- For what reasons does tachycardia occur in neurosis?
- Symptoms
- Diagnostics
- Treatment
- First aid for seizures
- Complications
- Prevention
Neurotic disorders often manifest themselves in the form of cardiac neurosis, when pain manifests itself, but no pathologies are detected in the heart. Tachycardia is a heart rhythm disorder when the heart cannot cope with the rush of blood and the release of cortisol. And this failure is often caused not by thinning of blood vessels, but by negative changes in the human psyche.
For what reasons does tachycardia occur in neurosis?
Neuroses are psychogenic diseases that require long-term treatment. We are talking about disorders of nervous activity, manifested in disorders such as fear, anxiety, depression, and mood swings. As a rule, it develops in patients who have little control over their behavior, but there are other reasons.
Tachycardia with neurosis occurs if:
- Vegetative dystonia.
- Hypertension.
- Hormonal changes in the body.
The impetus for cardialgia of nervous disorders can also be:
- bad ecology.
- bad habits.
- chronic infections.
Doctors say that the main cause of tachycardia against the background of neurosis is frequent stress, which undermines the human psyche for a long time.
What is the danger?
Severe tachycardia, which tends to recur periodically, is very dangerous for humans. The consequence may be the development of heart attacks and strokes. Of the 72% relapses, every fifth patient is susceptible to death. Therefore, people suffering from tachycardia are at risk of sudden death. Compared to people who do not have a rapid heart rate, the risk is doubled and sometimes 10-fold.
Tachycardia, especially persistent, can worsen the patient's condition.
If you do not deal with tachycardia during VSD, the consequences can be quite serious. An increased heart rate negatively affects a person’s quality of life, causing shortness of breath and dizziness. Lack of treatment will lead to hypertrophic changes in the myocardium. Over time, the heart wears out, its contractility decreases, and heart failure occurs.
Tachycardia accompanying vegetative-vascular dystonia is dangerous due to the development of:
- insufficient blood supply to the brain;
- cardiac asthma or pulmonary edema, which is associated with left ventricular failure;
- arrhythmic shock.
That's why it's so important to fix the problem in a timely manner.
Symptoms
Doctors often find it difficult to distinguish cardialgia of nervous disorders from angina pectoris. A characteristic sign of the first case is the behavior of people; with severe heart pain, patients try to move less so as not to aggravate it. And with cardioneurosis, the pain does not hamper movement, the person is able to walk, run and gesticulate briskly. Usually, such patients are brought to the doctor by increased heartbeat. In this case, the pulse rate is not high and not constant, but the number of beats can either decrease or increase.
Symptoms of cardiac tachycardia:
- Feeling of heat in the body.
- The skin becomes pale or very red.
- Hands and feet get cold.
- Body temperature rises.
Symptoms of tachycardia in neurosis:
- Heart pain can last from a few minutes to a couple of months. It radiates under the shoulder blade or into the neck area.
- The symptom disappears if the patient begins to move.
- Fear of death and anxiety arise.
- Panic attacks. The pulse becomes very rapid.
- Heavy loads.
- Dyspnea.
- Vegetovascular dystonia.
- Dizziness.
In hypertensive patients, cardiac neurosis can manifest itself in pressure surges; cardialgia often provokes spasm of the venous arteries.
Types of pathologies
From this article you will learn: what cardiac neurosis is, and why experts consider it a neuropsychic, and not a heart disease. Main causes and characteristic symptoms. Is it possible to be cured, and how to do it?
Cardiac neurosis is a functional disorder of the nervous regulation of the heart, not associated with a disorder of the structure or pathology of this organ. In 90% of cases, the disease occurs in people aged 14 to 50 years. Mostly women are affected (75% of patients).
Heart neuroses in terms of symptoms and treatment are not considered dangerous diseases. But they have to be diagnosed by excluding other cardiac pathologies, since there are no reliable methods for diagnosing this particular disease. Symptoms of cardiac neurosis slightly affect the general condition of patients. The main manifestation is pain in the heart area, similar to periodic attacks.
