Signs of arterial hypotension
A decrease in blood pressure can be acute or chronic. Let's consider each of the points.
Acute form
Its development is facilitated, which can lead to collapse. At the same time, there is a deterioration in the blood supply to vital organs, which is a very dangerous phenomenon.
Main symptoms of the disease:
- severe dizziness to the point of loss of consciousness;
- muscle weakness;
- trembling in the body, feeling of chilliness;
- pallor of the skin.
At the very beginning of the drop in pressure, the patient’s consciousness remains, he answers questions correctly, but his speech is slow and inhibited. In addition, the frequency of respiratory movements is noted, the pulse is rapid, thread-like, and weakly filled.
As collapse develops, natural reflexes fade, short-term loss of consciousness, problems with breathing and heartbeat may occur. Next, the pupils dilate, breathing and heartbeat stop, that is, death occurs.
Depending on the cause, the acute form can develop in different ways:
- if hypertension occurs as a result of a heart attack or blockage of the pulmonary artery, then there is a burning pain in the chest, short-term cessation of breathing, and discharge of pink foam from the oral cavity;
- with a sharp drop in body temperature due to infection, muscle weakness and sweating;
- in case of intoxication – diarrhea (up to 10-15 times), vomiting, weakness;
- with blood loss - the presence of excitability, and then apathy and agony. The skin color becomes sharply white and pale.
Treatment of acute form
Self-treatment of the acute form is not provided! At the first symptoms, you must call an emergency team! Before their arrival, you can lay the patient down, unbutton the top buttons, loosen the tie or scarf.
Medical therapy is aimed at increasing blood pressure and replacing blood loss.
Chronic form
It is observed in patients who suffer from low blood pressure for a long time. At the same time, they feel very bad and note the following symptoms:
- weakness, fatigue during physical activity;
- loss of coordination, dizziness, drowsiness;
- cold extremities - palms and feet - at normal ambient temperature;
- , pain in the heart area.
For high-quality and effective treatment of a chronic form of the disease, one should look for the cause that caused it. At your appointment, be sure to present ALL complaints, even those that, in your opinion, have nothing to do with the drop in blood pressure:
- a sign of the presence of Koch's bacillus or tuberculosis: decreased blood pressure, increased temperature, weight loss, blush on the cheeks, shortness of breath, frequent cough;
- adrenal insufficiency: hypotension, weak pulse, gray skin;
- orthostatic collapse: observed with a sharp rise of the body to a vertical position, decreased blood conductivity through large veins, gross excess of the dose of the drug.
Treatment of chronic hypotension
In addition to treating the leading disease, it is recommended to carry out additional therapy, which is aimed at increasing the readings on the tonometer.
Recommendations for hypotension:
- combating stress and negative emotions;
- auto-training classes;
- rational fortified diet;
- 10-minute morning exercises, relaxing shower;
- treatment with herbal medicines – ginseng, eleutherococcus;
- restorative massage;
- sanatorium treatment according to the cardiac profile.
You should also adjust your daily routine: sleep duration – 8-10 hours, timely meals, walks in the fresh air. In addition, daily blood pressure monitoring is recommended. So, if it decreases from the norm, the development of hypotension can be suspected.
Arterial hypotension (hypotension): causes, symptoms, diagnosis, treatment
Hypotension has traditionally received less attention than hypertension: it is believed that much fewer people suffer from this pathology, and its consequences are not so threatening to health. In fact, the deterioration in quality of life with arterial hypotension can be noticeable, so this disease cannot be ignored.
What is arterial hypotension and what are the types?
This term refers to a persistent (lasting significant periods of time) decrease in blood pressure, reaching 20 percent or more below nominal values. In practice, this is less than 90/60 mmHg. Art.
Classification according to ICD 10
According to the ICD-10 classification of diseases, arterial hypotension belongs to a separate category of diseases with code 195.
Within this category, there is a breakdown into several subtypes of hypotension:
- 0 – idiopathic;
- 1 – orthostatic;
- 2 – medicinal;
- 9 – unspecified;
- 8 – other forms.
Acute arterial hypotension
The acute form of hypotension, characterized by a rapid decrease in blood pressure, is considered the most dangerous.
A sharp decrease in blood flow can negatively affect all organs, especially the brain, which is the largest consumer of blood.
Oxygen starvation can cause fainting, arrhythmias and other health-threatening conditions that require immediate response from the patient or others.
The reasons for a sharp drop in blood pressure (blood pressure) can be different - banal food/chemical poisoning, infections, blood poisoning, dehydration.
Chronic hypotension
Prolonged or constant decrease in blood pressure is the main sign of chronic hypotension.
But if for some categories of the population (trained athletes, residents of high mountains, inhabitants of northern territories) such a condition is an adaptation of the body, considered the norm, then for others it is an abnormal condition. It is characterized by a permanent loss of strength, which does not allow one to work at full capacity in the professional field and in everyday life.
Primary arterial hypotension
This form of pathology is the most common, although the reasons for its occurrence are not fully understood.
It is known that reliably significant prognostic factors for the formation of the primary (essential) form of hypotension are prolonged stress, poor heredity, and the development mechanism is associated with vascular dysfunction. It is important to identify such cases in time to prevent them from progressing into a chronic form.
Secondary hypotension
If primary hypotension is considered an independent disease, then the secondary form is a consequence of other systemic diseases:
- pathologies of the cardiovascular system (cardiovascular system);
- osteochondrosis of the spine (cervical spine);
- previous brain injuries;
- diseases of the gastrointestinal tract (gastrointestinal tract);
- respiratory diseases;
- diabetes;
- malignant/benign neoplasms;
- circulatory dysfunction;
- alcoholism;
- the result of long-term use of medications.
