HOLLOW VEINS
[
venae cavae;
vena cava superior (PNA, BNA),
vena cava cranialis
(JNA);
vena cava inferior
(PNA, BNA),
vena cava caudalis
(JNA)] - the main venous trunks (superior and inferior vena cava), collecting blood from the entire body and flowing into the heart.
Upper P. v. collects blood from the head, neck, chest and upper extremities and flows into the right atrium. The lower venous vein is the largest venous trunk of the human body; it collects blood from the lower extremities, organs and walls of the pelvis and abdominal cavity and also flows into the right atrium.
Ancient anatomists mentioned only one P. v. Thus, K. Galen described the beginning of the vena cava from the liver, and the vein is divided into ascending and descending parts. Ibn Sina was of the same opinion, and only A. Vesalius pointed out the connection between the vein and the heart.
Comparative anatomy
For the first time, the posterior (lower) P. v. in phylogeny it appears in lobe-finned ganoids and double-breeding fishes in the form of an unpaired venous trunk flowing into the right atrium. In mammals, the renal portal system completely disappears, and the posterior (lower) renal v. acquires predominant importance compared to the posterior cardinal veins. The common cardinal veins (ducts of Cuvier) therefore carry blood from the anterior half of the body, head, neck and forelimbs. The large trunk, formed as a result of the fusion of the veins of the head, neck and forelimbs and flowing into the heart, is called the anterior (upper) P. v.
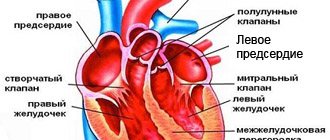
Only the heart is more important
In order to understand the vascular system of the heart, you need to know a little about its structure. The four-chambered human heart is divided by a septum into 2 halves: left and right. Each half has an atrium and a ventricle. They are also separated by a septum, but with valves that allow the heart to pump blood. The venous apparatus of the heart is represented by four veins: two vessels (superior and inferior vena cava) flow into the right atrium, and two pulmonary vessels into the left.
The circulatory system in the heart is also represented by the aorta and pulmonary trunk. The aorta, which extends from the left ventricle, supplies blood to all organs and tissues of the human body, except the lungs. From the right ventricle through the pulmonary artery, blood moves through the pulmonary circulation, feeding the bronchi and alveoli of the lung. This is how blood circulates in our body.
Embryology
Rice.
1. Schematic representation of some stages of the development of the vena cava in humans (a - embryo 4 weeks, b - embryo 8 weeks, c - fetus before birth): 1 - anterior cardinal vein, 2 - common cardinal vein, 3 - umbilical vein, 4 - vitelline-mesenteric vein, 5 - subcardinal vein, 6 - posterior cardinal vein, 7 - venous plexus of the primary kidney, 8 - liver, 9 - heart, 10 - external jugular vein, 11 - superior vena cava, 12 - azygos vein, 13 - hemizygos vein, 14 - inferior vena cava, 15 - adrenal vein, 16 - disappearing (reducing) vessels of the primary kidney, 17 - intercostal veins, 18 - right subclavian vein, 19 - right internal jugular vein, 20 - left brachiocephalic vein, 21 - left subclavian vein, 22 - coronary sinus of the heart, 23 - accessory hemizygos vein, 24 - adrenal gland, 25 - renal vein, 26 - left testicular (ovarian) vein, 27 - common iliac vein, 28 - external iliac vein, 29 - right brachiocephalic vein vein. In the early stages of ontogenetic development (4 weeks), bilateral symmetry of the systemic veins is characteristic. The main change during the development of the venous system is a change in the direction of blood flow from the left half of the body to the cardinal veins lying on the right, and the formation of unpaired venous trunks. As a result of complex transformations associated with changes in the direction of blood flow, the upper P. v. formed from the proximal part of the anterior right cardinal vein and the common right cardinal vein. Development of the lower P. v. associated with the expansion and lengthening of initially small veins of the abdominal cavity as a result of reduction of the posterior cardinal veins. Depending on from which veins or groups of veins the section of the lower P. v. is formed, it is divided into mesenteric, hepatic and postrenal parts, merging by the end of the 8th week. embryonic development into a single trunk (Fig. 1).
Characteristic
This system also includes the jugular vein, which carries waste blood from the vascular bed of the head and neck.
The vein has a wide trunk and fairly thin walls, due to which it expands and contracts without hindrance.
The beginning of the vessel emerges from the jugular foramen of the skull, uniting with the vagus nerve and the carotid artery.
