What medications to take for treatment after coronary artery stenting surgery?
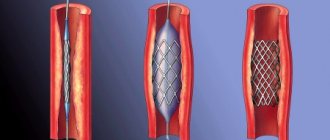
Stenting of the coronary arteries is a surgical operation on the vessels of the heart, during which the angiosurgeon from the inside, using a special balloon, expands the narrowed lumen of the vessel and installs a thin tube - a stent - into it.
As a result, blood flow is restored and angina attacks disappear. However, after stenting, continuous medication is required.
Medicines after a heart attack and stenting need to be taken for life, but some of them only for a year after the operation.
Taking medications after stenting may be even higher than before, due to increased antiplatelet (“blood thinning”) therapy.
It is believed that the long-term results of proper drug treatment of angina and stenting are the same. However, it is the installation of a stent that gives the patient a significant subjective improvement in condition.
Who receives free medicines?
After discharge from the hospital, the doctor gives written instructions for treatment. It is very important to follow it.
Typically, such patients are registered with a cardiologist and must visit him at least once a year.
If a patient has undergone stenting for a myocardial infarction, he is temporarily disabled, and after a certain time (usually six months) he undergoes a commission to determine the degree of disability.
After stenting without a heart attack, a “group” is usually not given, and the patient is forced to buy medications at his own expense.
Free medications after myocardial infarction and stenting are provided as part of government guarantees, but they are not always available in pharmacies. Therefore, many disabled people prefer to receive compensation in monetary terms.
It is worth understanding that over time, with good performance, the disability group can be removed. In this case, the person goes to work, and free medications after stenting the heart vessels are no longer given to him.
Thus, only patients with a disability group have the right to free medications after a myocardial infarction, including stenting. If the operation was performed for ordinary angina pectoris, the medications are purchased by the patient himself.
List of medications after stenting:
After stenting surgery, the patient is prescribed the following groups of medications:
- Antiplatelet. These medications reduce the risk of a blood clot forming inside the stent and causing it to become blocked.
- Statins. After stenting, patients with elevated cholesterol levels are prescribed statins or, less frequently, other cholesterol-lowering drugs.
- Other drugs. Prescribed by your doctor to reduce the risk of heart attack.
Antiplatelet drugs
Thrombosis can lead to myocardial infarction. Therefore, it is very important to take two antiplatelet drugs from the list presented:
- Aspirin (full analogues: Thrombo-ass, Ask-Cardio, Aspicard, Aspicor, Aspinat, Acetylsalicylic acid, Aspirin Cardio, Zorex Morning, CardiAsk, Sanovasc, Taspir, Thrombogard, Trombopol, Upsarin Upsa) in a dosage of 75 mg to 325 mg daily 1 time per day for life. Many of these drugs come in tablets that dissolve in the intestines, some in the form of effervescent tablets. This somewhat reduces the harmful effects of aspirin on the stomach.
- Clopidogrel (full analogues: Aggregal, Deplatt-75, Detromb, Zilt, Kardogrel, Cardutol, Clapitax, Clopigrant, Clopidex, Clopilet, Clopirel, Lirta, Listab 75, Lopirel, Pidogrel, Plavix, Plagril, Plogrel, Targetek, Troken, Trombex, Thromborel, Fluder, Egithromb). This drug is taken for a year after stenting at a dosage of 75 mg once a day and then discontinued.
There are also combination products that combine both of these drugs. Their use is more economically profitable:
- Acetylsalicylic acid + Clopidogrel (Russia);
- Clopigrant – A (India);
- Coplavix (France);
- Plagril A (India).
All questions about replacing a drug with an analogue or a combination should be resolved only with your doctor!
This dual therapy, aimed at preventing stent blockage, is dangerous due to excessive bleeding. Such complications occur in 1.7% of patients. This could be gastrointestinal bleeding, hemorrhagic strokes, intracerebral hematomas, bleeding from injection sites, and so on. If they appear, you cannot stop treatment on your own; you should urgently consult a doctor.
Aspirin is contraindicated in case of exacerbation of gastric ulcers, hemorrhagic diathesis, NSAID-dependent form of bronchial asthma, combined use with methotrexate at a dose of more than 15 mg per week, as well as in the 1st. and 3rd trimesters of pregnancy and during breastfeeding. In these cases, an individual approach to treatment after coronary stenting is required.
