What is it: description and code according to ICD-10
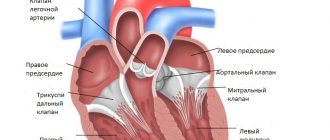
The doctor Etienne-Louis Fallot first described this disease in detail. It got its name due to the presence of 4 heart disorders:
- Absence or malfunction of the interventricular septum.
- Unnatural position of the aorta. Usually it is located above the left ventricle, but here a shift to the right occurs, and the aorta moves directly above the defective interventricular septum (dextroposition).
- Stenosis (narrowing of blood vessels) of the pulmonary artery or some part of the right ventricle, from where venous blood flows into the artery.
- Increase in tissue of the muscle of the right ventricle several times (hyperotrophy).
If the first three signs are an abnormality of the heart, then the last one is a consequence of the presence of this anomaly. When diagnosing and prognosis of the disease in the future, it will be extremely important how narrowed the pulmonary artery is and what the septal defect is. All signs in each case of the disease have a very different form of expression.
Due to the narrowing, only a small amount of venous blood enters the lungs, and the rest is sent through the deformed septum into the aorta. As a result, there is an overflow of blood in the large circulation and a lack of it in the small circulation, as a result of which oxygen starvation of the organs begins.
Tetralogy of Fallot is a congenital heart defect that is quite often diagnosed in newborns. The ICD-10 code is Q21.3.
Tetralogy of Fallot occurs in 3% of children, which is one fifth of all detected congenital heart defects. 30% of all miscarriages and non-developing pregnancies are associated with the presence of tetralogy of Fallot in the fetus, and another 7% of babies with this pathology are stillborn.
These sad figures do not at all indicate the absolute lethality of this disease, but draw attention to its severity and the inevitability of urgent medical intervention.
Tetralogy of Fallot is diagnosed if there is a combination of four anatomical defects in the structure of the cardiovascular system in a newborn:
- Stenosis or narrowing of the pulmonary artery, which leaves the right ventricle. Its immediate purpose is to conduct venous blood to the lungs. If there is a narrowing at the mouth of the pulmonary artery, then blood from the ventricle of the heart enters the artery with force. This leads to a significant increase in the load on the right side of the heart. With age, stenosis intensifies - that is, this defect has a progressive course.
- A defect in the form of a hole in the interventricular septum (VSD). Normally, the ventricles of the heart are separated by a solid septum, which allows them to maintain different pressures. With tetralogy of Fallot, there is a gap in the interventricular septum and therefore the pressure in both ventricles is equalized. The right ventricle pumps blood not only into the pulmonary artery, but also into the aorta.
- Dextraposition or displacement of the aorta. Normally, the aorta is located on the left side of the heart. In tetralogy of Fallot, it is displaced to the right and is located directly above the hole in the interventricular septum.
- Enlargement of the right ventricle of the heart. It develops secondarily due to increased load on the right side of the heart due to narrowing of the artery and displacement of the aorta.
Comparison table of triad, tetrad and pentad of Fallot.
| Disease | Triad | Tetrad | Pentad |
| Anatomical defects |
|
| Similar to tetralogy, but additionally there is a fifth defect - atrial septal defect. |
Pathogenesis
The abnormal structure of the heart in Fallot's triad leads to changes in hemodynamics at an early age. The main cause of disorders is valve stenosis. Because of it, blood cannot flow freely from the right ventricle, as a result of which the load on it significantly increases. Over time, this leads to its dilatation.
At the same time, blood flows from the left atrium to the right through a window in the septum. As a result, the pulmonary circulation becomes overcrowded.
At a late stage, Fallot's triad is characterized by such hemodynamic disorders as:
- hypoxemia – decreased oxygen concentration in the blood;
- relative tricuspid insufficiency - the reverse flow of blood from the ventricle into the atrium due to loose closure of the tricuspid valve leaflets.
Related pathologies
Tetralogy of Fallot in children is closely related to diseases such as Fallot's triad (failure of the interatrial septum, enlarged ventricle, narrowing of the pulmonary artery), Pentade of Fallot (tetralogy of Fallot and atrial septal defect).
Tetralogy of Fallot is often confused with the following diseases:
- Fusion of the pulmonary artery.
- Common arterial trunk.
- The presence of only one ventricle.
- Ebstein's anomaly.
- Double origin of the main vessels from the right ventricle.