The fusion forms a neurovascular bundle.
The jugular vein includes intracranial and extracranial tributaries. Its main function is to prevent blood stagnation in the brain structures of the brain.
Intracranial.
- Meningeal vessels.
- Veins of the inner ear.
- A network of vessels that carries blood flow to the eye orbits.
- Network of vessels of brain structures.
- Diploic vessels that supply blood to the bones of the skull.
This vascular network is responsible for supplying blood to the dura maters of the brain and does not have valves.
Extracranial.
- The facial vein, which carries blood from the cheeks, earlobes and lip folds.
- Submandibular vessel.
The internal jugular vein includes the pharyngeal, thyroid and lingual veins.
The vessels of the upper extremities are deep and subcutaneous, collect blood from the subcutaneous layers and are equipped with valves. Connecting with each other, they form a venous network.
The main vein arises from the palmar arch and passes through the forearm, dividing into the ulnar and radial vessels.
In the area of the shoulder joint, the vessels unite, forming at the exit two brachial veins, which pass into the axillary veins.
The axillary vein does not form a branch; it is continued by the subclavian vein, which is securely attached to the periosteum of the rib.
The vein expands its lumen when the arm is raised, making it possible to drain blood from the upper limb.
The venous vessels of the chest pass through the intercostal spaces, collecting blood from the chest cavity and abdominal wall.
Intervertebral weaves belong to the tributaries of these vessels and run from the back of the head to the sacral bone.
Anatomy
Rice.
2. Schematic representation of some variants of the formation of the superior vena cava and its sources: a - symmetrically developed internal jugular veins (short trunk of the right brachiocephalic vein), b - asymmetry in the development of the internal jugular veins (long trunk of the right brachiocephalic vein); 1 - internal jugular veins, 2 - right brachiocephalic vein, 3 - left brachiocephalic vein, 4 - superior vena cava. Superior vena cava
- a short trunk located in the thoracic cavity, in the upper mediastinum (see). It begins at the level of the cartilage of the first rib at the right edge of the sternum from the confluence of the right and left brachiocephalic veins (vv. brachiocephalicae dext, et sin.). Heading down, it flows into the right atrium at the level of the cartilage of the right third rib. To the left of it is the ascending part of the aorta, to the right it is partially covered by the mediastinal pleura and is adjacent to the right lung. The right phrenic nerve passes through this location. Behind the upper P. v. the root of the right lung is located. At the level of the cartilage of the right second rib, it is covered by the pericardium. Before entering the pericardial cavity in the upper P. v. The azygos vein (v. azygos) flows into it. Some options for the formation of the upper P. v. and its origins are presented in Fig. 2.
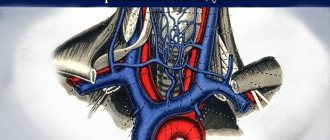
Inferior vena cava
begins in the abdominal cavity from the confluence of the right and left common iliac veins (vv. iliacae communes dext, et sin.) at the level of LIV-V and goes up to the right of the aorta, deviating from it to the right to the diaphragm.
At this point it lies in the groove of the inferior vena cava of the liver, and then through an opening in the tendon center of the diaphragm it passes into the chest cavity and flows into the right atrium. Rice.
3. Schematic representation of the trunk and tributaries of the inferior vena cava, the abdominal part of the aorta and its branches: 1 - inferior phrenic artery, 2 - left adrenal gland, 3 - left adrenal vein, 4 - left renal artery, 5 - kidney, 6 - left renal vein , 7 - superior mesenteric artery, 8 - aorta (abdominal part), 9 - inferior mesenteric artery, 10 - left ascending lumbar vein, 11 - left common iliac artery and vein, 12 - median sacral arteries and vein, 13 - right common iliac artery and vein, 14 - right ascending lumbar vein, 15 - right lumbar arteries and veins, 16 - right testicular (ovarian) artery, 17 - right testicular (ovarian) vein, 18 - right renal vein, 19 - right renal artery, 20 - celiac trunk, 21 - inferior vena cava, 22 - hepatic veins. In the lower P. century. drain (Fig. 3) lumbar veins (vv. lumbales), right testicular or ovarian vein (v. testicularis dext. s. ovarica dext.), renal veins (vv. renales), right adrenal vein (v. Suprarenalis dext.) , inferior phrenic veins (vv. phrenicae inf.) and hepatic veins (vv. hepaticae). At the confluence with the lower P. v. of the left hepatic vein lies the venous ligament (lig. venosum), the remnant of the ductus venosus (see).
