For common cardiovascular disease such as angina, treatment is aimed at relieving symptoms, slowing the progression of the disease and reducing the likelihood of complications, especially myocardial infarction and premature death.
Therapeutic tactics depend on the effectiveness of the initial drug therapy. Medicines of different pharmacological groups are used to improve blood supply to the myocardium. After additional diagnostics, the patient is offered surgical intervention.
Reasons for the development of pathology
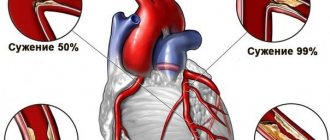
Often the symptoms of angina pectoris develop against the background of atherosclerosis of the coronary arteries. The lumen of the blood vessels narrows by 50-70%, which leads to the delivery of less oxygen to the heart muscle with constant consumption. Common causes of angina remain arterial hypertension, coronary spasm, aortic stenosis, and congenital anomalies of the coronary arteries. Pathology can become a complication in acute coronary thrombosis.
Risk factors include:
- systematic smoking;
- alcohol consumption;
- age over 55 years;
- obesity 3-4 degrees;
- early menopause;
- diabetes.
The risk group includes patients with pathologies of the cardiovascular system in a family history. Severe forms of anemia and hypoxia can complicate the course of the disease.
What it is?
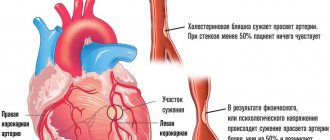
When the myocardial need for oxygen becomes greater than the ability to obtain it, cardiac ischemia occurs. It is a consequence of pathological narrowing of the coronary arteries. Most often this is caused by atherosclerosis. With this disease, cholesterol is deposited in the vessels, impeding the passage of blood.
The pathogenesis of ischemia is associated with diseases that provoke vasospasm:
- allergic;
- infectious;
- gastrointestinal.
Angina pectoris is the most common form of angina. The heart requires more oxygen, the greater the load on it.
Forms of pathology
Cardiologists distinguish three types of the disease: primary, stable and progressive. The first and second forms can transform into the third over time. A more extensive classification of angina pectoris is based on the patient's tolerance to physical activity. The intensity of the maximum permissible human activity allows us to distinguish four functional classes.
| Functional class (FC) | Description |
| I | Daily loads are tolerated without consequences. The attack develops against the background of unusual activity - running, climbing a large number of flights of stairs, lifting heavy objects. |
| II | Minor physical activity provokes the development of symptoms. Causes may include leisurely walking, climbing stairs to a height of more than one floor, emotional stress |
| III | The patient cannot tolerate minimal physical activity. An attack occurs when walking a distance of 50-100 meters. Climbing stairs is difficult |
| IV | Activity is significantly limited. Angina pectoris occurs when performing basic actions or while at rest |
Life after hospital
Stable angina does not require hospital treatment. Selection of therapy
performed on an outpatient basis. If attacks become more frequent, hospitalization is indicated. After discharge, the patient must visit the doctor regularly and take all prescribed medications. In addition, it is necessary to reduce the risk of myocardial infarction:
- normalize weight;
- monitor blood pressure and sugar levels;
- do not smoke or drink alcohol or large doses of caffeine;
- give up excess load that causes attacks;
- maintain daily physical activity that does not worsen the condition.
Symptoms of angina pectoris
Patients experience pain of varying intensity: from mild discomfort behind the sternum to severe pain in the heart muscle. The duration of a typical attack is 3-5 minutes, there are pronounced onset and end phases. The intensity of symptoms decreases when the provoking factor is eliminated. The pain of angina pectoris is radiating and can affect the jaw, shoulder blade, arm or neck.
During an attack, the patient feels weak, shortness of breath appears, and tachycardia and arrhythmia develop. Representatives of the older age group may experience a sharp increase or decrease in blood pressure. In rare cases, an atypical attack develops, accompanied by abdominal pain, nausea and vomiting.
The frequency of manifestations of angina pectoris varies. Patients may experience up to five attacks per day or experience a sharp increase in symptoms every few months. If left untreated, angina at rest may develop against the background of exertional angina.
Angina pectoris as a form of coronary heart disease (CHD)
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
There is a group of heart diseases that are based on impaired blood flow to the heart muscle. They are united under the general name of coronary heart disease (CHD). Among them, angina pectoris is a special form, since it actually signals patients about danger. It is not a fatal disease, but acts as its predecessor, which allows a person to pay attention to heart problems and take the necessary actions about it.
Angina is...
