Atrioventricular rhythm
AV junctional rhythm is a rare form of arrhythmia. This is the case when the AV node becomes the pacemaker of the heart. Fewer impulses occur in it than with normal indicators, heart rate fluctuates within 40 beats per minute.
Impulses arise in the proximal, middle or distal part of the AV node. If the impulse occurs in the upper part, then the heart rate becomes 70-80 beats. If an impulse occurs in the middle and distal part, the rhythm from the AV junction slows down.
The impulse from the AV node is sent to both the ventricles and the atria. If the impulse originates in the upper part of the node, then the atria contract first, if in the lower part, the ventricles contract.
Clinically, the atrioventricular rhythm is not particularly noticeable. The patients have no complaints about their health status. The pulse is large and slow. The first tone and apex impulse are slightly enhanced.
When AV conduction is disrupted, you can see that the pulse at the wrist and the neck veins pulsate simultaneously.
Atrioventricular dissociation
The phenomenon when the atria and ventricles of the heart work uncoordinated is called atrioventricular dissociation. A similar conduction disorder occurs if the upper and lower chambers of the heart have two different pacemakers.
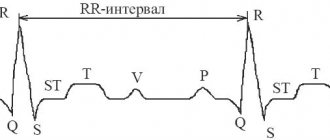
AV dissociation, which is not associated with blockade, can occur with AV junctional rhythm. If the sinus rhythm is similar to the escape rhythm, and the occurrence of P waves occurs just before the QRS, and the waves are superimposed on the complex, then this condition is called isorhythmic AV dissociation.
Dissociation may also occur due to increased activity of other pacemakers (ventricular, nodal or slave), which often exceed normal sinus rhythm. In this case, we talk about replacement AB dissociation.
AV dissociation on an ECG looks like this:
- P waves do not have a constant connection with the QRS complexes;
- QRS frequency is higher than P wave frequency;
- P waves may follow, be in the middle of, or precede QRS complexes.
Acceleration of av conduction on ecg
Hello! My husband's cardiogram was written as acceleration of atrioventricular conduction. What is it and what should I do?
Hello! Acceleration of atrioventricular conduction means that the time it takes for an electrical impulse in the heart to travel from the atria to the ventricles is shortened.
Without clinical manifestations and other changes on the ECG, this is not of particular significance, but once a year you need to undergo an ECG to monitor the situation.
If other ECG manifestations appear, you will need to consult a cardiologist. There is no need to do anything right now.
The sinus impulse, passing through the atrioventricular junction, undergoes a physiological delay (Chapter I.3), and in this regard, the PQ interval is 0.10 ± 0.02 s.
However, in a number of diseases and conditions (pubertal heart, menopause, NCD, etc.), accelerated conduction of the sinus impulse through the atrioventricular connection is observed, which significantly shortens the PQ interval.
This phenomenon was described by several researchers and named in their honor as Clerk-Levy-Christesco syndrome, abbreviated as CLC (after the first Latin letters of their surnames).
Thus, an ECG sign of CLC syndrome is a shortening of the PQ interval with a normal shape and duration of the ventricular QRS complex (the impulse reaches the ventricles in the usual way).
VIII.9 Syndromes of premature excitation of the ventricles
The essence of various syndromes of premature excitation of the ventricles is that the sinus impulse from the atria to the ventricles is carried out simultaneously in two different ways along the atrioventricular connection and through additional conduction bundles. Along these additional pathways, the sinus impulse reaches part of the ventricles faster than the same impulse that usually goes through the atrioventricular connection, undergoing a physiological delay in it.
These additional bundles of conducting tissue located between the atria and ventricles are named after the authors who discovered them.
The right and left Paladino-Kent bundles are distinguished. Mahaima and James. Depending on which of them passes the sinus impulse to the ventricles, several syndromes of premature excitation are distinguished
VIII.9 Syndromes of premature excitation of the ventricles
Atrioventricular communication
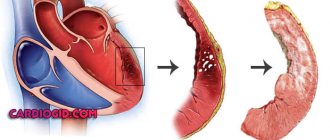
A heart defect associated with impaired development of the AV valves and cardiac septum is called atrioventricular communication.
- atrioventricular communication, full form;
- intermittent form;
- incomplete form.
Symptoms of this pathological condition are shortness of breath and increased fatigue of the patient, which occurs even with minimal exertion. The skin is anemic, children with this pathology develop physically slower than their healthy peers, they more often suffer from respiratory tract diseases.
During AV communication, patients are diagnosed with irregular heart rhythm, arrhythmia, and heart murmurs.
Treatment is surgical. After surgery, the survival rate for 20 years is 70%. If there is a need for reoperation, the prognosis is reduced by 5%.