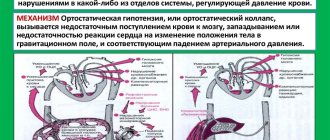
Orthostatic hypotension
As a rule, this is a short-term decrease in blood pressure when standing up (in the general case, when the body moves from a horizontal to a vertical position). People suffering from this form of the disease are at risk of falling and fainting, so they should move into a vertical state (stand up, jump up) with caution.
The etiology of hypotension is quite diverse. Let us list the main factors that provoke the development of low blood pressure:
- CVS pathologies: arrhythmias, atherosclerosis, HF (heart failure), significant aortic valve stenosis.
- Gastrointestinal diseases: stomach ulcers, gastritis, intestinal intoxications.
- Dysfunctions of the immune system: vitamin deficiency, autoimmune diseases.
- Pathologies of a neurological nature: neuroses, vegetative-vascular dystonia, chronic physical/mental fatigue, depression.
- Other systemic diseases: hepatitis, osteochondrosis of the spine, allergic reactions, endocrine pathologies, rheumatism, sepsis, previous spinal cord/brain injuries, anaphylactic shock, burns of 2nd degree and higher.
- Reasons for the adaptation plan (moving to an area with a cold, humid, high-mountain climate).
- Pregnancy period.
- Genetic predisposition.
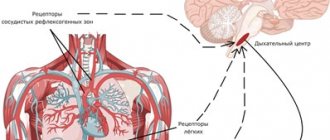
Formation mechanism
Despite the large list of reasons leading to a short-term or persistent decrease in blood pressure, the development of hypotension occurs according to a scenario consisting of four different options:
- decreased stroke/minute ejection rate of the left ventricle;
- a general decrease in the volume of blood circulating in the cardiovascular system;
- decreased venous tone;
- drop in peripheral blood vessel resistance.
A decrease in ejection fraction is typical for patients who have had a heart attack or have a history of other cardiac pathologies.
A decrease in peripheral vascular tone usually occurs against the background of anaphylactic shock and infectious-toxic collapse. The cause of the CBV (circulating blood volume) is internal/external bleeding.
Pleurisy/ascites are the main factors in the development of hypotension due to a decrease in the volume of venous blood returned to the heart.
Symptoms
The most reliable sign of arterial hypotension is a blood pressure value less than 90/60.
Unfortunately, when the condition worsens, it is not always possible to measure blood pressure using a tonometer, so it is important to know the external symptoms of the disease:
- fatigue, apathy, permanent state of general weakness;
- long lasting dizziness;
- pale skin;
- headaches in the temporal, frontal, occipital regions;
- darkening of the eyes, tinnitus;
- fainting;
- pain in the heart area;
- absent-mindedness, sclerosis, memory impairment;
- problems with potency;
- increased sweating;
- temperature drop to 36 degrees;
- disruptions of the menstrual cycle;
- dyspeptic symptoms (nausea, feeling of heaviness in the abdomen, vomiting);
- yawning (a consequence of oxygen deficiency).
The course of the disease is characterized by different degrees of severity.
I degree – moderate, characterized by rare (1 time/day or less) attacks. With grade II hypotension, a drop in blood pressure can occur several times a day; grade III is a severe form with multiple attacks. Mild/moderate forms of the disease are treatable with adequate drug therapy; severe hypotension is considered stable and rarely completely curable.
Arterial hypotension in children
Low blood pressure in children is quite common, especially in adolescence, and the development of pathology may be caused by the following factors:
- past infectious diseases;
- overwork;
- hormonal changes in the body;
- nutritional imbalance.
As in adults, a decrease in blood pressure in children is accompanied by dizziness, frequent headaches, memory impairment, absent-mindedness, and sudden changes in mood.
A prerequisite for normalizing the condition is the correct daily routine, proper sleep, reducing the intensity of physical activity, a balanced diet, and the exclusion of any unfavorable factors.
A persistent decrease in blood pressure during pregnancy develops against the background of a double load experienced by the systems and organs of the expectant mother. Hypotension is caused by additional blood circulation to the fetus and vasospasm caused by a hormonal surge.
As a rule, hypertension appears towards the end of the first trimester and is either asymptomatic or accompanied by fatigue, irritability, loss of appetite, and sometimes heart pain and nausea.
Diagnostics
The most important factor in making a correct diagnosis of hypotension is collecting the patient's medical history. Diet, past illnesses, daily routine and habits, taking medications - this information will help determine the causes of the development of hypertension.
The main method for diagnosing hypotension itself is measuring blood pressure. To determine the degree of advanced disease, it is advisable to use the method of daily blood pressure measurement. Since the symptoms of the pathology are similar to some cardiovascular diseases, an ultrasound of the heart may be prescribed.
As a rule, they try to treat hypotension of I-II degrees of severity without the use of drug therapy, especially if the patient belongs to the category of children/adolescents or pregnant women.
Regardless of age, the patient is recommended to normalize their daily routine, ensure proper rest, a healthy, nutritious diet, and should limit physical activity.
The daily menu should include foods with a high content of microelements and vitamins. It is allowed to drink 2-3 cups of coffee/day; tonic drinks and foods can have the same effect.
For severe hypotension, medications with active substances that increase blood pressure (midodrine, caffeine, ephedrine) are prescribed.
Fainting: first aid
A sharp decrease in blood pressure is fraught with unpleasant consequences such as fainting. In such cases, the patient should be placed on his back, the lower limbs should be elevated, ensuring a greater flow of blood to the brain.
