Vasculitis (ICD code 10) is a pathological condition of the body in which the walls of blood vessels of different sizes become inflamed: capillaries, venules, arteries, veins, arterioles.
They can be located in the dermis, at the border with the hypodermis, or in any other body cavity. The disease vasculitis is not one disease, it is a group of pathologies that are united by a single characteristic.
Doctors identify several types of illness, differing in location, severity of the process, and etiology:
- Primary. It begins as an independent disease with its own symptoms.
- Secondary. Develops in the presence of other pathologies (tumors, invasion). May occur as a reaction to an infection.
- Systemic. The disease progresses in different ways. It is characterized by vascular damage with inflammation of the vascular wall and may be accompanied by necrosis.
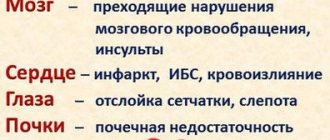
With vasculitis, inflammation can lead to serious problems. Complications depend on which blood vessels, organs, or other body systems are affected.
What kind of disease is this?
Vasculitis – what is it in simple terms? This is a group of diseases accompanied by inflammation and subsequent necrosis (death) of the vascular wall. This group of pathologies leads to a significant deterioration in blood circulation in the tissues surrounding the vessel. Different forms of these ailments have both characteristic and general symptoms (fever, weight loss, rash that does not disappear with pressure, joint pain). If left untreated, the primary lesion may spread and cause damage to other tissues or organs. Subsequently, the disease can lead to disability and even death.
So far, vasculitis remains insufficiently studied, and experts have not come to a consensus on the causes and mechanisms of inflammation, classification and treatment tactics. Now this disease is classified as a systemic connective tissue disease, and is treated by rheumatologists. If necessary, infectious disease specialists and dermatologists may be involved in therapy.
According to statistics, vasculitis affects both men and women equally often, and they are most often detected in children and the elderly. Every year the number of such rheumatologist patients increases, and experts believe that this increase in incidence is associated with the uncontrolled use of immune stimulants and environmental deterioration.
Symptoms
Ocular disorders may be the first diagnostic manifestation of a potentially life-threatening disease.
Redness and pain in the eyes may be the first symptom of a dangerous disease of the visual system.
Retinal vasculitis has the following symptoms:
- redness and pain in the eyes;
- fogging;
- increased sensitivity to light;
- hemorrhages and tissue compactions (infiltrates) on the retina;
- the appearance of exudates around the vessels of the eye, which lead to the formation of a white membrane or peculiar couplings, which are areas of swollen retina.
Neurovasculitis is a disease that develops as a result of neuroses or hypothermia of the body. With this type of pathology, a veil or bright flashes may appear before the eyes, brain spasms, disorientation, and headaches. Retinovasculitis is most often a secondary manifestation of rheumatism, fungal, viral infections, brucellosis and affects the arteries supplying the optic nerve head. It is characterized by retinal edema, pinpoint hemorrhages, and noticeable cotton wool-like fibrin formations. Lack of treatment leads to an irreversible, serious decrease in visual acuity.
Causes
The etiology of vasculitis has not been thoroughly studied. This pathology is often associated with a variety of viral infections and immune diseases. Vasculitis often causes an allergic reaction to certain medications.
Vasculitis can develop as a complication of previous infections. In this case, the body experiences an abnormal response of the immune system to the infection, resulting in the destruction of blood vessels.
Precursors of vasculitis can also be old or chronic autoimmune diseases (glomerulonephritis, reactive arthritis, inflammation of the thyroid gland, systemic lupus erythematosus, Schwartz-Jampel syndrome, etc.)
Treatment
When a diagnosis of vasculitis is made, treatment can be jointly carried out by surgeons, ophthalmologists, neurologists, therapists, otolaryngologists, nephrologists and other specialists who will monitor both internal damage and the effect of prescribed drugs. During the treatment process, first of all, inflammation is relieved so that the picture of the disease becomes clearer. The immune system is then suppressed so that the hostile system no longer resists the blood vessels. The last stage is improving blood flow.