Reasons for slowing intraatrial conduction
Slowing of intraatrial conduction is a serious pathology that can provoke life-threatening conditions. What it is - everyone who has any dysfunction of the heart should know. It is diagnosed when a patient has a slow cardiac impulse due to poor automaticity, contractility and excitability. With this disease, there is a change in the rhythm and force of contraction of the central circulatory organ. In a certain area there may be no such cycles at all.
Definition
Before treating the disease, it is necessary to understand what this means and find out the reason why intra-atrial conduction has slowed down.
Changing the order of heart contractions negatively affects the functioning of the heart, putting a person’s life in danger. Such a disorder may mean that the process of blood flowing from the main circulatory organ to the aorta is difficult. Several stages of development of this pathology are classified. Depending on the nature of the heart conduction disorder, the following blockades are distinguished:
- Incomplete. Diagnosed at an early stage of the development of the disease. Characterized by slow impulse transmission along the conductive fibers of the heart.
- Full. Occurs in the absence of proper treatment. As a rule, it is not compatible with life, since it completely stops the passage of impulses through the conduction system.
The reason why such violations occurred may lie in heart damage, the presence of defects, or coronary artery disease. Bad habits such as smoking and alcohol abuse play an important role in this. An unhealthy lifestyle, frequent stress, and taking medications that have a stimulating effect on the cardiovascular system do not have a very good effect on the condition of the heart.
Atrioventricular conduction disorders
They can manifest themselves either as shortening or difficulty.
Shortening of atrioventricular conduction
(absence of atrioventricular delay) leads to almost simultaneous contraction of the ventricles and atria, as a result of which the atria do not have time to fully contract and eject blood into the ventricles. It is observed in congenital diseases: Wolf-Parkinson-White syndrome and Clerk-Levy-Christesco syndrome. In both syndromes, there are additional fast conduction bundles between the atria and ventricles. In Wolff-Parkinson-White syndrome, additional bundles of Kent are located around the fibrous rings of the atrioventricular valves. Clerk-Levy-Christesco syndrome is characterized by the presence of an additional fast-conducting James bundle between the atrial myocardium and the trunk of the His bundle.
Functional shortening of atrioventricular conduction is possible with stress, physical activity and the use of drugs that excite β-adrenergic receptors. See also Beta-agonists.
Obstruction of atrioventricular conduction
(atrioventricular (AV) block) can be either functional or a symptom of many organic heart diseases.
Functional slowing of atrioventricular conduction (1st degree AV block) is often observed in athletes with severe vagotonia. Interval PQ(R)
in this case, it can reach 0.2 seconds, but blockade with interruption of impulse conduction from the atria to the ventricles (2nd and 3rd degree AV block) is never observed. With severe vagotonia associated with increased ascending afferentation from internal organs (surgeries on the abdominal organs with an inadequate level of anesthesia and the use of M-cholinergic blockers, a blow to the solar plexus) or the use of anticholinesterase drugs, M-cholinomimetics, cardiac glycosides, etc., conduction may deteriorate up to complete atrioventricular block (AV block 3rd degree). Functional atrioventricular block is also observed with the use of β-blockers, antiarrhythmic drugs, and with inferior (posterior phrenic) myocardial infarction. Atrioventricular block of the 2nd and 3rd degrees can lead to fainting (Morgagni-Adams-Stokes syndrome), since due to the rare rhythm of heart contractions, the brain experiences a lack of oxygen.
Organic obstruction of atrioventricular conduction is observed with myocardial infarction (especially anterior), myocarditis, Lenegra's disease (sclerosis of the conduction system of the heart), after heart surgery.
How does pathology affect the functioning of the body?
With a partial disorder of sinoarterial conduction, no symptoms appear, but with a complete disorder, an adult may experience pain in the chest and dizziness caused by poor blood flow in the brain against the background of rare heart contractions.
As for interatrial block, it does not pose a threat to life. But its presence increases the risk of developing atrial fibrillation, which is a serious threat to human health. This disorder is accompanied by shortness of breath at rest and when walking, swelling of the legs, bluish discoloration of the skin, and discomfort in the chest.
Atrioventricular block is not always expressed by symptoms, but its combination with bradycardia can lead to an attack of MAS (Morgagni-Adams-Stokes). The patient at this moment may suddenly feel weak in the body. It is possible that you may experience dizziness or even loss of consciousness. Seizures associated with deterioration of blood supply to the blood vessels of the brain may also occur. This condition requires emergency medical attention. Inaction can cause cardiac arrest.
The intraventricular type of pathology occurs due to a disorder of ventricular conduction through the bundle branches. Partial blockade does not always manifest itself, but complete blockade is accompanied by a rare pulse, loss of consciousness, and pain in the chest.
Impairment of cardiac impulse conduction
The property of the heart, when an impulse originating in the sinus node propagates to cardiomyocytes, is called cardiac muscle conductivity. Myocyte conductivity is directly related to excitability, that is, the ability of a muscle cell to respond to an impulse.