Clothes that restrict breathing should be removed and fresh air should be provided (open a window/door or take the patient outside).
Sprinkle cold water on your face and let it breathe for a few seconds with cotton wool soaked in an ammonia solution.
If the pulse is faintly noticeable and heartbeats can hardly be heard, call an ambulance. Read more about how to provide first aid for hypotension here.
Medications
As noted above, drug therapy for hypotension is used only in advanced cases. The main groups of drugs designed to normalize blood pressure:
- cerebroprotective drugs (actovegin, stugeron, cinnarizine);
- nootropics (nootropil, lucetam);
- antioxidants (beta-carotene, succinic acid);
- anticholinergics (platifilin, amizil);
- tranquilizers/antidepressants;
- vitamin complexes (A/E/B).
When blood pressure is critically low, vasoconstrictors (phenylephrine), glucocorticoids (prednisolone, hydrocortisone), cardiotonics (amlodipine, dobutamine) are administered intravenously.
Physiotherapeutic procedures
To normalize blood pressure, improve myocardial functioning, and increase vascular tone, the following physiotherapeutic procedures are prescribed, characterized by a pronounced tonic effect:
- electrophoresis with potassium/novocaine solution;
- microwave therapy;
- diadynamic therapy;
- ultraviolet treatment;
- turpentine/carbon dioxide/oxygen baths;
- rain shower;
- reflex massage.
: how to deal with low blood pressure
How to cope with arterial hypotension using available remedies at home:
Folk remedies
It is possible to avoid attacks of low blood pressure at home, but such treatment cannot be carried out without consulting a doctor.
Good results can be achieved by drinking a cup of coffee with lemon juice and honey after each meal. Chinese lemongrass tincture also increases blood pressure.
To prepare a folk remedy, pour the crushed berries of the plant with alcohol or vodka (take 10 parts of liquid for 1 volume of lemongrass), leave for 15 days, take before meals (dilute 30 drops of tincture in a tablespoon of water).
You can also add ginger powder to tea (0.5 teaspoon of powder per glass of tea), take after meals for 20 days.
Low blood pressure fees
Many hypotensive patients use tinctures prepared from herbal preparations to treat high blood pressure. The principle of their preparation is approximately the same: pour two tablespoons of herbs into a two-liter thermos, pour two glasses of boiling water, leave for 10-12 hours. Take 50 mg three times a day for 30-60 days.
Examples of fees:
- St. John's wort, milkweed, Echinops, chicory, dandelion, Leuzea, licorice, juniper fruits (in the ratio 3:2:2:2:2:2:3:1);
- speedwell, St. John's wort, wormwood, sage, watch, immortelle, tansy, chicory, dandelion, elecampane (in the ratio 2:5:1:3:4:2:2:1:1:1);
- tartar, nettle, horsetail, birch leaves, mint, strawberries, currants, dandelion, elecampane, rose hips (in the ratio 10:2:2:4:1:2:2:4:1:6).
Prevention
The best way to prevent hypotension is an active lifestyle. A balanced diet, regular physical activity (exercise, going to the gym), and proper rest will help normalize blood pressure.
To strengthen vascular tone, water procedures are recommended: contrast showers, swimming.
Positive emotions, lack of stress, psychotherapy for depressive and hypochondriacal conditions will also help prevent the occurrence of hypotension.
Forecast
A non-critical decrease in blood pressure, even in a chronic form, does not pose a serious threat to the patient’s health, but in most cases this pathology is provoked by other ailments, so we should talk about the prognosis in the context of the complications that these diseases are fraught with.
But symptoms of hypotension such as fainting can also cause injury if you fall. A persistent decrease in blood pressure, as well as hypertension, are conditions that can rarely be completely cured, but they can and should be kept under control by regularly visiting your doctor.
Source: //serdce.biz/zabolevaniya/ard/gipotoniya/arterialnaya-gipotenziya.html
What are the dangers of drug-induced hypotension?
A decrease in blood pressure while taking medications is dangerous due to the development of severe complications. The fact is that, unlike chronic hypotension, with drug-induced hypotension, blood pressure decreases quite quickly and for a long time - until the metabolism of the drug taken occurs. In itself, a slight decrease in pressure is not dangerous and does not threaten health, however, with drug-induced hypotension, the pressure can drop to critical values.
When the pressure drops below 80 mmHg. brain tissue experiences oxygen deficiency. This leads to hypoxia.
Hypoxia is especially dangerous for elderly patients, as it can cause the death of brain neurons, which provokes the development of dementia.
With a sharp decrease in blood pressure, the patient may lose consciousness. Fainting may be accompanied by a fall and injury.
When the pressure is below 60 mmHg. disturbances occur in the functioning of the brain and myocardium. Pressure drop to 50 mmHg. and below can cause the development of coma.
A sharp decrease in blood pressure can lead to the development of a stroke due to cerebral hypoxia due to circulatory disorders.
Prolonged oxygen deprivation of the brain leads to the gradual death of its parts
How to prevent the development of drug-induced hypotension?
To prevent the development of drug-induced hypotension, it is necessary to influence the cause of this disorder - taking medications. Any new drug recommended to a patient must be started with a minimum therapeutic dose. This allows you to analyze the body's response to a new drug.
If it is necessary to take tranquilizers and antipsychotics, preference is given to a drug with a mild effect. It is better to choose daytime tranquilizers that do not suppress the activity of the nervous system.
Related Articles
Hypotension: causes, symptoms, medications and alternative treatment
Hypotension during pregnancy: why is it dangerous and how to treat?