Recovery is difficult, but possible. This requires medications and special psychotherapy sessions. But the most important thing in treatment is the desire of the patient and compliance with all recommendations of specialists. Diagnosis and treatment are carried out by cardiologists, neurologists, psychoneurologists and psychotherapists.
What kind of disease is this
The nervous system regulates the functioning of all body systems (respiratory, cardiovascular, excretory, digestive, etc.). Neurosis is a breakdown in the nervous system - a neuropsychic disorder that leads to disruption of the normal functioning of internal organs.
Click on photo to enlarge
With cardiac neurosis (also called cardioneurosis), the nervous regulation of cardiac activity is disrupted. This means that the disease does not disrupt the structure of the myocardium, valves or blood vessels. No pathological changes occur in the organ. The heart copes with its function of pumping blood.
But its contractile activity is accompanied by periodic pain in the chest, intermittent heartbeat interruptions, weakness and dizziness. All these disorders (attacks) are associated with psycho-emotional instability and experiences (stress, panic, fear, depression, etc.).
Heart neurosis is a distorted perception by the nervous system of impulses that emanate from this organ. The result is the occurrence of unpleasant pain or the formation of incorrect commands in the brain, which only slightly disrupt the normal functioning of the heart. Therefore, cardioneurosis can resemble any cardiac pathology (ischemic disease, arrhythmia, myocarditis).
The heart contracts on its own – automatically. But even this autonomy is only partial. The nervous system, through the autonomic centers and conscious signals from the cerebral cortex, perceives and regulates cardiac activity. Violation of the regulatory relationship between the nervous system and the heart leads to the fact that this organ either begins to work incorrectly, or a person has a feeling that something is wrong with it (pain, interruptions, etc.).
We suggest you read: Hypertension and sex is it dangerous or not?
The following reasons can trigger the pathological process:
- Severe stressful situations and neuropsychic shocks.
- Congenital instability of the psyche, individual characteristics of a person’s psychotype (irritability, hot temper, tearfulness, despondency, anxiety, depression, tendency to exaggerate) and psycho-emotional lability.
- Diseases of the endocrine system, accompanied by hormonal disorders, as well as periods of hormonal changes in the body (puberty and menopause).
- Overwork of the nervous system (study, mental work, etc.).
- Improper lifestyle – insufficient or excessive physical activity, alcohol abuse and smoking.
- Chronic, long-term diseases that lead to weakening of the body in general and the nervous system in particular.
As a result of exposure to provoking factors, a vicious circle of disease initiation and progression occurs, destroying the correct relationship between the heart and the regulatory centers of the brain.
Typical symptoms
The course of cardiac neurosis can be different - from short-term mild periodic attacks (once every few months or weeks) to constant (daily) occurrence and intensification of symptoms. In any case, the manifestations of the disease are associated with tension in the nervous system - stress, insomnia, anxiety, mental work, etc.
Classic symptoms of cardiac neurosis:
- Pain in the heart area, behind the sternum, in the left half of the chest. They can be represented by mild discomfort, heaviness, squeezing, burning, stabbing and other pains.
- A feeling of trembling or freezing in the chest (slow heart rate). Patients focus on their sensations that the heart seems to be bursting out of the chest or stopping.
- General weakness and impotence.
- Changes in blood pressure.
- Trembling in the body, numbness in the arms and legs.
- Headache and dizziness.
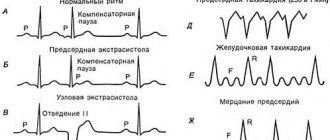
- Heart rhythm disturbances - slight acceleration (tachycardia about 90–100 beats/min), slowdown (about 60 beats/min), extrasystoles (unscheduled contractions and interruptions).
- Dyspnea.
- Feeling of fear, anxiety.
- Anxiety and insomnia.
- Pale or reddened facial skin.
Heart neurosis is a kind of transitional state between normality and pathology. By itself, it rarely disrupts the general condition of patients, but can provoke the occurrence of more severe diseases (atrial fibrillation, angina pectoris and even heart attack, neurotic personality disorder).