The signal initially arises in the sinoatrial node, travels through the structures one by one, leading to excitation of the atria, then the ventricles. The entire process aims to push blood from the heart into the aorta.
Impulse delay can occur at any point and cause cardiac conduction disturbances.
Causes
The causes of cardiac impulse conduction disturbances are either very simple or indicate serious heart disease. It is necessary to clearly define what the slowing down process means and what is conduction slowing down.
If periods of first degree atrioventricular block are visible on the ECG of the heart, then they speak of a slowdown in conduction.
At the time of the cardiogram, the patient’s condition does not cause concern, but in the future there is a high probability of disease progression.
If the ECG shows a second or third degree block, then a cardiac conduction disorder is determined, which, in turn, can be partial or complete. The second option is much more dangerous and requires urgent medical intervention.
Conduction system of the heart
Sinoatrial blockade
Violation of sinoatrial conduction of the heart is a condition when impulses that appear in the sinus node do not fully reach the atria, which delays excitation. This situation is sometimes typical for a healthy person and does not require urgent treatment. But most often, heart block occurs against the background of organic heart disease.
The reasons for the violation may be:
- NCD with a predominant effect on the sinus node, which causes a slowdown in heart rate;
- an increase in heart size in people actively involved in sports;
- uncontrolled use of glycosides used to treat arrhythmia;
- congenital and acquired heart defects;
Symptoms of complete sinoatrial block:
With partial violation, there are practically no signs.
Intraatrial block
Slowing intraatrial conduction is not dangerous to human life, but can cause irregular heart function, which leads to very dangerous consequences.
The causes of intraatrial conduction of the heart are:
- glycoside intoxication;
- rheumatism;
- heart development disorders;
- persistently high blood pressure.
Signs of acute manifestations of conduction slowing do not appear until the electrocardiogram.
In the chronic course of the disease, patients complain of shortness of breath both during movement and at rest, swelling of the legs, acrocyanosis of the skin, pain in the sternum, and others.
Atrioventricular block
Violation of cardiac conduction through the atrioventricular node of the first and second degrees appears when there is a delay in the transmission of impulses from the atria to the ventricles.
With third-degree blockade, the ventricles contract independently of the atria, since impulses do not reach them at all. Thus, a dangerous condition for the body arises, and sudden death is possible.
Causes of atrioventricular block:
- heart pathologies, congenital and acquired;
- estate;
- myocardial inflammation;
- toxic hormonal influence.
The danger of the condition is that in the absence of treatment, active development of the blockade is noted.
The symptoms of a blockade of the first two degrees are not pronounced, especially if the pulse is within fifty-five beats per minute.
The third degree is characterized by cardiac bradycardia (pulse rate within forty beats), weakness, and short-term fainting. In this state, convulsions occur.
The patient requires urgent medical care, the absence of which can lead to death.
Intraventricular block
Violation of intraventricular conduction of the heart is a complete or partial block of the bundle branches. There are disorders of the contractility of the right or left ventricles.
The causes of intraventricular conduction of the heart are as follows:
- opening between the atria;
- myocardial proliferation;
- ischemia;
- myocardial infarction;
- pulmonary diseases;
- cardiosclerosis.
An ordinary person may experience a partial right bundle branch block that is asymptomatic.
Complete blockade is manifested by bradycardia, pain in the sternum, and short-term loss of consciousness. If there is pressing pain in the thoracic region, nausea, weakness, the cardiogram will show complete blockade on the left, then a heart attack can be diagnosed. Only a multiple cardiogram shows this accurately. For such indications, urgent inpatient treatment of the patient is required.
Sometimes the impulse is blocked in distant parts of the heart - Purkinje fibers. This phenomenon is called nonspecific intraventricular conduction disorder. The reasons are the same, but the symptoms are practically absent.
Wolff–Parkinson–White syndrome
This is a condition in which the impulse is accelerated. This disruption occurs due to the activity of accessory pathways. As a result of this, impulses reach the ventricle in greater quantities than they should, the ventricles contract more often, and the impulses pass in the opposite direction. The result of this process is supraventricular tachycardia of the heart.
Normal heart rhythm on ECG and atrial fibrillation
Wolff–Parkinson–White syndrome is congenital. During normal pregnancy, the fetal accessory pathways close at approximately twenty weeks.
This pathology can be caused by various external factors affecting the unborn child. This includes an increased radioactive background, the use of drugs and alcohol by the expectant mother during pregnancy. A genetic factor may also be the cause.
Signs are noticed in early childhood, although sometimes the disease is asymptomatic until adulthood. Rarely, the disease is detected during a medical examination by analyzing the electrocardiogram.
A symptom of arrhythmia is an increase in heart rate up to two hundred beats. In this case, the patient complains of pain, breathing problems, and oxygen deficiency.
In some cases, cardiac fibrillation may develop, which is a threat to the patient’s life.