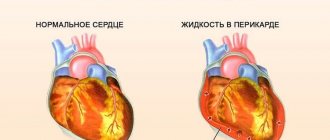
Normal heart and with Tetralogy of Fallot
Causes
Fallot's triad in children occurs due to a disruption in the process of heart formation, which occurs in the first trimester of pregnancy. Negative factors lead to improper development of endocardial folds, from which valves are then formed, destruction of the tissue of the primary interatrial septum, abnormal arrangement of blood vessels and their stenosis.
The main prerequisites for congenital heart disease in a child that arise during pregnancy:
- infectious pathologies – measles, influenza, rubella;
- endocrine disorders - diabetes;
- consumption of alcohol or drugs with teratogenic effects;
- avitaminosis;
- irradiation with gamma rays;
- prolonged fetal hypoxia.
In addition, Fallot's triad may result from chromosomal mutations or genetic predisposition.
Causes and risk factors
The anatomical structures of the heart are formed in the fetus in the first three months of intrauterine development.
It is at this time that any damaging external influences on a pregnant woman’s body can have a fatal impact on the formation of congenital heart disease.
Risk factors at this time are:
- viral diseases occurring in acute form;
- use of certain medications, psychoactive and psychotropic substances (including tobacco and alcohol) by a pregnant woman;
- heavy metal poisoning;
- radioactive exposure;
- The age of the expectant mother is more than 40 years.
European scientists have discovered that tetralogy of Fallot correlates with some genetic diseases in infants, which allowed them to assume the hereditary nature of this defect.
Disorders occur during fetal development. Tetralogy of Fallot develops before the 9th week of pregnancy, during the formation of the unborn child's heart.
Causes of Tetralogy of Fallot in newborns:
- Early illnesses suffered by the mother such as measles, rubella, scarlet fever.
- Consumption of alcoholic beverages and drugs.
- Use of sedative, hormonal, and sleeping pills.
- Exposure to bad factors.
- Ionizing radiation.
- Heredity, genetics (if one of your close relatives also had this disease)
Another reason could be a chronic illness of the mother, bad habits, or poor nutrition.
Very often, the pathology of heart disease occurs in children with Amsterdam dwarfism syndrome, which also includes syndactyly of the feet, mental retardation, Gothic palate, lack of fingers, strabismus, ear deformation, dysfunction of internal organs and much more.
Rehabilitation, lifestyle
The rehabilitation period lasts from 6 to 12 months and includes:
- High-calorie protein nutrition;
- Gymnastic exercises with a rehabilitation specialist;
- Classes at the cardiology school;
- Education for children and parents.
Patients must adhere to a certain lifestyle for life . Basic recommendations:
- Conducting physical education classes in special groups;
- Exclusion of professional sports;
- Medical examination at least 2 times a year;
- Sanitation of foci of infection (tonsillitis, caries);
- Attention to the psychological state, avoidance of stress;
- Preventive procedures (hardening, swimming) - after consultation with a doctor;
- Exemption from military service.
Prevention of the disease consists of proper planning of pregnancy and the elimination of negative factors that can provoke the development of congenital heart defects in infants (uncontrolled use of medications, alcoholism, drug addiction, unfavorable production factors, etc.).
It is very important for parents to monitor the health of their child from the first days of his birth and at the first symptoms of disorders of the heart and vascular system, immediately seek advice from a specialist.
Symptoms
Blueness of the nasolabial triangle is the main symptom of tetralogy of Fallot.
Then shortness of breath is added, by 2-3 years the child is no longer active, but breathes frequently and deeply, and sometimes faints.
External signs and symptoms of Tetralogy of Fallot in a child:
- A small hump is a bulge on the heart.
- The fingers look like drum sticks.
- The nails take on a convex shape and are rounded.
- Developmental delay.
- Frequent infection with infectious and colds (acute respiratory viral infections, sinusitis, pneumonia, and in older adults - pulmonary tuberculosis).
There are 5 types of tetralogy of Fallot in the fetus:
- Early cyanotic form (symptoms appear in the first month).
- Classic (manifestation at 2-3 years of life).
- Severe (constant attacks of shortness of breath, symptoms from 3-4 months of life).
- Late cyanotic (symptoms appear at 6-10 years of age).
- Acyanotic (pale).
Deformation of nails with Tetralogy of Fallot
Depending on the degree of narrowing of the artery and the size of the hole in the interventricular septum, the age at which the first symptoms of the disease appear and the degree of their progression changes. Let's look at the clinical picture of the disease; tetralogy of Fallot is characterized by:
- Cyanosis. Most often it appears in children under the age of one year, first on the lips, then on the mucous membranes, face, arms, legs and torso. Progresses as the child’s physical activity increases.