Drugs from the group of statins
After stenting, patients with elevated cholesterol levels are prescribed statins or, less frequently, other cholesterol-lowering drugs.
It has been proven that taking drugs from the statin group after stenting reduces the risk of any complications from the heart and blood vessels, as well as death from any other causes, by 30%.
Cholesterol is synthesized in the body mainly at night. Therefore, statins after stenting are prescribed in the evening during dinner in a dosage of 10 to 80 mg.
The goal of their appointment is to achieve a safe level of total cholesterol of 4.6 mmol/L or lower and low-density lipoproteins of less than 2.6 mmol/L.
This will help prevent not only blockage of the stent, but also the formation of atherosclerotic plaques in other arteries of the heart.
Drugs from the group of statins against the formation of atherosclerotic plaques are widely used for the treatment of men and women after coronary stenting surgery.
After every month of taking statins, you need to monitor your cholesterol and lipoprotein levels. If the target values are not achieved, the dosage is doubled.
Every six months when taking statins after stenting, you need to check the following blood parameters:
- total cholesterol and its fractions;
- triglycerides;
- ALT and AST.
This is necessary not only for assessing the effectiveness of treatment, but also for timely detection of the harmful effects of statins on the liver.
The following drugs from the group of statins are usually prescribed:
- Simvastatin (Vasilip, Zocor, Zocor Forte, Zorstat, Ovenkor, Simvahexal, Simvakol, Simvastol, Simvor, Simgal, Simlo, Sincard, Kholvasim);
- Lovastatin (Cardiostatin);
- Pravastatin;
- Atorvastatin (Anvistat, Atomax, Ator, Atoris, Atorvox, Vasator, Lipoford, Liprimar, Liptonorm, Novostat, Torvacard, Tulip);
- Rosuvastatin (Acorta, Crestor, Lipoprime, Mertenil, Reddistatin, Ro-statin, Rozart, Rosistark, Rosucard, Rozulip, Rozufast, Roxera, Rustor, Suvardio, Tevastor);
- Pitavastatin (Livazo).
Substances in this group are being actively studied. Many of them have specific application features, so it is impossible to independently replace one drug with another after stenting or myocardial infarction.
You also need to take into account that there are now many analogues on the market, mainly made in India. They are much cheaper than original drugs.
However, it is necessary in each case to clarify whether there have been studies on the comparative effectiveness of these funds.
Statins are not prescribed for active liver diseases (cancer, hepatitis, cirrhosis) and an increase in ALT and AST levels by more than 3 times, as well as in pregnant and lactating women. In these cases, it is necessary to individually select a cholesterol-lowering agent from another group (fibrates, ion-exchange resins, etc.).
Medicines for heart attack risk
Depending on the risk factors for heart attack, the doctor prescribes other medications after myocardial infarction and stenting:
- for high blood pressure - antihypertensive;
- for diabetes mellitus - hypoglycemic agents.
How many months do you take medications after stenting?
- clopidogrel for a year;
- statins – until cholesterol targets are achieved;
- other means - constantly.
With normal blood pressure, blood sugar and cholesterol levels, and good recovery after surgery, after a year the patient switches only to constant use of aspirin.
What can and cannot be done after surgery?
What can you do after stenting:
- morning exercises;
- calm walking for 30 – 60 minutes 3 – 4 days a week without effort;
- walking can be replaced by moderate exercise on a treadmill, exercise bike, swimming, skiing for a total duration of up to 6 hours per week;
- replace coffee with tea; if you cannot refuse this drink, you can afford 1 cup of coffee in the morning;
- from alcohol, you can only occasionally drink 50 ml of red wine, but it is advisable to refuse this too;
- eat more fish, seafood, sunflower, soybean, corn oils, vegetables and fruits, rye or bran bread, crackers, lean meat is allowed.
What not to do after stenting:
- lead a sedentary life;
- smoking or staying in smoky areas;
- drink strong alcoholic drinks and beer;
- eat eggs, fatty meats, cream and butter;
- consume more than 4 grams of table salt per day.
- Ignore a routine examination by your doctor.
- Independently replace one drug with another.
- Take medications from the statin group for cirrhosis and hepatitis.
