Symptoms
Arterial hypertension often occurs without significant symptoms. But with a sharp increase in pressure, the following manifestations may occur:
- headache. Unpleasant sensations may be localized in the temples, the back of the head, or may not have a clear localization;
- nausea with vomiting. An attack of vomiting does not bring relief;
- dizziness and severe weakness, the appearance of spots before the eyes, tinnitus;
- pain in the heart, loss of sensitivity in the limbs, numbness. These signs are observed in severe cases.
There are many reasons why a sharp increase in blood pressure can occur.
Danger of hypertensive crisis
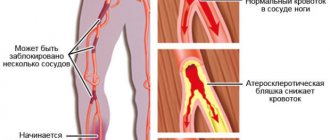
Very often, such a condition requires treatment in a hospital setting, since a hypertensive crisis can provoke serious disorders. High blood pressure is most harmful to the heart and blood vessels. They also cause circulatory problems that are dangerous to the brain. The most vulnerable in this condition are the kidneys and liver. Tissue damage occurs because there is not enough oxygen and nutrients reaching it.
A sharp jump in blood pressure readings can lead to:
- myocardial infarction or cerebral stroke;
- encephalopathy;
- Parkinson's disease;
- decreased intellectual abilities;
- paralysis;
- visual impairment;
- acute renal failure;
- disruptions in liver function;
- cardiovascular failure;
- arterial thromboembolism;
- hypertrophic changes in the ventricles of the heart;
- pulmonary or cerebral edema;
- coronary heart disease;
- aortic aneurysm.
Constant headaches and dizziness are considered a relatively mild complication of the crisis. It is important to remember that severe forms of pathology can cause death.
There are several factors that increase the likelihood of complications. These include a history of diabetes mellitus, coronary artery disease, and increased blood cholesterol levels.
At what pressure should you call an ambulance?
If a person knows what blood pressure parameters are normal and what condition requires medical attention, he will be able to avoid extremely dangerous consequences for his health in time.
As you know, the generally accepted normal indicator is a pressure of 120/80, however, taking into account certain factors, its parameters may fluctuate slightly. These include:
- Gender of a person.
- Physical activity.
- Times of Day.
However, in situations where there is a striking deviation from the acceptable normal parameters - more than 15 units, and is accompanied by characteristic symptoms, which indicates the presence of serious diseases of the heart and blood vessels, there is a risk of developing serious complications. To avoid their occurrence, it is necessary to seek highly qualified medical advice.
At what pressure should you call an ambulance? Cardiologists emphasize that there are no strict recommendations regarding calling the emergency room in case of an increase or decrease in blood pressure. In this situation, the well-being of the sick person plays an important role.
Elderly people and pregnant women should be especially careful about pressure surges:
- For people over 60 years of age, the maximum blood pressure reading is 147/91. If the tonometer shows above 169/95, this is already a critical figure at which it is necessary to call an ambulance.
- If during pregnancy the blood pressure monitor shows a blood pressure level above 150/70, you should call the emergency room. This pressure indicator is fraught with the development of eclampsia, which is dangerous for the expectant mother due to the manifestation of severe symptoms leading to the death of the fetus.
Let us consider in more detail the situations of acute increase and decrease in blood pressure, in which it is necessary to call an emergency team.
High performance
Hypertension is a pathological process in which an increase in arterial levels is diagnosed much greater than 140/90.
In what episodes does an ambulance arrive when you have high blood pressure? Doctors emphasize that if the tonometer records blood pressure no higher than 110/70-139/89, then this is not a critical figure. This indicator of blood condition can be stabilized by proper rest. But if the measuring device shows more than 140/90, measures must be taken to regulate it.
An extremely dangerous situation occurs when the measurement results show a blood pressure level above 169/95. It is necessary to urgently call a doctor - this condition is fraught with stroke and other consequences.
However, emergency medical intervention may be required in such a clinic:
- Hypertensive crisis happened for the first time.
- The medications taken to normalize blood pressure did not give the expected effect. Within an hour after consuming them, the pressure did not decrease.
- With high blood pressure, a person experiences sharp chest pain that cannot be relieved with medication.
- Against the background of a jump in blood pressure, there is a decrease in hearing and vision, a significant loss of motor functions, and numbness of the limbs.
When such factors occur, specialists decide to hospitalize a seriously ill person.
Low performance
Hypotension is diagnosed much less frequently than hypertension, but it can also be dangerous for a person. Hypotonic disease means a blood pressure state below:
- 100/60 in men.
- 95/60 in women.