Classification
Vasculitis is classified according to the 2012 Chapel Hill Consensus Conference (CHCC) as follows:
By formation:
1) Primary - the development of the disease is caused by inflammation of the walls of the blood vessels themselves;
2) Secondary - the development of the disease is caused by the reaction of blood vessels against the background of other diseases. Secondary can be:
- Vasculitis associated with hepatitis B virus (HBV);
- Cryoglobulinemic vasculitis associated with hepatitis C virus (HCV);
- Vasculitis associated with syphilis;
- ANCA vasculitis (ANCA) associated with medications;
- Drug-associated immune complex vasculitis;
- Vasculitis associated with cancer (syn. “paraneoplastic vasculitis”)
- Other vasculitis.
Vasculitis of small vessels
ANCA-associated vasculitis (AAV):
- Microscopic polyangiitis (MPA) is a not fully understood disease that is associated with the production of antibodies to the cytoplasm of neutrophils, which causes an inflammatory process to develop simultaneously in several organs (most often the lungs and kidneys become victims), and granulomas do not form. Doctors note the following features of the clinical course of GPA: the development of severe pulmonary-renal syndrome (about 50%), damage to the kidneys (about 90%), lungs (from 30 to 70%), skin (about 70%), and visual organs (about 30%). ), peripheral nervous system (about 30%), gastrointestinal tract (about 10%).
- Granulomatosis with polyangiitis (GPA, Wegener's granulomatosis) is a severe and rapidly progressive autoimmune disease characterized by granulomatous inflammation of the walls of small and medium-sized blood vessels (capillaries, venules, arterioles and arteries) involving the eyes, upper respiratory tract, and lungs in the pathological process , kidneys and other organs. If not adequately treated, it can lead to death within 1 year. Doctors note the following features of the clinical course of GPA: damage to the upper respiratory tract (90% or more), kidneys (about 80%), lungs (from 50 to 70%), visual organs (about 50%), skin (from 25 to 35% ), peripheral nervous system (20 to 30%), heart (20% or less), gastrointestinal tract (about 5%).
- Eosinophilic granulomatosis with polyangiitis (EGPA, Churg-Strauss syndrome) is an autoimmune disease caused by an excess of eosinophils in the blood and outside the bloodstream, characterized by granulomatous inflammation of the walls of small and medium-sized vessels involving the upper respiratory tract, lungs, kidneys and other organs in the pathological process. Often accompanied by bronchial asthma, runny nose and other sinusitis, elevated body temperature, shortness of breath, eosinophilia.
Immune complex vasculitides of small vessels:
- Immunoglobulin-A associated vasculitis (hemorrhagic vasculitis, Henoch-Schönlein purpura, Henoch-Schönlein disease, allergic purpura);
- Cryoglobulinemic vasculitis is characterized by damage to the walls of small vessels, mainly the kidneys and skin, the main cause of which is an excessive amount of cryoglobulins in the blood serum, due to which they first settle on the walls of the vessels and then modify them.
- Hypocomplementary urticarial vasculitis (anti-C1q vasculitis);
- Anti-GBM disease.
Vasculitis of medium-sized vessels
— Periarteritis nodosa (polyarteritis nodosa, periarteritis nodosa) is an inflammatory disease of the arterial wall of small and medium-sized blood vessels, leading to the development of aneurysms, thrombosis, and heart attacks. At the same time, there is no kidney damage (glomerulonephritis). The main causes are considered to be intolerance to certain medications, as well as persistence of the hepatitis B virus (HBV).
— Kawasaki disease is an acute and febrile disease characterized by inflammatory damage to the walls of small, medium and large-diameter veins and arteries, which is often combined with mucocutaneous lymphatic syndrome. Occurs mainly in children.
Vasculitis of large blood vessels
— Giant cell arteritis (GCA, Horton's disease, temporal arteritis, senile arteritis) is an autoimmune disease characterized by granulomatous inflammation of the main branches of the aorta, most often the branches of the carotid and temporal arteries. In many cases, it is combined with polymyalgia rheumatica, pain and some stiffness in the joints of the pelvic girdle and shoulders, as well as an increase in ESR. The cause is considered to be human infection with hepatitis, herpes, influenza and other viruses. It occurs mainly in people over 50 years of age.