One type of SVC syndrome is shortened PQ interval syndrome. The James bundles play the role of pathological pathways. When diagnosing a disorder only by a cardiogram, without outwardly having any signs, experts call the phenomenon a phenomenon, and in case of rapid heartbeat - shortened PQ syndrome. The difference can only be seen in the cardiogram readings.
Diagnostics
If even minor manifestations of the disease are detected, the patient should visit an arrhythmologist. If there is no such specialist in your area of residence, you should contact a cardiologist.
Diagnosis of cardiac conduction disorders includes:
- An ECG using the Holter method is the main method that will help identify the degree of disturbance, mark periods of decreased heart rate, and identify the relationship of pathology with the use of medications, as well as with the time of day.
- An electrocardiogram with exercise is a special test on a treadmill or exercise bike, when electrodes are attached to the patient and the relationship of the disorder with physical activity is revealed.
- An ultrasound examination of the heart shows the appearance and structure of heart tissue and helps determine the disease and functionality of the myocardium.
- Laboratory tests of blood and urine.
- Biological and chemical blood test.
- Study of hormone levels.
Additional examination methods are prescribed by the attending physician, based on the individual course of the disease.
Parents who notice shortness of breath, decreased attention, forgetfulness, poor school performance, and recurrent heart pain in their children should be especially attentive. At the slightest suspicion, you must show the child to the doctor, strictly follow his recommendations and undergo all necessary examinations.
Treatment
Treatment of cardiac conduction disorders depends entirely on the cause that triggered the onset of the disease.
A heart attack, for example, requires therapy aimed at eliminating cardiac ischemia, but does not provide a special effect on conduction disorders.
Myocarditis is treated with antibiotics and glucocorticosteroids, which does not allow atrioventricular and intraventricular conduction disturbances to actively develop.
Treatment must be carried out under the supervision of a doctor. All recommendations must be followed to avoid the sudden development of complete atrioventricular block, when the patient’s life can be very difficult to save.
If such a complication occurs, temporary electrical stimulation is recommended to deliver impulses to restore cardiac conduction. After such a situation, doctors advise all patients to install an pacemaker.
If during the examination no heart disease was found, but the patient complained specifically about this area, then the doctor prescribes vitamins to nourish the heart, and also registers the patient for further observation.
There are situations when an ambulance should be called immediately:
- pulse less than forty-five beats per minute or more than one hundred and twenty beats;
- short-term loss of consciousness;
- pain in the heart area;
- general weakness of the body, increased sweating;
- sudden shortness of breath.
Timely assistance will protect the patient from serious complications.
If you have severe pain in the heart area, you should immediately call an ambulance
Forecast
Partial disruption of cardiac conduction almost always goes away without a trace.
With the development of complete blockade, serious complications of cardiac conduction disorders are observed:
- pulmonary artery thrombosis;
- stroke;
- sudden death;
- others.
The prognosis of cardiac conduction disorders depends on the severity of the underlying disease and its reversibility. The prognosis for the first manifestations of heart attacks is much better than for subsequent ones, one of which can lead to the death of the patient.
Symptoms
Among the typical complaints, patients most often note:
- strong heartbeat;
- heart failure;
- periodic stopping of contractions;
- dizziness;
- fainting;
- angina pain in the heart;
- shortness of breath.
When intraventricular conduction slows down, symptoms are rarely observed. The clinical picture becomes pronounced only if there are signs of the disease that caused the violations that occurred. Sometimes patients experience fatigue, weakness in the body and decreased performance. It is possible that you may have memory problems. Sudden mood swings, feelings of fear and anxiety may also cause concern.
With a complete primary blockade, a local disorder occurs, accompanied by various heart defects, which can only be corrected surgically. Such problems are quite common among newborns. They are diagnosed in children born from mothers with cardiovascular or autoimmune diseases.
Diagnostics
If you have one of the listed symptoms, you should immediately consult a cardiologist or arrhythmologist. To make an accurate diagnosis and prescribe effective treatment, the patient needs to undergo a number of studies:
- cardiogram and Holter monitoring;
- ECG tests in the presence of load;
- ultrasound examination of the heart or echocardiography.
If an intra-atrial defect was confirmed during diagnosis, it is necessary to obtain specialist advice as quickly as possible in order to prevent serious consequences.
If a young man is facing the army, then with such a diagnosis he can count on release, especially if the conduction disorder is observed for more than 7 days. Persistent heart rhythm disturbances require long-term treatment.
How does pregnancy go with this diagnosis?
Any disruptions in the functioning of the female body during pregnancy are unpredictable, especially when it comes to heart pathologies. Rhythm disturbances are a serious medical problem that threatens the life of the fetus. The mechanisms for the development of such deviations are usually associated with hormonal changes and functional changes that occur in a pregnant woman.
If there is any deviation in the functioning of the cardiovascular system, the patient is referred for diagnostics. The research methods are practically no different from the generally accepted ones. If necessary, drug therapy is prescribed, including antiarrhythmic drugs.