In most cases, to normalize blood pressure, it is enough for hypotensive patients to rest fully, take a cup of coffee or sweet tea and take a walk in the fresh air.
What should be the value of low pressure at which an ambulance is called? Experts emphasize that if it was not possible to normalize a low blood pressure level, while the tonometer shows that blood pressure has dropped by as much as 20% of its original state, this is considered a reason to urgently call the ambulance.
Algorithm of action in case of sudden increase in blood pressure
With periodic increases in blood pressure, every hypertensive patient should know how to help themselves. If the attack occurs for the first time, the patient may become confused, so his relatives should know what to do in this situation.
First of all, you need to calm down. It is strictly forbidden to be nervous; this can aggravate the situation. Under the influence of emotional experiences, blood pressure may increase even more.
If a hypertensive crisis develops, you should call an ambulance. Before her arrival, it is necessary to normalize the psycho-emotional state. The patient should be seated so that the legs are lower than the body, remove constrictive clothing, provide fresh air, and measure blood pressure.
First aid for high blood pressure may include foot baths. They have the following properties:
- Bring vascular tone back to normal.
- Promote blood flow to the legs.
This allows you to reduce the blood load on the vessels by several points. Hypertensive patients should always have antihypertensive drugs in their medicine cabinet. To reduce the levels, you need to take a tablet of Captopril or Nifedipine, or another medicine prescribed by your doctor.
These drugs act quickly and stabilize systolic and diastolic blood pressure within half an hour. If relief does not occur, you need to take the medicine again. For quick results, the tablet should be placed under the tongue.
Urgent assistance should imply a gradual decrease in indicators. If this is done abruptly, an ischemic stroke may occur. The parameters should stabilize within several hours. During this period, the patient should not make sudden movements: it is better to sit or remain in a horizontal position.
In cases where the crisis is accompanied by severe pain in the chest area, you need to give a Nitroglycerin tablet.
You can get rid of feelings of fear and anxiety and normalize your psycho-emotional state with the help of Corvalol and Valocordin.
Modern methods of treating hypertension
* Additional and “new” risk factors (not taken into account when risk stratification).
Risk levels of hypertension:
Low risk group (risk 1).
This group includes men and women under the age of 55 years with stage 1 hypertension in the absence of other risk factors, target organ damage and associated cardiovascular diseases. The risk of developing cardiovascular complications in the next 10 years (stroke, heart attack) is less than 15%.
Medium risk group (risk 2).
This group includes patients with grade 1 or 2 hypertension. The main sign of belonging to this group is the presence of 1-2 other risk factors in the absence of target organ damage and associated cardiovascular diseases. The risk of developing cardiovascular complications in the next 10 years (stroke, heart attack) is 15-20%.
High risk group (risk 3).
This group includes patients with grade 1 or 2 hypertension who have 3 or more other risk factors or target organ damage.
The same group includes patients with grade 3 hypertension without other risk factors, without target organ damage, without associated diseases and diabetes mellitus.
The risk of developing cardiovascular complications in this group over the next 10 years ranges from 20 to 30%.
Very high risk group (risk 4).
This group includes patients with any degree of hypertension with associated diseases, as well as patients with grade 3 hypertension, with the presence of other risk factors and/or target organ damage and/or diabetes mellitus, even in the absence of associated diseases. The risk of developing cardiovascular complications in the next 10 years exceeds 30%.
