What is this department and where is it located?
Anatomy
The structure of the left atrium, like the right, is similar to an irregular cube.
Chamber walls:
- The anterior one protrudes and forms the left ear, which is adjacent to the pulmonary trunk on the left.
- Rear.
- Upper.
- Internal - takes part in the formation of the interatrial septum. It has a thinner part that corresponds to the oval fossa.
- The lower one forms the basis of the left ventricle.
- Outdoor.
The LA wall is thinner than the right one. The inner surface of the auricle is lined with pectineus muscles, the rest of the atrium is smooth.
Four pulmonary veins drain into the LA (two from each lung):
- Top right.
- Bottom right.
- Top left.
- Bottom left.
They carry arterial blood from the lungs. The openings of these veins are located on the posterior wall of the left atrium and do not have valves.
Function
Main functions of the left atrium:
- Depositing. The chamber is a container that receives blood from the pulmonary veins.
- According to the pressure gradient, it conducts blood into the left ventricle after the mitral valve opens.
- Helps complete filling of the left ventricle through its contraction.
- When the atrium walls stretch, the pressure rises, which stimulates the formation of natriuretic peptide (NUP). The biologically active substance reduces circulating blood volume and blood pressure. It has been proven that NUP prevents the development of cardiac hypertrophy.
- There are many baro- and mechanoreceptors located in the LA. The former respond to an increase in central venous pressure, which in turn leads to the activation of the latter, which contribute to the development of tachycardia (accelerated heartbeat).
Which Vessels Enter the Right and Left Atrium
The heart is the center of a closed cardiovascular system, pumping blood through the vessels.
Its work allows it to provide cells with oxygen and nutrients, remove carbon dioxide and metabolic products from them, and also respond to damage, inflammatory processes and the penetration of bacteria, viruses and other microorganisms. Some vessels flow into the right atrium, others into the left. Thus, all the venous (waste) and oxygenated arterial blood in the lungs enters the heart.
The human heart is a 4-chamber “pump” of 2 atria and 2 ventricles
Blood is pushed out from the other 2 chambers of the heart - the ventricles. Venous blood goes to the pulmonary lobes along the pulmonary trunk from the right ventricle, and oxygenated arterial blood from the left ventricle enters the aorta.
In this article, we will briefly consider which vessels enter the left atrium and what flows into the right atrium. In fact, we will talk about the end of the systemic and pulmonary circulation of the human cardiovascular system.
The functions of the first circle are listed in the introduction above, but the small closed circle between the heart and lungs, in addition to heat transfer, faces only one global task - gas exchange: freeing the blood from carbon dioxide and saturating it with oxygen.
Vessels draining into the atria of the heart
Vessels flow into the right atrium, through which venous blood flows with a high content of CO2 and waste. They close the large circle of blood circulation.
There are two such veins:
- Inferior vena cava . It is the largest venous vessel, which is often called the venous trunk. “Waste” blood from the legs, tissues and organs located in the pelvis and abdomen is collected here.
- Superior vena cava . It is a short trunk formed by two brachiocephalic venous vessels. It opens with an orifice into the right atrial chamber at the level of the third right rib. Venous blood from the arms, head, tissues and organs of the chest flows here.
The thickness of the upper and lower hollow venous vessels flowing into the heart is different, since they experience different loads. In addition, there are gender differences in the topographic and anatomical characteristics of the thickness of their walls.
For your information. Histological maturity of the tissue of the walls of the inferior and superior vena cava occurs at the age of 10, and starting from the age of 70, there is a gradual reduction in the number and atrophy of circularly located smooth muscle cells.
By the way, answering the question: “What vessels flow into the right atrium?” – we should remember the lymphatic system. Its ducts connect into trunks, which open into veins located near the clavicular bones.
Thus, venous blood flowing in the area between the mouths of the lymphatic trunks and the superior vena cava has the highest degree of bactericidal activity.
Veins draining into the atria of the heart
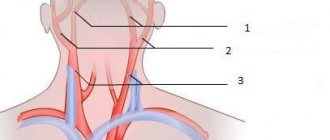
Paired vessels flow into the left atrium, closing the pulmonary circulation:
- The two left (superior and inferior) pulmonary veins drain oxygenated blood into the left atrium. Their mouths are located vertically, one above the other, and are located in the left posterolateral region of the wall of the atrial chamber. The upper vessel collects blood from the upper lobe of the left lung, and the lower left pulmonary vein, respectively, from the lower lobe of the left lung.