Dangers and possible complications
The danger lies in the development of heart failure, myocardial infarction, and atrial fibrillation. This is what slows intraatrial conduction threatens:
- angina pectoris;
- pulmonary artery thrombosis;
- attack of MES;
- cerebral ischemia;
- stroke;
- sudden cardiac death.
The most dangerous to health are considered to be attacks of MES, loss of consciousness, and epileptiform convulsions. The severity of such phenomena depends mainly on the duration of the ventricular stop and the level of the pulse drop (its indicators can drop by 10-20 beats per minute or even lower). At the time of an attack, blood pressure almost always reaches critical levels. This condition can repeat several times a day lasting more than 5 minutes. This often ends in cardiac arrest.
The consequences of the disease are especially dangerous.
In addition to MES attacks, which are caused by oxygen starvation of brain tissue, the patient may experience memory impairment, worsening of coronary artery disease, and decreased intellectual ability. If the blockade goes from partial to complete, it threatens ventricular fibrillation and cardiogenic shock, which ends in cardiac arrest and sudden death.
clc syndrome
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
CLC syndrome got its name from the names of the scientists who described it - Clerk, Levy and Critesco. Another name for this condition is LGL (Launa-Ganong-Levine) syndrome. In this article we will talk about how and why this syndrome occurs, how dangerous it is for health and life, how to be treated and live with this diagnosis.
Development mechanism
Conduction system of the heart
OUR READERS RECOMMEND!
Our readers successfully use ReCardio to treat hypertension. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
The heart contracts under the influence of impulses that are produced in a cluster of nerve cells located in the right atrium - the sinus node. This is a kind of battery that regularly sends electrical signals to the cells of the heart muscle. The impulses travel along nerve pathways in the atria, causing them to contract. During this process, blood from the atria is squeezed into the ventricles.
In order for the ventricles of the heart to fill well with blood and contract a little later than the atria, nature has provided a special filter at the border between them - the atrioventricular node. Excitement, once in it, comes slowly. Only after passing through the atrioventricular junction, electrical impulses quickly spread throughout the ventricular myocardium and cause their contraction. As a result, blood is pushed into the aorta and pulmonary trunk.
It takes up to 0.1 s for nerve impulses to travel along the intraatrial pathways. It takes them the same amount of time to overcome the atrioventricular node. Therefore, the total time from the onset of atrial contraction to the exit of the signal from the atrioventricular junction and the beginning of ventricular contraction normally does not exceed 0.2 s. On the electrocardiogram, this distance corresponds to the PQ interval.
However, in some people, from birth, bypass pathways for impulses are formed in the heart, bypassing the atrioventricular connection. One such additional conduction pathway is the James bundle. Passing through it, excitation does not linger at the border between the atria and ventricles. Therefore, the duration of the PQ interval is reduced to less than 0.11 s. The CLC phenomenon arises. This is just an electrocardiographic term that reflects changes in the cardiogram recording itself.
However, sometimes impulses, having passed along the short James path, return back through the atrioventricular node and again follow this path. In other cases, the impulse passes through the atrioventricular node and returns through the James bundle. A circular course of excitation is formed. In this circle, the impulse circulates very quickly, causing the development of a heart rhythm disorder - paroxysm of supraventricular tachycardia. When such deviations appear, accompanied by patient complaints and changes in the electrocardiogram, they speak of CLC syndrome. Thus, CLC syndrome is distinguished from a phenomenon by the presence of clinical manifestations. The same applies to the Wolf-Parkinson-White phenomenon/syndrome.
Reasons for development
The phenomenon and syndrome of CLC are congenital diseases. Their exact cause is unknown. One can only assume that it is associated with a harmful effect on the fetus at that moment in pregnancy, when the heart and its pathways are formed. A genetic cause is also possible - a “breakdown” of a certain gene responsible for the development of intracardiac pathways.
A shortening of the PQ interval is observed in two out of a hundred healthy people, more often in middle-aged men. CLC syndrome can also be caused by coronary artery disease, hypertension, myocardial infarction, rheumatism, hyperthyroidism, hypovitaminosis B and other conditions affecting nerve cells and blood supply to the heart.
Symptoms and diagnosis
Patients with CLC syndrome may not know about their disease for a long time, since it does not always cause any symptoms. Only an ECG study allows a correct diagnosis.
The CLC phenomenon is manifested by a shortening of the PQ interval on the electrocardiogram and does not cause any symptoms. A person can live his whole life with such changes and not feel any health problems.
The development of CLC syndrome is accompanied by the appearance of sudden attacks of palpitations - paroxysms of supraventricular tachycardia. Paroxysmal cardiac arrhythmias with this type of ventricular preexcitation occur less frequently than in patients with Wolff-Parkinson-White (WPW) syndrome.
