple medications at the same time;
- The need to carefully monitor the dosage of drugs and the duration of their use. Usually, at the beginning of therapy, the doctor prescribes a small dose, which can be increased later;
- High risk of side effects, including allergies;
- Forgetfulness of an elderly patient, lack of discipline in taking medications;
- The patient lacks motivation to recover.
Medications
There are no drugs that are prescribed only for the treatment of insufficiency; they are all used to treat other diseases of the cardiovascular system.
Most often, older people are prescribed drugs for complex treatment. These include drugs from the following groups:
| Drug group | Name of drugs | Action | Contraindications |
| ACE inhibitors | Captopril, Enalapril, Quinapril, Lisinopril, Ramipril | Improve metabolism, reduce the body's need for oxygen. | Contraindicated in cases of narrowing of the renal arteries or renal stenosis, or with initially low blood pressure. When using the drug during hypotension, it is fraught with consequences - stroke, heart attack. |
| Combined ACE inhibitors | Capozide, Enap N, Enap HL, Korenitek | Used for persistent fluid retention in the body together with the diuretic hypothiazide | The same |
| Diuretics (diuretics) | Hydrochlorothiazide, Cyclomethiazide, Furosemide, Torasamide, Chlorthalidone. Potassium-sparing: Triamterene, Amiloride | Prescribed for fluid retention accompanied by stagnation of blood in the lungs or peripheral edema. Designed to remove excess salt from the body | Low potassium levels in the body, diabetes, kidney failure. Potassium-sparing diuretics are contraindicated for hyperkalemia. |
| Glycosides | Aurocard, Digosin, Digofton | Prescribed to change the basic functions of the heart - shortening systole, reducing heart rate, improving blood flow, increasing stroke volume, slowing heart rate. | Myocardial infarction, ventricular arrhythmia, heart block, acute coronary syndrome |
| Beta blockers | Anaprilin, Atenolol | Reduce heart rate, lower blood pressure. As a result, oxygen consumption by the heart muscle decreases. | Bronchial asthma, chronic lung diseases, heart failure, diabetes mellitus |
| Nitrates | Nitroglycerin, Isosorbide dinitrate, Isosorbide mononitrate | Used to relieve angina attacks | Low blood pressure, acute myocardial infarction, increased ICP, severe glaucoma |
| Antiarrhythmic drugs | Magnesium, Adenosine | Reducing arrhythmia, improving metabolism | Sinus bradycardia, sick sinus syndrome, low blood pressure, hormonal disorders |
| Calcium antagonists | Verapamil, Diltiazem | Prescribed to inhibit the flow of calcium into smooth muscles | Myocardial infarction, acute coronary syndrome |
Prevention of heart failure in old age
The most important factor for a healthy, fulfilling life is proper balanced nutrition. This is especially true for older people with heart failure. So, let's talk about what principles should be followed.
- Diversify your diet, include products of both plant (fruits, vegetables, cereals, baked goods, etc.) and animal (fish, meat, eggs, dairy products, etc.) origin. Such a menu will provide your body with those vitamins, minerals and nutrients that are necessary for its normal functioning.
- Follow your diet . Nutritionists recommend eating at the same time, because under the influence of a reflex, gastric juice, which is necessary for normal digestion, begins to be secreted most actively. The daily diet should be divided into breakfast (or two breakfasts), lunch and dinner (or two dinners). On average, food should be taken three to four times a day, but if you have health problems, say, being overweight, doctors advise doing this in four to five meals, without expanding your diet. It is recommended to consume the largest amount of food not before bedtime, but in the first half of the day. However, going to bed “on an empty stomach” is not at all necessary. A glass of kefir or yogurt, fruit will only bring benefits.
- Do not overeat, because this can become a habit and threatens not only excess weight, but also the development of many diseases: diabetes mellitus, coronary heart disease, heart failure in old age, etc. In addition, overeating is a strong burden for the body, reduces performance and vitality. tone.
- Carry out proper culinary processing of products. For each type of product, there are recommendations regarding the optimal time for their temperature treatment. For example, in order for cabbage to retain its nutrients, vitamins and minerals, you need to stew or cook it for no more than 20-30 minutes. Otherwise, your dish will become absolutely useless for the body. And don’t forget about doctors’ recommendations to eat enough raw fruits and vegetables.