- Thickened fingers in the form of “drumsticks” and convex nails in the form of “hour glasses” are formed by the age of 1-2 years.
- Shortness of breath in the form of deep arrhythmic breathing. At the same time, the frequency of inhalations and exhalations does not increase. Shortness of breath worsens with the slightest physical exertion.
- Fast fatiguability.
- The cardiac hump is a bulge on the chest in the area of the heart.
- Delayed motor development due to forced restrictions in physical activity.
- Heart murmurs.
- The typical body position of a sick child is squatting or lying down with legs bent to the stomach. It is in this position that the baby feels better and therefore unconsciously accepts it as often as possible.
- Fainting up to the state of hypoxemic coma.
- “Blue” attacks of shortness of breath and cyanosis during a severe paroxysmal course of the disease, in which young children (1-2 years old) suddenly turn blue, begin to choke, become restless, and then may lose consciousness or even fall into a coma. After the attack, the child was lethargic and drowsy. Often, as a result of such an exacerbation, the baby may even die.
If you suspect tetralogy of Fallot, you should consult a doctor immediately. The child requires emergency consultation with a cardiologist or cardiac surgeon.
The attack develops with a significant narrowing of the pulmonary trunk and is typical for young children. Caused by spontaneous contraction of the right ventricle, which worsens hypoxemia. Oxygen deficiency provokes brain hypoxia, and excess carbon dioxide stimulates the respiratory center.
The attack is manifested by sudden inspiratory shortness of breath (difficulty and increased inhalation). The child's breathing resembles that of a foreign body and is accompanied by a generalized bluish discoloration of the skin. The patient takes a forced squatting position and loses consciousness within 1-2 minutes.
Algorithm of actions:
- Call an ambulance.
- Protect the child from strangers.
- Provide fresh air flow.
- Unbutton your clothes.
- Make sure the airway is clear.
Upon arrival of the ambulance, emergency measures are taken:
- oxygen therapy through a mask (20% moist oxygen);
- determination of vital signs;
- administration of bronchodilators and cardiotonics (aminophylline, norepinephrine);
- taking an ECG and simultaneous preparation for the administration of antiarrhythmics (the attack is often complicated by fibrillation);
- transportation to a hospital facility.
All drugs are administered intravenously. While providing assistance, paramedics keep a defibrillator at the ready. In the hospital, the child’s condition is stabilized with heart medications and oxygen therapy.
Symptoms of Fallot's triad
The clinical course of Fallot's triad is determined by the severity of hemodynamic disorders and can be different. Most children already at an early age experience shortness of breath when feeding, crying, or moving; fatigue, delayed physical development. Cyanosis usually appears by age 8–12 years; with the development of cyanosis at a younger age, one can usually think of severe pulmonary stenosis. With Fallot's triad, a child may develop hypoxemic attacks, characterized by sudden agitation, increased breathing, increased cyanosis, suffocation, loss of consciousness, and convulsions.
When examining a patient with Fallot's triad, all the signs of a “blue” type of defect are evident: cyanosis, “clubs”, a typical squatting position, swelling and pulsation of the neck veins. Ocular hypertelorism (widely spaced eyes) is often found.
Complications of Fallot's triad, which can lead to the death of a child, include thromboembolism and brain abscesses, infective endocarditis after respiratory or bacterial infections, massive bleeding caused by rupture of large collaterals or surgical interventions (tooth extraction, tonsillectomy, etc.), chronic cardiac failure.
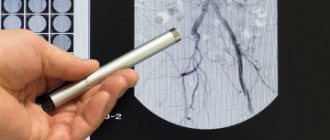
Diagnostics
Typically, blue heart disease can be seen on electrocardiography, which indicates the presence of right ventricular hyperotrophy, phonocardiogram, where a murmur can be heard over the pulmonary artery, and x-ray, where the heart appears like a shoe and the cardiac shadow is enlarged.
Pathology can be detected using the following diagnostics:
- Ultrasound - ultrasound examination (level of aortic displacement, level of pulmonary narrowing, malfunction of the interventricular septum).
- Catheterization and examination of the cavities of the heart (to detect increased pressure in the ventricles, oxygen starvation of the aortas).
- Doppler ultrasound.