Cardiac neurosis can be diagnosed only by excluding other cardiac pathologies. The thing is that with cardioneurosis there are no organic changes that could be detected by:
- ECG;
- Ultrasound of the heart;
- Holter monitoring;
- general and biochemical blood tests;
- chest x-ray.
But this minimum amount of examination must be performed for every person who has symptoms characteristic of cardioneurosis (primarily heart pain). The diagnosis is made if three factors are present:
- During the diagnosis, no pathological changes were revealed at all or they were represented by minimal rhythm disturbances in the form of tachycardia (acceleration), bradycardia (slowdown) or single extrasystoles (interruptions).
- There are no other reasons for the appearance of pain in the heart area (intercostal neuralgia, diseases of the lungs, esophagus and other organs).
- The appearance of symptoms is associated with nervous overstrain.
For help, contact a cardiologist, neurologist, psychoneurologist or psychotherapist.
Features of treatment
The treatment program for cardiac neurosis involves:
- Normalization of lifestyle: exclusion of neuropsychic and mental stress, bad habits and other causative factors of the disease.
- Regular, balanced, vitamin-enriched meals, excluding spicy and any irritating foods, strong coffee, and alcohol.
- Sufficient physical activity - physical therapy, sports games, walks in the fresh air. Both overwork and physical inactivity are excluded.
- Physiotherapeutic treatment: massage, water procedures (best in a sanatorium).
- Sessions of psychotherapy, acupuncture and hypnosis are the most effective methods with which you can not only reduce symptoms, but also cure the disease forever.
- Drug treatment:
- sedatives and sedatives (Valerian, Motherwort, Gidazepam, Adaptol, Phenazepam, Fitosed, Glycised, Eglonil);
- antianginal and diversion drugs (Validol, Corvalol, Corvalment);
- beta blockers (Anaprilin, Metoprolol, Bisoprolol) under the control of blood pressure and pulse;
- multivitamin complexes (Cardiovit, Magne B6, Neurobeks).
Heart neurosis can be cured. To do this, it is necessary to take the utmost responsibility to comply with absolutely all treatment recommendations of specialists. Otherwise, the disease will become progressive, and treatment will bring only temporary relief.
Forecast
It is difficult to predict how cardiac neurosis will end, even with proper treatment. The forecast depends on several factors:
- person's age;
- characteristics of the nervous system and mental status of the patient;
- duration and causes of the disease.
Full recovery occurs in 80–90% of people with minimal psychoneurological disorders aged 15 to 40 years with mild, rare attacks of cardioneurosis.
People over 35 years of age with an unstable psyche or psychotrauma, frequent and severe attacks of the disease, fully recover in 20–30% of cases. About 95% of those who do not recover with treatment report a decrease or temporary disappearance of symptoms.
In only 5% of people, treatment does not bring any effect or neurosis develops into more severe disorders.
Sinus tachycardia with VSD is the most common form of deviation characteristic of patients with VSD (especially in adolescence). Causes palpitations at night. The pulse can reach up to 90 beats per minute.
Paroxysmal tachycardia with VSD (paroxysmal) can begin in any part of the heart, therefore it can be supraventricular (atrial, atrioventricular) and ventricular; in patients with VSD, this type of tachycardia is much less common.
Paroxysmal tachycardia is caused mainly by more serious pathologies in the body than vegetative-vascular dystonia; VSD itself is characterized by sinus tachycardia.
Sinus tachycardia with VSD
In addition to the patient’s descriptions of his condition, the type of tachycardia during VSD can be determined using an electrocardiogram. The ECG result will show an almost unchanged pattern of waves, but the intervals (RR) between heart rhythms will be noticeably shorter, and sometimes the end of the previous and the beginning of a new cycle will even overlap each other. The electrical systole line will also be shorter with tachycardia at the time of VSD. The ST segment falls below the isoline.
Diagnostics
In order to accurately establish the diagnosis and ensure the normal functioning of the heart, procedures are prescribed that make it possible to determine the nature of tachycardia, its causes, type, and formulate a possible prognosis.
Recommended Research:
- Electrocardiogram. Electrical impulses from the heart are measured.
- Daily monitoring. Recording heart function for one day.
