Whatever the health problems, they always affect the quality of life. The group of the most common diseases that can cause death is cardiovascular diseases. People do not always pay attention to some symptoms, but their timely treatment can save health and life. For example, angina pectoris 2 FC requires a high-quality examination and adequate treatment. What it is, how this health problem is diagnosed and treated will be discussed in this article.
Angina: symptoms
Heart problems, unfortunately, are a very common cause of deterioration in health.
According to the World Health Organization, of all deaths, more than 30% occur due to diseases of the cardiovascular system of the human body. Moreover, half of such cases occur as a result of coronary heart disease and strokes.
Such diseases have several pronounced symptoms, which allow them to be diagnosed quite clearly and first aid to be used to relieve pain. One of these symptom complexes is angina pectoris. The ICD (International Classification of Diseases) classifies this pathology as a block of coronary heart disease in the group of cardiovascular diseases.
IHD: causes of occurrence
Coronary pain occurs as a result of atherosclerotic lesions due to:
- Genetic predisposition;
- Aging of the body;
- Diabetes mellitus;
- Menopausal (menopausal) period;
- High blood pressure;
- Lipid metabolism disorders (obesity);
- Smoking.
The development of the disease at a young age occurs with a hereditary predisposition. In other cases, sclerosis occurs after 40. During this period, people become vulnerable to coronary disease. Individuals with genetic risks have an increased chance of developing angina.
IHD is a companion to metabolic diseases: obesity, diabetes. Increased blood pressure is one of the signs of vascular atherosclerosis. Concomitant diseases increase the risk of heart attacks and strokes. An unhealthy lifestyle, physical inactivity, and smoking make a person a candidate for acute coronary insufficiency.
Foreboding
Doctors say that angina itself is not even a disease, but a serious warning from the body about an impending danger not only to well-being, but also to life. Painful sensations behind the sternum, which are colloquially called “angina pectoris”, serve as a reason to consult a doctor for examination and an adequate diagnosis. After all, angina pectoris is one of the symptoms of coronary heart disease - the main cause of disability and death even among young people.
The feeling of pain in the heart area, radiating to the arm, neck, upper abdomen, should be considered as a serious symptom of impending trouble. Treatment of angina pectoris and its other types should be carried out in a timely manner, after diagnosis. Such pain cannot be left to chance, because only a competent examination and consultation with a specialist will help determine the diagnosis and quality therapy.
Symptoms of the disease
The symptoms of angina attacks of FC 2 and 3 have much in common. Typically, a malfunction of the heart is accompanied by pain in the heart area and has a clear moment of onset and end. The attack can be alleviated by stopping the impact of the load on the body or by taking special heart medications (for example, Nitroglycerin).
In most cases, the pain is localized in the heart area, behind the breastbone. It can be either clearly limited or spread over the entire left half of the chest. The nature of the pain is pressing, squeezing, accompanied by a lack of air. Because of these sensations, patients often experience fear of death and become restless and irritable, covered in cold sweat.
As is known, half an hour of oxygen starvation of the heart leads to myocardial infarction, so if the symptoms of angina pectoris do not stop after taking medications or stopping the load, it is necessary to call an ambulance to provide qualified assistance in a hospital setting.
Risk factors for angina pectoris
The occurrence of chest pain, even in isolated cases, is an alarming symptom indicating a problem in the body. There can be several risk factors for heart problems at the same time. Most often their appearance is influenced by:
- atherosclerosis of the coronary arteries;
- high blood cholesterol levels;
- arterial hypertension;
- sedentary lifestyle;
- smoking;
- obesity;
- increased level of blood clotting;
- diabetes;
- thrombosis;
- thrombophlebitis;
- phlebothrombosis.
Doctors note, and this is confirmed by numerous observations and studies, that stress has a significant impact on the development of angina. And it doesn’t matter at all whether it’s an emotional outburst or a chronic stressful situation. In both cases, chest pain may appear, indicating serious problems, one of which may be exertional angina FC 2 (we will look at what this is in this article).
Prevention of angina pectoris 2 fk
There are many methods for preventing coronary artery disease. The most ideal is an active lifestyle, proper and balanced nutrition combined with physical activity. All measures started at an early age will be a good investment in health, since they will allow you to avoid severe coronary diseases at 40 years of age.
Young age is the best period for disease prevention. Avoid alcohol abuse and smoking. These two factors create favorable conditions for heart disease. Preventing disease is the most effective way to maintain optimal health.
Always follow a culture of nutrition, work and rest - this is the basis of well-being. No matter how difficult it is to adhere to the correct lifestyle, this is the only way to stop the progression of atherosclerosis of blood vessels.
Basics of the development of angina pectoris
The basis for the development of angina pectoris FC 2, as well as any other type of this serious symptom, is a change in tone and endothelial dysfunction of the arteries and coronary vessels, leading to a narrowing of their lumen and spasm. Coronary heart disease is based on a lack of blood supply and, as a consequence, a lack of oxygen.
Angina pain, which is a characteristic sign of coronary artery disease, manifests itself precisely because of an imbalance in the oxygen balance in the cardiovascular system and the heart muscle, in particular. This happens during physical activity, emotional stress, and stress. In some cases, such pain appears at rest.
Causes
We need to talk about three groups.
- The former act as provocateurs of angina attacks.
- The latter determine the pathological process at a fundamental level, making anatomical deviations possible.
- Still others increase the risk of developing the condition. If it already occurs, progression is accelerated.
Among the first
- Anger. The strongest negative emotion. As the affect increases, a large amount of corticosteroids is released. They provoke a narrowing of blood vessels, including the coronary arteries. Against the background of existing pathologies, this leads to the formation of an attack.
- Stress. The intensity of the affect may vary. If it is at a moderate level, “compensation” is achieved through duration. At high intensity, one episode is enough.