- The two right (superior and inferior) pulmonary veins drain blood into the left atrial chamber of the heart from the right lung. The length of these vessels is greater than that of the left pulmonary veins, since before they enter the posterior wall of the left atrium near the interatrial septum, they still pass through the thickness of the posterior wall of the right atrium (pictured below).
The thickness of the walls of the vessels that flow into the left atrium is almost the same in men and women. However, there are also differences. The thickness of the wall between the orifices and the diameter of the superior venous vessel are greater in women, and the diameters of both inferior pulmonary veins are greater in men.
Location of the pulmonary veins
We also note that during intrauterine development the pulmonary circulation does not work. Oxygen-enriched blood comes from the mother through the umbilical vein and is drained through the umbilical arteries of the placenta.
The pulmonary circulation, starting with the pulmonary column and ending with the pulmonary veins, begins to function immediately after birth, as soon as the baby takes his first breath.
Congenital defects
The most common anomalies in the development of blood vessels flowing into the atria of the heart are:
- The presence of 2 hollow superior or 2 hollow inferior veins, instead of one. It is rare, but the location of the inferior vena cava to the right of the spine occurs. Typically, these defects do not affect health and do not require surgical correction.
- Anomalous pulmonary venous drainage (APVD). This pathology is an unnatural entry of these vessels not into the left, but into the right atrium, which occurs in various combinations. The total proportion of such anomalies is 3% of all congenital heart defects. These defects require surgical treatment. The type of operation and timing depend on the type of ADLV (see below).
To diagnose ADLV, the doctor will prescribe a set of examinations, including: ECG, echocardiography, MRI, CT, atrio- and ventriculography, as well as many other instrumental studies.
Options for partial and one of the total (in the center) anomalous pulmonary vein drainages
ADLV can be partial or complete (total). In the first case, 1 or 2 pulmonary veins flow into the right atrium instead of the left one and, in most cases, such an anomaly is accompanied by an atrial septal defect.
Partial ADLV causes cyanosis, shortness of breath, frequent pneumonia, weakness, pain in the heart, and retarded physical development. The pathology requires surgery according to indications.
Patients with ADPV can live up to 30 years before dying due to cardiac arrest due to heart failure or pulmonary infection.
For your information. In addition to atrial or ventricular septal defect, ADLV is often accompanied by other developmental defects. Among them: tetrado of Fallot, coarctation of the aorta, Turkish saber syndrome, truncus arteriosus, abnormalities in the development of the gastrointestinal tract and genitourinary system.
Total ADPV are congenital pathologies in which all 4 pulmonary venous vessels open separately not into the left atrium, but into the right atrium. Often there are options when they all connect into one common collector vessel, flowing either into the coronary sinus, or into the superior or inferior vena cava.
Children with total ADLV defects are born full-term, and the body, although with difficulty, copes with this situation for several days (months). However, the health condition is critical from the very first day, and it is necessary to perform reconstructive surgery as quickly as possible.
Diseases
Among the pathologies of vessels flowing into the atria acquired during life, the most common are:
- obstruction of the upper or lower hollow venous vessels flowing into the right atrial chamber, caused by thrombosis or a tumor process;
- pulmonary vein stenosis;
- obliterating endarteritis of the pulmonary venous vessels.
All these diseases cannot be treated conservatively and require surgical intervention.
And as a conclusion, we suggest watching a video that tells in more detail about the largest vein in the human body, the Inferior Vena Cava, which flows into the right atrium.
Source: https://Cardio-help.ru/anatomiya/vpadayut-v-pravoe-predserdie-688
Normal dimensions of the left atrium
Camera parameters are measured using echocardiography (EchoCG), a non-invasive ultrasound research method.
Normal dimensions of the left atrium in adults:
- cavity size – 8-40 mm;
- anterior-posterior – 1.3-3.7 cm;
- width: front – 1.2-3.1 cm, back – 1.4-3.3 cm;
- height – 1.5-3.9 cm;
- wall thickness – 1.5-2 mm;
- thickness of the interatrial septum – 0.7-1.2 cm;
- weight – 15-25 g (5.6-9.2% of the total).
Adequate performance indicators
The volume of the cavity (the amount of blood that fits in the atrium) is 110-130 cm3.