- Event recorder . A device that records signals when the patient experiences characteristic symptoms. Helps examine rhythm disturbances at selected time intervals.
- Electrophysiological studies . A special catheter is inserted into the vein and advanced towards the heart, controlling the process. Having reached the goal, the device begins to stimulate contractions, and heart rate indicators are recorded.
- Table tilt test . Helps determine how the nervous and cardiovascular systems respond to changes in posture. The patient is injected with a drug that provokes arrhythmia, and then placed on a table that rhythmically changes position.
Treatment
The main method of treating cardiac neurosis is psychotherapy. Sessions help to find out the cause of the nervous condition, in most cases it is dissatisfaction with work, problems in personal life. An excited state undermines the immune system and causes fatigue. Sessions are more effective when combined with medications selected by the doctor. They start with light sedatives on a homeopathic basis.
Neurotic attacks can be treated with stronger medications:
- Antidepressants: azaphene, amitriptyline, nialamide.
- Beta-blockers : Trazicor, anaprilin. Prescribed when tachycardia and hypertension reach a borderline state.
- Sleeping pills to improve sleep . Selected individually. It is recommended to take the medicine for no more than three weeks to avoid addiction.
Physiotherapeutic procedures
Complex prescriptions give a good effect:
- Electrosleep.
- Electrophoresis.
- Pearl and pine baths.
- Sharko's shower.
During treatment it is necessary to exclude alcohol, smoking and coffee.
Folk remedies
Traditional methods are widely used to treat tachycardia in neurosis. The most popular recipes are tinctures of valerian and peony. Collecting hop cones or calamus rhizomes is effective. Disorders accompanied by dizziness and attacks of suffocation can be relieved by a collection of cumin, motherwort, chamomile, cudweed and hawthorn.
Hawthorn decoction
Ingredients:
- Dried hawthorn flowers – 1 tbsp. spoon.
- Water – 1 glass.
Preparation: pour boiling water over the raw materials, leave for 20 minutes. Drink three times a day, before meals.
Melissa tincture
Ingredients:
- Melissa – 100 g.
- Alcohol – 200 g.
Preparation: pour alcohol over the plant and leave for 10 days. Strain. Drink 1 teaspoon 4 times a day, can be diluted in 50 ml of water.
Valerian decoction with calendula
Ingredients:
- Calendula flowers – 1 tbsp. spoon.
- Valerian roots – – 1 tbsp. spoon.
- Water – 400 ml.
Preparation: pour the raw material into a thermos and pour boiling water over it. Leave for 3 hours. Drink 100 g three times a day. The course lasts 20 days, then you need to take a break for a week.
Diet
Even if the cause of heart pain is neuralgia, the manifestation itself indicates that the heart needs help. Well-established nutrition can be such support.
Recommended:
- Nuts. They have a positive effect on the nervous system thanks to magnesium and potassium. They nourish the muscle, making the fibers more resistant to the effects of nerve impulses.
- Vegetables and fruits. Vitamins and minerals help maintain the elasticity of blood vessels.
Prohibited:
- Spices, marinades, preservation.
- Fatty meat and fish.
- Sour cream and cream with a high percentage of fat.
How to get rid of the disease 7 ways
Everyone who is familiar with the diagnosis of vegetative-vascular dystonia knows the concept of tachycardia. Why tachycardia occurs during VSD should be examined in more detail.
Need to know! The very concept of “tachycardia,” translated from medical language, means “rapid heartbeat.” Normally, in a middle-aged adult at rest, the number of heart beats per minute should correspond to an average of 72 beats. These parameters differ slightly between women and men (from 65 to 90 and from 60 to 80, respectively).
In children under 2 years of age and elderly people, heart rate is increased to 100-140 beats per minute. This means that if a thirty-five-year-old woman sitting quietly in front of the TV has a pulse exceeding 90 beats per minute, we can detect an attack of tachycardia during VSD.
It is completely impossible to recover from tachycardia with VSD. In order for the tachycardia caused by VSD to disappear, the disease of vascular dystonia itself must be cured. There is a separate article on how to treat VSD, so it is worth considering ways to eliminate pulse instability in the presence of VSD.