- Little physical activity. With FC 2, an attack is possible by simply moving up the stairs to 1-2 floors. Running, gym classes, and swimming are excluded. All activities lead to risk. At the second stage, it is not recommended to strain the body at all; this can end badly.
- Hypothermia affects. The only exception to the presented range of factors.
Second group of reasons
Etiological points:
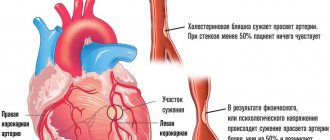
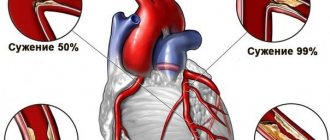
- Atherosclerosis of the coronary arteries. It develops in almost every third person on the planet (according to American scientists).
The essence of the process is the deposition of cholesterol plaques on the walls of large vessels. As a result, the lumen narrows, blood passes through with great resistance, and blood pressure rises.
Tissue ischemia occurs, restoration is carried out using conservative methods. And in the case of deposition of calcium salts into lipid formations - through surgery.
Contrary to possible perception, not only elderly patients, but also young people, especially those who smoke and drink, are at risk of suffering from atherosclerosis. Not the least role is given to diet and nutritional errors.
- Endocrine diseases that provoke vasospasm. Hypercortisolism (excessive production of adrenal hormones), excessive synthesis of thyroid substances, diabetes mellitus as options. Recovery requires a long period of time. The likelihood of success depends not so much on the doctor himself, but on the patient’s willingness to follow all the specialist’s recommendations. In this case, the role of the patient as the creator of his own health is great.
- Vasculitis. Both primary, caused by viral and autoimmune causes, and secondary, developing as a result of systemic lupus erythematosus, rheumatism, and some forms of arthritis. The essence of the disease lies in inflammation of the vascular walls. Not selectively, but all in a row. The coronary arteries are also affected. Treatment is urgent, in a hospital. In the absence of competent assistance, the likelihood of complications increases. What consequences are possible? Vessel stenosis, closure of the lumen as a result of the formation of special strands. In such a situation, recovery is strictly surgical. Drugs are no longer enough.
- Arterial hypertension. Causes increased stress on the cardiac structures on one side. On the other hand, the root cause factor in the formation of the process plays a role. The release of angiotensin-II, renin, aldosterone, corticosteroids and others provokes a narrowing of the lumen of the coronary arteries. The dual mechanism leads to disruption of the normal functional activity of the heart. Angina pectoris is a clinical variant.
Attention:
In some cases, it is possible to develop an attack even at rest; a heart attack without preliminary symptoms is also typical.
- Congenital malformations of the coronary vessels. Anomalies lead to fusion, bends and other types of changes. Treatment is carried out surgically as necessary. But the connection between angina pectoris and abnormalities still needs to be confirmed. Because in reality they rarely turn out to be provocateurs of the disease.
- Compression of arteries by overgrown cardiac structures. As a result of hypertrophy of the ventricles, atria and other conditions. Removal is always surgical. The prospects are vague.
- Metabolic disorders. Usually we are talking about improper lipid metabolism in the body. Externally, the condition manifests itself as obesity. Increased body weight is not the only sign.
Note:
Despite the abundance of etiological causes, the basis is atherosclerosis. The mass fraction in the overall picture is 90-95%. Everything else is unimportant.
Diagnosis is also carried out with an eye to this condition, but if cholesterol deposition is excluded, further searches for atherosclerosis are indicated, which still require continued diagnosis. Perhaps we are talking about a system of factors.
Third group of reasons
Causes increased risks:
- Age 45+.
- Being male. According to various estimates, women suffer several times less often (m/f ratio is defined as 3-4:1). There is also a less aggressive course in the weaker sex.
- Smoking. Provokes persistent stenosis of arteries, including coronary ones. Over time, this reaction becomes stereotypical and does not require repeated stimulation. It is extremely difficult to cope with this option; even giving up a bad habit does not give full results.
- Caffeine abuse. All drinks are excluded: including tea, energy drinks.
- Excess alcohol. The amount of alcohol does not play a big role. It all depends on individual resistance and reaction to ethanol. For one a sip is enough, for another a bottle is not enough. Still others may drink alcohol their entire adult life and die from a cold. It’s not worth taking risks and experimenting on yourself. Alcohol has no place in the life of a healthy person.
- Burdened heredity. The genetic factor plays an important role.
- History of diabetes mellitus, hypertension, endocrine conditions.
- Obesity. Indirect risk factor.
All possible causes are taken into account in a comprehensive manner. Without this, there can be no talk of high-quality diagnosis, much less treatment.
Typical and atypical manifestations of angina pectoris
Often, after examination, the patient is diagnosed with angina pectoris 2 FC. What it is? This name has one of the pain symptoms indicating a violation of the cardiac blood supply. This sign is clear enough that it allows you to immediately make a diagnosis.
The pain appears behind the sternum and is burning, pressing or uncomfortable. These sensations can radiate to the left side - the shoulder blade, arm, lower jaw, as well as to the left side of the neck or throat. Pain can also radiate to the upper abdomen to the right side of the body - also to the arm, throat, and shoulder blade.
The most important thing is that the disease does not manifest itself in any way outside of an attack. That is, the patient does not experience any other sensations other than attacks of pain. The attack passes and the pain disappears until the next peak.
A typical sign of such an attack is suddenness. It occurs unexpectedly against the background of stress, emotional outburst, or physical activity. Another feature that makes it possible to clearly diagnose a typical angina attack is its ability to pass on its own or with the use of Nitroglycerin, which expands the lumen of blood vessels, thereby relieving spasm and increasing oxygen access to the heart.