Blood pressure: 2-4 mm Hg. Art. in diastole and 9-12 mm Hg. Art. at systole.
In addition, the adequacy of filling with blood from the pulmonary veins, the uniformity of contraction of muscle fibers of all walls and the direction of blood flow in different phases of the cycle are assessed.
There are four cavities in the human heart
The two cavities are like hallways in a residential building. These cavities “meet” and “receive” blood, which is transported through the vascular bed to the heart. These cavities are called atria.
Why are there two hallways? Because the heart is a house for two owners. Each owner has his own hallway and his own room. These two halves of the house do not communicate with each other in any way. Because they belong to different owners.
So, there are two hallways or two atria: right and left. This is where the blood that rushes to the heart from a long journey through the human body comes.
The right half receives blood, which has passed through the human body, washing all its organs. To the left is the blood that has traveled through the lungs.
Read the articles: “Structure of the human heart”, “How does the heart work?” and “Two circles of blood circulation.”
But blood completely filled two small hallways. Now she should be invited further into the room. Each owner has such a room - this is the left and right ventricle. And so that blood can get from the hallway into the room, there are holes in the walls separating these rooms.
How to determine pathology?
The main methods that can be used to determine the condition of the left atrium include: electrocardiography (ECG) and echocardiography (EchoCG).
ECG
The function of the left atrium on the ECG is assessed by the P wave in leads I, II, aVL, V5, V6.
This method allows you to see:
- Atrial hypertrophy (thickening of the walls). Signs on the cardiogram: increased height and bifurcation of P in I, II, aVL, V5, V6 (the so-called “P - mitrale” - raising the second part of the tooth); negative or biphasic P, P duration is more than 0.1 s.
Hypertrophy is the basis for the occurrence of atrial fibrillation (fibrillation). On the ECG it is expressed by: absence of the P wave, the presence of chaotic f-waves (especially in II, III, aVF, V1, V2), irregular ventricular rhythm. In addition, the proliferation of muscle fibers contributes to the appearance of sinus tachycardia - an increase in the number of impulses arising in the sinoatrial node. On the ECG, the P wave is normal, the RR distance is shortened. - Atrial dilatation (an increase in the size of the cavity against the background of a thinning of the wall) can be suspected using an electrocardiogram only in the presence of arrhythmias.
EchoCG signs
EchoCG or ultrasound (ultrasound) determines the size and performance of the left atrium, which makes it possible to diagnose hypertrophy and dilatation of this section.
The method is used to diagnose coarctation of the aorta, mitral and aortic valve defects, cardiac tumors (myxomas), the presence of which affects the size and function of the left atrium.
Structure of the human heart
You need to understand that the human heart is a rather complex mechanism. In itself, for any of us, however, like all representatives of birds and mammal families, it consists of four parts. This is represented by two atria and two ventricles. Between the atria and ventricles there are inlet valves - they are also called fibromuscular valves. On the left side of the heart, one of the most important valves for the functioning of blood flow functions - the bicuspid (consisting of connective tissue) mitral valve, and on the right in the diagram you can see the tricuspid valve, which is no less important for the functioning of the muscular organ, which in science is also called tricuspid.
Signs of dysfunction
Left atrial overload
Signs of dysfunction of the left atrium are called overload (hyperfunction). The condition is based on hemodynamic tension of the walls by resistance or volume.
Prolonged load on the muscle mass of the myocardium of the chamber first causes hypertrophy of the fibers. However, depletion of energy reserves and progression of pathology contribute to muscle atrophy, and the atrium begins to dilate.
Characteristic clinical symptoms:
- fatigue;
- dyspnea;
- interruptions in heart function;
- pain in the heart area;
- decreased endurance to physical activity.
The most common causes of overload:
| Acute conditions | Long-term illnesses |
|
|
ECG signs of overload: increased height and duration of P (mostly its second phase) in V1, V2, sometimes negative P in V1.
LA overload most often leads to its hypertrophy or dilatation. During an objective examination (using percussion), pathology can be suspected by the upward displacement of the upper border of the heart.
Treatment always depends on what pathology led to overload and, as a consequence, to hypertrophy or dilatation. If we are talking about acute conditions, then they are treated by doctors according to emergency care protocols in each case. Long-term, chronic diseases are treated with lifelong medication, and many require surgical intervention.
If the above conditions are not treated, there is a high risk of a number of dangerous complications:
- severe heart failure;
- cardiac asthma;
- atrial fibrillation.