Any problems with the heart muscle always manifest as pain in the chest. Angina pectoris is one of the types of heart pain. It is so specific that to make a diagnosis, only a certain set of its characteristics is sufficient, even without the use of additional research methods. The basis of coronary heart disease and angina pectoris is a decrease in the volume of blood flowing to the myocardium due to narrowing of the coronary (heart) arteries. The specific type of disease depends on how disrupted this process is.
In general, the criteria for angina are:
- Painful feeling of pressure in the chest area and left side of the chest;
- Paroxysmal course;
- Occurs suddenly at rest or during physical activity;
- The duration of the attack should not exceed 20-30 minutes, otherwise it is already a heart attack;
- It can be easily relieved by taking nitroglycerin or other nitrates.
It is imperative to pay attention to all these criteria. This is very important in making a differential diagnosis between angina pectoris and heart attack. Their presence indicates the reversibility of circulatory disorders in the heart if the necessary treatment is prescribed.
Reasons for the development of the disease
The core of coronary artery disease and angina pectoris is the narrowing of the lumen of the coronary vessels. This can lead to:
- Atherosclerosis of the heart arteries;
- Rupture of an atherosclerotic plaque with the appearance of a blood clot at this site;
- Spasm (contraction) of the artery with a decrease in its diameter;
- Stressful situations and nervous overstrain;
- Excessive physical activity;
- Active smoking;
- Alcohol abuse;
- Uncontrolled hypertension;
- Myocardial hypertrophy (thickening of the heart muscle mass);
- Age-related decrease in the elasticity of vascular walls.
Types of coronary heart disease
The division of pathology into subtypes is very important for determining treatment tactics, since they take into account the reversibility and speed of development of the disease.
| Type of pathological changes in the heart muscle | ||
| The myocardium is not destroyed (ischemia) | The myocardium is destroyed (necrosis) | |
| Angina pectoris (occurs during physical activity) | Stable angina |
|
| Unstable angina | ||
| Angina at rest (occurs at rest) | Prinzmetal's angina | |
| Vasospastic angina | ||
Angina pectoris
It is the occurrence of substernal pressing pain during physical activity. The degree of severity and appropriate treatment depend on the time of onset of angina depending on the intensity of the load. Typically, patients with this form of the disease note the appearance of discomfort and pain in the chest, or in the left half of the chest (heart area) when climbing stairs, walking normally, or doing housework. Pain during angina pectoris radiates (radiates) to the left shoulder, shoulder blade, neck and forces you to stop performing the actions that provoked it. After some time, the pain goes away on its own or is relieved by taking nitrates.
If a load of equal intensity over a long period of time provokes attacks, then this condition is characterized as stable angina pectoris. It suggests that ischemic processes in the heart are at a constant level and do not progress. On the other hand, this makes it possible to evaluate the effectiveness of treatment measures. The presence of stable angina pectoris in a patient is an indicator of a relatively favorable course of coronary heart disease, which rarely ends in a heart attack. This is due to the fact that the longer it exists, the more the heart muscle adapts to the conditions of impaired blood supply. If the intensity of pain or the factors causing angina pain change, such angina is called unstable.
Angina at rest
The disease is characterized by the occurrence of attacks of chest pain in a state of complete rest. This is possible in two situations. In the first case, an instant reflex spasm of the coronary arteries occurs, which causes myocardial ischemia. The second situation is typical for a specific type - Prinzmetal's angina. It also occurs instantly, but its cause is the blocking of the lumen of the coronary vessels by a torn atherosclerotic plaque, which moves freely and can change its position at any time. Usually this type of angina is very insidious, as it often ends in a heart attack.
Unstable angina
This term characterizes either exertional angina, which becomes progressive, or variable resting angina. Isolating this type of disease is advisable from the point of view of its danger. After all, the appearance of pain under loads that did not cause it before or the inability to stop an attack with standard doses of nitrates indicates that the pathological process is getting out of control. The same lack of control is characteristic of new-onset angina. The presence of this form of the disease should encourage patients and specialists to actively search for a solution to this problem.
Treatment of the disease
The entire scope of treatment has clear goals that are achieved by prescribing medications or surgical treatment.
| Treatment goal and mechanism | How treatment is achieved |
| Dilatation of narrowed coronary arteries |
|
| Blood thinning |
|
| Metabolic therapy |
|
| Fight against atherosclerosis | Drugs that affect lipid metabolism - statins: atorvastatin, Atoris, lovastatin; |
| Restoration of the vascular lumen | Reconstructive surgical treatment:
|
It is important to remember that only timely detection of angina and its qualified treatment can help prevent the progression of the disease and its transformation into a heart attack.