Angina pectoris: what is it and how does it manifest?
The coronary vessels, through which the heart is supplied with blood, are often susceptible to atherosclerotic changes.
They narrow due to the presence of cholesterol plaques, making it difficult to deliver oxygen to the myocardium. As a result, coronary heart disease develops. Angina pectoris is the main symptom of acute hypoxia. The manifestation of the syndrome is associated with the influence of certain factors.
Most often, an attack is related to physical activity.
What is angina pectoris 2 FC?
Angina pectoris 2 is a symptomatic complex that occurs in response to severe oxygen deficiency. It can be stable and unstable. In the first case, we are talking about stable ischemic angina pectoris 2 fc.
A person feels its signs during moments of intense physical activity, when the heart requires more oxygen. In a calm state in the absence of provoking factors, attacks do not appear.
There is a certain degree of activity, after exceeding which the patient’s well-being deteriorates sharply.
Unstable angina develops at any time, regardless of the level of physical activity. It can bother the patient even in a calm state. This is a more severe form of the pathology, leading to life-threatening complications. It almost completely limits a person in everyday situations, making him incapable of self-care.
Angina pectoris can belong to different functional classes. It is customary to distinguish four such classes. Each of them has its own characteristics and features of their manifestation. Pathology of the fourth class (4 fc) is considered the most severe; fc 1 has almost no symptoms and is detected only during the examination. FC 3 is a transitional phase between moderate and severe disorders.
Most often, medical specialists have to deal with angina pectoris of the second functional class (ICD-10 code 120.8 “Other forms of angina”), which develops steadily under certain conditions.
Symptoms at this stage are already noticeably manifested, the person feels limited in some physical activities, and the quality of his life noticeably deteriorates.
But at the same time, the syndrome responds well to preventive treatment and control, and serious complications can be prevented.
The diagnosis of “coronary heart disease, class 2 exertional angina” is the reason for establishing one of the disability groups in the patient.
Causes
The main reason for the development of stable angina pectoris type 2 as a symptom of coronary artery disease is the presence of atherosclerosis of the coronary arteries. It constricts blood vessels, preventing proper blood circulation to the heart. A painful attack occurs when a discrepancy occurs between the need of myocardial tissue for oxygen and the ability of the bloodstream to satisfy this need.
There are other pathologies that can cause angina attacks. These include:
- hypertension;
- aortic stenosis;
- diabetes;
- obesity;
- post-infarction period with the development of cardiosclerosis;
- tachycardia;
- cardiomyopathy with hypertrophy of the heart chambers;
- increased pressure in the blood vessels of the lungs;
- coronary
An ischemic attack occurs when the need for oxygen and additional nutrition of the heart increases. These situations can be represented by the following list:
- Strong emotions that contribute to the release of adrenaline. This hormone constricts blood vessels, stimulates the myocardium, and increases blood pressure. Blood is pumped more intensely.
- The load on muscle tissue is accompanied by biochemical reactions, which are accompanied by the absorption of large amounts of oxygen. The heart rate increases, blood pressure inside the vessels increases, which aggravates ischemia.
- Overeating causes stretching of the stomach and intestines. They put pressure on the lung tissue, making it difficult for a person to breathe. In this case, most of the blood resources are sent to the organs of the digestive system to promote the active processing of what is eaten. For these reasons, the heart lacks oxygen.
- Cooling the body provokes vasoconstriction and an upward pressure surge, which causes acute hypoxia of the main muscle of the circulatory system.
- Smoking a cigarette leads to a rapid heartbeat, norepinephrine is released into the blood, and blood pressure rises. The heart works harder.
- When a person takes a lying position, blood rushes to the myocardium, it is forced to contract more often and faster. In addition, the internal organs shift slightly, putting additional pressure on the heart muscle and blood vessels of the lungs.
Clinical symptoms
Angina pectoris FC 2 is identified by specific signs:
Sharp pain in the chest on the left. They are of a pressing, cutting, burning nature. There is a heaviness in the heart. The pain spreads to the left half of the body (arm, shoulder, scapula), penetrates into the neck, lower jaw, ear. Your stomach or back may hurt.
- The duration of an attack of severe pain is from 3 to 5 minutes.
- Severe shortness of breath occurs, it is difficult to take a deep breath. Such a symptom may be equivalent to the pain syndrome of angina or accompany it.
- Sudden loss of strength.
- Panic, a premonition of imminent death.
- Sweating increases.
- The rhythm of heart beats is disrupted.
- There are differences in the tonometer readings.
- The possibility of nausea or vomiting cannot be ruled out.
Such manifestations arise under certain conditions, which will be different for each functional class.
Features of angina pectoris 2 fc
The 2nd functional class of angina is distinguished by the following features:
- A man has difficulty climbing one flight of stairs.
- A distance of half a kilometer at a moderate walking speed causes noticeable discomfort.
- Running, even slow, provokes an attack.
- Heightened emotional reactions are potentially dangerous.
- Adverse weather conditions in the form of wind, rain, snow, frost also cause a deterioration in health.
- Sometimes there is a morning predisposition to the development of unpleasant symptoms.
Modern diagnostic methods
Numerous types of studies can detect angina pectoris:
- Questioning the patient to determine the nature of the pain and the conditions under which it occurred. The possibility of hereditary predisposition is revealed. Lifestyle and the presence of provoking factors are studied.
- Laboratory testing of biological fluids is necessary to determine the possible causes and complications of ischemia. Allows you to assess the risk of developing atherosclerosis. A coagulogram and lipidogram are required.
- An informative diagnostic method is an ECG. Readings are taken during an attack. It is advisable to use Holter ECG monitoring throughout the day, this allows you to record cases of ischemia that are asymptomatic. Stress tests are used to artificially provoke pathogenic symptoms with recording of cardiogram readings.