Anatomy and diseases of the cardiovascular system
January 23, 2007 01:50
The great circle includes the aorta (ascending and descending, aortic arch, thoracic and abdominal sections), through which blood flows from the left side of the heart.
From the aorta, blood enters the carotid arteries that supply blood to the brain, subclavian arteries, blood supply to the arms, renal arteries, arteries of the stomach, intestines, liver, spleen, pancreas, pelvic organs, iliac and femoral arteries, and blood supply to the legs.
Blood flows from the internal organs through veins that drain into the superior vena cava (collects blood from the upper half of the body) and the inferior vena cava (collects blood from the lower half of the body). The vena cava drains into the right heart.
The pulmonary circulation includes the pulmonary artery (through which, however, venous blood flows). Through the pulmonary artery, blood enters the lungs, where it is enriched with oxygen and becomes arterial. Through the pulmonary veins (four), arterial blood enters the left heart.
The heart pumps blood - a hollow muscular organ consisting of four sections. These are the right atrium and right ventricle, which make up the right heart, and the left atrium and left ventricle, which make up the left heart.
Oxygen-rich blood coming from the lungs through the pulmonary veins enters the left atrium, from there into the left ventricle and then into the aorta.
Venous blood enters the right atrium through the superior and inferior vena cava, from there into the right ventricle and further through the pulmonary artery into the lungs, where it is enriched with oxygen and again enters the left atrium.
There are pericardium, myocardium and endocardium. The heart is located in the cardiac sac - the pericardium. Cardiac muscle - the myocardium consists of several layers of muscle fibers; there are more of them in the ventricles than in the atria. These fibers, contracting, push blood from the atria into the ventricles and from the ventricles into the vessels. The internal cavities of the heart and calves are lined by the endocardium.
|
Between the left atrium and the left ventricle there is a mitral (bicuspid) valve, and between the right atrium and the right ventricle there is a tricuspid (three-leaf) valve. The aortic valve is located between the left ventricle and the aorta, the pulmonary valve is between the pulmonary artery and the right ventricle.
From the left and right atria, blood flows into the left and right ventricles, while the mitral and tricuspid valves are open, the aortic and pulmonary valves are closed. This phase in the work of the heart is called diastole.
Then the mitral and tricuspid valves close, the ventricles contract and through the opened aortic and pulmonary valves, blood rushes into the aorta and pulmonary artery, respectively.
This phase is called systole, systole is shorter than diastole.
We can say that the heart works autonomously - it itself generates an electrical impulse that spreads through the heart muscle, causing it to contract. The pulse must be generated at a certain frequency - normally about 50-80 pulses per minute. In the conduction system of the heart, the sinus node is distinguished (located in the right atrium), from which nerve fibers go to the atrioventricular (atrioventricular) node (located in the interventricular septum - the wall between the right and left ventricles). From the atrioventricular node, nerve fibers run in large bundles (right and left bundle branches), dividing into smaller bundles in the walls of the ventricles (Purkinje fibers). An electrical impulse is generated in the sinus node and spreads through the conduction system throughout the myocardium (heart muscle). Like all organs, the heart must receive oxygen. Oxygen is delivered through arteries called coronary arteries. The coronary arteries (right and left) arise from the very beginning of the ascending aorta (at the origin of the aorta from the left ventricle). The trunk of the left coronary artery is divided into the descending artery (also known as the anterior interventricular) and the circumflex artery. These arteries give off branches - the artery of the obtuse edge, diagonal, etc. Sometimes the so-called median artery branches off from the trunk. The branches of the left coronary artery supply blood to the anterior wall of the left ventricle, most of the interventricular septum, the lateral wall of the left ventricle, and the left atrium. The right coronary artery supplies part of the right ventricle and the posterior wall of the left ventricle.
Now that you have become an expert in the anatomy of the cardiovascular system, let’s move on to its diseases.
The basis of coronary heart disease is an insufficient supply of oxygen to the heart muscle. That is, there is a discrepancy between demand and delivery. The most common cause of IHD is atherosclerosis of the coronary arteries. An atherosclerotic plaque forms inside the coronary artery, which closes its lumen.
With increased stress (physical, psychological stress), the heart requires more oxygen, but its delivery is limited due to partial stenosis (blockage) of the coronary artery. Therefore, the main symptom of angina pectoris is retrosternal (squeezing, pressing) pain during physical activity.