— Takayasu arteritis (nonspecific aortoarteritis) is an autoimmune disease in which a productive inflammatory process develops in the walls of the aorta and its branches, leading them to obliteration. As the disease progresses, pathological processes such as the formation of fibrous granulomas, destruction of elastic fibers, necrotization of smooth muscle cells of the blood vessel wall are observed, after which, after some time, thickening of the intima and medial tunic of the vessel is possible. Sometimes there may be no pulse in the hands, which is why the disease has another name - “pulseless disease.” According to statistics, Takayasu arteritis most often develops in women, in an approximate proportion of men 8 to 1, and patients are young people, from 15 to 30 years old.
Vasculitides that can affect blood vessels of varying sizes
- Behçet's disease is characterized by an inflammatory process in the arteries and veins of small and medium caliber, accompanied by frequent relapses of ulcerative formations on the mucous membranes of the mouth, eyes, skin, genitals, as well as damage to the lungs, kidneys, stomach, brain and other organs.
- Cogan's syndrome is a rare rheumatic disease characterized by inflammation of the eyes and ears. Therefore, Cogan syndrome leads to hearing, vision and balance disorders.
Systemic vasculitis
- Hemorrhagic vasculitis (Henoch-Schönlein purpura) is characterized by aseptic inflammation of the walls of small vessels (arterioles, venules and capillaries), multiple microthrombosis, developing mainly in the vessels of the skin, kidneys, intestines and other organs. Often accompanied by arthralgia and arthritis. The main cause of hemorrhagic vasculitis is the excessive accumulation of circulating immune complexes in the bloodstream, in which antigens predominate, due to which they settle on the inner surface of the blood wall (endothelium). After re-activation of proteins, the vascular wall changes;
- Lupus vasculitis;
- Behçet's disease;
- Rheumatoid vasculitis;
- Vasculitis in sarcoidosis;
- Takayasu arteritis;
- Other vasculitis.
Vasculitis of individual organs:
- Cutaneous arteritis;
- Cutaneous leukocytclastic angiitis - characterized by an isolated inflammatory process of blood vessels in the skin, without concomitant glomerulonephritis or systemic vasculitis;
- Primary angiitis of the central nervous system;
- Isolated aortritis;
- Other vasculitis.
Diagnosis of cerebral vasculitis of the brain (vasculitis of the central nervous system)
The diagnosis is made based on the results of clinical, laboratory and neuroimaging (MRI, angiography) studies. To confirm it, a biopsy of the affected area of the vessel with histological examination is required.
The combination of inflammatory processes in the central nervous system and vascular lesions indicates cerebral vasculitis.
To diagnose vasculitis, the American College of Rheumatology classification should be used.
- General laboratory diagnostics: blood test, inflammatory parameter (C-reactive protein, erythrocyte sedimentation rate), creatine kinase, electrophoresis, immunoelectrophoresis, creatinine, glomerular filtration rate (GFR), urine status, including protein, glucose, albumin.
- Special laboratory tests:
- hepatitis serology (positive results up to 60% in patients with polyarteritis nodosa)
- pANCA (Churg-Strauss syndrome, microscopic polyarteritis)
- cANCA (Wegener's granulomatosis)
- ANA (titer is increased in almost all collagenoses)
- antibodies to ds-DNA, lupus anticoagulant (lupus erythematosus)
- complement C3 and C4 (lowered in systemic lupus and generalized vasculitis, increased in systemic inflammation = acute phase protein)
- aHTH-Ro-(SS-A-) and aHTH-La-(SS-B-) antibodies (Sjogren's syndrome)
- anti-5Cb-70 antibodies (scleroderma)
- RNP antibodies
- cryoglobulins (often elevated in non-ANCA vasculitis)
- rheumatoid factor
- serology for syphilis, antibodies to borrelia, HIV confirmation
- CSF: cell number, protein, glucose, oligoclonal bands, lactate.
Ultrasound of the abdominal organs, electroneurography, somatosensory evoked potential, electromyography.