- Aortography and pulmonary arteriography (existence of collateral blood flow and pulmonary artery disease).
- MRI of the heart.
- Left ventriculography.
- Multislice computed tomography.
Detecting Tetralogy of Fallot on X-ray
It is also often possible to identify a diagnosis with the help of certain studies and analyses, and geneticists can also help with this, since the basis of the disease is a violation of all genes in the body, and therefore a violation of the embryo.
A gynecologist can also diagnose Tetralogy of Fallot, since the causes are often:
- Hydrops fetalis.
- Maternal phenylketonuria syndrome.
- Fetal alcohol syndrome.
The disease is diagnosed based on anamnesis, after a clinical examination and auscultation of the chest, taking into account the results of instrumental research methods.
Inspection:
- Universal blue discoloration of the skin and mucous membranes throughout the body.
- Growth retardation, dystrophy 2-3 degrees.
- Heart hump.
- Fibrous changes in the fingers and nails (“watch glasses”, “drumsticks”).
Palpation:
- In the projection of the pulmonary artery (the level of the second intercostal space on the left of the sternum), systolic tremor is determined.
- A cardiac impulse is detected in the costal angle.
Auscultation:
- A continuous systolic murmur is heard in the 2nd intercostal space on the left.
- The second tone is muted.
- At Botkin's point there is a soft systolic murmur caused by the discharge of blood through a septal defect.
Laboratory data:
- Polycythemia (increased levels of blood cells and hemoglobin).
- Slowing down of ESR to 2-0 mm per hour.
X-ray:
- Decreased blood supply to the lungs (pallor of the roots).
- Flattening of the pulmonary trunk arch.
- Horizontal position of the right ventricle.
- Shift of the aortic arch to the right.
- Emphasized heart waist on the left.
- Shift of the heart axis to the right.
- Significant elevation of the R wave in the right leads (V1-V2).
- Possible signs are bifurcation of the R wave, arrhythmias.
- Confirmation of all components of the vice.
- Heart in the shape of a “shoe”.
- Discharge of blood from right to left.
- Pressure difference between the ventricles.
From a diagnostic point of view, the most valuable is cardiac ultrasound with Doppler. Invasive research methods such as angiography and cardiac catheterization in newborns are rarely performed, only in case of unsatisfactory quality of results using other diagnostic methods.
In most cases (50-70%), the defect is diagnosed after birth. A large number of diagnostic omissions are due to the insufficient quality of the ultrasound machine (ultrasound diagnostics is the main method of diagnosing the fetus).
Comprehensive diagnostics during pregnancy for the presence of tetralogy of Fallot in the fetus includes:
- Genetic counseling with karyotype determination (the defect is often combined with congenital syndromes - Patau, Down).
- Determination of the size of the collar space in the 1st trimester - the size exceeds 3.5 mm.
- An ultrasound scan in the 1st trimester indicates gross disturbances in the formation of the heart (often also in other organs).
- Ultrasound of the fetus in the 2nd trimester - pulmonary stenosis, septal defect, dextroposition of the aorta.
- Color mapping – turbulent blood flow, insufficient venous flow into the pulmonary artery.
Further tactics:
- When diagnosed before 22 weeks, a woman must determine whether she wishes to continue the pregnancy.
- If consent is given, the pregnant woman is observed by a therapist and an obstetrician-gynecologist before birth.
- Delivery is carried out naturally.
- The child comes under the supervision of a neonatologist, after which he is registered with a cardiologist and cardiac surgeon.
- The time of surgery is planned.
The timing of the intervention depends on the degree of narrowing of the pulmonary artery. With significant stenosis, the operation is performed in the first month of life, with moderate stenosis - within 3 years from birth.
Diagnosis of the disease
Differential diagnosis of the pentade of Fallot is carried out with other congenital heart diseases accompanied by pulmonary artery stenosis. The following methods are used for diagnosis:
- General examination and listening to heart rhythm . Typical signs of the defect are a rough systolic murmur, which is heard in the left region of the sternum and weakening of the second sound of the pulmonary artery. Pulse and systolic pressure in patients is reduced.
- Electrocardiogram . The electrocardiogram shows signs of right-sided cardiac hypertrophy (positive T wave, high P wave).
- X-ray examination . Determines the expansion of the borders of the heart and its shape, as well as post-stenotic expansion in the pulmonary trunk. The pattern of the lungs and their roots may be normal (if the ductus arteriosus is open) or slightly weakened.