Causes and treatment of hypotension in a child
Paroxysmal atrial fibrillation: clinical picture, diagnosis, treatment, emergency care
VSD of the hypertensive type: ICD code, symptoms and treatment
Muscle hypotonia in children (newborns) and adults: symptoms, complications and treatment
Medication
A person suffering from low blood pressure must realize that hypotension is not an independent illness, but the result of the effects of other diseases on the body.
The main principle of treatment of secondary type hypotension is treatment of the underlying pathology, which is as follows:
- If the cause is an endocrine disease, then long-term use of hormonal drugs will be required.
- Anemia can be treated with medications containing iron and other vitamins. Taking appropriate medications should only be done after receiving medical prescriptions.
- If a patient is diagnosed with a heart defect, he may be offered surgery. Low blood pressure is often due to aortic insufficiency. A similar situation is observed with mitral valve stenosis.
Many drugs for increasing blood pressure include caffeine, which can quickly increase the readings on the device and normalize the hypotensive state. Before taking, you need to agree on the instructions for using the tablets with your doctor.
Drug-induced hypotension, which has a code according to ICD-10 No. 195, can be cured with medications, but you cannot select medications yourself.
Other types of disease
Code I95.8 is assigned to the section “Other types of hypotension” and, according to the ICD, includes chronic hypotension. This broad concept covers 2 forms of chronic hypotension:
- primary;
- secondary.
The first occurs as an independent disease for a number of reasons that correlate with a violation of blood pressure regulation systems in the body.
The following have a chronic course:
- congenital hypotension;
- AGT in trained people;
- adaptive hypotension of residents of high mountain regions, the Arctic, or tropical latitudes.
This is usually a physiological condition that does not cause severe symptoms.
Secondary (pathological) hypotension is always a symptomatic manifestation or consequence of other diseases:
- myocarditis, defects, heart attack and other heart pathologies;
- diseases of the endocrine glands;
- anemic conditions and other blood diseases;
- obstructive jaundice, hepatitis and other liver pathologies;
- lobar pneumonia and other lung lesions;
- brain diseases;
- intoxications of external and internal nature.
Physiotherapy
In order to normalize blood pressure and improve the tone of the body as a whole, along with drug treatment, properly selected physiotherapy is prescribed:
- Electrosleep therapy.
Affects the central nervous system with low-frequency impulses. An electric current passes through the eye sockets into the area of the skull. It acts on serotonergic neurons.
Due to increased production of serotonin, the emotional and reflex functionality of the brain decreases. In other words, the person falls into a restful sleep. In addition, the procedure helps improve recovery processes, blood flow and breathing.
- Aeroionotherapy.
You can influence the body with air saturated with ions. This procedure leads to normalization of the respiratory tract and improvement of vascular tone.
Arterial hypotension ICD 10
CHAPTER 21 ARTERIAL HYPOTENSION AND SYNCOPAL CONDITIONS
Arterial hypotension (Ht) is determined by the level of blood pressure, which with repeated measurements is less than 100/60 mm Hg.
Primary arterial hypotension (PAT) in ICD 10 is classified under heading 195.0 - idiopathic hypotension. Ag with a specified etiology refers to chronic Ag (195.8 according to the ICD). The clinical picture of PAT is dominated by complaints of palpitations, irregularities and pain in the heart area, there are autonomic disorders and, in 1/3 of the patients, orthostatic hypotension (OH).
OT is manifested by a decrease in systolic and diastolic blood pressure by 20/10 mmHg. and more when getting up from a lying position. Patients with OT are prone to syncope (SS). SS is a syndrome of sudden short-term loss of consciousness with impaired postural tone and complete reversibility of the condition. There are neurogenically caused, reflex, dyscirculatory fainting and SS in somatogenic diseases. The diagnosis of OT and SS is based on anamnesis, instrumental studies and orthotest. To prevent and treat these syndromes, tilt training, wearing elastic stockings, a diet with a high salt content of up to 20 g/s, and fludrocortisone are used. To prevent vasovagal SS, Relanium, anaprilin or atenolol, teopek, midodrine, and mineralocorticoids are used. For sinocarotid SS, midodrine and fludlocortisone are used. In case of cardiac inhibitory variants of CV, a pacemaker is implanted. In patients with long QT syndrome and Brugada syndrome, a cardioverter is used. Prevention of SS in somatogenic diseases depends on the successful treatment of the latter. Key words:
arterial hypotension, orthostatic hypotension, syncope.
Arterial hypotension (ICD-10 code: I95)
Characterized by systolic pressure below 100 mmHg. Art. and diastolic pressure - below 60 mm Hg. Art.
Pages
I95.2 Drug-induced hypotension (drug-induced hypotension)
Taking medications that lower blood pressure: nitrates (especially in combination with alcohol, Viagra), ACE inhibitors, beta blockers, diuretics, etc. A decrease in SBP by 20% or more from the age norm.
ICD 10 diagnosis tree
An alphanumeric system is used to code diseases. Arterial hypotension is called hypotension. It has the following codes:
- 195.0 – idiopathic pathology;
- 195.1 – orthostatic (but not neurogenic);
- 195.8 – chronic disease;
- 195.9 according to ICD 10 – unspecified hypotension.
The list also includes drug-induced hypotension, referred to as 195.2. This pathology appears after the use of certain medications.
Diagnostics
The cardiologist will first interview and examine the patient in order to look for ailments that have caused the blood pressure to drop. May be prescribed:
- Echocardiography, both during exercise and daily monitoring;
- Doppler echocardiography;
- Electroencephalography;
- Orthostatic test
- Blood tests for lipid fractions, glucose levels, cholesterol and electrolytes.
To determine the exact level of pressure, the doctor measures blood pressure three times with an interval of 3-5 minutes.