Differential diagnosis
Cerebral vasculitis should be differentiated mainly from atherosclerotic stenosis of intracranial arteries (taking into account age and risk factors).
First signs
Common signs of vasculitis are:
- headaches, dizziness, fainting;
- visual impairment;
- sinusitis, sometimes with the formation of nasal polyps;
- damage to the kidneys, lungs, upper respiratory tract;
- increased fatigue, general weakness and malaise;
- increased body temperature;
- pale skin;
- lack of appetite, nausea, sometimes vomiting;
- weight loss;
- exacerbation of cardiovascular diseases;
- sensitivity disturbance - from minimal to hypersensitivity;
- arthralgia, myalgia;
- skin rashes.
The symptoms (clinical manifestations) of vasculitis largely depend on the type, location and form of the disease, so they may differ somewhat, but the main symptom is a violation of normal blood circulation.
Forecast
The prognosis for vasculitis depends on the form of the disease and how quickly treatment is started. Thus, with early therapy with cytostatics in combination with glucocorticosteroids, the five-year survival rate of patients with vasculitis reaches 90%. This means that 9 out of 10 patients live longer than 5 years. Without timely treatment, the five-year survival rate is 5%.
The prognosis worsens in the following cases:
- onset of the disease after 50 years;
- kidney damage;
- damage to the gastrointestinal tract;
- damage to the central nervous system;
- damage to the aorta and heart vessels.
This means that people with such conditions need to be careful about their health and strictly follow the treatment regimen. In this case, it is possible to avoid the development of severe complications.
Diagnostics
Most of the procedures used during the examination and treatment of a patient with vasculitis are carried out in the diagnosis and treatment of other diseases, so they are not specific to vasculitis. However, without them, a reliable and accurate diagnosis of vascular inflammation is impossible.
During the examination of the patient, various modern methods are used.
- Angiography.
This method evaluates the structure and passage of blood vessels, resulting in the identification of blockages, inflammation or other abnormalities. There are many ways to perform angiography. Ultrasound is most often used to examine large vessels without the use of X-rays or dyes. Magnetic resonance imaging (MRI) uses a magnetic field to create detailed images of certain blood vessels and, if necessary, can be combined with special dyes (contrast agents) given by injection to the patient. Computed tomography (CT), which uses X-rays, evaluates the structure of blood vessels. It is usually performed using contrast dyes. A positron emission tomography (PET) scan requires an injection of radioactive drugs and can be helpful in identifying where blood vessels are inflamed.
- Abdominal ultrasound examination.
It is based on the use of sound waves, with the help of which a picture of the organs and anatomical structures located in the abdomen is created. This test can show whether there are abnormalities in the abdominal cavity.
- Biopsy.
During the procedure, a small piece of tissue is removed from the affected area or organ, such as the skin or kidney. The tissue is then examined under a microscope by a pathologist. If necessary, special tests may be performed to identify disease affecting the organ.
- Bronchoscopy.
A procedure during which the doctor examines the patient's respiratory tract (trachea and bronchi). The purpose of the study is to determine the area of damage, and biological samples may also be collected for biopsy or washing. This allows you to clarify the cause of the disease, especially if it developed due to infection. The trachea and bronchi are the main tubes that carry air to the lungs. Typically a fiberoptic bronchoscope (thin, flexible, with a telescope at the end) is used.
- DEXA scan.
Also known as dual-energy X-ray absorptiometry. This is a test that measures bone density. Can be used to identify or monitor bone strength, especially in long-term patients treated with steroid drugs.
- Electrocardiogram.
A simple and painless diagnostic method for recording the electrical activity of the heart. Often provides useful information about the condition of the heart and can provide information on whether an organ is associated with vasculitis.
- Spirometry.
Refers to pulmonary function tests. The volume of the lungs, the amount of air inhaled and exhaled, and how well the transfer of oxygen from the lungs to the blood occurs is determined. This may be useful for monitoring patients whose lungs or airways have been affected by vasculitis.
- Tracheostomy.
Tracheostomy is sometimes necessary for patients whose main airway is blocked or narrowed as a result of damage caused by vasculitis. This provides direct access to the trachea by making a surgical opening in the anterior neck. This allows air to flow directly into the lungs, allowing patients to breathe properly when their upper airways are blocked.