- Ultrasound of the heart . Ultrasound examination can determine all the main components of the pentade of Fallot: the degree of pulmonary stenosis and aortic displacement, the size of the ASD, the severity of right ventricular hypertrophy (about the indicators of this pathology on the ECG - here).
- Angiography . Allows you to clarify the type of disorders and exclude other defects, which include pulmonary stenosis and other symptoms.
- Selective ventriculography . By injecting a contrast agent, the doctor sees the contours of the right ventricle and identifies defects in the aorta and interventricular septum.
Hemodynamics
With the defect, the following sequential hemodynamic disturbances develop:
- Due to narrowing of the pulmonary artery, the right ventricle experiences volume overload (from the right atrium) and pressure (from the pulmonary artery). The overflow of blood causes an increase in its striking force;
- When the pressure in the right ventricle becomes critical, venous discharge begins from right to left;
- From the left ventricle mixed blood enters the aorta;
- The aorta, due to congenital dextroposition, additionally receives blood from the right ventricle;
- The content of carbon dioxide in the blood increases, oxygen decreases (hypoxemia);
- Hypoxia begins in the internal organs, which is aggravated by depletion of the pulmonary circulation;
- Due to oxygen deficiency, polycythemia develops - an increase in the level of blood cells and hemoglobin.
Causes and classification of congenital heart disease (CHD)
Causes of congenital heart disease:
- manifestation of a hereditary disease (Down syndrome);
- effects of harmful factors on the fetus during pregnancy;
- manifestation of a non-hereditary disease.
All congenital heart defects of any complexity form four groups:
- with enrichment of the systemic circulation;
- with depletion of the systemic circulation;
- with enrichment of the pulmonary circulation;
- with depletion of the pulmonary circulation.
The fourth type includes three complex similar heart defects: tetralogy, triad and pentad of Fallot. All three types cause a characteristic cyanosis of the skin, for which they are called “blue” defects.
Types of congenital heart disease and stages of its development
Depending on the anatomical features of the defect, several types of tetralogy of Fallot are distinguished:
- Embryological - the maximum narrowing of the artery is at the level of the demarcating muscle ring. The stenosis can be corrected by sparing resection of the conus arteriosus.
- Hypertrophic - the maximum narrowing of the artery is at the level of the demarcating muscle ring and the entrance to the right ventricle. The stenosis can be corrected with massive resection of the conus arteriosus.
- Tubular - the entire arterial cone is narrowed and shortened. Patients with this defect cannot undergo radical surgical correction of pulmonary artery stenosis. For them, palliative plastic surgery is preferable to prevent the worsening of the disease.
- Multicomponent - arterial stenosis is caused by a number of anatomical changes, the position and characteristics of which determine the successful outcome of surgical correction of stenosis.
Depending on the characteristics of the clinical manifestations of the defect, the following forms are distinguished:
- cyanotic or classic - with pronounced cyanosis (blueness) of the skin and mucous membranes;
- acyanotic or “pale” form - more common in children in the first 3 years of life as a result of partial compensation of the defect.
Depending on the severity of the disease, the following forms of the disease are distinguished:
- Heavy. Shortness of breath and cyanosis appear almost from birth during crying and feeding.
- Classic. The disease debuts at the age of 6-12 months. Clinical manifestations closely correlate with increased physical activity.
- Paroxysmal. The child suffers from severe dyspnea-cyanotic attacks.
- Mild form with late onset of cyanosis and shortness of breath - at 6-10 years.
In its course, the disease goes through three successive stages:
- Relative well-being. Most often, this phase lasts from birth to 5-6 months. There are no pronounced symptoms of the disease, which is due to partial compensation of the defect due to the structural features of the newborn’s heart.
- Cyanotic phase. The most difficult period in the life of a child with tetralogy of Fallot lasts 2-3 years. At the same time, all clinical manifestations of the disease are clearly expressed: shortness of breath, cyanosis, attacks of suffocation. This age group accounts for the greatest number of deaths.
- Transitional phase or phase of formation of compensatory mechanisms. The clinical picture of the disease remains, but the child adapts to his illness and is able to prevent or weaken attacks of the disease.
Types of tetralogy of Fallot
It is customary to distinguish 4 types of tetralogy of Fallot according to the characteristics of anatomical changes.
- Embryological - narrowing is caused by anterior displacement of the septum to the left and low localization. Maximum stenosis coincides with the level of the anatomical demarcation muscle ring. In this case, the structures of the pulmonary valve are practically unchanged, moderate hypoplasia is possible.
