White blood cells or leukocytes themselves are heterogeneous. This is the general name for five structures. The goal of all of them is the same: the fight against infectious and other abnormal agents that invade the human body. Accordingly, they form the basis of the immune system.
Neutrophils are one of the subtypes of leukocytes. They are most numerous in relation to other similar cells and make up up to 70% of the total mass of such cells. They perform important functions but are heterogeneous in nature.
In a sense, these structures are universal, capable of fighting most types of pathogens and foreign objects. Deviations from the norm always indicate the development of pathological processes, not counting a small number of subjective reasons, for example, taking certain medications.
The appropriateness of treatment is determined by the specific clinical situation. Neutrophils in a blood test reflect immune function, therefore any deviation is potentially dangerous, which is what doctors proceed from when considering the need for therapy.
Functions of neutrophils
These cells solve a large group of specific tasks facing the human body’s defenses:
Release of bactericidal substances
The structures of cytological units contain specialized compounds that have the ability to kill pathogenic flora. When a target is detected, the neutrophil releases a substance that dissolves the cell membranes of the pathogen.
Thus, the genetic material is not encapsulated and the bacterium dies. This is one of the main mechanisms of neutrophil activity.
Antigen binding
The cells in question on the membranes have special receptors for specific immunoglobulins of class G; they are the most common in the body and are highly active in the fight against infectious agents of all types.
Due to the ability to bind such substances, neutrophils can quickly transport them to the site of injury to enhance the immune response. Thus, the destruction of pathogens is achieved much faster.
Direct absorption of microorganisms
Formed cells are capable of phagocytosis. They are large and aggressive enough to destroy bacteria by “eating” them. On average, a neutrophil can eliminate up to 20-30 foreign structures using different methods. Which indicates its high efficiency.
Inhibition and inactivation of viral agents
White blood cells have the ability to reduce the rate of replication of foreign pathogens and reduce the productivity of their existence. In favorable cases, complete suppression of the structures is achieved, due to which the inflammatory processes disappear.
The functions of neutrophils ultimately come down to one thing - the destruction of bacteria, viruses, fungi, and other objects in various ways. Therefore, an increase in the Neut indicator in a blood test indicates an immune response, be it a reaction to an infectious lesion or allergic processes. Next, you need to understand it in detail, in essence.
Functions
The main function of neutrophils is phagocytosis, that is, the absorption and dissolution of foreign particles, but they are able to dissolve only small particles or cells, and after their dissolution they die. Each cell is capable of only one phagocytic event. At the same time, the cell creates a certain respiratory explosion. During the respiratory burst, NADPH (nicotinamide adenine dinucleotide phosphate), an enzyme that produces large amounts of superoxide (reactive oxygen), is activated. Superoxide spontaneously mutates into hydrogen peroxide, which is then converted to HOCI.
Kinds
Neutrophils, despite the same name, are also heterogeneous. There are several types of these. Depending on the functional purpose (narrow specialization) or the degree of readiness for work.
In total, four types can be defined:
- Myelocyte. Relatively speaking, it cannot be called a type of white blood cell. This is an extremely immature cell. In essence, it has not even differentiated yet. This is a rough “preparation” of the organism for future transformation into other structures. Not necessarily neutrophils.
Transformation into anything is possible: from a platelet to an eosinophil. Normally, such structures should not exist in the bloodstream at all. They concentrate in the bone marrow and are finally formed there, only then they enter the body and begin to do their job.
- Young or immature neutrophils. Intermediate form. It is also stored in the place of its own synthesis, providing a conditional reserve. In case more immune cells need to be released. Similar varieties are also absent from the bloodstream. Because they are not yet capable of working.
On the other hand, as a result of random phenomena, a small number of them may be released. This is not critical, but the quantity should be within the error level. About 0.1-1%, with a possible downward deviation. All obvious changes indicate the development of one or another pathological process in the body.
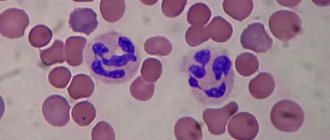
- Band neutrophils. Make up a minimum of the total mass. Not more than 5% of the quantity. They got their name due to the peculiarities of their shape, which is clearly visible during microscopic analysis. These cells have approximately the same functions, but are more highly specialized. They get involved out of necessity when the majority cannot cope.
- Neutrophils are segmented. The most numerous subtype of white blood cells. According to various estimates, it accounts for up to 70% of the number of structures. Solve the problems described above constantly and fully. The work of neutrophils of this type is especially noticeable during the development of an infectious-inflammatory process in the body.