Paroxysmal supraventricular tachycardia is clinically manifested by a sudden attack of palpitations with a heart rate of 140 to 220 beats per minute (usually 150 to 180 beats per minute). Before this, the patient sometimes feels a jolt in the heart or neck. An attack of palpitations may be accompanied by dizziness, noise in the head, squeezing pain behind the sternum, and fainting. In some cases, sweating, bloating, nausea or even vomiting may occur. At the beginning or end of a long paroxysm of arrhythmia, there may be copious urination.
The attack can be stopped with the help of vagal tests - straining while inhaling, lowering the face into cold water while holding your breath, massaging the carotid sinus area in the neck.
In rare cases, CLC syndrome may be accompanied by paroxysmal atrial fibrillation: frequent, irregular heartbeat.
CLC syndrome is diagnosed using electrocardiography and 24-hour electrocardiogram monitoring. In addition to these studies, transesophageal electrophysiological examination of the heart is recommended.
Treatment
In many cases, CLC syndrome does not require special treatment. If an attack of arrhythmia occurs, it is recommended to perform vagal tests yourself, and if they are ineffective, call an ambulance. Paroxysm of supraventricular tachycardia or atrial fibrillation can be stopped (stopped) using drugs such as sodium adenosine triphosphate (ATP), verapamil, beta blockers, procainamide, amiodarone and others.
It should be noted that for various forms of tachycardia, some of the listed drugs are contraindicated, so only a doctor should stop the paroxysm with medication. Once the rhythm is restored, some patients may be prescribed antiarrhythmic drugs to prevent attacks.
In arrhythmology departments, the doctor can restore normal rhythm using electrical cardioversion. This method involves applying a series of electrical impulses to stop the circular excitation.
For frequently recurring paroxysms that worsen the patient’s quality of life and prevent him from performing his professional duties, surgical treatment is performed. It is aimed at destroying the additional pathway. This intervention is carried out after an intracardiac electrophysiological study, which is carried out using a special probe inserted into the heart through a vessel. The operation is called radiofrequency catheter ablation. This intervention is low-traumatic, after which the patient quickly returns to normal life.
How to decipher a cardiogram of the heart? The formation of a conclusion on an electrocardiogram (ECG) is carried out by a functional diagnostics doctor or cardiologist. This is a difficult diagnostic process,...
Ventricular extrasystoles: causes, signs, treatment Ventricular extrasystoles (VES) are extraordinary contractions of the heart that occur under the influence of premature impulses that originate from the intraventricular...
Right atrial hypertrophy: causes, symptoms, diagnosis Right atrial hypertrophy (RAH) is a term that refers to the enlargement of this part of the heart. Let us remember that venous blood enters the right atrium...
Treatment
The method of treating patients is determined individually for each person. In this case, concomitant diseases, characteristics of the body, lifestyle, health status and age are taken into account.
In the fight against pathology, different treatment regimens are used. The first stage is medication. With its help, you can slow down the development of the disease if it was detected at the initial stage. To correct the condition, a complex of vitamins and minerals is prescribed. Very often in such situations, Productal is prescribed. In order to prevent the disease from progressing to a more severe form, calcium antagonists, thrombolytics and anticoagulants are used. Among other means that are recommended to combat impulse conduction disorders, the following should be highlighted:
- potassium and magnesium preparations;
- anti-ischemic drugs;
- beta blockers and adrenergic agonists.
What is av conduction retardation what is it
In electrocardiography
Three qualitatively different types of A-V conduction disturbance are considered.
The first type includes slowing down of A - V conductivity
. In this case, the ECG shows an increase in the P - Q interval (P - R) of more than 0.20 seconds. This type is called incomplete atrioventricular block of the first degree or, according to the classification proposed by WHO (N. A. Mazur, 1980), A - V blockade of the first degree. However, there is no true blockade here; all impulses are conducted into the ventricles. Therefore, when prolonging the P-Q interval, it is more correct to use the term atrioventricular conduction slowdown. This terminology was used by A. M. Seagal (1958), Wenckebach R. and Winterberg H. (1927), etc. This type of conduction disorder does not cause disturbances in the rhythm of the atria and ventricles.
The second type of A-V conduction disorder
- these are different types and degrees of incomplete A - V blockade. Incomplete A-V blockade is characterized by the fact that some atrial (sinus) impulses are conducted into the ventricles, others are not conducted - they are blocked in the A-V node or the His system. If one or more impulses are blocked in a row, then such a blockade is designated as A - V blockade of the second degree.
It seems to us
It is more correct to designate this kind of A-V conduction disorder with the term incomplete A-V blockade, indicating the ratio of the total number of atrial (sinus) impulses to the number of impulses conducted into the ventricles. For example, 4:3, i.e., out of every four atrial impulses, three are conducted into the ventricles (one is blocked); 2:1, when every second atrial impulse is blocked in the A - V node; 4:1, if out of four atrial impulses only one passes into the ventricles. Since all these and other similar cases of incomplete A-V blockade characterize varying degrees of its severity, it is inappropriate and inaccurate to designate them only as II degree.