- Hypertrophic - pronounced hypertrophy of the exit zone from the right ventricle and the dividing muscle ring is added to the mechanism of the previous type.
- Tubular - obstruction is caused by incorrect division in the embryonic period of the common arterial trunk, due to which the pulmonary cone (the future of the pulmonary artery) turns out to be underdeveloped, narrowed and short. At the same time, it is possible to change the valve apparatus.
- Multicomponent - all of the listed factors are partially involved in the formation.
Possible postoperative complications
The diagnosis of tetralogy of Fallot is classified as a severe heart defect with high mortality. If the course of the disease is unfavorable, the average life expectancy of the patient is 15 years.
The following complications of the disease are common:
- thrombosis of blood vessels in the brain or lungs due to increased blood viscosity;
- brain abscess;
- acute or congestive heart failure;
- bacterial endocarditis;
- delayed psychomotor development.
Complications occur in 2.5-7% of cases and are associated with injury to the microstructures and blood vessels of the heart, and incorrect surgical technique:
- Damage to conductive fibers.
- Sudden cardiac arrest.
- Rupture of the pulmonary valve and the entire fibrous ring.
- Inadequate resection of the right ventricle (removal of too much myocardium).
Fallot's triad prognosis
The prognostic value for Fallot's triad is mainly the degree of pulmonary artery stenosis. Patients with a mild form of Fallot's triad can remain active for up to 40-50 years. An unfavorable criterion is the early appearance of shortness of breath and cyanosis. With a significant degree of stenosis, patients, as a rule, die at a young age due to heart failure. Surgical correction of Fallot's triad is accompanied by increased survival and good long-term results.
Patients with Fallot's triad require sanitation of chronic foci of infection and dynamic monitoring by a cardiologist and cardiac surgeon.
Treatment methods
Surgical treatment is indicated. The optimal age for surgery is up to 3-5 years. But you still need to grow to this age, having gone through the stage of severe cyanosis and shortness of breath in a child at 1-2 years old.
Quite often, children with tetralogy of Fallot die during severe dyspnea-cyanotic attacks at an early age, if they are not provided with competent medical care and support:
- prevention and treatment of concomitant diseases (anemia, rickets, infectious diseases);
- prevention of dehydration;
- sedative therapy;
- treatment with adrenergic blockers;
- treatment with antihypoxants and neuroprotectors;
- oxygen therapy;
- maintenance therapy with vitamins and minerals.
The only contraindication to radical surgical correction for tetralogy of Fallot may be severe
pulmonary hypertension in newborns
. Otherwise, surgery is the most effective method of treatment.
Depending on the anatomical features of the existing defect, preference is given to the method of surgical intervention:
- Palliative surgery is practiced when it is impossible to completely eliminate a heart defect. Necessary to optimize the patient’s quality of life. Most often, an aortopulmonary anastomosis is performed - that is, the pulmonary artery is connected to the subclavian artery using synthetic implants. Sometimes palliative surgery is just the first stage of surgical intervention in a child under 1 year old - it allows the baby to live for several more years before undergoing radical correction of the defect.
- Radical correction involves elimination of the ventricular septal defect and expansion of the pulmonary artery. This is an open heart surgery, after which the child will be able to lead an almost normal life after some time. It is important to note that this operation is recommended for children at least 3-5 years old.
Treatment of Fallot's triad
Regardless of the severity of the clinical manifestations of Fallot's triad, surgical treatment of the defect is indicated. The exception is cases of Fallot's triad, complicated by irreversible pulmonary hypertension. When hypoxemic crises occur, oxygen therapy is administered, sedatives, beta-blockers, and cardiac glycosides are administered.
With Fallot's triad, palliative anastomotic operations are not performed, since they cause even greater overload of the right side of the heart. Radical correction of Fallot's triad involves immediate or staged elimination of pulmonary artery stenosis by Broca's valvotomy and closure of the atrial septal defect. After the operation, there is a disappearance of cyanosis, a decrease in pressure in the right ventricle and an increase in the pulmonary artery, and restoration of the volume of pulmonary circulation.
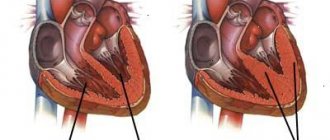
Stages of surgical treatment
The operation consists of two stages - radical and palliative. Palliative surgery is performed to alleviate the condition of life, radical surgery is performed to eliminate the defect.