Risk stratification for assessing the prognosis of patients with hypertension
| Modern methods of treatment of hypertension Standards of treatment of hypertension Protocols for the treatment of hypertension Modern methods of treatment of arterial hypertension Standards of treatment of arterial hypertension Protocols for the treatment of arterial hypertension Hypertensive disease primarily affecting the heart Hypertensive crisis. Profile: therapeutic. ICD codes: I11.0 Hypertensive (hypertensive) disease with predominant damage to the heart with (congestive) heart failure. Definition: Hypertension (arterial hypertension) – a stable increase in systolic blood pressure of 140 mmHg. or more and/or diastolic blood pressure 90 mmHg. and more. Hypertensive crisis is a sudden increase in blood pressure, accompanied by clinical symptoms and requiring immediate reduction (not necessarily to normal values) to prevent target organ damage. Classification: WHO/IAS 1999 Categories of normal blood pressure: Optimal blood pressure 110 Isolated systolic hypertension >140/ 55 years - women > 65 years • Smoking • Total blood cholesterol level > 6.5 mmol/l • Diabetes mellitus • Family cases of early development of cardiovascular diseases. 2. Other factors that adversely affect the prognosis:* • Reduced HDL cholesterol • Increased LDL cholesterol • Microalbuminuria (30-300 mg/day) in diabetes mellitus • Impaired glucose tolerance • Obesity • Sedentary lifestyle • Increased levels of fibrinogen in the blood • Socioeconomic groups at high risk •High risk geographic region | • Left ventricular hypertrophy (ECG, EchoCG, radiography); • Proteinuria and/or a slight increase in plasma creatinine (106 – 177 µmol/l); • Ultrasound or radiological signs of atherosclerotic lesions of the carotid, iliac and femoral arteries, aorta; • Generalized or focal narrowing of the retinal arteries. | Cerebrovascular diseases: • Ischemic stroke; • Hemorrhagic stroke; • Transient ischemic attack. Heart diseases: • Myocardial infarction; • Angina pectoris; • Revascularization of coronary vessels; • Congestive heart failure. Kidney diseases: • Diabetic nephropathy; • Renal failure (creatinine > 177 µmol/l). Vascular diseases: • Dissecting aneurysm; • Damage to peripheral arteries with clinical manifestations. Severe hypertensive retinopathy: • Hemorrhages or exudates; • Swelling of the optic nerve nipple. | |
| Other risk factors* (except hypertension), target organ damage, associated diseases | Blood pressure, mmHg. | ||
| Level 1 SBP 140-159 DBP 90-99 | Degree 2 SBP 160-179 DBP 100-109 | Grade 3 SBP >180 DBP >110 | |
| I. No risk factors, target organ damage, associated diseases | Low risk | Medium risk | High risk |
| II. 1-2 risk factors | Medium risk | Medium risk | Very high risk |
| III. 3 or more risk factors and/or target organ damage | High risk | High risk | Very high risk |
| IV. Associated (concomitant) clinical conditions and/or diabetes mellitus | Very high risk | Very high risk | Very high risk |
Classification of hypertensive crises (JNC-6):
– Complicated hypertensive crisis (critical, emergency) is accompanied by the development of acute clinically significant and potentially fatal damage to target organs, which requires emergency hospitalization and immediate reduction in blood pressure using parenteral antihypertensive drugs. - Uncomplicated hypertensive crisis (non-critical, urgency) occurs with minimal subjective symptoms and objective symptoms against the background of an existing significant increase in blood pressure. It is not accompanied by acute development of target organ damage. Requires a decrease in blood pressure within several hours. Does not require emergency hospitalization. Uncomplicated hypertension is characterized by low-symptomatic hypertension in the following conditions associated with increased blood pressure: severe and malignant hypertension without acute complications, extensive burns, drug-induced hypertension, perioperative hypertension, acute glomerulonephritis with severe hypertension, crisis in scleroderma.
Admission:
emergency.
Indications for hospitalization: complicated hypertensive crisis, i.e.
The following conditions associated with increased blood pressure are diagnosed: - acute hypertensive encephalopathy; - acute cerebrovascular accident; - acute left ventricular failure (cardiac asthma, pulmonary edema); - acute coronary syndrome (myocardial infarction, unstable angina); - dissecting aortic aneurysm; - severe arterial bleeding; - eclampsia.
Diagnostic criteria:
- relatively sudden onset; - individually high blood pressure level (DBP usually exceeds 120-130 mmHg); - presence of signs of dysfunction of the central nervous system, encephalopathy with cerebral encephalopathy (intense headaches of a diffuse nature, a feeling of noise in the head, nausea, vomiting, blurred vision. Possible convulsions, drowsiness, severe disturbances of consciousness) and focal symptoms (paresthesia of the tips of the fingers, lips, cheeks, feeling of weakness in the arms, legs, double vision, transient speech disorders, transient hemiparesis); - neurovegetative disorders (thirst, dry mouth, feeling of “internal trembling”, palpitations, chill-like tremor, hyperhidrosis); - cardiac dysfunction of varying degrees of severity with subjective and objective manifestations; - pronounced ophthalmological signs (subjective signs and changes in the fundus - sharply expressed spasm of arterioles , dilation of venules, swelling of the optic nerve nipple, hemorrhages, retinal detachment); - new or worsened renal dysfunction.
List of main diagnostic measures:
1. Measure blood pressure every 15-30 minutes; 2. Electrocardiography;3. Echocardiography4. General blood test;5. General urine analysis;6. Biochemical blood tests - sodium, potassium, calcium, urea, creatinine, coagulogram, fibrinogen;7. Ophthalmoscopy;8. Consultation with a neurologist.