There are thus only two functionally active species. Both of them are approximately equivalent in features, role and potential for combating pathogenic agents, microorganisms, viruses, fungi.
Standard tables
Neutrophils are designated in a blood test as Neut, and the number of cells is calculated as a percentage. But in laboratory and clinical practice, the absolute content of neutrophils is also used, this is an indicator that is calculated in the number of units per liter of blood.
Which method will be used depends on the specific institution and research methods.
Among women
The indicators vary quite widely. On average, the norm of neutrophils in the blood of women is 50-59%, which is slightly higher than that of men. This is due to the peculiarities of the immune system and other factors.
| Age (years) | Neutrophils as a percentage (calculated according to the most numerous variety - segmented) |
| 16-18 | 51-56% |
| 18-21 | 52-57% |
| 22-35 | 52-59% |
| 35-45 | 51-58% |
| 45-60 | 50-55% |
| After 60 years | 52-58% |
The data in the table is approximate; slight individual fluctuations downward (but not upward) are possible. It is also necessary to take into account the patient’s condition at the time of the study.
Interpretation of results
A clinical blood test can now be done both in public medical institutions and in private clinics. As a rule, the normal values are indicated on the study form . This used to be a uniform standard, but is now necessary because the values may vary slightly between laboratories. The test should be deciphered by a doctor; only he can correctly interpret the indicators.
In the body of a healthy adult, neutrophils should be contained in quantities from 1.8 to 7.7 billion per liter (47−72%), in children the figures vary depending on age. An increase in the number of immature white blood cells means a neutrophil response (the leukoformula shows a shift to the left), which is a marker of acute inflammation, infectious diseases, intoxication of various origins, myocardial infarction and other conditions. Chronic infections most often manifest themselves in a lymphocytic response.
Natural causes of increase
An increase in the concentration of neutrophils (a shift in the leukocyte formula to the right) is not always of an abnormal origin. Although this is true for most possible clinical situations.
If we talk about natural factors, they will be like this:
- Pregnancy. Gestation creates a large load on the mother’s body, and all immune processes intensify. Which ultimately causes an increase in levels in a laboratory study. This is not dangerous, because the answer is false. However, just in case, you need to check other indicators. Sluggish manifestation of pathology is possible.
- Delivery.
- The menstrual cycle and the period right before it. The body considers the natural monthly processes of egg maturation and release as intense stress. The result is a false immune reaction. This does not pose any danger; you need to wait until the end of the period and everything will return to normal on its own.
- Exercise stress. The more intense it is, the more significant the deviations in neutrophil levels will be. Levels return to adequate levels without medical assistance or external influence in general.
- Consuming large amounts of food. In general, food causes a temporary increase in the concentration of formed cells. The relationship is directly proportional. Everything returns to normal after a few hours.
Stress affects performance in the same way. This also applies to any emotional manifestations.
Pathological factors for increasing neutrophil concentration
The norm of neutrophils in the blood changes mainly for abnormal reasons. If we talk about specific conditions:
- Inflammatory processes. There are two types. Infectious. The most numerous group. It is typical for them to enter the body of foreign structures. Ultimately, increasing the levels of neutrophils and more is an adequate and correct response of the body to an external attack.
The situation is somewhat more complicated with the second subtype of the pathological process. When an autoimmune response develops. Inflammatory phenomena of this kind are characterized by the absence of a pathogen as such. The body attacks itself, its own cells.
This is the result of a malfunction of the immune system. Neutrophils do not perform a useful function, but the increase is obvious.
- Endocrine disorders. Mainly those that provoke severe metabolic disorders. The leader of this group is considered to be diabetes mellitus. This can also include pathologies of the thyroid gland and adrenal glands. Various types.
- Malignant tumors. Regardless of location and type. Neutrophil counts especially increase if bone marrow function is disrupted. Metastases or primary neoplasia, this no longer plays a role in the context of determining the causes.
- In addition to the actual diseases, they call the iatrogenic factor. That is, all kinds of traumatic surgical interventions. The change in levels persists throughout the entire rehabilitation period. Only then does it fade away.
Attention:
There are also a few exceptions to the rules. If neutrophils in an obvious pathological process are within the normal range, this is not natural. We are talking about the weakness of the immune system; it is necessary to treat the underlying disease as quickly as possible.
Reasons for the downgrade
There are also many factors that shift the leukocyte formula to the left.