Know how to listen to what your heart tells you, and it will never let you down!!!
Why do you feed pharmacies if hypertension is afraid of the usual like fire...
Tabakov has revealed a unique remedy against hypertension! To reduce blood pressure while preserving blood vessels, add to…
Diagnosis of pathology
The patient is examined by a cardiologist. The most effective way to diagnose exertional angina is an ECG obtained during an attack. Ischemia is induced by stress testing. Conducting them in a clinical setting eliminates the possibility of complications developing in the patient. Holter monitoring can detect myocardial ischemia and heart rhythm disturbances.
EchoCG is aimed at assessing myocardial contractility. The use of this technique allows for differential diagnosis and exclusion of other pathologies of the cardiovascular system from the patient’s medical history. Laboratory tests - general and biochemical blood tests - provide an opportunity to detect signs of atherosclerotic damage to the patient’s blood vessels.
Does diet matter?
The chances that exertional angina will not develop into a progressive form are largely related to proper nutrition. A diet for angina pectoris should help normalize blood circulation, inhibit the development of atherosclerosis, and maintain weight within normal limits.
- Animal fats and easily digestible carbohydrates are limited.
- The content of fresh vegetables, fruits, fish, seafood, lean meats, poultry, and dairy products increases. All these products contain elements that are beneficial for the heart muscle: potassium, magnesium, iodine, lipotropics, fiber.
- Salt, canned food, smoked meats, stimulating foods and drinks (coffee, chocolate, alcohol) are sharply limited or completely excluded.
It is not recommended to fry foods.
Treatment
Therapy begins with the elimination of all provoking factors that can affect the condition of a person suffering from the pathology. The attacks are controlled by taking nitroglycerin. After making a diagnosis, the cardiologist can prescribe the patient long-acting nitrates, antiplatelet agents, calcium channel blockers and beta-blockers.
The persistence of symptoms during conservative treatment becomes a reason to refer a child or adult for surgery. During the intervention, surgeons perform stenting of the coronary arteries and perform endovascular angioplasty. Clinical recommendations provide for the possibility of coronary artery bypass grafting against the background of exertional angina. The effectiveness of surgical treatment is 90-95%.
Exercise tests
An ECG recorded at rest, outside of an attack of pain, in a patient without a history of MI, may appear unchanged. Much more complete diagnostic information can be obtained from an ECG while the patient is performing dosed physical work in the form of bicycle ergometry or treadmill test. Considering the great importance of the information that can be obtained when performing an exercise test (PE), it is necessary to strive to perform it in patients with stable angina in all cases in the absence of contraindications.
During the exercise test, the patient performs an increasing load on a treadmill or bicycle ergometer, while heart rate (HR) and ECG values are constantly recorded, and blood pressure is recorded at regular intervals (1-3 minutes).
The main indications for performing stress tests:
- differential diagnosis of ischemic heart disease and its individual forms;
- determination of individual tolerance to FN in patients with an established diagnosis of coronary artery disease and clarification of the FC of angina pectoris;
- assessment of the effectiveness of therapeutic, including surgical and rehabilitation measures;
- examination of the patient’s ability to work;
- assessment of disease prognosis;
- assessment of the effectiveness of antianginal drugs.
Absolute contraindications to the FN test are the acute stage of myocardial infarction (2-7 days from the onset of the disease), unstable angina, cerebrovascular accident, acute thrombophlebitis, pulmonary embolism, heart failure class III-IV according to the New York Heart Association classification (NYHA), severe pulmonary insufficiency, fever. It is not advisable to perform a diagnostic test for tachyarrhythmias, complete block of the left bundle branch, or a high degree of sinoatrial and atrioventricular block.