It is also important to conduct 24-hour blood pressure monitoring.
In addition to the cardiologist, you may also have to undergo:
- ophthalmologist;
- neurologist;
- endocrinologist.
Read below about how to treat manifestations of arterial hypotension.
What are the dangers of possible complications?
A pathology such as drug-induced hypotension often leads to serious complications. Compared with the chronic degree of the disease, in this case blood pressure decreases very quickly.
Low indicators are alarming until the drug taken from the body, which has such an effect, is removed from the body.
A slight drop in pressure does not pose a health hazard. But if we are talking about drug-induced hypotension, the parameters can drop to a critical state.
If the number on the tonometer is below 80, less oxygen enters the brain tissue, as a result of which hypoxia is diagnosed. Hypotension is dangerous for older people. It can trigger the death of neurons, which leads to dementia.
A sharp drop in blood pressure can cause loss of consciousness. If you suddenly faint, there is a risk of injury during a fall.
When pressure parameters drop below 60, the brain and myocardium cease to function normally. If the readings drop to 50, the person may fall into a coma.
Sometimes a sharp drop in pressure becomes a provoking factor for a stroke. This happens against the background of oxygen starvation of the brain and deterioration of blood flow.
Pathogenesis
Muscle hypotension, whatever its etiology, develops under the influence of general pathophysiological mechanisms. Muscle tone is regulated by the structures of the brain stem, the striopallidal system and the cerebellum, and the implementation of tonic reactions depends on the activity of the formations of the segmental reflex apparatus, which includes:
- alpha and gamma neurons of the anterior horns of the spinal cord;
- motor and sensory fibers of nerve trunks;
- afferents of neuromuscular spindles.
Diffuse muscle hypotonia can occur as a result of:
- disorders of suprasegmental regulation of motor neurons (alpha and gamma);
- hypofunction of spinal alpha motor neurons;
- denervation, which occurs when the fibers of the nerve trunks are damaged;
- increasing the activity of mediator inhibitory mechanisms;
- ion channel pathologies;
- muscle cytoskeletal disorders;
- decrease in energy supply to muscle tissue.
Symptoms and signs
Arterial hypotension, as a rule, is manifested by general weakness, increased fatigue, and decreased concentration.
Table 2. Possible symptoms of hypotension
| Sign | Description |
| Mood changes | The person becomes irritable, emotionally unstable, sometimes apathetic |
| Drowsiness, lack of energy | It is especially difficult for hypotensive patients in the morning. |
| Meteosensitivity | Changes in atmospheric pressure can negatively affect your well-being |
| Head pain, dizziness | A clear sign of hypotension is a headache, usually localized in the temples or crown. The nature of the sensations is dull, squeezing, sometimes pulsating |
| Sweating, impaired thermoregulation | Hypotonicity can cause cold sweats, hands and feet remain cold even on a warm day |
| Fainting | Loss of consciousness can be caused by high ambient temperatures and stuffy rooms. Late consumption of food or lack of sleep increases the likelihood of fainting. |
Pallor of the skin, nausea, heart rhythm disturbances, etc. are detected. The symptoms of hypotension in women and men are identical. However, representatives of the fair sex may experience a deterioration in their condition during menstrual periods.
Principles of treatment of hypotension
To alleviate the condition, complex therapy is usually used. Its components depend on the causes of hypotension in men and women. The following principles exist:
- Taking pharmacological agents. What to take for hypotension to increase blood pressure is determined exclusively by a specialist.
- Lifestyle changes. With low blood pressure, adequate sleep, a healthy diet, and adherence to physical activity play an important role.
- Getting rid of irritants. Positive emotions are recommended.
Symptoms of drug-induced hypotension
In the international classification of diseases ICD-10, drug-induced hypotension is included in the list of hypotonic disorders. Symptoms of drug-induced hypotension completely repeat the symptoms of a decrease in blood pressure caused by any other reasons. These include:
- decrease in pressure below 100 by 60 mm Hg;
- drowsiness;
- prostration;
- dizziness;
- headache;
- bradycardia;
- disorientation;
- nausea and vomiting;
- fainting.
With a sharp decrease in blood pressure, blurred vision and tinnitus may occur. A person loses support and may fall and lose consciousness.
Low blood pressure headaches resemble migraines. This is a throbbing pain in one part of the head, mainly from the left or right temple.
With drug-induced hypotension, a slowing of the pulse is noted. A decrease in heart rate below 59 beats per minute is called bradycardia. This condition is accompanied by loss of strength, dizziness, and lack of air. With hypotension, chills of the extremities, pale skin, and cold sweat are observed.
In particularly severe cases, hypotension may cause renal failure. This occurs when taking large doses of drugs that lower blood pressure.
If blood pressure drops rapidly, a person may lose consciousness
Forms of arterial hypotension
Depending on the form, hypertension is usually divided into
- Spicy;
- Chronic, which in turn is divided into: Primary;
- Secondary.
It is worth talking about each of the forms separately:
- The acute form of hypertension is characterized by hypoxia, that is, a decrease in the supply of oxygen to the brain, and with it important organs. It occurs in acute circulatory failure, infection, severe poisoning and some other ailments. Its characteristic symptom is a sharp drop in blood pressure. This symptom often accompanies pulmonary embolism, heart attack, allergies, and arrhythmic disorders.
- Chronic , or as it is also called physiological hypotension, can occur due to poor heredity, as well as in trained athletes. At a young age, it worsens the quality of life, and at an older age it can increase the risk of cardiovascular complications.
- Primary hypotension (also idiopathic/essential) is an independent disease. It is believed to be a form of neurosis-like disease of the vasomotor centers of the brain.