- HIV. Huge problem. The pathological process provokes depression of the entire immune system. In this case, even against the background of a real threat, damage to the body, there will be no growth indicators at all. On the contrary, they will be lowered. Maintenance therapy is required.
- Aplastic anemia. Accompanied by a violation of the synthesis of all possible formed blood cells. Leukocytes of different types are no exception here. Without specific treatment, potentially fatal complications are likely. Action needs to be taken faster.
- Severe infectious processes. In this case, the need for shaped cells for active combat is growing. The body may not have time to produce new ones, hence the temporary decline.
- General weakness of all systems. Neutrophils are lower than normal if a person has suffered a serious illness in the recent past or does not receive enough nutrients.
- History of alcoholism. The same goes for those who drink heavily. The concentration of neutrophils is less than adequate values, since their synthesis is suppressed by ethanol breakdown products. The general exhaustion of the body of such people also affects.
- Hepatitis. Inflammatory process of the liver. It has an infectious, particularly viral origin.
- Sepsis. Generalized damage to the body.
- Radiation sickness.
- Intoxication. In case of poisoning with certain poisons. A group of drugs also has a similar effect. The possibility of such a side effect is reflected in the annotations for specific pharmaceutical products.
Reasons for the increase in some cells and the decrease in others
It is necessary to take into account other factors of growth or decrease in indicators. This applies to natural, natural phenomena caused by physiology. There are many shaped cells designed to fight external attacks. In this case, several situations are possible.
- Neutrophils are increased and lymphocytes are decreased. The first phase of eliminating foreign structures is underway. The central immunity is not yet active enough, and there is no need for it. If effective, changes in laboratory parameters will not be so significant.
- If neutrophils are low and lymphocytes are high, this indicates the second phase of the defense response. When central cells begin to work more actively, and local-level structures temporarily reduce the intensity of activity.
Without going into complex biological mechanisms, it is worth mentioning the general rule: when neutrophils increase, lymphocytes decrease and vice versa. This is normal and natural. There is no simultaneous increase or decrease observed.
What additional examinations are needed?
Usually, a general blood test is sufficient to establish the fact of an increase in the level of neutrophils. It shows a fairly comprehensive picture of the shaped cells.
But this is not enough. To understand the situation and help the patient, the main task is to identify the root cause of the disorder. This is somewhat more complicated and requires additional research.
- Oral survey. Allows you to evaluate a person’s complaints about the condition. The symptomatic complex gives an idea of the primary source of infection or other factors of deviation.
- Anamnesis collection.
- X-ray of the chest organs.
- Visual assessment of the condition of the oropharynx and ENT organs in general.
- Study of biochemistry indicators.
- Ultrasound of the abdominal cavity.
Other activities are scheduled as needed. It all depends on the hypotheses expressed by the specialist. There may be several specialized doctors here, because we are not talking about a specific diagnosis, but about a laboratory finding. First of all, it makes sense to contact a therapist (pediatrician).
When and how the analysis is carried out
A blood test for neutrophils is necessary when an adult develops unexplained symptoms:
- anemia in any form;
- signs of poisoning with heavy metals and poisons;
- aching pain localized in joints, bones, muscles;
- fainting, dizziness;
- loss of balance;
- skin rash;
- drowsy state;
- sudden weight loss;
- regular increase in body temperature;
- long-term depression, which is accompanied by aggressiveness;
- increased heart rate;
- hematomas that appear without mechanical impact;
- difficulty swallowing;
- enlarged lymph nodes;
- change in urine color;
- constant thirst.
Important information: How to quickly raise white blood cells after chemotherapy at home (what to do and what products increase)
A general blood test for neutrophils is necessary if a person’s cuts and scratches do not heal for a long time. Neutrophils in a general blood test can detect inflammatory diseases or tissue necrosis.
NEUT in a blood test is checked in patients during the postoperative period to monitor their condition.
The analysis is carried out in the morning on an empty stomach; before visiting the clinic you should refrain from:
- physical activity;
- eating fried and fatty foods;
- smoking;
- alcohol.
Blood is taken from a finger or vein.
Treatment
Correction is determined by the specific cause of the pathological process. The goal is not to raise neutrophils in the blood using artificial methods; it is necessary to eliminate the source of the problem. Drug therapy is practiced.
In case of infectious genesis of the disorder, the following means are used:
- Antibiotics. Different types.
- Stimulators of leukocyte synthesis. Leukogen and others. Carefully.
- Local antiseptic drugs.