An exercise test is performed before the development of an attack of angina, the appearance of signs of myocardial ischemia on the electrocardiogram, the achievement of the target heart rate, the development of severe fatigue that makes it impossible to continue the load, or if the patient refuses to perform the test. Therefore, the exercise test should be stopped when:
- development of a typical attack of angina pectoris;
- the appearance of life-threatening heart rhythm disturbances, such as frequent or polytopic or volley ventricular extrasystole, paroxysmal tachycardia or paroxysmal atrial fibrillation;
- the occurrence of severe shortness of breath (respiratory rate more than 30 per minute) or an attack of suffocation;
- development of conduction disorders - bundle branch block, atrioventricular block of 2 degrees or more;
- ischemic displacement of the ST segment upward > 1 mm in any of the leads except V1-2, where elevation is considered to be 2 mm or more, or downward from the isoelectric line > 1 mm and lasting 80 ms from the J point, slow obliquely ascending decrease in the ST segment at the J point +80 ms > 2 mm (rapid obliquely ascending ST decrease is not considered ischemic);
- rise in systolic blood pressure>220 mm Hg. Art., diastolic blood pressure>110 mm Hg. Art., a decrease in systolic blood pressure by 20 mm Hg. Art.;
- the appearance of neurological symptoms - dizziness, loss of coordination, severe headache;
- development of sudden fatigue of the patient, his refusal to further perform the test;
- reaching 75% of the maximum age-related heart rate.
If the above criteria are met, the sensitivity of the exercise test for identifying patients with anatomically significant atherosclerotic lesions of the coronary arteries, that is, their stenosis of more than 50%, is 65-80%, and the specificity is 65-75%. Patients with positive test results are more likely to have severe disease in multiple coronary arteries. An exercise test is considered positive for the diagnosis of coronary artery disease if it causes pain or tightness in the chest that is typical for the patient and changes in the electrocardiogram characteristic of ischemia. Pain does not always accompany a decrease in the ST segment; the test is considered positive if the decrease appears without pain, or if a typical attack of angina develops without a decrease in the ST segment.
However, load testing has limitations and disadvantages. An exercise test is not informative in the presence of an initial block of the left bundle branch, a pacemaker rhythm, or Wolff-Parkinson-White syndrome. The sensitivity and specificity of the exercise test are lower in women than in men, and its information value may be reduced by certain medications. Beta blockers or some calcium channel blockers (which lower heart rate) do not allow the target heart rate to be achieved during the test. In these cases, you should keep in mind why the stress test is being performed. If it is being done to determine whether a patient has CAD, then these medications should be stopped 24-48 hours before the test. In patients with diagnosed coronary artery disease, if it is necessary to evaluate the effectiveness of the selected treatment regimen, the test is carried out while taking medications.
Taking into account the listed limitations of ECG during physical activity, the new European recommendations for the diagnosis of stable angina pectoris strengthen the position of stress tests in combination with echocardiographic visualization of the heart and blood vessels, as well as with myocardial perfusion scintigraphy with thallium or technetium radiopharmaceuticals. Drug tests in combination with the above-mentioned cardiovascular imaging methods are becoming increasingly popular.
Indications for stress imaging studies are:
- complete left bundle branch block, pacemaker rhythm, WPW syndrome and other ECG changes associated with conduction disturbances;
- decrease in the ST segment > 1 mm on the resting ECG, including those caused by left ventricular hypertrophy, medications (cardiac glycosides);
- inability of patients to perform sufficiently intense physical exercise;
- angina attacks after coronary revascularization;
- the need to determine myocardial viability.
During echocardiography control, disturbances in myocardial contractility in two or more segments are taken into account; during myocardial scintigraphy with thallium-201, local perfusion defects and other signs of impaired myocardial blood supply are recorded when compared with its initial state.
It should be taken into account that stress ECG tests (bicycle ergometry, treadmill test) are the cheapest of the functional tests, however, the accuracy of the stress test with ECG registration is inferior to the accuracy of stress echocardiography, as well as radionuclide research methods.
Questions and answers
Is there a set of preventive measures to prevent the development of angina pectoris?
Recommendations from cardiologists are addressed to people with a family history of coronary heart disease. Doctors insist that patients stop smoking and drinking alcohol. Fatty foods should be excluded from the diet. The dosage of medications prescribed for pathologies of the cardiovascular system should be observed.
Is surgery necessary for exertional angina?
The need for surgical intervention is determined by the clinical picture of the disease. For mild cases, patients are prescribed medication. The risk of complications or a severe form of pathology can become a decisive factor when a doctor makes a decision on surgical treatment.
Attention! You can cure this disease for free and receive medical care at JSC "Medicine" (clinic of Academician Roitberg) under the State Guarantees program of Compulsory Medical Insurance (Compulsory Medical Insurance) and High-Tech Medical Care. To find out more details, please call or visit the VMP page for compulsory medical insurance
Providing first aid for an angina attack
A painful symptom can occur suddenly during exercise or at rest, on the street or at home. Therefore, providing first aid for angina pectoris has its own nuances in each case. When walking, climbing stairs, the patient needs to stop physical activity, stop or sit down. In a home environment, you need to unfasten constrictive clothing, open a window to allow fresh air in, a calm atmosphere will help the attack pass faster.