In a wedge, in practice, it is customary to distinguish the following sections of the lower P. v.: infrarenal, renal (or renal), hepatic.
Rice. 1. Human veins (the portal vein and its tributaries are indicated by thick black stripes). Connections of tributaries of the portal vein with tributaries of the superior and inferior vena cava (cavo-portal anastomoses - at the junction of the black and light elements of the picture): 1 - v. subclavia; 2 - v. jugularis int.; 3—v. brachiocephalica dext.; 4 - v. brachiocephalica sin.; 5 - v. cava sup.; 6 - vv. intercostales post.; 7 - v. hemiazygos accessoria; 8 - v. hemiazygos; 9—v. lienalis; 10 - v. lumbalis ascendens; 11—v. renalis; 12 - v. cava inf.; 13 - v. mesenterica inf.; 14 - v. testicularis; 15 - v. rectalis sup.; 16 - v. iliaca communis; 17 - v. iliaca ext.; 18 - v. iliaca int.; 19 - v. epigastrica superficialis; 20 - v. epigastrica inf.; 21 - vv. paraumbilicales; 22 - v. mesenterica sup.; 23 - v. portae; 24 - v. epigastrica sup.; 25 - vv. esophagae; 26 - v. thoracoepigastrica; 27 - v. thoracica int.; 28 - v. azygos.
Anastomoses
. Anastomoses of the roots of the upper and lower P. are of great practical importance. between themselves and with the roots of the veins, which are tributaries of the portal vein (see Fig. 1). They are observed ch. arr. in the area of the anterior and posterior walls of the chest and abdominal cavities, as well as in a number of organs (for example, in the esophagus, rectum).
Blood supply
. Arteries and veins of the walls of the P. v. are branches and tributaries of nearby large arteries and veins. In the outer shell of P. v. arteries and veins form plexuses, due to which all layers of the walls of the P. v. are supplied with blood. According to V. Ya. Bocharov (1968), in the middle shell of the lower P. v. arterioles and a three-dimensional network of capillaries lie. In this layer, venules are formed that flow into the veins of the outer shell. In the subintimal layer of the wall of the lower P. v. There is a planar network of blood capillaries. Wall of the upper P. v. differs in a smaller number of intramural blood vessels than the wall of the lower P. v. This circumstance is explained by the smaller number of muscle elements in its wall. I.M. Yarovaya (1971) indicates that the network of blood capillaries in the wall of the upper ventricle. thickens towards the heart.
Lymphatic drainage
. Lymph. capillaries and vessels form in the walls of the P. v. networks and plexuses located mainly in the outer and also in the middle shell. The draining lymph vessels flow into nearby lymph, collectors and nodes.
Innervation
complex. Nonidez (J. Nonidez) was the first to show two types of nerve endings in the walls of the venous v., and morphologically substantiated the origin of the Bainbridge reflex (increased heart contractions in response to an increase in venous blood flow). B. A. Dolgo-Saburov described P. v. in all membranes. nerve plexuses, especially well expressed in the middle. In the outer shell of P. v. nerve cells were found. According to V.V. Kupriyanov et al. (1979), in the wall of the lower P. v. they are represented by spinal type afferent neurons and Dogel type II cells, as well as efferent autonomic multipolar neurons. Neurons with high cholinesterase activity (parasympathetic) are found predominantly in areas of the P. v. close to the heart; extensive accumulations of adrenergic (sympathetic) neurons are found throughout its entire length. Adrenergic nerve fibers accompany blood vessels and form plexuses in the outer membrane and among smooth muscle cells. Cholinergic system of conductors in the wall of the lower P. v. It is represented by large nerve bundles and forms plexuses that penetrate all membranes. In the wall of the P. v. Various types of encapsulated and non-encapsulated receptors were found, as well as areas of their predominant accumulation, especially near the heart, and in the lower half of the vein, in addition, in the area of the confluence of the renal and the confluence of the common iliac veins.
Pelvic veins - characteristics, functions, pathologies
In the human body, everything is interconnected and you simply cannot do without veins and arteries. These important vessels help the body function properly. For example, the veins of the pelvis collect blood from the tissues of the lower peritoneum. Then they direct it to the heart.
What it is
The anatomy of the pelvic veins is quite simple. There are a pair of common iliac veins. They are adjacent to the external and internal iliac. They unite and move into the lower hollow.
Plexuses are located in the area of tributaries of the internal iliac vein.