- Angiographic examination of the coronary vessels. The injection of a contrast agent and x-rays are used.
- Computed tomography (multispiral method) is needed to obtain a three-dimensional image of the heart.
- Doppler ultrasound diagnostics of peripheral vessels. It is carried out to detect atherosclerosis.
- EchoCG in combination with physical activity records deviations in myocardial contractility in a tense state.
Treatment
Angina pectoris is not an independent disease. It is a sign of coronary insufficiency. It is this pathology that needs to be treated.
Complete elimination of irreversible changes in blood vessels leading to ischemia is only possible through surgery.
Therefore, drug control of angina pectoris is aimed only at stopping attacks and reducing the frequency of their occurrence, but cannot permanently rid a person of this disease.
The most commonly used drugs for angina pectoris:
- Antiplatelet agents that thin the blood and reduce the risk of developing blood clots: Aspirin, Dippridamole.
- They quickly expand the lumen of blood vessels, relieve an acute attack, and improve blood flow with drugs from the group of nitrates - emergency drugs: Pentacard, Nitrolong, Nitroglycerin.
- Statins reduce cholesterol levels in the body: Atoris, Torvakar.
- Beta blockers help reduce stress on the heart. They affect the heart rate, normalizing it: “Bisoprolol”, “Concor”.
- Agents that prevent the penetration of calcium ions into muscle tissue. This leads to the relief of vascular spasm and the free flow of blood. Examples of drugs: Amlodipine, Diltiazem.
- ACE blockers: Enalapril, Ramipril, Captopril reduce blood pressure on the walls of blood vessels, dilating them.
In addition to drug therapy, you need to eat right (less fat and carbohydrates, more fruits, vegetables, fish), exercise with a moderate degree of exercise under the guidance of a doctor (volleyball, football training, cycling, walking, and swimming classes are allowed).
Methods of surgical treatment:
- Plastic surgery of coronary vessels.
It involves installing a stent (metal frame) inside a narrowed section of an artery to improve its patency or balloon angioplasty with the introduction of a special expanding balloon into the vessel. Both procedures are minimally invasive.
- Coronary artery bypass grafting.
During the operation, the surgeon creates an additional blood path (shunt) that bypasses the affected area.
The material for the shunt is a part of the vessel taken from other organs (for example, from the limbs).
This type of surgical intervention is more complex; the procedure is carried out with the patient connected to the artificial blood supply system. Another option is open heart surgery.
Consequences of coronary artery disease, angina pectoris 2 fk
Angina pectoris of the second functional class generally does not pose a mortal threat to humans. Complications are possible, but in rare cases.
In this case, the patient leads an incorrect lifestyle, does not adhere to the proposed recommendations, and does not take prescribed medications. Proper treatment and adequate behavior of the patient will help him for a long time and with minimal restrictions.
A person has a chance of a full recovery after surgery on damaged vessels.
Possible complications:
- Atrial fibrillation and other types of heart rhythm disturbances.
- Sudden death of a patient from cardiac arrest.
- Acute form of myocardial infarction.
- Progression of angina pectoris of the second functional class, development of an unstable form of pathology.
- Chronic myocardial failure.
A person diagnosed with angina pectoris 2 FC can count on receiving group 3 disability.
IHD and exertional angina syndrome FC 2 are a common and quite alarming medical conclusion. It indicates the development of serious disorders in the coronary blood supply. The obvious symptoms of an attack are hard to miss.
Their first appearance should be a signal for urgent medical attention. Self-treatment can be fatal. Traditional medicine methods can only complement basic therapy.
With timely diagnosis and the use of supportive medication, you can live with angina into old age.
Source: https://MirKardio.ru/bolezni/szhatie/stenokardiya-napryazheniya-2-fk-chto-ehto-takoe.html
Types of Angina
For many of those who suffer from attacks of angina pectoris, such pain seems insignificant, because they pass quickly enough, often even without taking special medications. But this is a big mistake that can lead to a heart attack, disability or death. Experts divide angina pain into two types:
- angina at rest;
- angina pectoris.
The diagnosis is made taking into account the features that can be seen in the names of the types themselves.
Angina pectoris is quite predictable, because the patient knows that in a certain situation that causes stress, both physical and emotional (and this could be fast walking, a sharp change in air temperature, stress), there will be an attack that must be stopped by taking Nitroglycerin.
And angina at rest can develop in any situation, even calm for a person, when it seems that there are absolutely no prerequisites for it. Experts divide this type of heart problem according to the nature of its course - stable and unstable. The names speak for themselves:
- Stable - predictable, occurring with a certain frequency.
- Unstable can be either new, progressive, or post-infarction.
Only a specialist can correctly understand the essence of angina pain.
Angina pectoris FC 3 is a special case of IHD. What it is
Coronary heart disease has many clinical forms. One of the most common is “angina pectoris”. This is what people call angina pectoris.
The disease mainly affects people over 45 years of age. Depending on the severity, the pathology can limit the ability of patients to work.
Angina pectoris FC 3 significantly worsens the patient's quality of life. What kind of disease is this and what does this condition entail?
General description of the disease
Stable angina pectoris is understood as a chronic cardiac pathology of an ischemic nature, the classic manifestation of which is chest pain after physical activity, emotional stress, due to a sharp temperature change or exposure to a strong gust of wind.
It should be noted that in the grading of coronary artery disease, angina is divided into stable and unstable. The latter includes pathology that first appeared less than 1 month ago or progressive pain attacks.
The stability of the condition is indicated by pain of the same type, occurring under the same loads and having the same duration.
Cardiac ischemia develops on the basis of a number of processes, the main of which are coronary spasm and atherosclerotic lesions of the coronary arteries. The situation is further aggravated by the presence of anemia, diabetes and arterial hypertension.