If the patient has already experienced angina attacks, then you need to use the medicine prescribed by the doctor. As a rule, this is nitroglycerin in sublingual (under the tongue) tablets or in aerosol form. The first dose should be minimal; if there is no effect, take it again after 5-6 minutes. Large doses are contraindicated because they can cause the body to become addicted to the drug.
Statistical data
Pathologies of the cardiovascular system remain the most common cause of death among Muscovites – 55% of cases in 2019. This figure is three times higher than the European average. The total number of Russian residents suffering from heart disease exceeds 16 million people. A quarter of them have congenital pathologies of the cardiovascular system. Prevention of attacks of myocardial ischemia remains one of the key tasks of cardiologists when monitoring patients at risk.
Echocardiography
Echocardiography at rest is today a routine method of instrumental examination of patients with suspected stable angina in many Ukrainian clinics. It is important for the differential diagnosis of non-coronary chest pain arising from aortic valve stenosis and hypertrophic cardiomyopathy. This method is invaluable in patients with auscultatory noises, which are sometimes beyond the power of even experienced specialists to interpret correctly. Ultrasound examination of the heart makes it possible to simultaneously analyze in real time both the morphology and function of cardiovascular structures, especially the left ventricle; the parameters of its operation are important in terms of risk stratification and the choice of tactics for managing a patient with coronary artery disease.
Coronary arteriography (CAG)
CAG is the reference method for diagnosing coronary artery disease in accordance with European recommendations (2006) and is indicated for all patients with severe stable angina of class III-IV. In this category of patients, the likelihood of having stenosing atherosclerosis of the coronary arteries is highest, while drug therapy is often inadequate and does not provide relief from the symptoms of the disease. In accordance with the new European document on stable angina, CAG is indicated for all patients who have suffered cardiac arrest, revascularization interventions on the coronary arteries (if clinical signs of moderate or severe angina were noted in the early period after revascularization), as well as all patients with concomitant severe ventricular arrhythmias.
Despite the intensive development of non-invasive research methods, coronary angiography allows the most objective choice of treatment method: medication or myocardial revascularization. The degree of narrowing of the vessel is determined by a decrease in the diameter of its lumen compared to the proper one and is expressed as a percentage. Until now, experts have used visual assessment, which is characterized by: normal coronary artery, altered arterial contour without determining the degree of stenosis, narrowing ≤50%, narrowing 51-75%, 76-95%, 95-99% (subtotal), 100% (occlusion). A narrowing of the artery >50% is considered significant; a narrowing of the lumen of the vessel ≤50% is considered hemodynamically insignificant.
In addition to the location of the lesion and its extent, coronary angiography may reveal other characteristics of arterial lesions, such as thrombus, tear (dissection), or spasm. When deciding whether to prescribe coronary angiography, it is necessary to assess not only the feasibility, but also the risk of this intervention.
There are currently no absolute contraindications for prescribing CAG; relative contraindications for CAG are: chronic renal failure, allergic reactions to contrast media and iodine intolerance, severe coagulopathy, severe anemia, uncontrolled arterial hypertension, high likelihood of bleeding and restrictions on the use of anticoagulants. , intoxication with glycosides, hypokalemia, the occurrence of irreversible heart rhythm disturbances, fever and acute infections, endocarditis, inability to apply revascularization, decompensated heart failure and pulmonary edema.
The main tasks of the CAG:
- clarification of the diagnosis in case of insufficient information content of the results of non-invasive examination methods;
- determining the possibility of myocardial revascularization and the nature of the intervention.
Indications for prescribing coronary angiography to a patient with stable angina:
- severe angina pectoris III-IV FC, persisting with optimal antianginal therapy;
- signs of severe myocardial ischemia according to the results of non-invasive research methods;
- the patient has a history of dangerous ventricular arrhythmias;
- progression of the disease according to the dynamics of non-invasive tests.
Thus, the more pronounced the clinical symptoms of angina pectoris, the worse the prognosis of the disease based on clinical signs, the more grounds there are for prescribing CAG to the patient and deciding on myocardial revascularization.
Additional opportunities for non-invasive and highly informative diagnosis of stable angina are provided by the methods of computed tomography and magnetic resonance arteriography, however, they are considered in the European recommendations as additional and have not yet become widespread in our country for objective reasons.