- Consider the chemical composition and calorie content of food . Products for preparing a particular dish must be selected correctly. This rule applies to all people. However, it is especially relevant for those who suffer from diabetes, atherosclerosis, heart disease, including heart failure in old age. Nutritionists recommend focusing on foods with minimal or no cholesterol content. Those who are overweight should give preference to low-calorie foods.
- Learn the chemical characteristics of each food product . Any vegetable oil, for example, is an excellent choleretic agent, so eating it will protect you from cholecystitis. In addition, this popular product is rich in polyunsaturated fatty acids, which can strengthen the body's defenses, and vitamin E, which plays an important role in the prevention of atherosclerosis. It is no coincidence that experts recommend excluding animal fats from the diet and supplementing it with vegetable fats. However, remember that processing at high temperatures partially destroys the beneficial properties of vegetable oil. Therefore, it is better to use it for seasoning various cold dishes.
- Consult a specialist, do not self-medicate. Preparing a daily diet without a detailed study of the patient’s health status often leads to exacerbation of diseases. There are diets that have been tested in practice and are effective for a specific disease. Before making nutritional recommendations for a patient who suffers from heart failure in old age, the specialist must find out whether there are any concomitant diseases or allergic reactions to certain foods.
A sedentary lifestyle, which can cause disruption of neuro-reflex reactions in the body, also has a negative impact on our health. Such changes can lead to metabolic disorders, the development of atherosclerosis and diseases of the cardiovascular system, including heart failure in old age.
In everyday life, each of us performs some physical activity that has already become habitual, but it is not always enough. There are standards for physical activity necessary for full functioning.
To express the volume of muscular work performed, an indicator of the amount of energy consumption is used. On average, human energy consumption per day is 2880-3840 kcal. The value of this indicator varies depending on the individual characteristics of a person - gender, age, body weight. Part of the energy is spent on basic metabolic processes and maintaining normal functioning of the body. About 1200-1900 kcal every day is needed for muscle activity.
Physical activity is the most important factor in the prevention of heart failure in old age. Thanks to it, the immune system is strengthened, the body resists hypoxia, stress, temperature changes, radiation, etc. An active lifestyle also has a beneficial effect on the state of the cardiovascular system, reducing the risk of death from a heart attack by 70% compared to those people who move little. Older people in good physical shape remain able to work much longer.
As we age, the human body, including its cardiovascular system, changes significantly. Physical exercise, for example, gymnastics, will help to avoid many negative phenomena. By performing them regularly, you can get rid of excess fat mass, normalize your heart rate and blood pressure, lower blood cholesterol levels, and also stop the development of atherosclerosis.
Moderate physical activity is an excellent prevention of heart failure in old age, because it helps strengthen the main engine of blood circulation - the heart muscle.
Recreation in the fresh air, walking, short leisurely jogs, and swimming have a beneficial effect on health. No less useful are winter outdoor activities: ice skating, skiing.
Do not forget about the enormous benefits of water procedures: a bath (with healing salts), a shower (contrast is recommended for hardening), swimming in the pool.
Those who suffer from heart failure in old age need to consult a doctor about permissible physical activity, as well as the usefulness of certain procedures, for example, visiting a sauna and steam bath. A specialist will help you choose a set of exercises to perform daily.
Read material on the topic: Hypertension in the elderly: treatment and consequences
Consequences
The consequences of heart failure are nonspecific; they largely depend on the type of pathology and the form of its course.
In medical practice, the following are the most common complications:
- Heart rhythm disturbances leading to death. People diagnosed with heart failure are 50% more likely to die than older people without a diagnosis.
- Infectious lesions and bronchopneumonia. Due to stagnation of blood and fluid in cells and tissues, as well as a decrease in respiratory function, favorable conditions appear for the spread of infection, in particular to the lungs and upper respiratory tract.
- Bleeding in the lungs. As a result of pulmonary edema and the onset of cardiac asthma, patients are at risk of bleeding in the lungs.
- Infarction of the lungs and heart, embolism.
- Liver failure. As a result of prolonged venous stagnation, liver function is impaired.
- Chronic renal failure.
- Chronic cardiocerebral insufficiency.
- Cachexia of the heart. Appears as a result of disrupted metabolic processes, insufficient absorption of fats. Leads to generalized anorexia.
