BIOLOGICAL DEPARTMENT OF THE CENTER OF TEACHING EXCELLENCE
Author of the article Zybina A.M.
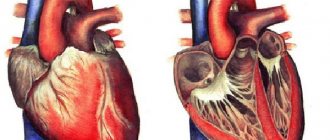
The heart is a pump that moves blood through the blood vessels through repeated rhythmic contractions. The heart consists of three layers (Fig. 1). The inner endocardium is homologous to the vascular endothelium, the middle myocardium consists of cardiomyocytes and has a contractile function, the outer epicardium consists of connective tissue. The human myocardium is thick, so its nutrition is provided by the coronary arteries. The heart is surrounded by a sac called the pericardium. The space between the epicardium and pericardium is filled with fluid, which reduces friction between the heart and adjacent tissues.
Rice. 1. The structure of the heart wall.
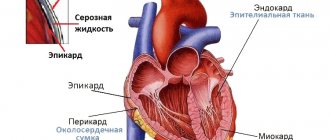
Rice. 2. Internal structure of the heart.
The heart consists of atria (right and left), two ventricles (right and left) (Fig. 2). The right and left halves of the heart do not communicate and are filled with different types of blood: the right - venous (depleted in oxygen), the left - arterial (enriched in oxygen). Blood always enters the atria of the heart through the veins, passes into the ventricles and then into the arteries. The backflow of blood is prevented by the heart valves. Between the atria and ventricles there are leaflet valves: tricuspid (tricuspid) on the right, bicuspid (mitral) on the left. Between the ventricles and arteries there are semilunar valves: on the right is the pulmonary valve, on the left is the aortic valve (Fig. 2, 3).
Rice. 3. Heart valves.
The process of contraction is called systole, relaxation is called diastole. The systole of both atria occurs simultaneously, as does the systole of both ventricles. The cardiac cycle at rest is approximately 0.8 s. Of these, 0.4 s the heart is completely in diastole, 0.1 s is in atrial systole and 0.3 s is in ventricular systole. During general diastole and systole of the atria, the leaflet valves are open and the semilunar valves are closed. During ventricular diastole, the leaflet valves close, and when the pressure in the heart begins to exceed the pressure in the aorta, the semilunar valves open.
The heart contracts autonomously from the nervous system because it has myogenic automaticity. This means that there are automatic nodes (pacemakers) that trigger the contraction of the heart. Automation nodes are located in certain places and obey a strict hierarchy (Fig. 4). The main node of automation, or the node of first-order automation, is located at the junction of the venous sinus into the right atrium and is called the sinoatrial (sinoatrial, SA node). Normally, from this node, excitation spreads throughout the heart and the heart contracts at its rhythm (60-80 beats/min at rest). The second-order automation node is located on the border of the atria and ventricles, and is called the atrioventricular (atrioventricular, AV node). Its rhythm is lower (about 40 beats/min) and does not appear during normal heart function. In order for the excitation to spread quickly and the contraction of the ventricular CMC to occur synchronously, there are special conducting fibers: the bundle of His, the branches of His and the Purkinje fibers. These cells can also generate spontaneous APs at a low frequency (about 20 beats/min), therefore such fibers are called the third-order automaticity node. Normally, this rhythm also does not appear.
Rice. 4. Location of automation nodes in the heart.
Despite the fact that the heart is capable of contracting autonomously, the nervous system adjusts the heart rate (HR). The sinoatrial node receives influence from the autonomic nervous system. With the action of the parasympathetic nervous system, heart rate decreases. In this case, the neurotransmitter is acetylcholine, and the regulation centers are located in the medulla oblongata. Activation of the sympathetic nervous system leads to an increase in heart rate. The neurotransmitter is norepinephrine, and the centers are located in the upper thoracic segments of the spinal cord. Regulation by the nervous system ensures that the heart rhythm is adjusted to the body’s load.
Rice. 5. Circulation circles.