- Use aspirin for the treatment of exacerbation of stomach ulcers or hemorrhagic diathesis.
- Purchase analogues of drugs that have not yet undergone medical research.
Combined with the right medications and regular visits to your doctor, these measures will help you recover from stenting and lead a completely normal, healthy life.
If you could not find the answer to your question in this article or you need to get more detailed information on a particular aspect, do not rush to leave.
( 22 ratings, average 4.82 out of 5 )
Source: https://PulsNorma.ru/serdtse-i-sosudy/lekarstva-posle-stentirovaniya.html
What can and cannot be done after surgery?
What can you do after stenting:
- morning exercises;
- calm walking for 30 - 60 minutes 3 - 4 days a week without effort;
- walking can be replaced by moderate exercise on a treadmill, exercise bike, swimming, skiing for a total duration of up to 6 hours per week;
- replace coffee with tea; if you cannot refuse this drink, you can afford 1 cup of coffee in the morning;
- from alcohol, you can only occasionally drink 50 ml of red wine, but it is advisable to refuse this too;
- eat more fish, seafood, sunflower, soybean, corn oils, vegetables and fruits, rye or bran bread, crackers, lean meat is allowed.
What not to do after stenting:
- lead a sedentary life;
- smoking or staying in smoky areas;
- drink strong alcoholic drinks and beer;
- eat eggs, fatty meats, cream and butter;
- consume more than 4 grams of table salt per day.
- Ignore a routine examination by your doctor.
- Independently replace one drug with another.
- Take medications from the statin group for cirrhosis and hepatitis.
- Use aspirin for the treatment of exacerbation of stomach ulcers or hemorrhagic diathesis.
- Purchase analogues of drugs that have not yet undergone medical research.
Combined with the right medications and regular visits to your doctor, these measures will help you recover from stenting and lead a completely normal, healthy life.
If you could not find the answer to your question in this article or you need to get more detailed information on a particular aspect, do not rush to leave.
Answers on questions
Mikhail Yakovlevich Ruda, Doctor of Medical Sciences, Professor:
– Now we will hold a short question and answer session.
Dear Sergey Alexandrovich. While there are questions here, I will use the microphone to ask you a question that, it seems to me, is closer to the issue of invasive treatment of patients who are in the “PLATO” group.
In this case, I mean a group of patients who are not very widely represented in our country, but will be more and more widely represented. These are patients who are expected to use coronary artery bypass grafting (CABG) as reperfusion therapy.
It seems to me that there are some ambiguities in determining the timing of use and discontinuation of drugs in connection with the operation. What I mean.
If the half-life of the drug is somewhere around 2 - 2.5 days, if in the design, in the study protocol it was recommended to stop the drug 24 - 72 hours before the corresponding intervention, which ultimately resulted in the recommendation to stop the drug 5-7 days before the start of the intervention .
There is some element of divergence here.
Sergey Aleksandrovich Abugov, Doctor of Medical Sciences, Professor:
– Mikhail Yakovlevich, I don’t have a categorical answer. There is a soft answer to this. As far as I understand, experiments have not been carried out with Clopidogrel, and the standard procedure is withdrawal 7 days in advance, this experience has been extended to Ticagrelor. If I’m wrong, my respected colleagues will correct me.
“PLATO” had recommendations about 24 – 72 hours in advance. But in reality the figure turned out to be about five days. When approved by the FDA, this figure of five days was chosen, which was not really studied
Mikhail Ruda: You don’t get the impression that such a recommendation will be a little disturbing. It will serve as a formal obstacle to, if necessary, starting intervention in patients earlier.
Sergey Abugov: I absolutely agree with you. It seems illogical, given the pharmacodynamics of the drug. But if a fact has not been studied in serious research, then we cannot make such recommendations. I think this fact requires further study.
The fact that it will slow down - yes. The first thing we expect from the drug is that this drug is reversible, with a very fast onset. We actually put it on the table. We get the effect very quickly. If we need to send a patient for CABG, we almost send him from the operating laboratory to the surgeon’s table.
03:39
Mikhail Ruda: How long to take Brilinta after PCI and stenting?
Sergey Abugov: I hope this is a question from the group led by Dr. Vlasova.
Year. We have no other information on this matter.