They have specific names:
- vaginal, which passes into the place where the uterine venous plexus of the small pelvis is located;
- prostatic;
- vesical;
- rectal;
- sacral
The following veins are adjacent to the tributaries:
- ovarian;
- renal;
- adrenal;
- hepatic;
- iliopsoas;
- lower and upper gluteals;
- lateral sacral;
- obturator.
The deep veins of the legs include: femoral, deep, popliteal, anterior and posterior tibial and peroneal.
Characteristic
These vessels mainly accompany the pelvic arteries and have many valves. Veins intertwine internal organs, creating plexuses. From the pelvic organs, blood flows through the iliac veins into the inferior vena cava.
External iliac
The external iliac vein is a vessel that is a continuation of the femoral vein. It originates in the area of the inguinal ligament and is directed to the sacroiliac joint.
The inferior epigastric and deep veins adjoin it.
The first collects blood from the lower part of the peritoneum, and into the second it flows from the sides.
Internal iliac
This name is given to a rather large vessel that passes behind the artery of the same name. Collects blood from the pelvic organs.
In most cases there are no valves. It is a thick short trunk.
Common iliac
This vessel has a pair. It originates in the area of the sacroiliac joint.
The left common iliac vein is longer than the right.
Bottom hollow
It includes both common iliacs. It is the thickest venous trunk and is located behind the peritoneum.
Rising upward, it flows into the right atrium.
Where is blood collected from?
Blood enters the veins of the uterus from the uterine plexus, which surrounds it. The vesical veins carry blood from the sides of the bladder and its bottom.
The most complex outflow is from the plexus of the lower rectum. Blood in this area flows through three pathways that connect to each other in the walls of the rectum.
Based on the diagrams of the veins of the pelvis and lower extremities, you can see that they are connected by multiple anastomoses.
Where do they flow
They carry blood from the tissues and organs of the abdominal cavity to the heart. The inferior vena cava and portal vein play a major role in this case.
The first takes in blood from the internal organs, gonads and liver. It passes along the right wall of the abdomen to the right of the aorta.
Main functions
Their function is to ensure normal blood circulation in internal organs and tissues. Disruptions in blood flow or expansion and lengthening of the pelvic veins can lead to the formation of various diseases.
They participate in the absorption of nutrients by tissues and help remove waste products through the urinary system.
What doctors treat diseases
If you suspect a disease, you should contact a phlebologist or andrologist.
If pain occurs in the lower abdomen, women should consult a gynecologist.
If there are any complications, it would be useful to undergo an additional examination by a neurologist and urologist.
The treatment involves: a physical education specialist, a physiotherapist, and a nutritionist. In some cases, the assistance of a vascular surgeon may be required.
Possible pathologies and their symptoms
Most vein damage occurs in the groin, buttocks and back of the thighs. Sometimes pathologies are formed due to congestion of the venous plexus of the bladder.
There are no particularly pronounced symptoms of dilated pelvic veins at the initial stage of the disease. But, as the disease progresses, women may experience:
- severe pain in the middle of the menstrual cycle, in a lying position and during sexual intercourse;
- severe premenstrual syndrome;
- disruptions in the menstrual cycle;
- heavy discharge;
- frequent spontaneous abortions;
- urinary disorders.
Also, dilated blood vessels are visible to the naked eye on the thighs, buttocks and groin.
Men experience aching pain in the perineum and lower abdomen, radiating to the lumbar area. It intensifies after vigorous activity and ejaculation.
Visually, the pathology can be recognized by the swollen scrotum and perineum.
Damage to the pelvic veins can be either congenital or acquired. In the first case, the walls of blood vessels expand at the genetic level. In the second, for pathologies of connective tissue or the presence of neoplasms, under the influence of blood pressure.
Such vascular deformation can lead to the formation of blood clots or inflammation of the vessel walls.
Doctors also attribute poor nutrition and an inactive lifestyle to the causes of varicose veins of the small pelvis.
In women, the main factors that provoke the disease are difficult working conditions, pregnancy and childbirth, and gynecological diseases.
Hormone replacement therapy and oral contraception can influence the occurrence of pathology.
Thrombosis of the iliac vein is more common than those localized in other places. This is an extremely serious disease that can be fatal.
It manifests itself as pain in the groin, legs, and increased venous pressure.
One of the reasons for the formation of the disease is a slowdown in blood flow. Thrombosis can occur when blood vessels are damaged or due to blood clotting pathology.
Diagnostic methods
If a developing pathology is suspected, a certain diagnosis is prescribed.
Consists of a complex of several procedures.