How it manifests itself
Stable angina pectoris is divided into classes depending on the factors that provoke the appearance of pain. The mildest degree (FC 1) corresponds to the occurrence of an anginal attack when performing extremely strong work.
A pathology with a slight limitation of normal physical activity is placed one step higher, when the patient finds it difficult to walk more than two blocks or climb to the second floor.
Angina pectoris, in which an attack develops when climbing one flight of stairs or walking at a normal pace of 100-200 m, corresponds to FC 3.
Functional class 4 is considered the most severe, with the development of the syndrome at rest up to difficulty in self-care.
The nature of pain in ischemic heart disease:
- Localized behind the sternum;
- They have a pressing, squeezing character. Some patients describe burning pain.
- They radiate to the shoulder blade, left shoulder girdle, arm, lower jaw.
The clinical picture is complemented by increased heart rate, pallor, the appearance of sweat on the forehead, and other subjectively unpleasant sensations.
Among the common features inherent in cardiac ischemia, some individual differences can be identified for each form of coronary artery disease.
Pain syndrome with stable angina is characterized by attacks lasting up to 3–5 minutes, which subside on their own or after taking nitrates.
The equivalent of pain can be shortness of breath, which impedes activity and replaces cardiology.
Additional research methods
A history of the disease with characteristic complaints of chest pain that occurs under certain circumstances is a subjective criterion for making a diagnosis. To objectify the data, they resort to an ECG and stress tests. During ischemia, classic changes in the form of a decrease (less often an increase) in the ST segment are recorded on the film.
Bicycle ergometry (“bicycle”) and treadmill test (“treadmill”) make it possible to qualitatively assess the load that entails the development of a painful attack and/or registration of ischemic manifestations on the electrocardiogram.
Daily ECG monitoring helps to detect ischemia during the day during the patient’s usual daily routine.
The main task for the patient during this study is to keep a diary noting his actions and state of health. In this way, it is also possible to detect painless episodes of angina.
Echocardiography, X-ray examination methods are prescribed, and laboratory blood parameters are studied.
Treatment
Therapy is based on regular intake of pharmacological drugs of various groups.
Patients are forced to take for a long time:
- nitrates, to prevent angina attacks and relieve them;
- antiplatelet agents (clopidogrel, aspirin) to reduce blood clots;
- statins, which stabilize existing atherosclerotic plaques;
- ACE inhibitors or angiotensin II receptor antagonists (ARAs), if arterial hypertension, diabetes mellitus, left ventricular dysfunction, or complicated angina are detected.
- β-blockers in the presence of heart failure and myocardial infarction.
Patients with progression of pathology or stabilization of the process with disruption of normal physical work are often unable to perform their previous professional duties in full.
In such cases, the task of medical and social examination is to assess the ability to work of a patient with coronary artery disease.
Angina pectoris FC 3 is a diagnosis that requires removal from heavy physical labor and psycho-emotional stress, transfer to work with less energy consumption and activity.
Also, patients with IHD with this form should not be allowed to drive vehicles, electrical equipment and other dangerous objects due to the possible development of an attack at the workplace.
As a rule, such patients are assigned disability group II, less often milder - III, since FC 3 angina is often not an isolated disease.
Forecast
Under optimal conditions, it is possible to achieve control over the course of the pathology, identify positive dynamics with subsequent revision and assignment of a smaller functional class.
To do this, you must carefully follow all medications and normalize your lifestyle and diet. Patients with angina pectoris FC 3 must rationally resolve the issue of organizing the labor process.
Stable heart problem
Angina pectoris is divided into functional classes, which were determined through numerous studies conducted by doctors, physiologists, and scientists.
For each patient, a competent diagnosis is necessary, taking into account the medical history, general condition at the time of the onset of angina pain, concomitant diseases or pathological conditions, which is necessarily reflected in the medical history.
Angina pectoris 2 FC is a fairly common diagnosis for people of different ages and genders, because FC - functional classes - take into account the degree of physical activity that causes angina pain. We can talk about the stability of the problem when the patient feels attacks for more than a month.
Angina pectoris II FC: causes, diagnosis and treatment
The most common form of coronary artery disease is angina pectoris.
An exacerbation of this disease occurs with increasing physical stress on the body and the inability of affected or narrowed vessels to fully satisfy the increased demands of the myocardium for blood flow.
According to statistics, IHD diseases are the most common causes of death, both in Russia and throughout the world. They account for up to seventy percent of all deaths associated with human cardiovascular diseases.
Signs
The main signs of exertional angina in a patient are:
- dyspnea;
- the appearance of pain in the heart;
- tightness of breathing and discomfort in the chest area.
With this disease, pain can be felt in the sternum, but can radiate to the cheek, neck, left arm or under the left shoulder blade. When an attack of illness occurs, other phenomena are possible:
- sudden weakness;
- the appearance of cold sweat;
- Heart arythmy;
- pressure surges.
Sometimes such an attack causes stomach pain, vomiting, nausea, and flatulence. A typical attack of the disease lasts from two to five minutes. Depending on the form of the disease, such exacerbations can be repeated from several attacks a day to one over several weeks or even months.
Prevalence of the disease
Angina pectoris is most common among older people. For example, among men aged 45 to 55 years it occurs in 2-5%, and among men over 65 years old - in 10-20%. Among women, this disease is less common. Factors that increase the risk of contracting this disease are:
- smoking;
- physical inactivity;
- diabetes;
- obesity.
Classification
Angina pectoris is divided into the following forms:
- primary;
- stable;
- progressive.
The disease is considered primary if less than one month has passed since the first attack. Then the disease can behave differently - either go into the second (stable) form or disappear completely.