Mikhail Ruda: Decipher the concept of “reversible dyspnea syndrome during treatment with Clopidogrel.”
Sergey Abugov: “Ticagrelor”, naturally. Perhaps my colleagues were mistaken.
A certain number of patients experienced shortness of breath. But a small number of patients demanded its transfer to thienopyridines. This is the reversibility of shortness of breath. The fact that it arose and went away without changing antiplatelet therapy.
Mikhail Ruda: If Ticagrelor begins to act an hour after prescription, then why do differences in effectiveness appear after one to two months? Do differences in effectiveness only appear after one or two months?
Sergey Abugov: I showed a slide that was on a small scale. There a very significant divergence of the “curves” was shown. But a significant divergence of the “curves” occurs during the first 24 hours.
Mikhail Ruda: How long before an emergency PCI should a saturating dose be given? Amount of drug before elective PCI.
Sergey Abugov: We do not have any evidence base for planned PCI. In the Russian instructions for Ticagrelor, this drug is used in patients with ACS. The rest you decide based on this knowledge.
Like clopidogrel, Ticagrelor is given as early as possible in patients undergoing percutaneous coronary intervention or not. It also saves lives in patients who have not undergone percutaneous coronary intervention.
06:05
Mikhail Ruda: I’ll ask you a tricky question from me. How should we deal with this situation? A patient with ACS. He is being taken to the hospital. Should he be given Ticagrelor at the prehospital stage or not?
Here, on the one hand, the sooner you give Ticagrelor, the more likely, by the time the balloon is inflated, its effect will already appear. On the other hand, you don't know what you'll get on an angiogram. This patient may need to undergo CABG rather than angioplasty. What kind of CABG is it when you are already giving Ticagrelor.
Sergey Abugov: This is a very difficult question, Mikhail Yakovlevich. It should probably stand wider. Should an emergency patient receive heparin? If he should receive heparin, what kind. Does the ambulance take into account what drugs will be used in the clinic?
Will, for example, “Bivalirudin” be used? Will Ticagrelor be used? If there is serious continuity between the emergency and clinic phases, then that would probably be a good thing.
But in real life, when a line team is transported to a relatively unknown place with an unknown availability of a free operating room, the presence of a team on site, I think that the delay to the clinic doors is acceptable.
Mikhail Ruda: If we take the optimal option. We are located in a city where an ideal treatment plan is possible. The patient will be admitted to a specialized center where full treatment capabilities are available. Do we give Ticagrelor at the prehospital stage or not?
Sergey Abugov: We do not have an evidence base on this matter, so I can only express my own judgment. If all our services have continuity, probably yes.
Emergency CABG, after all, can be performed in the conditions (inaudible, 08:39). Our clinic has quite a lot of experience in such operations.
08:47
Male voice: I will take the opposite point of view regarding pre-hospital Ticagrelor. The medicine must be used in the conditions in which it was studied.
The population of patients encountered by the ambulance is not the same population that is ultimately treated for ACS in the hospital. This is a much broader definition. Many more patients are admitted with chest pain of other origins. It was studied in a hospital, which means it should be given in a hospital. This applies to Ticagrelor.
Mikhail Ruda: I think that you are right from the point of view that we live in an era of evidence-based medicine. It is necessary to recommend to practicing doctors only what has actually been proven.
But if you think about it. If you present some kind of working hypothesis, which may or may not be subsequently investigated.
Sergey Abugov: It seems to me that in any case, giving Ticagrelor to a patient who does not need antiplatelet agents, and not giving it to a patient who needs antiplatelet agents, would probably be of greater benefit to give Ticagrelor than not to give it. I would still be in that position.
I understand perfectly what Oleg Valerievich says. This is evidence-based medicine. What percentage of you experience chest pain? One hundred?
Mikhail Ruda: We have people who want to ask a live question.
Male voice: Sergey Alexandrovich, my name is (Unintelligible, 10:42) Alexey Mikhailovich, chief cardiologist of Russian Railways. This is the question.
Without any exaggeration, you are the No. 1 specialist in coronary artery intervention in our country. A purely practical task.
Do you have experience combining Ticagrelor with modern parenteral platelet inhibitors? “Angioks”, “Rutsaramb”. Does the use of parenteral forms of modern antithrombotic drugs and such a modern drug as Brilinta increase the risk of bleeding?