- Secondary hypertension appears against the background of other ailments (eg osteochondrosis, rheumatism, stomach ulcers, anemia, arrhythmias, diabetes, various diseases of the endocrine system, etc.).
Often, in addition to acute and chronic forms of arterial hypotension, a third one is identified - with severe orthostatic syndrome.
How dangerous is hypotension and how to treat it correctly
Hypotension is gaining more and more attention due to its widespread prevalence. Pathology is usually found in young people whose age ranges from 20 to 30 years. The chronic form of the disease is found predominantly in women (estimates have a fairly wide range, reaching up to 39% in the upper limit). Men suffer from low blood pressure less often - up to 15% of all representatives in the population.
The pathology leads to a deterioration in general well-being, decreased performance, and rapid fatigue. However, in some cases, hypotension does not have negative consequences for a person. What the disease is, what measures should be taken and in what cases, as well as what consequences the pathology is fraught with, we will consider in the article.
What it is?
The pathology is also known as arterial hypotension. The word “hypotension” has ancient origins, and translated from Greek means “tension below.”
There are acute and chronic forms of the disease. They have similar manifestations, but develop differently from each other. In turn, chronic hypotension is divided into:
Primary hypotension is an independent pathology, but what exactly leads to its appearance is not known for certain. Presumably it is a neurosis-like disorder that arose against the background of regular stress. The secondary form is a consequence of other diseases. For example, damage to the cardiovascular, endocrine, respiratory or other body systems.
Codes according to ICD 10
Since 1989, an alphanumeric system has been used to code pathologies. It was approved at a congress held in Switzerland and was called the International Classification of Diseases, Tenth Revision. The paper edition includes three volumes, divided into different topics.
Arterial hypotension according to ICD 10 is called hypotension, and has the following codes:
- idiopathic – I95.0;
- orthostatic (except neurogenic) – I95.1;
- chronic hypotension ICD 10 code – I95.8;
- unspecified – I95.9.
Also in ICD 10, drug-induced hypotension is identified; it has code I95.2. This is a pathology caused by the use of pharmacological drugs. To clarify the class of tools used, their identification using an additional code is allowed.
Causes of low blood pressure
Low blood pressure is a consequence of a variety of factors. Treatment of hypotension directly depends on the causes that led to the development of the pathology.
Table 1. What causes arterial hypotension
Description
Hypotension (hypotension) is a violation of vascular tone. In a healthy person, the narrowing and dilation of blood vessels occurs quite quickly. In hypotensive patients, this reaction is slowed down, which leads to poor blood circulation and insufficient oxygen saturation of the brain, heart and other organs.
The mechanism of development of hypertension is associated with one of the factors:
- the volume of blood circulating in the body decreases sharply (during bleeding);
- reduction in stroke and cardiac output (diseases of the cardiovascular system);
- decline in venous blood flow (in case of heart attack, arrhythmia);
- deterioration of tone and resistance of peripheral vessels (a consequence of an allergic reaction or infection).
In pregnant women, it may occur due to the release of hormones that reduce vascular spasm or due to the creation of an additional circulation and increased load on the heart.
Important! Hypotension can lead to oxygen starvation of the fetus, which can subsequently affect the development of the baby. .
Reasons for development
Only a comprehensive medical examination can establish the exact cause of the development of hypotension in a child. Most often, muscle hypotonia syndrome in a newborn indicates the presence of congenital diseases that can manifest themselves during the first six months of life. The most common causes of hypotension are genetic diseases:
- Down syndrome is a genomic pathology in which in most cases, instead of the normal 46 chromosomes, the karyotype contains 47 due to an extra copy of chromosome 21.
- Aicardi syndrome is a rare congenital disease of unknown etiology, which is characterized by epileptic seizures of the infantile spasm type, partial or complete absence of the corpus callosum, chorioretinal lacunar lesions and mental retardation.
- Robinow syndrome is a rare disease that is inherited in an autosomal dominant and autosomal recessive manner. Patients are born with prenatal hypoplasia and are distinguished by the presence of macrocephaly, a protruding forehead, a wide bridge of the nose, and other clinical signs.
- Opitz-Kavedzhia syndrome (FG syndrome) is a rare recessive X-linked disease characterized by significant variability in clinical signs (osseous-facial abnormalities, severe muscle hypotonia, etc.).
- Martin–Bell syndrome, which is caused by a mutation in the FMR1 gene on the X chromosome. As a result of suppression of transcription of the FMR1 protein, the normal development of the nervous system is disrupted (mental retardation, incoordination of movements, and slight hypotension are observed).
- Griscelli syndrome (type 1) is an autosomal recessive disease characterized by combined immunodeficiency and partial albinism.
- Marfan syndrome is a hereditary connective tissue pathology that is inherited in an autosomal dominant manner. This syndrome is characterized by elongated tubular bones of the skeleton, hypermobile joints, and pathology of the cardiovascular system and visual organs.
- Patau syndrome is a chromosomal disease associated with the presence of an additional chromosome 13 in cells and is accompanied by severe developmental defects.
- Leigh syndrome is a rare hereditary neurometabolic syndrome characterized by central nervous system lesions.
- Prader-Wili syndrome is a rare disease caused by the loss of the paternal copy of chromosome 15q11-13.
- Williams syndrome is a disease caused by chromosome rearrangements. Patients are distinguished by a specific appearance and general mental retardation combined with the development of certain areas of intelligence.
- Rett syndrome is a neuropsychiatric disease that occurs mainly in girls and is manifested by severe mental retardation.