On ECG
at the same time, against the background of normal sinus cycles PQRST, a periodically increased R-R pause is recorded, during which there is a P wave without a QRST complex following it. This P wave is located at the same distance from the P waves of the preceding and following cycles, i.e. there is no arrhythmia of atrial contractions. However, the absence of the ventricular complex causes arrhythmia of ventricular contractions.
When describing the ECG
in case of incomplete A-V blockade, it is necessary to indicate how often the blockade occurs, i.e., what is the ratio of the number of atrial and ventricular complexes: 3:2, 4:3, 5:4, etc. This gives an idea of the severity of the conduction disorder . The more frequently the cycles are blocked, the higher the degree of incomplete blockade. Thus, M. S. Kushakovsky (1974) rightly considers incomplete A-V blockade 2:1 to be a separate type, since it is characterized by a high frequency of loss of the ventricular complex.
Both types of incomplete A - V blockade
, classified by Mobitz (1928), with increasing damage to the A-V systems, they can go into a 2:1 blockade and an even higher degree of blockade (3:1, 4:1, etc.). In these cases, it is not always possible to determine which type of block (according to Mobitz) preceded the 2:1 block.
For incomplete A - V blockade type I
(according to Mobitz), first described by Wenckebach R. (1907) and interpreted by A.F. Samoilov (1929), is characterized by a gradual increase in the P - Q interval in the cycles performed. At the same time, the increase in the duration of the P-Q interval increases unevenly. In the second cycle after the loss of the ventricular complex, P - Q significantly exceeds P - Q of the first cycle. However, already in the third cycle P - Q exceeds P - Q of the second cycle to a lesser extent, etc. Thus, the P - Q interval from cycle to cycle becomes longer, but increases to a lesser extent. According to the increase in the P-Q interval, the R-R interval gradually decreases until the ventricular complex falls out (pause).
Option “high-grade blockade”
What will be the frequency of excitation (contraction) of the ventricles at a periodicity of 4:1, if the sinus node produces, say, 80 impulses per minute? A total of 20 contractions per minute. Of course, at this heart rate the patient will be in critical condition. Therefore, taking into account the particular danger to the patient’s life, periods of 4:1 and higher are classified as a special variant of incomplete atrioventricular block - high-grade block. Finally, as atrioventricular conduction deteriorates further, a state occurs where no sinus impulse passes through the atrioventricular junction. This is complete atrioventricular block.
Description, causes and types
The conduction system of the heart consists of several sections. The electrical impulse is produced in the sinoatrial node, where the vena cava enters the right atrium. The signal is transmitted along the fibers of the Bachmann, Thorel and Wenckebach bundles inside the atrial myocardium (first left, then right) to the atrioventricular node. Excitation of atrial cells is provided primarily by the functioning of the Bachmann bundle. The signal is transmitted to the ventricular myocardium through the His bundle and Purkinje fibers.
Adequate passage of the impulse while maintaining intervals and pauses corresponds to the systolic and diastolic phases of the cardiac cycle.
Sometimes the conduction of an electrical signal slows down in one of the sections of the conduction system (blockade). This process is called conduction disturbance. Pathophysiologically, the blockade develops for two reasons: insufficient activity of nerve fibers and their low sensitivity to mediators.
There are two variants of pathology:
- Incomplete - the impulse passes from the right atrium to the left over a longer period of time.
- Full – both cameras operate independently of each other. Most often, the rhythm of the ventricles is provided by the sinus node, and the rhythm of the left atrium is provided by ectopic foci.
Violations are most often associated with an overdose of cardiac glycosides and other antiarrhythmic drugs. They also occur against the background of chronic ischemic heart disease, cardiomyopathy, and rheumatic endocardial damage.
In pregnant women, arrhythmia can be caused by: an increase in the amount of estrogens and chorionic gonadopropin, increased sensitivity of adrenergic receptors and accumulation of fluid in the body.
What is cardiac conduction
The heart has a complex structure, consisting of many departments, the work of which is interconnected. For example, an electronic impulse occurs in the sinus node. It goes to cardiomyocytes. Their conductive capacity is determined by the ability of muscle cells to respond to an incoming impulse. The signal generated in the sinus node passes through a number of structural divisions, causing excitation in the atria and ventricles. The essence of this complex process is to push blood flow from the heart muscle into the aorta and further throughout the body.
The impulse can be delayed at any point along its path, thereby causing a violation of the intraventricular conduction of the heart - that’s what it is. We tried to present the essence of the problem briefly and in an accessible form. If we succeed, then we can move on.
Examination and instrumental diagnostics
Slowing of intraatrial conduction is characterized by nonspecific symptoms of rhythm disturbances:
- a feeling of interruptions in the work of the heart - additional extraordinary contractions;
- sudden attacks of increased heart rate;
- “freezing” in the chest;
- shortness of breath - in case of long-term progression of the pathology.