The human heart provides continuous blood circulation through two circulation circles: large and small. The systemic circulation supplies oxygen to all tissues of the body. To effectively transport blood to the brain and other tissues, high pressure develops in the left ventricle and systemic arteries. The systemic circulation begins in the left ventricle, from where arterial blood enters the left aortic arch and is further distributed through the arteries, arterioles and capillaries. Capillaries are metabolic vessels that consist of a single layer of cells. Through them, gases, nutrients and metabolites diffuse from and into the blood. From the capillaries, venous blood collects into venules and veins. The veins coming from the intestines break up into a capillary network in the liver (portal system of the liver), where harmful substances that could come from food are neutralized. Veins from the lower extremities and abdominal organs are collected in the inferior vena cava, from the upper extremities and head - in the superior vena cava. From the back of the heart, the vena cava merges into the sinus venosus, which flows into the right atrium, from which blood flows into the pulmonary circle.
The pulmonary circulation serves to enrich venous blood with oxygen. Since the heart and lungs are located at approximately the same level, the pressure in the pulmonary circle is low. Venous blood moves through its arteries, and arterial blood moves through its veins. The small circle begins with the right ventricle, the contraction of which leads to the ejection of blood into the pulmonary arteries. Next, the blood enters the capillaries of the lungs, where it is enriched with oxygen. Arterial blood collects in veins, which drain into the left atrium.
Rice. 6. Heart during various types of medical examination. a) Ultrasound, b) MRI.
ECG
Electrocardiography (ECG) is a method of graphically recording the potential difference in the electrical field of the heart that arises during its activity. Registration is carried out using a device - an electrocardiograph. Simply put, electrical impulses always travel through the heart in a certain sequence. An ECG allows you to record the spread of electrical activity of the heart over time.
For the first time, an electrocardiogram was recorded by Auguste Desiree Waller (Fig. 7). He developed the theory of electrical fields of the heart, which was later developed by the Dutch physiologist Willem Einthoven. He was the first to use this method for diagnosis in 1906. Einthoven developed not only the theory of the ECG, but also methods for standardizing recording. For his services, he was awarded the Nobel Prize in Physiology or Medicine in 1924. Three standard leads according to Einthoven and is currently one of the main methods of ECG research.
Rice. 7. Auguste Desiree Waller and the first ECG recording.
Rice. 8. Standard leads according to Einthoven.
To measure the electrical activity of the heart, it must be placed in a coordinate system. As such a system, Einthoven adopted a triangle, the vertices of which are electrodes placed on the arms and legs. The side of the triangle directed from the right arm to the left is called the first lead, from the right arm to the left leg - the second lead, and from the left arm to the left leg - the third lead. The propagation of excitation is a vector quantity; the ECG recording reflects the projection of the electrical activity of the heart onto each lead. If the vector coincides with the direction of abduction, then the deviation will be positive, if they are opposite - negative (Fig. 9).
An ECG, in the case of standard electrode application, consists of a number of periodically repeating elements. Positive and negative deviations from the isoelectric line are usually called teeth. There are five teeth: P, Q, R, S, T.
Rice. 9. Projection of the vector of excitation propagation in the heart onto three standard leads. Source https://med.wikireading.ru/35207
Rice. 10. Interpretation of the ECG and its correspondence to the phases of the cardiac cycle. Source https://1poserdcu.ru/diagnostika/rasshifrovka-ekg-u-detej.html
The P wave is the lowest amplitude element of the ECG and reflects the spread of excitation through the atria. When the atria are excited, an isoelectric line can be seen on the ECG. As excitation spreads through the ventricles, the vector changes direction several times. This process reflects the QRS complex. At the same time, atrial repolarization occurs. Ventricular repolarization is reflected by the T wave.
With various pathologies of the heart, the conductivity of its parts for electricity changes, which leads to disruption of the ECG structure. The most striking example of a disorder is myocardial infarction. During a heart attack, the CMC group is affected. These cells are no longer capable of conducting electricity. Metabolites are released from them and disrupt the composition of the intercellular substance and the activity of neighboring cells. Those, in turn, close the slot contacts and stop conducting electricity. Over the course of several months or years, some of these cells can recover and begin to conduct PD again, while the other part may die. Since the thickest wall and the heaviest load are in the left ventricle, the likelihood of a heart attack is greatest there. Consequently, the QRS complex and T-wave will change on the ECG. Moreover, due to the constant change in the number of conducting cells, the shape of the ECG will change (Fig. 11). Typically, signs of a heart attack include the fusion of the QRS complex and the T-wave like a “cat’s back”, a strong increase in or inversion of the T-wave.