- De Morcière syndrome (septo-optic dysplasia) is a heterogeneous disease in which hypoplasia of the optic nerve, pituitary gland and abnormalities of the midline structures of the brain are observed.
- Riley-Day syndrome (familial dysautonomia), which is caused by mutations in Q319 and is transmitted in an autosomal recessive manner. The syndrome is characterized by sensory disturbances and disorders of the autonomic nervous system.
- 22q13 deletion syndrome (loss of part of a chromosome), which is characterized by neonatal hypotonia, mental retardation and mild dysmorphic features.
- Ehlers-Danlos syndrome is a heterogeneous disease that affects the joints and skin.
- Canavan disease, which is characterized by progressive damage to nerve cells in the brain.
- Dejerine-Sotta disease is an autosomal recessive inherited disease in which hypertrophic changes in the Schwann sheath of nerve fibers, compression and degeneration of axons, and a slow increase in peripheral paresis and muscle atrophy are observed.
- Krabbe disease is a rare autosomal recessive disease characterized by damage to the myelin sheath of nerve fibers and a progressive decline in intelligence and vision.
- Niemann-Pick disease, in which lipid metabolism is disrupted. The symptoms of the disease depend on its type.
- Tay-Sachs disease, which manifests itself as progressive damage to the central nervous system.
- Centronuclear myopathy, which is characterized by generalized muscle weakness and ophthalmoplegia, respiratory distress syndrome and other signs.
- Achondroplasia, which is manifested by the presence of congenital anomalies (spinal stenosis, etc.) and underdevelopment of long bones.
- A disease of the central core, which is characterized by delayed motor development and disorders of the musculoskeletal system.
- Pituitary dwarfism, manifested by significant retardation in growth and physical development.
- Menkes disease, the symptoms of which are slow growth, pathologies of the nervous system and characteristically curled hair.
- Spinal muscular atrophy, in which voluntary movements are impaired (pathological processes mainly affect the striated muscles of the legs, head and neck), and mental development does not deviate from the norm.
- Deficiency of 3-methylcrotonyl-CoA carboxylase, in which the child quickly gets tired, muscle tone is weakened, and diarrhea, vomiting and malnutrition are often observed.
- Methylmalonic acidemia, in which there is a delay in mental and physical development, and methylmalonic acid is present in the urine.
- Non-ketotic hyperglycinemia, which in the classical course of the disease develops rapidly and is manifested by lethargy, myoclonic seizures, and episodes of apnea. Surviving children have severe delays in psychomotor development and seizures.
- Myotonic dystrophy, which is characterized by variability in clinical manifestations. It is distinguished by the presence of myotonia, progressive muscle weakness, heart damage, endocrine-vegetative disorders, the presence of cataracts and decreased intelligence. With Becker's myodystrophy, muscle hypotonia often manifests itself in adults, since this form of the disease is more benign and manifests itself at the age of 10-20 years, and sometimes later.
Muscular hypotonia in infants can be a consequence of developmental defects:
- congenital cerebellar ataxia, in which a “drunk gait”, asynergia, ataxia in the hands, etc. are observed;
- sensory integration dysfunction;
- dyspraxia (movement disorders);
- congenital hypothyroidism;
- hypotonic cerebral palsy;
- teratogenesis, which arose as a result of intrauterine intoxication with benzodiazepines.
Muscle hypotonia can be a consequence of diseases that appear throughout life. Such diseases include:
- muscular dystrophy (observed most often);
- metachromatic leukodystrophy;
- spinal muscular atrophy;
- encephalitis, meningitis, poliomyelitis, Guillain-Baré syndrome, sepsis;
- childhood botulism, which develops under the influence of botulinum toxin produced by the spore-forming bacillus Clostridium botulinum;
- myasthenia gravis;
- pathological reactions to vaccination;
- celiac disease;
- hypervitaminosis;
- kernicterus;
- rickets;
- Sandifer syndrome, which is characterized by a triad of symptoms: hiatal hernia, reflux esophagitis and torticollis.
Muscle hypotonia in children also develops with asphyxia during childbirth, mercury poisoning, traumatic brain injury, damage to lower or upper motor neurons, dysfunction of the central nervous system (damage to the cerebellum, cerebral palsy, etc.) and hypothyroidism.
Features of the disease
Arterial hypotension (HTN) is characterized by low blood pressure (less than 95/60 mm Hg for women and 100/60 for men), that is, 20 percent lower than normal values. And although with hypotension there is not such a high probability of myocardial infarction or stroke than with its opposite (hypertension), it can bring a lot of inconvenience to the patient (for example, constant weakness).
According to ICD-10, arterial hypotension has its own code: I95.
As for the manifestation of the disease during pregnancy, hypertension most often manifests itself in the first trimester (at the end), rarely at 17–24 weeks of pregnancy. Often the disease is asymptomatic, but still threatens complications for both the baby and the mother.
In children, hypotension is most often accompanied by headaches and often dizziness. Often the disease becomes.
A specialist talks about the features of arterial hypotension in the video below:
Symptoms
Diffuse muscle hypotonia syndrome manifests itself:
- In varying degrees of muscle hypotonia (from mild lethargy to complete atony). The muscles are soft and flabby to the touch, there is hyperextension in the joints (knees, elbows, wrists), resistance to passive movements decreases.
- Decreased or complete absence of unconditioned reflexes and active movements, increased tendon reflexes. The child is unable to maintain a posture, crawl, or stand as a result of muscle mismatch.
- Feeding difficulties and, in some cases, gastroesophageal reflux, in which stomach contents back up into the esophagus.
- Breathing disorders due to cerebral hypotension.