It is performed routinely for children under 3 years of age in a cardiac surgery hospital. Access is only open (opening the chest).
Stages:
- Dissection of the ribs and removal of the sternum.
- Opening of the chest cavity and incision of the pericardial sac.
- Insertion of a valvulotome into the heart cavity.
- Dissection of the walls of the pulmonary trunk to expand its diameter.
The result of the operation is to improve the flow of venous blood into the lungs and eliminate hypoxia.
Instead of valvotomy, other interventions may be performed:
- Resection – removal of a narrowed area of the right ventricle in order to increase its cavity;
- Creation of bypass pathways of blood flow - suturing the subclavian artery or aorta to the branches of the pulmonary trunk.
It is performed when a heart-lung machine is connected 3-6 months after the first intervention.
Stages:
- Opening the chest cavity.
- Connecting a heart-lung machine.
- Cardioplegia (exclusion of the heart from the systemic circulation).
- Compression of the aortic walls.
- Opening of the right ventricle.
- Suturing a septal defect.
- Additional suturing of a patch to the right ventricle to increase the size of its cavity.
The mechanism of circulatory disorders in Fallot's defects
As pathology develops, the arterial cone rotates in such a way that the aortic valve moves to the right of the pulmonary valve. In this case, the aorta itself takes the “rider” position, located above the interventricular septum of the heart. The wall of the arterial cone is unable to join the septum, so a defect occurs in it.
With an abnormal location of the aorta, the pulmonary trunk narrows and becomes long. The right ventricle (RV) enlarges, as it is difficult for it to push blood through the narrow lumen of the pulmonary artery, and it is difficult for it to enter the pulmonary artery from the RV. Since there is an opening between the two ventricles, mixed blood enters the aorta. It contains less oxygen than normal.
Hemodynamic disorders in tetralogy of Fallot
If the mouth of the pulmonary artery is completely blocked, then the lungs are supplied with arterial blood through additional vascular branches. With moderate narrowing, blood from the left ventricle enters the right, and the “white” form of the disease develops. Subsequently, it becomes mixed, then there is a discharge of venous blood into the left ventricle - the “white” form changes to “blue”.
Possible postoperative complications
Without surgery, 3% of patients survive to 40 years of age. Successful surgery allows patients to achieve longevity (70 years or more). Further observation leads to lifelong registration, monitoring of physical activity, and treatment of concomitant diseases.
Statistics on how long people with this diagnosis live:
- Five-year survival rate after surgery: 92-97%.
- Live up to 20 years: 87-88% of patients.
- Live up to 30 years: 77-80% of patients.
- The average life expectancy after intervention is 66-72 years.
- Life expectancy with concomitant diseases (arrhythmia): 50-55 years.
Prognosis after treatment
Survival rate after surgery for pentade of Fallot is 96%. The prognosis is relatively favorable. The life expectancy of those treated is reduced by 10-15 years compared to healthy people and averages 65-70 years.
Possible postoperative complications (anastomotic thrombosis, arrhythmias, endocarditis) occur in 4-5% of cases and worsen the prognosis, as they often require new surgical intervention on the injured myocardium.
Without surgery, 50% of children survive to 5 years of age; only 25% survive to 10 years of age.
The quality of life of those treated may be reduced by concomitant arrhythmia, arterial hypertension, and angina pectoris. Patients are registered for life and undergo treatment for these diseases.
Tetralogy of Fallot in newborns: what is it, symptoms, treatment
Tetralogy of Fallot is one of the types of congenital heart defects.
It is characterized by four signs: dextraposition (incorrect right-sided position) of the aorta, the presence of a gap in the wall located between the two ventricles, significant dilation of the right ventricle and stenosis of its outlet section.
Features of the pathology
This form of the defect is closest to the triad and pentade of Fallot, which have, respectively, 3 (there is no displacement of the aorta) and 5 characteristic signs (including pathology of the interatrial septum), the same as those that characterize tetralogy of Fallot.
This pathology accounts for about 10% of all cases of congenital heart defects. If we talk about congenital heart disease of the cyanotic type, it occurs in half of the cases.
With such a violation, the conus arteriosus changes its location, and the aortic valve moves to the right of the pulmonary valve. It appears above the septum located between the two ventricles, while there is no attachment of the wall of the arterial cone to the septum itself: this occurs because a defect occurs in it.