The duration of pain is from seconds to minutes (no more than 30 minutes). The pain is usually relieved with nitrates (nitroglycerin). To make a diagnosis of angina, an ECG, stress tests, ECHO CG, 24-hour ECG monitoring, myocardial perfusion scintigraphy, and coronary ventriculography are performed.
Angina is divided into stable (angina pectoris, angina at rest) and unstable (progressive, first occurring). A special form of angina is vasospastic (Prince-Menthol), which occurs due to spasm of the coronary arteries.
There are three main ways to treat angina - medications (nitrates, b-blockers, angiotensin converting enzyme inhibitors, etc.), balloon angioplasty and coronary artery bypass surgery.
Myocardial infarction is necrosis (death) of a section of the heart muscle. The causes of myocardial infarction are the same as angina pectoris. The main symptom is prolonged chest pain (more than 30 minutes), which is not relieved by nitrates. The diagnosis of myocardial infarction is made based on the clinical picture, characteristic ECG changes and elevated blood enzyme levels.
Treatment is medication (aimed at relieving pain, reducing blood oxygen demand, dilating the coronary arteries); in some cases, within a few hours of the development of a heart attack, it is possible to dissolve a blood clot by administering special drugs (streptokinase, urokinase, etc.).
Emergency balloon angioplasty is sometimes performed.
As a result of a myocardial infarction, or due to other diseases (myocarditis), the muscle tissue of the heart is replaced by connective tissue, that is, a scar is formed. Scar changes in the myocardium are called cardiosclerosis.
Classification
Change in sinus node automaticity:
- sinus bradycardia (slow heart rate),
- sinus tachycardia (accelerated rhythm),
- sinus arrhythmia (irregular rhythm)
Escape rhythmsAtrioventricular dissociation
Atrial tachycardia
Atrioventricular reciprocal tachycardia Ventricular tachycardia Ventricular fibrillation Ventricular preexcitation Weakness of the sinus node
Blockades:
- Sinoatrial
- Atrioventricular
- Bundle branch blocks
Atrial fibrillation and flutter Parasystole
Since it is quite difficult to explain to a non-specialist the essence of these violations, we will decipher only the basic concepts. Extrasystole is an extraordinary contraction of the heart. A distinction is made between atrial extrasystoles (“incorrect” impulse occurs in the atria) and ventricular extrasystoles (“incorrect” impulse occurs in the ventricles).
The patient perceives extrasystoles as pauses in the work of the heart. In healthy people, a small amount of extrasitol is recorded per day. Atrial fibrillation (atrial fibrillation) is frequent, chaotic, irregular contraction of the atria and irregular ventricular rhythm.
The main causes of atrial fibrillation are damage to the mitral valve, thyrotoxicosis (pathology of the thyroid gland), and cardiosclerosis.
To treat rhythm disturbances, there are several groups of antiarrhythmic drugs; in some cases, pathological foci or nerve pathways are destroyed.
Conduction disorders - delay in the conduction of impulses through the conduction system of the heart - blockade, or vice versa, accelerated conduction of the impulse along additional conduction pathways. Conduction delay is a block; there are sinoauricular, atrioventricular, and bundle branch blocks. Accelerated conduction - WPW (Wolf-Parkinson-White) syndrome is more common.
The main manifestation of hypertension (HD) is increased blood pressure (BP). This is often manifested by headaches, tinnitus, and flickering of “spots” before the eyes. Hypertension is divided into two large groups - essential (primary) and symptomatic (secondary) hypertension. Essential hypertension is a disease at the level of the whole organism.
With secondary hypertension, there is damage to one or another organ, which leads to an increase in blood pressure. Secondary hypertension is divided into renal (glomerulonephritis, pyelonephritis, renovascular hypertension, etc.
), endocrine (pheochromocytoma, paraganglioma, Cohn syndrome, Itsenko-Cushing syndrome), vascular (coarthation of the aorta), hypertension with damage to the central nervous system.
When blood pressure increases, changes occur in various organs. The organs most susceptible to the effects of high blood pressure are called target organs. These are the brain, heart, blood vessels, retina, kidneys.
When treating symptomatic hypertension, it is important to eliminate the cause of the increase in blood pressure. The main antihypertensive drugs are b-blockers, angiotensin converting enzyme inhibitors (ACEIs), calcium antagonists, and diuretics.