You can stop an attack of tachycardia during VSD (with a heart rate of more than 160 beats per minute) by observing the following measures:
- Take a reclining position to ensure a state of rest;
- Release your neck and chest if you have tight underwear (open your shirt collar, loosen your tie, unfasten your bra);
- Rinse your face with cold water, place a damp, cool cloth or towel on your forehead;
- Try to cough or induce vomiting (if an attack of tachycardia during VSD is accompanied by nausea);
- Provide fresh air access to the room and use classical breathing techniques. For five minutes, inhale deeply and exhale quickly;
- Take from 15 to 30 drops of Corvalol, Valoserdin or Valerian tincture;
- If an attack of tachycardia during VSD caused a violent emotional outburst, accompanied by an increased release of adrenaline into the blood, beta-blockers will help calm the heart. The simplest and most accessible among them is “Anaprilin” at the time of tachycardia during VSD. Taking one tablet under the tongue blocks the release of adrenaline, slightly lowers blood pressure, and reduces heart rate. The effect of “anaprilin” is symptomatic and short-term. Taking it as a therapeutic agent at the time of tachycardia with VSD does not make sense. Another important note: if two sublingual Anaprilin tablets did not have the desired effect, ten will not help, and an overdose will lead to serious complications.
If, 10 minutes after the onset of an attack of tachycardia during VSD, at the time of applying the above measures, the heart rate does not fall below 150 beats per minute, you should urgently call an ambulance. Since the development of complications such as myocardial infarction, stroke, and clinical death is possible.
Tachycardia with VSD manifests itself constantly. The pulse rate at rest may be 30 beats per minute higher than normal. Sometimes a person does not even feel this state, because he is used to it. Such tachycardia with VSD leads to serious problems in the functioning of the heart and to dangerous disorders.
To avoid the development of negative consequences of tachycardia during VSD, you should undergo a thorough examination of the body. The cause of chronic tachycardia may not be VSD at all, but more serious health problems.
First aid for seizures
During treatment or remission, heart attacks may occur. Although they do not pose a threat to life, they cannot be ignored. First aid recommendations:
- Lay the patient down and provide air access.
- Measure blood pressure and pulse.
- Distract with conversation on neutral or interesting topics.
- Offer a mild sedative: valerian, motherwort, Corvalol.
If the pulse rate increases, dizziness occurs, you need to call an ambulance.
Complications
Any disease can provoke complications, and tachycardia, which manifests itself against the background of cardiac neurosis, is no exception. Ignoring the problem can result in a general weakening of the body, severe nervous breakdowns, and migraines.
Complications:
- Stroke or heart attack.
- Inability of the heart to pump the required amount of blood.
- Fainting.
Prevention
As you know, it is easier to prevent a disease than to treat it, this is especially true for neuralgia. If you follow a daily routine, devote time to physical activity, walks and control your weight, it is quite possible to avoid unpleasant consequences.
Additional recommendations:
- Control blood pressure and cholesterol levels.
- To refuse from bad habits.
- Limit or eliminate coffee and strong tea.
- Use a contrast shower.
It is very important to remember that cardiac neurosis is associated with the psyche; doctors note that the success of treatment largely depends on the positive mood of the patient, his ability to tune in to the optimal result. Otherwise, the drugs will not help much. The main thing is to learn to manage your emotions and not fall into despair when at first there is no expected result.
General information
It is still not completely known what leads to cardiac neurosis. The following reasons are identified:
- asthenic appearance of the nervous system;
- VSD;
- increased blood pressure;
- problems with hormones;
- chronic heart and kidney diseases;
- psychological stress.
Emotional unrest provokes a rapid heartbeat.
The manifestations of the disease are different for everyone. Symptoms depend on the person's emotional state and level of fatigue. The person feels a headache and pain in the heart (as if the chest is being squeezed), nausea, lack of oxygen and suffocation. The patient feels weak and his legs cannot support him. It's hard to talk and think. A person has a rapid heartbeat. He feels fear.
Tags: neurosis, dangerous, tachycardia
About the author: admin4ik
« Previous entry