The stable form continues for a longer time and is distinguished by the fact that under the same load the body behaves in the same way.
The disease in this form can persist for several years.
The third (progressive) form is unstable. With this form, the same load causes more and more severe attacks, which become more and more prolonged.
Depending on the patient’s ability to tolerate stress, angina pectoris is divided into 4 functional classes (FC). At the same time, the lightest classes are 1FC and 2FC, and the more dangerous are 3FC and 4FC.
In the presence of a disease of the first functional class, a person easily overcomes standard loads, and exacerbations occur only with relatively large efforts. For example, during a long climb up the stairs or a short jog.
A person who has been diagnosed by a doctor with “effort angina of functional class 2” has some restrictions on exercise. Ordinary walking over a distance of 500 m or climbing stairs to the second floor of a house can cause seizures in such a patient. In this case, the occurrence of exacerbations can also be affected by wind, cold weather or human emotions.
Persons with such a diagnosis may qualify for group 3 disability. But this is only possible if they previously suffered an uncomplicated myocardial infarction.
For a person diagnosed with a disease of the third functional class, the loads have significant limitations.
Exacerbations in him can be caused by walking a hundred to five hundred meters or climbing the stairs of a house just one flight.
In a patient with a fourth functional class disease, physical activity is severely limited. He may have seizures with little effort or even in a calm state.
Diagnostics
The diagnosis of the disease can be made by a cardiologist after conducting a series of studies. They may be:
- ECG;
- EchoCG;
- load tests (bicycle ergonometry, treadmill test, walking tests);
- stress echocardiography;
- Holter monitoring;
- positron emission tomography.
In addition, a biochemical blood test is performed. According to this analysis, depending on the content of cholesterol and lipids in the blood, the possibility of vascular atherosclerosis is assessed. When diagnosing this disease, the cardiologist must distinguish this disease from other diseases that may have similar symptoms. Such diseases include:
- osteochondrosis;
- myocardial infarction;
- dysfunction of the gastrointestinal tract;
- lung diseases (pneumonia).
Folk remedies
When treating angina, in consultation with your doctor, you can use folk remedies along with medications. For example, these include:
- hawthorn;
- horseradish with honey;
- herbal infusion.
To obtain a hawthorn tincture, seven tablespoons of berries are brewed with boiling water and infused. Then strain and drink 1 glass during meals. Horseradish, grated, is mixed with honey (ratio 1:4). Take 1 teaspoon twice. This remedy is used for mild angina if it occurs without pain in the chest.
An infusion of herbs helps with palpitations and relieves pain in the heart area. The infusion consists of hawthorn, lemon balm, horsetail and valerian, poured with boiling water. To obtain an infusion, pour 1 tablespoon of the mixture into 1 glass of boiling water. Then infuse and drink one third of a glass before meals.
How is angina pectoris classified?
To make an adequate diagnosis of coronary artery disease, the doctor must ask the patient about the nature of the pain and the accompanying details of life activity that cause the attack. Based on these data, as well as the examinations and tests performed, a conclusion is made about an accurate diagnosis.
Functional classes of angina pectoris indicate the nature of the physical or emotional stress that gives rise to the attack:
- FC 1 is characterized by a practically asymptomatic course of the problem, although ECG and ultrasound of the heart show disturbances in the functioning of the cardiovascular system.
- Angina pectoris of functional class 2 is more pronounced than the previous type.
- Functional class 3 involves quite serious restrictions on physical and emotional stress.
- The last, class 4, manifests itself with minimal stress and requires maximum peace both physically and emotionally.
Diagnosis of angina pectoris
It is quite simple for a cardiologist to determine stress angina. In order to diagnose the disease, a number of studies are carried out - an electrocardiogram, ultrasound diagnostics of the heart. If necessary, coronary angiography may be performed to make the diagnosis more clearly. After the doctor decides on the main diagnosis - angina pectoris, he will conduct additional studies to determine the functional class of angina pectoris. Load tests will help with this: treadmill test, bicycle ergometry, cold test.
The treadmill test is an informative technique that allows you to determine IHD at an early stage, when even hardware methods do not always cope with this task. This test is recommended for all persons over the age of fifty, regardless of the presence of cardiac complaints. In addition, doctors resort to a treadmill test if necessary to make a differential diagnosis of pain in this area.
The essence of the test is to load the patient's heart to a certain level, when deviations in its functioning appear. Typically, the load is given on a treadmill, and electrodes are attached to the patient, which will record heart performance. With their help, the doctor will be able to see when the patient’s heart begins to work abnormally and stop the load. A cuff is placed on the patient to measure blood pressure. At first, the patient just begins to walk along the path, but after three minutes the doctor changes the angle of the path relative to the floor and slightly increases the speed. At the end of the test, the results are interpreted and a diagnosis is made.
Bicycle ergometry is a type of treadmill test. The essence of the technique is the same load on the heart, only it is given not on a treadmill, but on an exercise bike. A cold test involves immersing your hand in a container with cold water or ice cubes, and after a certain time, blood pressure is measured and an electrocardiogram is taken.
The methods described above make it possible to diagnose exertional angina with high accuracy and assign it a functional class number.
Features of II FC
One of the common health problems that can lead to death is coronary heart disease. Angina pectoris 2 FC is a symptom complex of such a disease. It is characterized by a fairly high level of physical and emotional stress that the patient can endure.
Many signs of this class of angina pain are familiar to most people, many of whom do not even suspect they have such a problem. The attack occurs when running or fast walking, as well as when climbing stairs at an active pace.
A characteristic feature of functional class II of exertional angina, in contrast to FC I, is a response-attack to frosty air, breathless strong wind, as well as to rich, heavy food.
Symptoms
Manifestations of FC 2 of exertional angina occur as a result of moderate physical and emotional activity and are quite pronounced.