List of additional diagnostic measures:
1. Glycemic profile;2. Lipid spectrum; 3. 24-hour blood pressure monitoring;4. Rehberg test;5. Rheoencephalography and determination of the type of cerebral hemodynamics.
Treatment tactics:
The choice of therapeutic measures (drug, route of administration, expected rate and degree of blood pressure reduction) depends on the severity of the crisis and the presence of complications.
Emergency measures should be aimed at reducing the increased work of the left ventricle, eliminating peripheral vasoconstriction and hypervolemia (if present), cerebral ischemia (especially with seizures), acute coronary or heart failure.
Treatment tactics for complicated HA are intravenous administration of antihypertensive drugs, blood pressure monitoring, emergency hospitalization in the ICU, controlled hypotension, followed by transfer to tablet medications. In case of deterioration due to a decrease in blood pressure, the administration of drugs should be stopped. Within 30-120 minutes.
Blood pressure is reduced by 15-25%. Within 2-6 hours - up to 160/100 mmHg. Treatment tactics for uncomplicated HA - observation for 3-6 hours. Gradual reduction of blood pressure with the help of tablet medications, correction of previous therapy.
Treatment of an uncomplicated crisis
• Nifedipine – 10-20 mg orally, chew (in the absence of signs of deterioration in cerebral hemodynamics and atherosclerotic vascular lesions) • Enalaprilat – 1.25 mg IV, slowly over 3 minutes • Captopril – 25-50 mg sublingually ( It is proposed to include this short-acting drug of the ACEI group in the list of vital drugs as a drug for the relief of uncomplicated GC).• Clonidine - 0.075 mg sublingually (for GC while stopping clonidine).• b-blockers: Anaprilin 10-40 mg .; propranolol 40-80 mg. Hypertensive crisis with hypertensive encephalopathy requires careful lowering of blood pressure. For this, an intravenous infusion of sodium nitroprusside (0.25-10 mcg/min) is used. For convulsive syndrome, diazepam is administered (IV 10 mg).
Hypertensive crisis with acute left ventricular failure.
IV infusion of nitroglycerin is indicated (initially 5 mcg/min, if necessary, the dose is increased by 5 mcg/min every 3-5 minutes to 20 mcg/min, if the effect is not achieved, the dose is increased by 10-20 mcg/min to 100 mcg /min). In the absence of acute myocardial infarction, intravenous jet administration of enalaprilat is possible (0.625 - 1.25 mg over 5 minutes.
, if necessary, again every 6 hours). Dilatation of the pulmonary and peripheral veins in combination with suppression of tachypnea and reduction of psychomotor agitation is achieved by fractional intravenous administration of 2-4 mg of morphine hydrochloride every 5-25 minutes. To reduce blood volume and pressure in the pulmonary artery, furosemide is administered intravenously at a dose of 0.5-1 mg/kg.
Peripheral vasodilation in normal and elevated blood pressure is achieved by first taking nitroglycerin sublingually, then by intravenous drip infusion of nitroglycerin (infusion of 10 mcg/min, if necessary, increasing the dose by 5-10 mcg/min every 5-10 minutes until shortness of breath or mean blood pressure decreases by 10% with initially normal blood pressure and 30% with hypertension).
IV infusion of nitrates is especially indicated in the case of the development of acute left ventricular failure during myocardial infarction, as well as against the background of GC without cerebral symptoms. Ensuring optimal oxygenation of arterial blood is achieved by breathing humidified oxygen; in severe cases, tracheal intubation and mechanical ventilation are indicated.
Hypertensive crisis with acute coronary syndrome.
The drug of choice is intravenous infusion of nitroglycerin (5-200 mcg/min). It is undesirable to use sodium nitroprusside for myocardial ischemia.
Dissecting aortic aneurysm.
Propranolol 1-3 mg or verapamil 5 mg IV, nitroglycerin IV, morphine.
List of essential medications:
1. Nifedipine 10-20 mg, table 2. Enalapril 1.25 mg/1 ml, amp3. Captopril 25-50 mg, table 4. Furosemide 0.5-1 mg/kg, amp5. Nitroglycerin 0.0005 g, tablet, 0.1% amp List of additional medications: 1. Clonidine 0.15 mg, table 2. Morphine 1% 1 ml, amp 3. Verapamil 5 mg, amp4. Breathing humidified oxygen.