Rice. 11. Changes in the ECG shape during myocardial infarction. Source https://studopedia.info/9-34971.html
Rice.
12. ECG after a heart attack in three standard leads. Source https://zabserdce.ru/infarcire/infarkt-na-ekg.html # Human anatomy
Normal rhythm and propagation of the impulse in the heart
The contraction of the heart is the result of the generation of a cardiac impulse, the action potential of the pacemaker cells of the sinus node. The maximum number of pacemakers is located here, generating rhythm at a frequency of 60-100 times per minute. It is transmitted through conducting cells to the atrioventricular node, the main task of which is to delay the rhythm. Excitation reaches the AV node through bundles of conducting cardiomyocytes, which also have automaticity. However, they are capable of generating a rhythm at a frequency of 30-40 times per minute.
After the AV node, the rhythm normally spreads along conducting atypical cardiomyocytes to the His bundle, the automaticity of which is extremely low - up to 20 impulses per minute. Then the excitation reaches the final element of the conduction system - the Purkinje fibers. Their ability to generate rhythm is even lower - up to 10 per minute. Moreover, the main pacemaker, that is, the sinus node, generates impulses much more often. And each subsequent propagation of the action potential suppresses the rhythm of the underlying sections.
A decrease in the ability of the cardiac conduction system to generate a high-frequency rhythm from the sinus node to the Purkinje fibers is called an automaticity gradient. This process is explained by a decrease in the rate of membrane depolarization: in the sinus node, spontaneous slow diastolic depolarization is the highest, and as it moves towards the distal areas it is the least. The automaticity gradient is directed downward, which is a sign of a normally functioning cardiac conduction system.
Changes in the membrane potential of pacemakers
During cardiac diastole, the following ionic picture is observed in pacemaker cells: the number of potassium cations in the cell significantly predominates over sodium ions. Outside the cell, the concentration of cations is exactly the opposite. In this case, the resting potential of the pacemaker cell is -60 mV. Potassium currents at rest are ineffective because there are very few potassium ion channels on the membrane. This distinguishes them from contractile myocytes, where the resting potential is approximately -90 mV.
The nature of automaticity and its regulation
An atypical cardiomyocyte is able to perform its function due to calcium current through slow ion channels, resulting in the formation of an action potential. It is this process that underlies myocardial excitability. In contrast, SMDD has a different purpose. Its task is to automatically trigger the onset of depolarization at a certain frequency. It is the presence of the SMDD phase that is the nature of heart automaticity, the ability to spontaneously generate excitation in pacemaker cells.
The rate of development of SMDD is directly regulated by the somatic autonomic nervous system. At rest it is minimal due to the inhibitory effect of the vagus nerve. However, this does not mean that the automaticity of the heart stops. It’s just that the SMDD stage will last longer, which will provide a longer diastole. The intensity of metabolic processes in the myocardium and the conduction system of the heart decreases, and the organ experiences less stress.
The effect of accelerating spontaneous slow diastolic depolarization is achieved by the influence of the sympathetic nervous system and its transmitter adrenaline. Then the rate of SMDD increases, which ensures early activation of the sodium-calcium exchanger and the opening of slow-type calcium channels. The result is an acceleration of the rhythm frequency, increased heart rate, and increased energy consumption.
Description of the automation process
The automaticity of the human heart begins with the diastole phase, its manifestation is the movement of sodium into the cell. In this case, the membrane potential decreases significantly, the value tends to the minimum level of depolarization. The membrane charge decreases and slow depolarization of diastole begins. Channels for calcium and sodium open in the phase of rapid depolarization, and the ions begin to actively move toward the cell. As a result, the charge first decreases sharply and reaches zero, after which it is replaced by the opposite one. Sodium moves until equilibrium is reached among its ions (electrochemical).
The plateau phase begins. The calcium movement continues here. The heart tissue remains unexcited at this moment. When equilibrium is reached for the corresponding ions, the phase ends and repolarization occurs, which means the membrane charge returns to its original level.