The occurrence of pathology is always associated with organic damage to the myocardium, therefore, during a clinical examination of the patient, the symptoms of the underlying disease come to the fore:
vegetative-vascular dysfunction – sweating, redness of the face;- arrhythmic pulse with satisfactory filling and amplitude characteristics;
- lability of blood pressure;
- Ultrasound examination reveals areas of hypokinesia, significant expansion of the left atrium cavity.
The diagnosis of intraatrial block is determined by the results of electrocardiography (ECG). Criteria:
- P wave lengthening more than 0.12 s in II, III, aVR;
- change in tooth shape – splitting, two-phase, flattening.
Depending on the cardiogram data, the degree (1, 2, 3) of pathology is distinguished. The first degree is most often accompanied by other rhythm disturbances - atrioventricular or intraventricular blockade, ectrasystole.
Diagnosis and treatment
Atrioventricular block on the electrocardiogram
The patient has no specific manifestations of intraatrial conduction disturbances. All clinical signs and symptoms are due to the underlying disease. The presence of intraatrial conduction disturbances can be judged based on the analysis of the electrocardiogram. Intraatrial block has the following electrocardiographic signs: 1st degree is characterized by the presence of changes in each cycle:
- The duration of the P wave is more than 0.11 seconds;
- The P wave in its amplitude can be expanded, split, jagged, double-humped;
- The amplitude of the P wave may be reduced.
2nd degree is characterized by the following features:
- Gradual increase in the duration and splitting of the P wave,
- Periodic disappearance of the left atrial phase of the wave in lead V1.
A number of authors distinguish 2 types of 2 degrees. The first type is characterized by a gradual increase in conduction slowdown and expansion, followed by loss of the QRST complex with preservation of the first “hump” of the P wave. The second type is characterized by a sudden loss of the complex without a previous slowdown in expansion. The P waves are equally widened.
Atrioventricular block 3rd degree
Grade 3 is characterized by atrial dissociation and is quite rare. Diagnostic signs:
- The presence of a short P wave on the ECG, reflecting excitation of the right atrium;
- The presence of small left atrial P waves (flicker waves).
After an ECG diagnosis of intra-atrial conduction disturbance, a number of additional laboratory and instrumental studies are carried out aimed at identifying the underlying disease. There is no isolated treatment for intraatrial conduction disorder, since it is caused by a specific disease or pathological condition. Treatment is aimed at the underlying disease.
Correction methods and treatment: what and when to do
An isolated disturbance in the conduction of impulses along the interatrial fibers, which is not accompanied by clinical symptoms, does not require treatment. Drug therapy is prescribed for the development of arrhythmias with hemodynamic disturbances: atrial fibrillation, extrasystole, paroxysmal tachycardia.
Groups of drugs used:
- antiari, Cordarone, Etatsizin, Bisoprolol.
- cardiac glycosides: Digoxin;
- diuretics: Eplerenone, Spironaloctone, Torsemide.
High-degree intraatrial blocks that cause symptoms of heart failure require a pacemaker (artificial pacemaker). Installation of electrodes in both atria allows synchronizing the work of the myocardium.
conclusions
Disturbance in the conduction of electrical impulses from the right atrium to the left is caused by various diffuse pathologies of the myocardium of rheumatic, coronarogenic or unknown origin. Isolated intraatrial blockades do not cause hemodynamic disorders and clinical signs of heart failure, but may cause further high-grade arrhythmias. Treatment of the pathology is carried out depending on the underlying disease and existing symptoms and involves the use of pharmaceuticals or the installation of an artificial pacemaker.
The following sources of information were used to prepare the material.
Treatment of atrioventricular conduction disorders
Approaches to the treatment of atrioventricular conduction disorders depend on the underlying disease.
Shortening of conduction, if it does not lead to severe arrhythmias, usually does not require treatment. But if the condition is accompanied by frequent extrasystole or recurrent paroxysmal tachycardia, then surgical treatment is the most effective (for example, destruction of the additional bundle of Kent in Wolff-Parkinson-White syndrome). Antiarrhythmic drugs are used as palliative treatment. It is undesirable to use group IV antiarrhythmic drugs (calcium channel blockers: verapamil, diltiazem, etc.) for Wolff-Parkinson-White and Clerk-Levy-Christesco syndromes, since they significantly slow down nodal conduction without affecting the conduction of additional bundles. This can provoke the occurrence of re-entry arrhythmias: extrasystole and paroxysmal tachycardia.
Treatment for atrioventricular conduction delays depends on its etiology. Physiological prolongation of the PQ(R)
does not require treatment. With progressive atrioventricular block associated with the presence of organic heart disease (coronary heart disease, myocardial infarction, myocarditis, Lenegra disease, etc.), implantation of a pacemaker is indicated