If we translate abstract words into something concrete: it is impossible to climb to the 2-3 floor, sports are also no longer available. Even intensive walking is difficult.
The following manifestations occur:
- Chest pain of moderate intensity, not too pronounced, is the main characteristic symptom. It radiates to the shoulder blade and left arm, moving as if through the veins and reaching the hand. It does not intensify with movement or breathing, which distinguishes it from the discomfort caused by intercostal neuralgia. Treated with Nitroglycerin. Duration: 10-12 minutes, but no more than half an hour. Deviations towards intensification indicate a possible heart attack.
- Dyspnea. Increase in the number of movements per minute. In the second class of angina, it is already difficult not to notice it. Characterized by discomfort and dissatisfaction with inhalation. Accompanies moderate physical activity.
- Cyanosis of the nasolabial triangle, blue discoloration of the area around the mouth.
- Paleness of the skin.
- Panic attack. The patient becomes anxious and is in an inadequate state. Help Wanted.
- Increase in blood pressure. Not always, but often. Within insignificant limits.
- Nausea, dizziness.
- Arrhythmias. By type of tachycardia, as a rule. The frequency of contractions remains normal, but the intensity of work is higher.
- Fainting is possible. Relatively rare. Indicate the involvement of cerebral structures in the pathological process.
At the end of the attack, the entire clinical picture disappears.
Attention:
If it lasts more than 30 minutes, there is a high risk of a heart attack. It is easy to confuse it with angina pectoris without experience. Mortality is many times higher. It is also possible to smoothly flow from one state to another.
First aid
For those who are experiencing the symptoms of angina for the first time, what to do is an unexpected and difficult question. After all, pain in the heart can cause horror from the possibility of a heart attack and death or disability. The main goal of such assistance is to relieve an attack of pain, which Nitroglycerin does well.
If you feel pain in your heart, you need to sit comfortably with your feet on the floor, unbutton the top button of your shirt, removing the scarf and jewelry from your neck to make breathing easier. For the same purpose, it is necessary to open the window to get fresh air.
Nitroglycerin should take effect within 2-3 minutes; if the pain does not subside, you need to take another tablet of the drug. If there is no effect from taking this medicine, you must call an ambulance.
It is also necessary to call an ambulance if:
- an attack of pain in the heart area happened to a person for the first time;
- the pain does not go away after 5-7 minutes;
- Nitroglycerin does not help;
- weakness and pain increase;
- Nausea and vomiting appeared.
In these cases, the person most likely develops a heart attack rather than angina. Symptoms in this case require qualified medical care and hospitalization.
IHD: treatment of angina pectoris 2fk
Medical care in the early stages consists of therapeutic methods that include medications and physical procedures. Medicines have vasodilating, hypotensive and cholesterol-lowering effects. Later stages of angina are subject to cardiac surgery.
There are non-invasive and invasive interventions: angioplasty, as well as bypass surgery with stenting.
Angioplasty is a mechanical dilatation of narrowed arteries. It is used for emergency restoration of patency in acute conditions, as well as routinely for angina pectoris and vasoconstriction of more than 50%.
Bypass surgery is a more complex procedure that restores blood flow by creating a bypass anastomosis. A piece of tissue is taken from the vessels of the limbs or chest to perform a shunt between healthy areas of the coronary vessels. The operation is performed using both artificial blood circulation and an open heart. Depending on the degree of coronary artery stenosis, the number of bypass grafts may vary for each patient.
In the treatment of mild forms of angina, preference is given to therapeutic treatment. The following drugs are used:
- Disaggregants (blood thinners);
- Beta blockers;
- ACE blockers;
- Statins;
- Nitrates.
The goal of therapy is to reduce the load on the heart, dilate the coronary vessels, lower cholesterol and blood pressure. The complex effect on these mechanisms leads to the elimination of attacks of angina pectoris 2.
How is angina pectoris 2 FC diagnosed?
Like any other health problem, angina pectoris must be properly diagnosed. This requires a thorough medical examination, including instrumental and laboratory tests, as well as functional diagnostics. There is no need to panic if you experience symptoms characteristic of a diagnosis of angina pectoris. What to do? Contact a medical facility for help, especially if an attack is registered for the first time. The doctor will prescribe the following set of measures to make a diagnosis:
- blood analysis;
- bicycle ergometry;
- coronary angiography;
- scintigraphy;
- Holter ECG monitoring (24-hour ECG);
- electrocardiography;
- echocardiography.
The specialist decides which instrumental examination to choose based on the medical history and preliminary diagnosis.
The essence and typology of forms of the disease
The heart, the main muscle of the body, receives nutrition through the supply of oxygen and nutrients through the arteries. The daily requirement may increase if a person performs a certain physical activity. Accordingly, blood flow to the main organ increases.
The coronary and coronary arteries, which “serve” the heart, come from the aorta. If they are not normal, blood flow is disrupted. This means that a certain part of the heart muscle will not receive enough oxygen and the necessary substances for normal functioning.
This failure is called ischemia. If this condition lasts more than 30 minutes, cardiomyocytes in the heart begin to die, which leads to myocardial infarction. The pathology can become more active when the permissible level of physical activity is exceeded and is accompanied by pain.
There are 4 functional classes of the disease (FC). The main criterion for differentiation is the severity of the form and the permissibility of physical activity:
- FC 1 is a relatively mild degree of the disease, in which moderate exercise is allowed. An attack is possible only in case of extreme physical stress.
- FC 2 involves restrictions on physical activity. This class includes patients whose angina attack begins after walking 500 m or when climbing stairs to the second floor. In addition, patients are not recommended to walk in cold and windy weather, to be active immediately after waking up from sleep, or to experience emotional stress. All this can also provoke a deterioration in well-being.