Tracheostomy may be a temporary measure, especially for patients who have severe vasculitis. It can also be used permanently if irreversible changes have occurred in the body. For patients with a permanent tracheostomy, a special tube is inserted to hold the opening open and allow normal speech. This allows you to live a more or less normal life.
- Electromyography.
Electrical stimulation of muscles (usually in the arms or legs) is assessed to look for evidence of abnormal muscle function, such as in vasculitis. Often the test is performed in combination with a nerve conduction study.
- Echocardiography.
An ultrasound test that uses sound waves to create images of the heart. The test reveals the size and shape of the heart, as well as the order in which the chambers and valves work.
- Computed tomography (CT).
Provides more detailed information about internal organs than conventional radiography (X-ray).
- Positive emission tomography.
The test is also known as a PET scan. During this procedure, three-dimensional images are taken that show the level of metabolic activity, which is an indicator of inflammation.
- Analysis of urine.
A simple but very important urine quality test identifies abnormal levels of protein or blood cells in the urine. If such signs are detected, then kidney damage is diagnosed.
Doctors' actions
Self-medication for vasculitis is unacceptable, especially since you cannot use folk remedies that promise a quick cure without the use of “harmful” drugs. This disease can be treated only with the use of medications selected by the attending physician in accordance with the individual characteristics of the patient’s body.
In addition to the oral interview, medical history, and initial examination, the physician must provide a referral for one or more of the following tests:
- general and biochemical blood test;
- general and biochemical urine analysis;
- ECG;
- immunological analysis;
- biopsy;
- angiography;
- X-ray;
- ultrasound;
- kT.
Based on the results of such an examination, a rheumatologist can make an accurate diagnosis, identify the cause of the disease and recognize complications that have spread to other internal organs, even if the patient does not feel symptoms. If adjacent lesions are detected, additional tests are prescribed from the corresponding area, but this is done by a highly specialized doctor.
Therapy for vasculitis may vary in each specific case, since it is influenced not only by the individual characteristics of the patient, but also by the form of the pathology, the causes of its occurrence and its localization. In general, treatment is aimed at eliminating the initial source of the lesion, be it an infection or allergy, normalizing the immune system, generally cleansing the body of toxins, as well as preventing relapses and complications.
How to treat vasculitis: list of drugs
The choice of certain drugs for the treatment of vasculitis in adults can only be made by a doctor who takes into account the patient’s examination data, the severity and type of the disease. For a mild form, medications are prescribed for 2–3 months, for a moderate form - for about 6 months, and for a severe form - up to a year. If vasculitis is recurrent, then the patient is given therapy in courses of 4–6 months.
The following drugs can be used to treat vasculitis:
- non-steroidal anti-inflammatory drugs (Ortofen, Piroxicam, etc.) - eliminate inflammatory reactions, joint pain, swelling and rash;
- antiplatelet agents (Aspirin, Curantil, etc.) – thin the blood and prevent the formation of blood clots;
- anticoagulants (Heparin, etc.) – slow down blood clotting and prevent thrombus formation;
- enterosorbents (Nutriklinz, Thioverol, etc.) – bind toxins and bioactive substances formed during illness in the intestinal lumen;
- glucocorticosteroids (Prednisolone, etc.) – have an anti-inflammatory effect in severe vasculitis, suppress the production of antibodies;
- cytostatics (Azathioprine, Cyclophosphamide, etc.) - prescribed when glucocorticosteroids are ineffective and rapid progression of vasculitis, suppress the production of antibodies;
- antihistamines (Suprastin, Tavegil, etc.) - are prescribed only to children in the initial stages of vasculitis in the presence of drug or food allergies.
Symptomatic therapy is also carried out to eliminate the manifestations of the disease and alleviate the patient’s condition.
In case of severe autoimmune reactions in the patient’s body, the following can be used:
- Hemophoresis. During this procedure, a small amount of the patient’s blood is taken, passed through special filters on the device, cleared of toxins, and returned back into the patient’s bloodstream.