Impaired heart function affects the entire body in particular, because our heart is our motor. The more wear and tear on the motor, the higher the chances of systematic and functional failures throughout the body. This is why, in old age, heart failure is a common problem for which people consult doctors.
Due to age-related changes and the presence of concomitant pathologies, which in one way or another force the heart to work much harder, signs of heart failure appear in older people. Timely treatment of the problem allows us to stop pathological changes in our body and allow the heart to function as before.
Heart failure in old age - prognosis for life
Medical statistics show that about 50% of patients with this diagnosis live more than five years. However, we should not forget about the seriousness of such a disease as heart failure, because the prognosis for life in old age in this case depends on many factors: the severity of the disease, the patient’s lifestyle, the presence of concomitant diseases, the effectiveness of therapy and many others. Therapy for heart failure in old age is aimed at restoring heart function, improving quality of life and restoring the patient’s ability to work. Timely and competent treatment of heart failure in old age significantly improves the prognosis for the patient’s life.
Diagnostics
To make a reliable diagnosis, there is a special algorithm that has been worked out over the years:
- collection of complaints, physical examination;
- UBC, OAM, biochemistry, testing for hormones, autoantibodies;
- load tests;
- ECG, EchoCG, Doppler - helps to identify the causes of heart failure;
- ventriculography with radioisotopes - assessment of the potential of the ventricles, their capacity, contractility;
- plain X-ray of the chest organs;
Diagnosis of heart failure is recommended for everyone who is at risk, that is, in one way or another, associated with provoking factors. Even if they don't have any symptoms. It must be remembered that heart failure is a symptom, the identification of which can prevent serious complications of other concomitant pathologies.
Why is it developing?
In the elderly, pathology manifests itself in connection with biochemical and physiological processes in the heart muscle associated with age-related changes in the body. The appearance of the first signs is observed after 70 years. In some patients, by this time the pathology is already in the stage of decompensation.
Atherosclerotic processes progress, under the influence of which the vascular wall thickens. The pathological process extends to large and small vessels.
The smallest ones are stretched, and damage affects the vessels of the brain and heart. As a result of the ischemic process, muscle tissue is gradually replaced by fibrous tissue, the development of diffuse or focal cardiosclerosis is observed, and the contractility of the myocardium is increasingly reduced.
As a result of stenosis and other vascular changes, the left ventricle is overloaded. A person suffers from orthostatic hypertension, accompanied by dizziness as a result of a sudden change in body position.
Scar changes appear on the aortic valve, tissue elasticity decreases and calcification is observed. Due to the fact that the valve leaflets cannot fully close, the load on the left ventricle increases. The pathological process extends to the mitral valve. After ten years, manifestations of deficiency appear.
Over the years, the functioning of the thymus gland is disrupted, the immune defense mechanisms weaken and can no longer compensate for functional disorders.
The heart does not pump all the necessary blood and leads to the development of oxygen starvation of tissues and overload of the right parts of the heart.
The risk of developing a pathological condition increases if a person suffers from:
- arterial hypertension;
- thyrotoxicosis;
- myocarditis;
- hypothyroidism;
- congenital or acquired defects;
- pericarditis;
- chronic obliterating pulmonary disease;
- cardiosclerosis as a result of atherosclerosis or myocardial infarction;
- damage to the heart muscle by toxic substances and allergic damage to the myocardium.
Therefore, in the presence of such pathologies, treatment must be carried out.
No. 2. Cardiac glycosides
Medicines are mainly made from herbal ingredients. When taken correctly, they provide a good antiarrhythmic and cardiotonic effect. Tablets are prescribed in therapeutic doses for chronic or acute heart failure. They improve myocardial function, ensuring smooth functioning of the heart muscle.
Strophanthin
It is fast-acting and does not accumulate in the body, thereby not turning from a medicine into a “heart poison”. It is withdrawn after the day following administration, but the therapeutic effect does not decrease. The result is visible after a quarter of an hour if administered intravenously.
Digoxin
It is most effective in chronic heart failure. Consists of foxglove woolly, which acts as a vasodilator. Among the main properties of the drug are a diuretic and inotropic effect. Against this background, swelling goes away and myocardial functions are restored.