- FC 3 significantly limits a person’s physical activity. An attack can be triggered by walking at an average speed for 100-500 m and climbing a flight of stairs.
- FC 4 is the most severe form. This is a disability in which seizures can occur even when at rest.
The most common form among heart patients is FC 3, which is regarded by doctors as a disability. In combination with other diseases, for example, tachycardia or arrhythmia, ischemic heart disease (IHD) angina pectoris can provoke attacks for no apparent reason when the patient is at rest.
It is also worth noting that patients with FC 3 disease can usually control their abilities well. They are also able to sense upcoming attacks. This helps to neutralize them in advance and reduce the intensity to nothing.
to the point ↑
How to treat?
Treatment of angina pectoris of any class is a whole range of measures necessary to maintain the functioning of the cardiovascular system within normal limits. Unfortunately, this problem cannot be completely cured, and after diagnosis, the patient will be forced to take certain medications for the rest of his life in order to avoid the development of a heart attack and sudden death. Only a qualified specialist can prescribe adequate medications. These include:
- calcium channel antagonists, which reduce the need for oxygen in the heart muscle;
- beta blockers, which reduce heart rate and blood pressure;
- angiotensin-converting enzyme inhibitors (ACEIs), used to prevent vasospasm;
- nitrates to dilate blood vessels and reduce the heart's need for oxygen;
- drugs that reduce blood clots;
- statins, which help reduce the amount of cholesterol in the blood.
In some cases, a patient with coronary artery disease is indicated for surgical intervention to restore high-quality blood supply to the heart muscle. The patient may undergo:
- coronary artery bypass grafting;
- coronary (balloon) angioplasty.
Is it possible to cure angina pectoris FC 3?
Considering that angina pectoris is a chronic pathology, it is impossible to completely get rid of this condition. However, the patient will still be able to maintain a normal condition. Most often, doctors prescribe drug therapy, including:
- Aspirin for thinning the blood, since plaques form precisely for this reason, the drug is effective;
- Nitroglycerin - available in the form of tablets or spray, it cannot be taken regularly, but only during attacks;
- Calcium antagonists – prevent vasoconstriction, eliminate their spasm and increase tone;
- Beta-blockers – prevent the development of a heart attack, reduce the myocardium’s need for oxygen;
- Drugs that prevent blood clots belong to the group of lipid-lowering drugs and contain anti-exchange resins.
In particularly advanced cases, when coronary artery disease and angina pectoris FC 3 progress, treatment is carried out using surgical methods. The most common is coronary angioplasty. The essence of the intervention is to insert a special balloon into the artery, which will destroy the atherosclerotic plaque.
Another radical treatment method is coronary artery bypass surgery, when an additional path is created for blood flow from the aorta. This operation is more complex and is performed if the patient does not have serious concomitant pathologies.
Prevention of coronary artery disease is the best medicine
If a person is diagnosed with coronary artery disease, angina pectoris FC 2, the lifestyle must be structured in such a way as to minimize the possibility of an attack and complications in the form of stroke, heart attack and death.
Doctors advise using the principle with the same abbreviation as the disease itself - IHD. The letter “I” here means: “get rid of tobacco smoke,” the letter “B” means “move more,” and the letter “C” means “lose excess weight.”
You also need a rational, balanced diet, rich in components that regulate the functioning of the whole body: vitamins, micro- and macroelements, amino acids, fiber.
Answering the question of what angina pectoris FC 2 is - what it is, doctors talk about a symptom complex of problems in the functioning of the heart and cardiovascular system, manifested in attacks of pain in the chest and are a harbinger of serious health problems.
Clinical symptoms
Angina pectoris FC 2 is identified by specific signs:
- Pain syndrome.
Sharp pain in the chest on the left. They are of a pressing, cutting, burning nature. There is a heaviness in the heart. The pain spreads to the left half of the body (arm, shoulder, scapula), penetrates into the neck, lower jaw, ear. Your stomach or back may hurt.
- The duration of an attack of severe pain is from 3 to 5 minutes.
- Severe shortness of breath occurs, it is difficult to take a deep breath. Such a symptom may be equivalent to the pain syndrome of angina or accompany it.
- Sudden loss of strength.
- Panic, a premonition of imminent death.
- Sweating increases.
- The rhythm of heart beats is disrupted.
- There are differences in the tonometer readings.
- The possibility of nausea or vomiting cannot be ruled out.
Such manifestations arise under certain conditions, which will be different for each functional class.
First aid for a seizure
Angina pectoris is a chronic disease. Therefore, a complete cure is not always possible and only through surgical intervention.
But first of all, the patient and his immediate environment need to learn how to provide first aid during attacks.
Nitroglycerin and drugs based on it are the main means for stopping a crisis. At the first symptoms, the patient needs to put one tablet under the tongue and dissolve it. If the attack is severe, you can give it twice. It is better if the oral cavity is sufficiently moist. The maximum dose, 5 tablets, is taken in extremely severe cases when medical help is not expected.
You can also use a spray instead of tablets. The results of the action of nitroglycerin can be seen within a couple of minutes.
Sometimes they try to stop the attack with validol. This is a grave mistake, since this medicine not only does not help, but can cause serious harm to health.
But those around you can use simple ways to ease the crisis. To do this, it is necessary to stabilize the patient’s condition as much as possible, both physically and morally:
- the person must be allowed to stand for a while and catch his breath if the attack was provoked by intense physical activity;
- if the cause is stress, the patient needs to be reassured;
- it is important to provide the person with a sitting or semi-sitting position, as well as an influx of fresh oxygen;
- the body should be freed from any oppressive objects, including belts, collars, and excess outerwear;
- You can place heating pads with warm water on your feet.
to the point ↑