If we are talking about autoimmune reactions:
- Suppressors. To suppress the activity of protective forces.
- Glucocorticoids. Prednisolone and similar.
- Others may be used. According to the needs and prescription of the treating specialist.
The number of neutrophils in the blood also shows the effectiveness of therapy, therefore it is possible to study the quality of the correction carried out according to this criterion.
Otherwise, the techniques depend on the clinical situation. Diabetes mellitus requires glucose control, malignant tumors require surgical treatment, etc.
Norms
The norm of young neutrophils differs only in the first two weeks after the birth of children. The newborn gets rid of the mother's blood cells and begins to produce their own. During this period, there is a violation of the ratio between band and segmented neutrophils: the level of “segments” is 50–70%, and “rods” is from 3 to 12%.
Such a “distortion” quickly normalizes and throughout the rest of the child’s life and in adulthood it will be in normal conditions from 1 to 6%.
The level does not depend on the age of the adult; it is the same in men and women.
What are neutrophils?
Neutrophils, or neutrophilic leukocytes, are the most numerous subtype of white blood cells.
Being present in the blood, neutrophils perform one of the most important functions of protecting the body from the effects of pathogenic bacteria, viruses and other harmful agents. Neutrophils detect a pathogenic microorganism, destroy it, and then die themselves.
The level of neutrophils in the blood is determined by a detailed clinical analysis, which contains information about all types of neutrophils.
Segmented neutrophils
Segmented neutrophils are mature granulocytes present in the circulating blood. The cell diameter is approximately 0.009 – 0.015 mm and the N:C ratio is approximately 1:3. The cell content resembles the cytoplasm of the stripe. The spots are faintly pink and contain numerous specific granules that are colored mauve.
A segmented neutrophil has the following characteristics:
- The nucleus is dark purple in color and the chromatin has a rough, lumpy texture.
- The nucleus has 2-5 lobes, with an average of 3.
- The lobes are connected to each other by a thin thread or thread of the nuclear membrane.
- The filament is a thread-like strip that is so narrow that there is no visible nuclear material between the two sides.
What types of neutrophils are there?
Before full maturation, neutrophils go through 6 stages, based on which, cells are classified into:
- myeloblasts,
- Promyelocytes,
- Myelocytes,
- Metamyelocytes,
- Band,
- Segmented.
Stages of neutrophil development
All cell forms, except segmented ones, are considered functionally immature neutrophils.
What is the maintenance standard?
The amount of neutrophils is measured in absolute units contained in 1 liter of blood and as a percentage of the total number of white cells (leukocytes).
Age Normal (x 10 9 /l) Normal (%)
| Age | Norm (x 10 9 / l) | Norm (%) |
| up to 1 year | 1,5 — 8,5 | 16 — 45 |
| 1-2 years | 28 — 48 | |
| 3-4 years | 32 — 55 | |
| 5-6 years | 1,5 — 8,0 | 32 — 58 |
| 7-8 years | 38 — 60 | |
| 9-10 years | 1,8 — 8,0 | 41 — 60 |
| 11-16 years old | 43 — 60 | |
| over 16 years old | 1,8 — 7,7 | 47 — 70 |
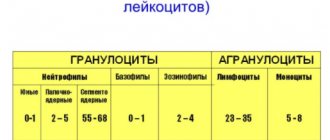
When examining blood with a detailed leukocyte formula, the ratio of neutrophil types is determined
| myeloblasts, promyelocytes, myelocytes (normal%) | metamyelocytes (normal%) | stab (norm%) | segmented (normal%) |
| 0 — 0,5 | 1-6 | 47 — 72 |
A decrease in the level of neutrophils is called neutropenia (agranulocytosis), an increase is called neutrophilosis (neutrophilia).
To determine the type of neutropenia and neutrophilia, data from reference values of the ratio of cell types is used.
How are they designated in the analysis?
A clinical blood test allows the doctor to determine how many white blood cells are in the body. There are five types of white blood cells, and the test also shows how many of each type are present. The absolute number of neutrophils is called ANC. The indicator is not measured directly. It is obtained by multiplying the white blood cell count by the percentage of neutrophils in the various white blood cell counts.
The percentage of neutrophils consists of segmented (mature) cells and stripes (almost mature). The normal range for ANC is 1.5 to 8.0 (1500 to 8000/mm3). In practical clinical settings, safe ANC is 500–1500, low ANC is less than 500. When neutrophils are normal, this means that the patient's activities should not be limited.