Digitoxin
The action is similar to the previous medicine, but is prescribed less frequently. Effective in chronic forms of heart failure. It has an overly active composition that can cause intoxication if used incorrectly. It acts more slowly, the result is noticeable after 6 hours.
General information about the disease
Symptoms of heart failure manifest differently in young and old people. Likewise, the reasons that provoke the development of this condition may differ.
HF before old age is usually associated with heart and vascular diseases. For example, it can be triggered by severe myocarditis, myocardial infarction, viral or bacterial infections that cause complications in the heart muscle.
In older age, heart failure develops slowly, and symptoms increase gradually. For some time, signs of functional deficiency may not appear at all. Due to its hidden course, the disease is often confused with other pathologies.
Treatment and care.
Treatment of patients with chronic heart failure is based on a combination of general measures and drug therapy.
Treatment should be well tolerated by the patient and not impair his quality of life. Slowing the progression of pathological changes is of great importance for protecting the heart.
General measures include: balanced nutrition with limiting table salt to 3-5 g and liquid to 1 liter per day, excluding fatty meats, fatty dairy products, including potassium-containing products in the diet (dried apricots, raisins, baked potatoes, nuts, Brussels sprouts, bananas, peaches, buckwheat and oatmeal, veal); constant control of body weight; complete cessation of smoking and limiting the consumption of alcoholic beverages; daily feasible physical exercise, walking for at least 30 minutes a day; the ability to restore emotional balance; education of the patient and his close relatives in “schools for patients with CHF”.
Drug treatment is carried out with angiotensin-converting enzyme inhibitors (cantonril, lisinoril, nerindonril), diuretics (gynothiazide, furosemide, torsemide), aldosterone receptor blockers (spironolactone, enlerenone), adrenoblockers (carvedilol, metonrolol, 6isonrolol, ne6ivolol ), cardiac glycosides (digoxin is necessary remember about glycoside intoxication, often in the form of rhythm and conduction disturbances), peripheral vasodilators (nitrates, sodium nitronrusside), anticoagulants (warfarin), antiplatelet agents (aspirin), antiarrhythmic drugs (amiodarone, sotalol).
Heart failure is the most common cause of hospitalization in elderly patients and the most common cause of disability and mortality.
No. 5. Nitrates
Drugs in this group have venodilating properties. In addition to eliminating stagnation in the blood channels, the drug reduces myocardial ischemia and dilates the coronary arteries.
Glyceryl trinitrate
The medication is used to prevent angina pectoris and dilate blood vessels. The medicine increases metabolic processes, reducing the heart's need for oxygen. Available in capsule and tablet form. You are allowed to take no more than 6 units per day. You can take 0.5 tablets at a time.
Nitroglycerine
The drug is aimed at reducing the heart's need for oxygen. When taken regularly, the main muscle gets rid of the stress that occurs due to heart failure. The daily norm is prescribed by the doctor, taking into account the characteristics of the patient’s body.
Symptoms
There are a number of signs that indicate the presence of heart failure. To reliably determine that a person suffers from this disease, it is necessary to establish a diagnosis in a hospital setting by conducting a series of examinations.
Characteristic symptoms:
- A hysterical cough, in which in some cases sputum comes out and may contain blood clots. Typically, this phenomenon begins when a person lies on a bed or other horizontal surface. As a result, regular sleep disturbance occurs, which negatively affects the general condition of the patient.
- Difficulties associated with the breathing process. Patients often suffer from shortness of breath.
- The skin looks pale and may have a bluish tint. This phenomenon is caused by insufficient blood circulation and a decrease in the amount of oxygen entering the cells.
- Swelling all over the body. They appear because the body cannot cope with the timely removal of fluid.
- Chronic fatigue, inability to work as usual, which patients often associate with the aging process.
- Irritability, nervous tension, gloomy mood.
- Violation of mnemonic processes, other problems associated with brain activity.
- Distracted perception, confusion, inability to remember even a minimum of new information.
- Dizziness, tinnitus, and other symptoms indicating chronic problems in the body.
- Loss of appetite, complete removal of certain foods from the diet.
- Chronic nausea, possible attacks of vomiting.
- Renal dysfunction.
- Involuntary urination, often patients suffer from it during sleep.
- Unpleasant sensations, heaviness in the sternum.