Diffuse muscle hypotonia syndrome in children may be accompanied by convulsions, delayed development of the child, dysmorphic signs, clonus (fast and rhythmic movements) of the feet, and involvement of internal organs in the pathological process.
The severity of symptoms is influenced by the patient's age, severity of hypotension, location of the lesion, and cause of hypotension.
Causes
The pathological condition develops during treatment with certain therapeutic drugs. For example, diuretics have a diuretic effect.
When they are consumed, excess fluid is removed from the body and sodium is washed out. Medicines in this group are often prescribed for the treatment of heart disease, genitourinary system and high blood pressure.
Other groups of medications can also lower blood pressure. They are recommended to be taken if the readings on the tonometer are too high.
Causes
Diseases of the cardiovascular system involve the use of medications that help lower blood pressure. Their incorrect use entails a complication such as drug-induced hypotension. The following groups of drugs have such an effect on the body:
- diuretics;
- ACE inhibitors;
- sartans;
- calcium channel blockers;
- beta blockers;
- centrally acting drugs;
- nitroglycerine.
An overdose of a drug from one of the above groups can lead to a sharp decrease in blood pressure, which will negatively affect the general condition of the body, and can also cause certain complications.
Important to remember! You should strictly adhere to the dosage of medications prescribed by your doctor! This will help avoid drug-induced hypotension.
Treatment
If there are obvious external signs of a hypotonic attack, it is necessary to provide the patient with emergency assistance:
- put it in a horizontal position;
- rub your ears (this will improve blood flow);
- give a glass of water.
An integrated approach is used to treat chronic forms of hypotension.
Medication
All drugs prescribed for hypotension are based on caffeine. With its help, it is possible to quickly raise low blood pressure and normalize the patient’s condition. The following medications are used for this:
- Hydrocortisone acetate;
- Askofen;
- Sedal-M;
- Citramon;
- Saridon.
Physiotherapy
To stabilize blood pressure and maintain body tone, physiotherapeutic procedures are recommended in combination with drug treatment.
- Electrosleep therapy is the effect of low-frequency (1-150 Hz) pulsed current on the central nervous system. Currents penetrate the skull through the eye sockets (special glasses are used) and affect serotonergic neurons. Serotonin reduces the emotional and conditioned reflex activity of the brain, thereby inducing a state of sleep. Electrosleep enhances redox processes, and also improves blood circulation and minute breathing volume.
- Aeroionotherapy (aeroinhalation) is the effect of ionized air on the body. It acts through respiratory tract receptors and saturates the body with useful elements.
ethnoscience
You can increase blood pressure at home using special herbal tinctures:
- immortelle - improves sleep, normalizes vascular tone;
- Radiola rosea - activates the activity of the central nervous system;
- Chinese Schisandra - normalizes blood pressure and improves blood circulation.
Classification according to ICD-10
To ensure the unity of methodological approaches to therapy, all diseases are collected in a regulatory document called the International Classification of Diseases (ICD) under various codes.
Once every 10 years, the World Health Organization revises the classification, making changes in accordance with new discoveries in medicine. Today the ICD 10th revision is used. According to ICD-10, arterial hypotension belongs to class IX “Diseases of the circulatory system”, is in the subclass “Other and unspecified diseases of the circulatory system” and has codes I95.0 - I95.9 depending on the types of the disease. The category of all varieties of AGT is indicated by code I95.
Idiopathic
Code I95.0 is assigned to arterial hypotension that arose as an independent disease. Such AHT is called primary, as well as essential or idiopathic. According to modern data, idiopathic hypotension occurs in 33% of women and 4% of men, which indicates a predisposition of women to this type of AHT.
The literal meaning of the term idiopathic means that it is a condition “without obvious causes”, “unclear”. The diagnostic difficulty of idiopathic arterial hypotension lies in the fact that it is characterized by a long latent (asymptomatic) or mild course. With such a clinical picture, patients prefer not to see a doctor, but to “treat” themselves. This, of course, is the wrong approach, since stimulating well-being using home methods leads to excessive stress in the adaptation (regulation) mechanisms and deterioration in vascular elasticity. Ultimately, this will lead to the inevitable transformation of AHT into “normotension”, and then arterial hypertension.
Orthostatic (postural)
Hypotension, called postural, is characterized by a violation of blood pressure regulation, due to various reasons and manifested by a drop in pressure of 20/10 mm or more when the body position changes from horizontal to vertical. This usually occurs within 3 minutes after changing body position, and if the decrease in blood pressure is significant, the person faints. According to ICD-10, this is - having code I95.1. The name postural comes from the Italian postura (posture), this name reflects the peculiarity of the pathology - it manifests itself when changing posture.
Drug-induced (drug-induced)
ICD-10 code I95.2 is assigned to drug-induced hypotension or drug-induced AHT. Medicines with antihypertensive properties are used in the treatment of cardiovascular and other diseases. The instructions for the use of these drugs warn about a possible strong drop in blood pressure, and the development of arterial hypotension is facilitated by uncontrolled or improper use of antihypertensive drugs (in particular, incorrect selection of dosages). Groups of drugs that have a hypotensive effect:
- beta blockers;
- calcium blockers;
- diuretics;
- ACE inhibitors;
- nitrates (Nitroglycerin);
- sartans and others.
A sharp drop in blood pressure is especially dangerous for patients with cardiovascular and other chronic diseases. Drug-induced hypotension provokes additional health problems:
- impaired renal function;
- increased or, conversely, decreased heart rate;
- various neurological dysfunctions;
- impaired perfusion (blood supply) to the brain.
To avoid the occurrence of this type of arterial hypotension, any drugs with antihypertensive properties should be taken under the supervision of a physician.