- Plasmophoresis. The effect of plasmaphoresis is similar to hemophoresis, only it is not the blood elements that are purified, but the plasma.
But despite the severe manifestations of the disease, the patient’s life is rarely endangered and the prognosis with timely treatment is in most cases favorable. But the treatment process takes a long time and his health depends on how accurately the patient follows medical recommendations.
Treatment of eye vasculitis in Moscow
As mentioned above, vasculitis rarely manifests itself as an independent disease, and therefore, when treating ocular vasculitis, priority is given to curing the disease that provoked the development of inflammation of the ocular vessels. So, if the cause is an infection, it is necessary to take measures to cure it, that is, carry out drug antimicrobial therapy and strengthen the patient’s immune system.
There are three main types of treatment for ocular vasculitis:
- 1) medicinal - glucocorticoids, angioprotectors, antioxidants and some other groups of drugs are used for this;
- 2) extracorporeal - blood purification using plasmapheresis;
- 3) surgical - various operations to eliminate the consequences of vasculitis (laser coagulation of the retina, lensvitrectomy, etc.).
The choice of a specific method of surgical treatment of ocular vasculitis is made depending on the indications and contraindications. To prevent the development of the inflammatory process, all such operations are performed in combination with glucocorticoid therapy.
As for the prognosis for eye vasculitis, it depends on how timely the underlying disease was identified and treated. To prevent relapses of inflammation of the blood vessels of the eyes, it is necessary to prevent infectious diseases, dress according to the season, and strengthen your immunity in all possible ways. For any eye problems, contact experienced ophthalmologists with a good professional reputation.
Consequences of vasculitis
Deterioration of blood supply to tissues around the affected vessels leads to severe damage to internal organs. Without timely and competent treatment, the consequences of vasculitis can lead to severe disability.
- Chronic renal failure is a violation of all kidney functions. Damage to kidney tissue caused by poor circulation. Lack of oxygen and nutrients leads to massive death of kidney cells.
- Intestinal obstruction in patients with vasculitis is often associated with intussusception. In this condition, one part enters the lumen of another, clogging it and disrupting the movement of food masses.
- Bleeding of internal organs - bleeding into the lumen of internal organs or other natural cavities. The cause of internal bleeding is rupture of the wall of large vessels or destruction of infiltrates associated with necrosis. Vasculitis is characterized by various types of bleeding: pulmonary, intestinal, uterine in women, hemorrhage in the testicle in men.
- Perforation of the stomach or intestines is a rupture of the intestinal wall and the release of its contents into the abdominal cavity. It is the most common complication of the abdominal form of hemorrhagic vasculitis. When blood vessels are damaged, the wall of the gastrointestinal tract does not receive proper nutrition, atrophies and becomes thinner. Rupture may occur as a result of spasm or stretching by a bolus of food. A life-threatening complication of this condition is peritonitis, an inflammation of the peritoneum.
- Heart damage. Malnutrition leads to depletion of the muscle fibers of the heart. They are stretched and deformed. With a complete lack of nutrition, cell death occurs.
- Hemorrhagic stroke is an intracerebral hemorrhage associated with a rupture of the vessel wall.
The photo shows the external manifestations of vasculitis on the legs
Prevention
Considering the fact that scientists today have not yet been able to unravel the nature of autoimmune diseases, it is not possible to talk about reliable prevention tools. However, a reliable opinion is that a healthy lifestyle reduces the risk of developing pathology. Psycho-emotional hygiene and the ability to protect oneself from stress in everyday life are of enormous importance.
In addition, it is extremely important to observe a work and rest schedule. When a person experiences physical and mental overload day after day, the body is forced to draw strength from internal reserves. But when these reserves are empty, the risk of developing diseases, including autoimmune diseases, increases. The immune response is provoked by an infection that penetrates the cells. Therefore, it is extremely important to prevent chronic foci of infections: tonsillitis, tonsillitis, sinusitis, and even caries.
If a genetically healthy immune system is able to cope with the increased load, but the immunity of a person who is at risk of encountering a pathology of this nature will certainly begin to attack the body’s own tissues.