- Ultrasound and Doppler examination. They allow you to detect varicose veins.
- Phlebography. During the examination, a special solution is injected into the venous network, after which a series of X-rays are taken. This helps to see the sites of vascular damage.
- Laparoscopy. Usually prescribed to clarify the diagnosis.
- Selective ovariography. Helps identify valvular insufficiency.
- CT and MRI. They allow you to see the course of the disease in more detail and help distinguish it from other non-gynecological pathologies.
Upon visual examination, varicose nodes are visible on the labia and inner thighs of women. By touch you can detect an enlarged uterus and ovaries.
The speculum shows a hypertrophied, bluish cervix.
Varicose veins of the pelvis are quite a serious disease. Without timely treatment, it can lead to enlarged blood vessels of the reproductive organs, infertility and the inability to carry a pregnancy to term in women.
Against the background of pain, neurasthenia may develop. The most serious complications are venous thrombosis and pulmonary embolism.
Any appearance of pain in the lower abdomen cannot be ignored.
: inferior vena cava and its tributaries
Source: https://venaprof.ru/veny-taza/
Histology
Rice.
4. Microscopic specimen of the wall of the human inferior vena cava (cross-section): I - inner membrane, II - middle membrane, III - outer membrane; 1 - smooth muscle cells, 2 - bundles of longitudinally running smooth muscle cells, 3 - connective tissue, 4 - vascular vessels; hematoxylin-eosin staining; x 130. Gistol, structure of the walls of the upper and lower P. v. not the same due to their different functional load. The thickness of the wall of the upper p. in the extrapericardial part of an adult, 300-500 µm. In the wall of the upper P. v. the border between the inner and middle shells is not clearly defined. The middle shell contains a small number of circular bundles of smooth muscle cells, separated by layers of connective tissue, passing into the outer shell, the edges are 3-4 times thicker than the inner and middle shell combined. Bundles of collagen fibers in its composition have a predominantly oblique and circular direction, while elastic fibers have a longitudinal direction. In the middle shell of the lower P. v. Circularly arranged bundles of smooth muscle cells are clearly visible. The outer shell contains a large number of longitudinally arranged bundles of smooth muscle cells, separated by layers of connective tissue and makes up 3/5 of the thickness of the entire wall (Fig. 4). According to V. Ya. Bocharov (1968), the middle shell differs from the outer shell in a smaller number of connective tissue elements and thinner bundles of smooth muscle cells. In the inner shell, a layer of elastic fibers is detected, and at the border of the inner and middle shells there is a thin layer of connective tissue with a predominance of collagen fibers. At the confluence of the upper and lower P. v. in the heart, striated muscle fibers of the myocardium penetrate into their outer shell.
According to Bucciante (L. Bucciante, 1966), in newborns in the walls of the veins of the abdominal cavity, in particular in the lower abdominal cavity, there are only circular bundles of smooth muscle cells. After the birth of improvement in the wall II. V. in humans they are expressed in changes in the number, position and orientation of muscle cells. Longitudinal bundles of smooth muscle cells appear in the wall of the P. v. only after birth. Thus, it was noted that in a 7-year-old child in the wall of the lower P. v. the circular and longitudinal layers of smooth muscle cells are well developed. In the wall of the upper P. v. in a newborn, the muscle elements are very weakly represented, and only by the age of 10 do circular bundles of smooth muscle cells appear. Age-related hypertrophy and hyperplasia of muscle elements in the wall of the P. v. have been established. In old age, a decrease in circularly located smooth muscle cells is observed, and after 70 years, their atrophy. According to Bucciante (1966), elastic membranes in the subendothelial layer also become well defined by the age of 10 years. Elastic elements of the wall of the P. v. in the process of aging they thicken and undergo dystrophic changes. The number of collagen fibers in the subendothelial layer increases, as well as between the muscle bundles in the middle and outer membranes.
Diagnostic methods
If a developing pathology is suspected, a certain diagnosis is prescribed.
Consists of a complex of several procedures.
- Ultrasound and Doppler examination. They allow you to detect varicose veins.
- Phlebography. During the examination, a special solution is injected into the venous network, after which a series of X-rays are taken. This helps to see the sites of vascular damage.
- Laparoscopy. Usually prescribed to clarify the diagnosis.
- Selective ovariography. Helps identify valvular insufficiency.
- and MRI. They allow you to see the course of the disease in more detail and help distinguish it from other non-gynecological pathologies.
Upon visual examination, varicose nodes are visible on the labia and inner thighs of women. By touch you can detect an enlarged uterus and ovaries.