Criteria for transfer to the next stage of treatment:
– stabilization of blood pressure; – improvement of the patient’s well-being; – absence or reduction of signs of cerebral and focal symptoms of damage to the nervous system, neurovegetative disorders, cardiac complaints and other manifestations of dysfunction of the cardiovascular system.
Source: https://ruslekar.com/publ/standarty_lechenija_bolnykh_v_stacionare/sovremennye_metody_lechenija_gipertonicheskoj_bolezni/3-1-0-186
Hospitalization
A sharp change in blood pressure increases the load on blood vessels several times. The heart muscle suffers from a lack of oxygen, which can cause a heart attack.
First aid consists of the use of antihypertensive drugs and foot baths. But often it is not possible to do without a doctor. If it was not possible to correct the situation at home, then the pressure readings are normalized in a hospital setting.
If the development of a hypertensive crisis occurs for the first time, the patient is hospitalized. Medical assistance is needed when pain in the heart cannot be eliminated with Nitroglycerin, speech disturbances have occurred, sensitivity has decreased, the patient has lost consciousness, the drugs do not reduce blood pressure. Also read: Features of stage 2 hypertension
In a medical institution, the patient is examined to determine all the reasons that caused the abnormal increase in pressure. A suitable course of treatment can only be prescribed after a diagnosis has been made.
Treatment of hypertensive crisis is carried out in a hospital setting. Throughout the day, heart rate and blood pressure are monitored and blood pressure decreases.
After discharge, the patient must:
- Get at least eight hours of sleep.
- Avoid excessive physical activity.
- Take prescribed medications regularly.
- Get examined periodically.
- Monitor blood pressure readings daily.
- Treat in a timely manner concomitant diseases that can cause a crisis.
- Eat right, avoid bad habits.
With the help of such measures, you can increase life expectancy and reduce the risk of death and complications. With each new attack, the chances of a stroke or coronary artery disease increase.
Therefore, first aid must be provided before the doctor arrives. If you give the patient medicine and make a foot bath, you can hold out until the doctors arrive.
Treatment of hypertension
Arterial hypertension is a disease whose complications cause disability and premature death. At first, hypertension does not pose a health threat. But it is with minor symptoms that complex treatment of hypertension, selected by a specialist, should begin.
Groups of drugs intended for the treatment of arterial hypertension
Effective treatment of hypertension is focused on the mechanisms of disease development:
- if the etiology and clinical picture of hypertension is associated with salt and water retention, then antihypertensive drugs are prescribed along with diuretics;
- when angiotensin is involved in the pathological process, the doctor prescribes drugs that block the receptors of this hormone;
- It is possible to reduce the load on the heart and vascular resistance with the help of ACE inhibitors;
- Hypertension is often treated with drugs that affect the central nervous system;
- If clinical hypertension is accompanied by coronary heart disease, then the doctor prescribes beta-blockers.
Often, a specialist combines drugs, taking into account the etiology, pathogenesis, and concomitant diseases.
The most important thing in treating the disease is that clinical arterial hypertension does not manifest itself, and that blood pressure readings are within normal limits. Only then is the risk of complications minimal.
Drug treatment of hypertension
Treatment of hypertension in Moscow is carried out on an outpatient basis. This means that the doctor makes a diagnosis and prescribes medications that the patient must take under constant blood pressure monitoring.
Many people ask the question: where is hypertension treated in Moscow? Like any other somatic disease without complications, hypertension is treated in clinics or private clinics by a local physician.
In case of concomitant pathology, specialists can be involved in therapy - an ophthalmologist, nephrologist, etc. Treatment of hypertension without pills can be carried out only in the first stage of the disease. If a patient experiences a hypertensive crisis, he is hospitalized in a hospital.
There, medications are prescribed to reduce the symptoms of the crisis and prevent complications.
The best clinics for the treatment of hypertension in Moscow use the following drugs in treatment:
- ACEI - Enap, Lisinopril;
- AIR – Albarel, Moxonidine;
- calcium channel blockers – Nifedipine, Cinnarizine;
- sartans - Losartan, Eprosartan;
- diuretics – Indapamide;
- β-blockers – Concor, Atenolol.
Treatment of renal hypertension
The doctor identifies symptoms and treats renal hypertension in people with long-term kidney disease, as well as in their abnormal structure.
Symptoms of renal hypertension:
- increased blood pressure;
- swelling of the limbs;
- constant weakness;
- pain in the lumbar region;
- headache.
With a malignant course, pressure rises quickly, affects vision, and significantly reduces the quality and duration of life. With benign hypertension, the pathological process has a slow course.