Sergey Abugov: Alexey Mikhailovich, the answer is double. No, it doesn't increase it. No, I have no experience. No one in Russia has experience with Ticagrelor. According to “PLATO”. In “PLATO” there were patients who received Bivalirudin. 30% (or 20%) of patients who received 2B3A inhibitors. Bleeding did not increase.
11:57
Mikhail Ruda: In the PLATO study, an additional dose of 90 mg of Ticagrelor was allowed in addition to the loading dose during the period of percutaneous coronary intervention. What could this be connected with?
Sergey Abugov: I don’t know this information. I think this means an additional loading dose of Clopidogrel. An additional dose of 300 mg in patients who received 300 mg of Clopidogrel. There were no such patients at PLATO.
Mikhail Ruda: Is it possible to prescribe Clopidogrel and Ticagrelor for hemophthalmia? Contraindications to “Aspirin” (“Acetylsalicylic acid”) and “Curantil”.
Sergey Abugov: Is hemophthalmos caused by an eye injury? Any bleeding is relative in some cases and an absolute contraindication for antiplatelet agents.
Mikhail Ruda: In general, according to the classification, hemophthalmos refers to serious bleeding. Serious bleeding is a contraindication.
Brilinta is positioned as an effective replacement for Plavix. When using Brilinta, did the percentage of patients with contrast-induced acute renal failure increase?
Sergey Abugov: No, it has not increased. Although a greater negative effect on glomerular filtration rate was indeed noted with Ticagrelor.
Mikhail Ruda: But at the same time, it must be said that the insert that accompanies these boxes of Brilinta is quite liberal about the use of the drug for even moderate degrees of renal failure and in patients over 75 years of age.
Sergey Abugov: It says: “With caution in patients with altered glomerular filtration rate. But this is not about the fact that Ticagrelor aggravates contrast-induced nephropathy. The point is that he himself has some influence.
Mikhail Ruda: The higher the creatinine level, the more likely the likelihood of developing kidney damage also increases.
During PCI with the beam tube on, do your surgeons and you use protection? Do you wear special suits? Do you close the door to the angiooperative room? What do you think about the dangers of radiation?
Sergey Abugov: Yes, we use protection. No, we don't close the door because the dose falls proportionally to the square of the distance. We measured this dose. We know at which point in the operating room what quantity is located.
Recently we have begun to use additional screens very widely (both lower and upper screens). Roman Sergeevich Polyakov should be present here in the hall. At one time he tried to wear a lead cap. But it turned out to be very difficult. They are like that.
I'm trying to somehow connect this with Ticagrelor. But I can't do it.
Mikhail Ruda: Dear colleagues, if there are no more questions, allow me to thank Sergei Alexandrovich for the interesting message.
Source: https://internist.ru/publications/detail/6966/
Brilinta – No. 1 choice in cardiology
Brilinta - what kind of drug is it? Brilinta - what is it used for in cardiology? Brilinta – what does it help with and for what diseases is it prescribed? Brilinta – how to take it correctly? Brilinta: complications of Brilinta: drug withdrawal Brilinta: contraindications for use
Pathology of the cardiovascular system ranks first in the structure of diseases in almost all countries of the world. Moreover, it is heart disease that leads to the greatest number of deaths of patients both at home and in hospital hospitals.
The provoking factors of cardiovascular pathology are, first of all, a person’s lifestyle and hereditary predisposition.
Fortunately, pharmacologists together with cardiologists have developed a universal method for the prevention of heart diseases, in particular atherosclerosis and myocardial infarction. This is the prescription of antiplatelet agents - drugs that prevent the occurrence of blood clots and improve blood flow.
Brilinta is one of the best medicines that has these properties. Why is Brilinta needed, how to take it correctly and what side effects may occur when treated with this medication?
Brilinta - what kind of drug is it?
Brilinta is an antithrombotic drug prescribed for the treatment and prevention of many cardiovascular diseases. The active component of the drug is ticagrelor, an antagonist of special receptors that are located on the membrane of blood platelets.
The clinical effectiveness and safety of Brilinta have been confirmed in multiple studies.