On a note! Sometimes a deviation from the norm is a side effect after taking one or another strong medicine. Radiation therapy can also be a trigger.
What do the changes in the analysis indicate?
Increased neutrophil levels
An increase in the level of neutrophils in the blood is called neutrophilosis (neutrophilia).
Deviation from the norm of segmented neutrophils may indicate the following pathologies and conditions:
- Infectious diseases
- Pathologies of the lower extremities,
- Oncological diseases,
- Functional disorders of the urinary system,
- Rheumatoid inflammatory diseases,
- Increased blood sugar levels.
Exceeding the norm of band neutrophils occurs in acute infectious and inflammatory diseases, which provoke an acceleration of the penetration of immature neutrophils into the bloodstream.
The number of young neutrophils above normal is a consequence of:
- Pneumonia,
- Otitis,
- Pyelonephritis,
- Surgical intervention and postoperative period,
- Dermatitis,
- Holistic skin disorder
- Various types of injuries,
- Thermal, chemical burns,
- Gout,
- Rheumatoid diseases,
- Neoplasms of malignant/benign nature,
- Anemia (polysegmentation of neutrophils is observed),
- Autoimmune diseases,
- Extensive blood loss,
- Fluctuations in ambient temperature,
- Hormonal changes during pregnancy.
An upward deviation from the norm in band neutrophils can be caused by excessive physical or emotional stress.
There is also an increase in immature neutrophils while taking certain medications, such as:
- Heparin
- Corticosteroids
- Adrenalin
- Medicines containing the foxglove plant.
Band neutrophilia is observed during intoxication with lead, mercury or insecticides.
Uniform growth of band and segmented neutrophils is observed with:
- Localized purulent inflammations (appendicitis, infections of the ENT organs, tonsillitis, acute pyelonephritis, adnexitis, etc.),
- Generalized purulent inflammation (peritonitis, scarlet fever, sepsis, etc.),
- Necrotic processes (stroke, gangrene, heart attacks, etc.),
- Disintegration of a malignant neoplasm,
- Ingestion of bacterial toxins into the body without infection by the bacteria themselves (example: entry into the body of botulism toxin formed when the bacteria themselves die).
Neutrophilia is classified according to severity:
| degree | neutrophil level (x 10 9 /l) |
| moderate | to 10 |
| pronounced | 10 — 20 |
| heavy | 20 -60 |
Neutrophilia is asymptomatic and is most often detected by chance.
Decreased neutrophil levels
A condition in which the number of neutrophils in the blood is below normal is called neutropenia or agranulocytosis.
The classification of neutropenia is based on the course of the pathology:
- Chronic neutropenia , which lasts longer than 1 month,
- Acute neutropenia , developing from several hours to several days.
Neutrophil shift to the left is divided into degrees:
- Light – 1-1.5 x 109/l,
- Average – 0.5-1 x 109/l
- Heavy less than 0.5 x 109/l
The following types of agranulocytosis are distinguished:
- Primary , which is observed more often in patients 6-18 months of age. Primary agranulocytosis is characterized by an asymptomatic course. Sometimes pain in different localizations, cough syndrome, inflammation of gingival tissues, gingival bleeding,
- Secondary , the development of which is observed mainly in adults and is associated with previous autoimmune pathologies.
- Absolute , developing with whooping cough, sepsis, typhoid fever, acute leukemia, infectious mononucleosis,
- Relative , occurs in patients under the age of 12 years and is explained by the physiological characteristics of a person,
- Cyclic , characterized by the periodic development of fungal or bacterial diseases, the manifestation of symptoms with a frequency of 4-5 days every 3 weeks. Clinical manifestations of this form of the disease are migraine, fever, inflammation of small joints, inflammation of the throat, tonsils,
- Autoimmune , in which a decrease in neutrophil levels is associated with taking certain medications. Often found in patients with dermatomyositis, rheumatoid arthritis, and autoimmune diseases. A decrease in the level of cells in the blood is provoked by taking analgin, anti-tuberculosis drugs, immunosuppressants, and cytostatics. Also, this type of pathology occurs during long-term antibacterial therapy with drugs of the penicillin group.
- Febrile , which is the most dangerous form of the disease. The condition is characterized by a sudden and rapid decrease in the level of neutrophils to critical values (below 0.5 x 109/l). The development of pathology is observed during or immediately after chemotherapy, which is used to treat cancer. Febrile agranulocytosis indicates the presence of an infection in the body, the timely detection of which is often impossible. A small number of neutrophils in the blood leads to the rapid spread of infection in the body, which often leads to death. Characterized by a sharp increase in temperature to subfebrile levels, tachycardia, hypotension, weakness, profuse sweating,
The reasons for the decrease in neutrophil levels are:
- Infections,
- Inflammatory processes
- Taking certain medications
- Chemotherapy,
- Pathological processes in the spinal cord,
- Lack of vitamins
- Heredity.