Treatment of renal hypertension comes down to the following measures:
- restoration of kidney function;
- normalization of blood pressure.
It is possible to restore normal kidney function with the help of medications and surgical methods. Surgery will be required if there is polycystic disease, congenital anomalies, or cancer. In case of kidney failure, the patient is indicated for hemodialysis - that is, cleansing the blood of toxins that the kidneys are not able to remove on their own.
It is possible to normalize blood pressure with the help of drugs that are used to treat primary hypertension.
Complex treatment involves following a diet containing fruits and vegetables. Salt and products containing it should be excluded from the diet. There is a complete ban on alcohol and smoking.
You should be careful and sensitive to your health, do not self-medicate, follow doctor’s orders - only then can you improve your quality of life.
Dangerous misconceptions when taking medications
- You can often hear the misconception that medications should only be used when blood pressure values are above normal. This belief is dangerous to health and life. This approach increases the risk of adverse outcomes.
- Not every patient is confident that diuretics can be used constantly. Many people still think that these drugs wash potassium out of the body. In fact, modern diuretics wash it out in negligible quantities. Losses can easily be replenished by eating foods containing potassium.
- Long-term use of drugs affects liver health. In fact, not all drugs are so toxic that they should be abandoned at the expense of the health of the entire body. Drugs that significantly affect liver health are not prescribed to patients who have problems with this organ.
- Traditional medicine is better than pills. Indeed, some recipes using herbs can reduce blood pressure to normal values. However, it is not possible to achieve a qualitative reduction in stages 2 and 3 hypertension using similar methods.
Treatment of hypertension without drugs
The treatment of hypertension does not always involve medications. As a preventive measure, as well as during the first stage of the disease, following the rules of a healthy lifestyle will be useful. It is known that tobacco smoke and alcohol affect the lumen of blood vessels. Bad habits are incompatible with the disease.
Treatment of stage 1 hypertension is associated with proper nutrition. It has been proven that consuming more salt than the recommended amount leads to hypertension. You can prevent the disease or alleviate the condition of existing hypertension if you limit the consumption of fatty, fried foods, and include more fruits, vegetables, low-fat fish, and nuts in your diet.
Nervous excitability can be reduced using traditional medicine, for example, infusions, decoctions of mint, motherwort, valerian, etc.
It is possible to normalize blood pressure if you perform special exercises, do yoga, or influence the body with the help of a contrast shower.
The course, symptoms and treatment of stage 1 hypertension should only be monitored by a doctor.
What drugs are used
To provide effective assistance during a hypertensive crisis, it is necessary to use antihypertensive drugs. They are placed under the tongue so that the effect comes faster. The medicine is absorbed into the blood through vessels located under the tongue. In such cases, the following tablets are used:
- Nifedipine. The dosage should not exceed 20 mg. After consuming it, blood pressure decreases within half an hour. Indicators fall by 25%. If there is no result, then after 30 minutes you can take another tablet. Its effect can be observed within five hours. The drug is approved in the absence of heart pain and tachycardia.
- Captopril. It reduces blood pressure within a few minutes and maintains the effect for an hour.
- Nitroglycerine. It helps get rid of severe pain in the heart. A side effect of use can be severe headaches.
- Clonidine. Reduces blood pressure after a quarter of an hour.
For hypertension, tablets are always used.
But during a crisis they act too slowly, so the situation is corrected with injections or intravenous injections. A suitable technique for eliminating an attack is selected depending on the mechanism of development, cause, associated symptoms and complications. To speed up the therapeutic effect, drugs can be combined.
To fix the problem use:
- Magnesia. The product has an antispasmodic effect, eliminates stimulation of the nervous system, helps stabilize the heart rate and relax the muscles. With its help, you can prevent the development of stroke, atherosclerosis, and thrombosis. The medicine is produced in the form of a solution for droppers, which are dripped twice a day. Magnesia in its pure form is not used for blood pressure. It is diluted with glucose or Novocaine and administered very slowly.
- Dibazol. The drug prevents local circulatory disorders in the heart and brain, regulates blood flow in the kidneys. The drug is effective for hypertensive crisis and helps reduce blood pressure for several hours.
- Papaverine. It is often combined with Dibazol. After the drip, systolic and diastolic pressure levels are normalized. The drug is used to lower blood pressure for a short time. The combination of two medications relieves dizziness and headaches.
It is not advisable to try to correct the situation using folk remedies. Medicinal plants act rather slowly and do not help everyone. And in case of a hypertensive crisis, you need to act quickly.