Therefore, the drug can be safely taken by patients with various pathologies not only of the heart and blood vessels, but also of the kidneys, liver and other organs. In general, Brilinta is well tolerated by the body and causes virtually no complications.
Metabolism of the drug occurs in the liver. Brilinta metabolites then enter the bile and are excreted in the feces.
Brilinta - what is it used for in cardiology?
The active component of the drug, ticagrelor, acts on blood platelets and prevents their aggregation, that is, sticking together.
Thanks to this property of the active substance, Brilinta thins the blood, improves its rheological properties and fluidity, and prevents the formation of blood clots that can clog the vessel and cause ischemia (strokes, myocardial infarction).
Brilinta also slightly reduces blood pressure, due to the expansion of the walls of blood vessels, and prevents the deposition of low-density lipoproteins on them.
Brilinta – what does it help with and for what diseases is it prescribed?
The drug Brilinta for treatment and prevention is prescribed in combination with aspirin (acetylsalicylic acid) for the following diseases of the cardiovascular system:
- with ACS (acute coronary syndrome, including angina at rest and angina at exertion);
- with myocardial infarction;
- with atherosclerosis with the presence of blood clots in the lumen of blood vessels;
- with IHD (coronary heart disease);
- for arrhythmias;
- with arterial hypertension;
- during stenting.
Brilinta – how to take it correctly?
The loading dose of Brilinta is 120-180 mg per day. It is recommended to drink Brilinta in two doses:
- for ACS – 90 mg 2 times a day;
- for myocardial infarction - 60 mg 2 times a day.
Acetylsalicylic acid in a dosage of 75-150 mg per day is a drug that must also be used in combination with the drug Brilinta. How long to take the medication is determined by the attending physician. The duration of treatment depends on the disease and the severity of its course. For example, for ACS, the course of treatment is 12 months, and for myocardial infarction – up to 3 years.
Brilinta: complications
Although Brilinta is well tolerated by the body and has a pronounced clinical effect, it can cause side effects. Most often, when treated with this drug, the following occur:
- dyspnea;
- bleeding;
- increased levels of uric acid in the blood;
- headache and dizziness;
- loss of consciousness;
- decrease in blood pressure.
If adverse reactions occur while taking Brilint, you should consult your doctor. He will prescribe symptomatic therapy and reduce the dose of the drug or replace it with another analogue.
Brilinta: drug withdrawal
Withdrawal before surgery is the most common case when stopping Brilinta. Also, if the patient is indicated for stent installation, stop drinking Brilinta the day before the scheduled date of surgery. However, after stenting, antiplatelet therapy is immediately resumed.
In general, if it is necessary to complete treatment with Brilinta completely, discontinuation of the drug is carried out gradually. This is due to the high risk of bleeding during spontaneous withdrawal of Brilinta.
special instructions
Before starting Brilinta therapy, a careful assessment of the balance between the benefits of preventing atherothrombotic events and the possible threat of bleeding is required.
There is no data confirming the hemostatic effectiveness of platelet transfusions during the use of ticagrelor. Brilinta is capable of inhibiting transfused platelets in the blood.
The use of recombinant activated factor VIIa and/or antifibrinolytic treatment (aminocaproic or tranexamic acid) can lead to increased hemostasis. After determining the cause of bleeding and stopping it, it is possible to resume taking Brilinta.
Before undergoing elective surgery or using new medications, the attending physician must be informed about ticagrelor therapy. If a surgical procedure is scheduled for which an antithrombotic effect is not desired, Brilinta should be discontinued 7 days before surgery.
During CABG, the incidence of major bleeding with ticagrelor was the same as with clopidogrel on all days after discontinuation of therapy, with the exception of the first day, when the likelihood of major bleeding was higher with Brilinta.
The shortness of breath that occurs during treatment is usually mild or moderate in nature and resolves during therapy.
During Brilinta therapy, an increase in creatinine levels is possible, and therefore it is recommended to use the drug with extreme caution (assessing renal function) during concomitant treatment with angiotensin receptor antagonists.
Impact on the ability to drive vehicles and complex mechanisms
The effect of Brilinta on the ability to drive vehicles and other complex mechanisms has not been studied.
Given the likelihood of developing dizziness and confusion during ACS therapy, it is recommended to exercise caution when driving vehicles and operating any machinery.