Heart defects are divided into congenital and acquired. There are quite a large number of names that are congenital; we will not list them all; we will pay attention to the most common ones. These are patent oval window (ventricular septal defect), atrial septal defect, tetralogy and Fallot's triad. Treatment is surgical. Mitral valve prolapse is insufficiency of the mitral valve caused by the “bending” of its valves into the cavity of the left atrium during contraction (systole) of the left ventricle. The reason is connective tissue disorders.
Acquired defects include stenosis (incomplete opening) or insufficiency (incomplete closure) of the heart valves. Stenosis or insufficiency of the mitral and tricuspid valves are more common. The cause of the lesion is rheumatism, endocarditis, atherosclerosis, etc. Treatment is surgical, in the acute phase - antibiotic therapy, hormones, cytostatics, etc.
MyocarditisEndocarditisPericarditis
Cardiomyopathies
- Dilation
- Hypertrophic
- Restrictive
Myocarditis is an inflammation of the heart muscle, it can be bacterial, viral, or allergic.
This is a rather “complex” disease, since an autoimmune reaction is triggered - antibodies are produced to one’s own muscle. Treatment: antibiotics, hormonal drugs, hydroxyquinolines.
Endocarditis is inflammation of the endocardium, often bacterial. Ultimately leads to damage to the heart valves. Treatment: antibiotics, hormones.
Dilated cardiomyopathy is a lesion of the heart muscle, which causes expansion of the heart (enlargement of cavities) and thinning of its walls. The heart's ability to pump blood decreases.
The reason is not fully understood. The main manifestation is the occurrence of circulatory failure - shortness of breath, swelling, enlarged liver, attacks of suffocation.
Weakness, cardiac arrhythmias, and thromboembolism are common.
Hypertrophic cardiomyopathy is a thickening of the heart muscle, resulting in difficulty ejecting blood from the left ventricle. The reason is not fully understood. The main manifestation is rhythm and conduction disturbances, pain in the heart, weakness.
Restrictive cardiomyopathy is a reduction in the chambers of the heart.
Cor pulmonale is an overload of the heart that occurs due to increased resistance in the vessels of the lungs. The reason for this is primary pulmonary hypertension (primary damage to the blood vessels of the lungs), chronic pulmonary diseases (pneumosclerosis, emphysema, bronchiectasis, bronchitis, etc.) and anatomical changes in the chest.
Peripheral arterial diseases:
- Arterial stenosis and occlusion
- Arterial aneurysms
- Raynaud's disease (syndrome)
- Peripheral venous diseases
- Peripheral vein thrombosis
- Phlebitis
- Varicose veins
Based on materials from: cardioline.ru
January 19, 2007 | 02:01
Cardiologist
Various diseases of the cardiovascular system today are the most common in the registry of morbidity and causes of mortality in the population.
October 30, 2006 | 01:10
Arterial hypertension
High blood pressure, or hypertension, is the most common chronic disease today. It is well known that hypertension is a leading risk factor in the development of strokes, myocardial infarction, vascular and kidney damage, vision loss and other dangerous diseases. Fortunately, in the last 30-35 years there have been obvious breakthroughs in the treatment of this disease.
August 25, 2006 | 05:08
Cardiopsychoneurosis
The term neuro-circulatory dystonia or vegetative-vascular dystonia, alas, is familiar to many. But they don’t always correctly imagine what it actually is. So, let's try to figure it out.
Source: https://www.medicus.ru/cardiology/patient/anatomiya-i-zabolevaniya-serdechno-sosudistoj-sistemy-27994.phtml
Forms of blood supply
Heart with a right coronary type of blood supply: the right coronary artery (1) and its branches are more developed than the left coronary artery (2)
There are several types of blood supply to the heart. All of them are a variant of the norm and a consequence of the individual characteristics of the formation of heart vessels and their functioning in each person. Depending on the prevailing distribution of one of the coronary arteries on the posterior heart wall, they are distinguished:
- Legal type. With this type of blood supply to the heart, the left ventricle (posterior surface of the heart) is filled with blood primarily from the right coronary artery. This type of blood supply to the heart is the most common (70%)
- Left-handed type. Occurs if the left coronary artery predominates in the blood supply (in 10% of cases).
- Uniform type. With approximately equal “contribution” to the blood supply of both vessels. (20%).