Symptoms of neutropenia include:
- Febrile and subfebrile temperature,
- Ulceration of mucous membranes,
- Pneumonia,
- Sinusitis, sinusitis, rhinitis,
- Meningitis.
Changes in the leukocyte formula, including shifts in the level of neutrophils, almost always indicate the presence of a particular disease in the body. If any neutrophil changes are detected in a blood test, it is important to undergo a detailed examination and the necessary treatment.
If neutrophils in the blood deviate from the norm, it is very important to identify the cause of the disturbance as soon as possible.
The following can be used for diagnosis:
- X-ray examination of the chest,
- X-ray examination of ENT organs,
- Analysis of urine,
- Blood test for HIV,
- Bone marrow puncture.
Treatment of neutropenia and neutrophilosis is aimed primarily at treating the underlying disease that caused a violation of the level of neutrophils in the blood.
Classification of neutropenia
There are several classifications of low neutrophil levels.
By severity:
- mild degree – µl of blood contains 1000 – 1500 cells;
- medium degree - there are 500 - 1000 neutrophils per μl in the blood;
- severe - there are less than 500 cells per microliter of blood.
For reasons:
- primary – caused by genetic disorders, more common in children under 2 years of age. For example, congenital immunodeficiency conditions, dyskeratosis;
- secondary - resulting from a disease, for example, aplastic anemia or systemic lupus erythematosus, as well as taking medications. Mainly found in adults.
There is a rare disease - cyclic neutropenia, which occurs in children under 1 year of age. The level of neutrophils decreases for 3–10 days, and then returns to normal and goes down again. This cycle ranges from 14 to 36 days. The cause is a mutation in the ELANE gene, as a result of which neutrophil precursors undergo accelerated apoptosis (death) in the bone marrow.
Severe disease is characterized by the development of serious complications. Even minor deviations from the norm should not be ignored, as this may only be the initial stage of the pathology and should not be aggravated. Low neutrophil levels may be due to medication, and the cell count should return to normal when the medication is stopped.
Autoimmune neutropenia
This type of neutropenia occurs when antibodies to neutrophils are formed. It is more common in children with congenital disorders of the immune system. Antibodies to neutrophils are produced as a result of an existing autoimmune disease or in isolation to neutrophils in the absence of signs of other autoimmune lesions.
If the mother took any medications during pregnancy, the antibodies could enter the baby’s bloodstream and cause the development of autoimmune neutropenia.
Drug-induced neutropenia
Drug-induced neutropenia is characterized by a decrease in the level of neutrophils as a result of taking medications that have a toxic effect on white blood cells. These include:
- antibiotics – chloramphenicol, penicillins, cephalosporins;
- sulfonamides;
- some antipsychotics;
- anticonvulsants;
- anticonvulsants.
A low level of neutrophils is quite expected after chemotherapy and ionizing radiation, as the hematopoietic function of the bone marrow is suppressed. Neutropenia may persist for a month, so it is necessary to avoid contact with infections.
Infectious neutropenia
During an acute infectious disease, the level of neutrophils decreases. The body's immune system is weakened, which, if not properly treated, can lead to complications, for example, in the form of sepsis. In severe forms, the maturation of cells in the bone marrow is disrupted and their decay increases.
Typically, infectious neutropenia is transient and disappears on its own after 7 days.
Febrile neutropenia
Febrile neutropenia, or otherwise neutropenic fever, is a life-threatening condition that occurs suddenly in individuals with a neutrophil count of less than 500 per microliter of blood.
Such neutropenia occurs mainly after taking cytostatics for the treatment of cancer, for example, leukemia. As a result of decreased immunity, microorganisms are activated, causing intoxication of the body and an increase in temperature. The source of inflammation cannot be detected quickly; the infection can spread to other organs. Timely treatment with antibiotics helps avoid death.
Benign neutropenia
This type of neutropenia is chronic and is found in children. A low level of neutrophils does not manifest itself clinically. Doctors explain this by the immaturity of the bone marrow; tests return to normal by the age of 2 years. Until this point, it is necessary to constantly monitor the leukocyte count so as not to miss another disease.