The speculum shows a hypertrophied, bluish cervix.
Varicose veins of the pelvis are quite a serious disease. Without timely treatment, it can lead to enlarged blood vessels of the reproductive organs, infertility and the inability to carry a pregnancy to term in women.
Against the background of pain, neurasthenia may develop. The most serious complications are venous thrombosis and pulmonary embolism.
Any appearance of pain in the lower abdomen cannot be ignored.
Research methods
Rice.
5. Diagram of chest x-ray: a - direct projection, the superior vena cava is adjacent to the ascending aorta (shaded), b - lateral projection, the inferior vena cava in the form of a triangle is visible between the infero-posterior contour of the heart and the diaphragm (shaded). Conventional wedge methods (examination, changes in skin color, measurement of the circumference of the upper limb, etc.) allow one to suspect various pathologies of P. v. The main diagnostic method is x-ray, ch. arr. X-ray contrast study of P. v. - cavography (see). On a direct radiograph, the upper P. v. together with the ascending aorta it forms the right border of the vascular shadow (Fig. 5, a). When the upper P. v. expands, for example, with a defect of the right atrioventricular (tricuspid) valve or when the vein is displaced to the right, the contour of the vascular shadow shifts to the right. In the first oblique position, the shadow of the lower P. v. can be visible in the form of a strip running from the diaphragm to the posterior contour of the heart, and in a lateral position - in the form of a triangle between the shadow of the heart and the contour of the diaphragm (Fig. 5, b). The absence of a triangle indicates an enlargement of the left ventricle of the heart.
Superior cavography can be performed in an antegrade or retrograde manner. In the first case, a radiopaque substance is administered by puncture or catheterization of the veins of the shoulder or subclavian vein on one or both sides (see Puncture catheterization of veins). For retrograde contrasting of the upper P. century. the catheter is passed through the femoral, external and common iliac, and lower p. and the right atrium (see Seldinger method).
Rice. 6. Angiocardiogram (direct projection): 1 - left subclavian vein, 2 - left brachiocephalic vein, 3 - superior vena cava, 4 - right atrium, 5 - inferior vena cava (contrasted due to reflux).
On the angiocardiogram in a direct projection (Fig. 6) the contrasted upper P. v. serves as a continuation of two brachiocephalic veins, merging with each other below the right sternoclavicular joint; it is located to the right of the shadow of the spine and has the appearance of a clearly defined strip with a width of 7 to 22 mm (depending on age). At the level of the 3rd rib, the shadow of the upper P. v. passes into the shadow of the right atrium. In the first oblique position, the upper P. v. occupies the anterior section of the vascular shadow; in the second oblique position, its shadow is located slightly posterior to the anterior contour of the aorta. In direct projection, contrasted lower P. v. lies to the right of the spine, slightly overlapping it; in the lateral projection it is located in front of the lumbar region, and its upper section deviates anteriorly and flows into the right atrium.
Inferior cavography can also be done antegrade or retrograde. In the first case, a radiopaque substance is administered by puncture or catheterization of the femoral vein on one or both sides. For retrograde cavography, the catheter is inserted into the lower P. v. through the subclavian, brachiocephalic, upper P. v. and right atrium.
Diseases
Deprived of nutrients, blood from the superior vena cava enters the right side of the heart through the venous trunk.
Failure of blood circulation often occurs due to a pathological focus in the body or when a vein thromboses.
Congenital pathological anomalies of the vascular apparatus of the heart occur - an additional left superior vena cava is formed, where it is located as an ineffective inflow of the left atrium.
Pathologies of the venous network are summarized by the name - superior vena cava syndrome.
The syndrome combines many symptoms of impaired venous functioning and poses a threat to the patient’s life.
Superior vena cava syndrome occurs as a primary disease - the integrity of the vessel is compromised, resulting in a sharp rise in venous pressure.
In case of a secondary disease, concomitant diseases are the cause, putting strong pressure on the vessel.
The main cause of pressure on the vessel is a tumor process or blockage with a blood clot, which causes a rise in pressure and a dangerous complication in the form of rupture of the vessel.
Symptoms of the pathology increase gradually.
A typical clinical picture of the pathology is presented below.
- Dizziness.
- Pain in the head area.
- Pain behind the sternum.
- Loss of consciousness.
- Swelling of the face.
- Enlarged and swollen veins in the neck.
- Cyanotic bluish face.
It is possible to identify the cause of the failure of venous circulation with the help of diagnostic studies.