The pulmonary trunk becomes narrowed and lengthens, and the right ventricle enlarges, due to the fact that it is difficult for blood to enter the artery leading to the lungs.
The presence of an opening between the ventricles facilitates the mixing of blood entering the aorta. Mixed blood, in turn, has a low oxygen content.
How does hemodynamics change?
Most often, with this disease, the mouth located in the artery is blocked. In this case, additional branches of vessels appear that supply the lungs with arterial blood. After which it mixes, and venous blood is discharged into the left ventricle - the “white” form changes to “blue”.
Tetralogy of Fallot is of the “blue” type because the mixing of arterial and venous blood leads to cyanosis.
In general, the movement of blood through the vessels is determined by how severe the artery stenosis is. It also correlates with how clearly arterial hypoxemia manifests itself, as well as the severity of the condition of the body as a whole. If the stenosis is significant, then blood flows from the ventricles into the aorta, but its flow into the pulmonary artery is difficult.
The volume in which the systemic circulation is expressed is increased. Moreover, since the aorta is located in the shape of a “rider”, blood flows freely into it from the right ventricle, and insufficiency does not develop in it, and the pressure in the ventricles is equalized.
The extreme form of the disease involves the entry of arterial blood into the pulmonary circulation through collaterals or open arterial flow. The moderate form has the following features: the release of blood into the aorta is higher than into the lungs, a left-right discharge occurs, which is why the clinical manifestation has a pale form of the defect.
The moderate form of tetralogy of Fallot most often occurs in young children, but there are also cases of manifestation in adolescents.
Development factors
The most common factor due to which Fallot's disease occurs and develops is a disorder that occurs in the development of the heart during the period from the second to the eighth week of embryonic growth, when the formation of this organ occurs.
In addition, the disease can occur due to the fact that during pregnancy the woman suffered from infectious diseases, for example, measles.
The intake of alcohol, drugs and medications in the presence of contraindications for pregnancy also has a negative effect.
Sometimes this heart defect can occur unexpectedly, for no apparent reason. The processes that can lead to these consequences have not yet been sufficiently studied.
The influence of heredity on the possibility of a child developing a defect is also noted.
Possible types of pathology
There are several options for the development of the disease.
Anatomical signs can appear either together or one at a time:
| Type of leakage | Anatomical features | Treatment method |
| Embryological |
| Surgical intervention |
| Tubular | Narrow, shortened pulmonary cone, underdeveloped. | |
| Multicomponent | The conical septum is elongated and its origin is located high. | |
| Hypertrophic | The arterial conical septum is enlarged in size and its origin is high. | Palliative plastic surgery |
With tetralogy of Fallot, the following forms of hemodynamic disturbances occur, which were identified in the clinical and anatomical classification:
- cyanotic in combination with stenosis of the orifice;
- acyanotic.
Sometimes a third form is also distinguished: in this case, there is atresia of the mouth of the pulmonary artery.
Fallot's defect can also have a severe, classic and mild form:
- In the first case, shortness of breath and cyanosis occurs in infants during feeding from birth.
- In the second, the first manifestations of the disease occur in a child aged from six months to a year.
- In the third - from 6 years of age until puberty.
Characteristic symptoms
The manifestations of this disease vary depending on what stage of development it is at, there are three in total:
| Stage | Symptoms | Age |
| Initial | Most often there are no pronounced manifestations, but the baby may suffer from shortness of breath during feeding. | About 5 months |
| Cyanotic |
| 2-3 years |
| Transitional | Similar to the previous stage with the difference that the manifestations are stopped or weakened with the help of therapy. | From 3 years to the end of life |
According to the timing, the first manifestations begin to appear from birth and can either completely disappear or remain until the end of life.
Diagnostic methods
When diagnosing, the following clinical picture is usually distinguished:
- the patient experiences frequent fainting;
- he cannot take a deep breath;
- dextroposition of the aorta and myocardial hypertrophy are detected;
- Pain in the thoracic region periodically appears.
When identifying a disease such as tetralogy of Fallot, the most effective diagnosis is considered to be an intrauterine examination.
It is carried out using an ultrasound machine, the accuracy of the result depends on its level. If the fetus is examined by a specialist on time, then it is possible to detect the disease at an early stage: up to 21 weeks.
In the third trimester, the probability of detecting such a disorder is about 100%. In severe cases of the defect, differential diagnosis is carried out to help determine an accurate diagnosis: a number of obvious signs of the disease present in a newborn do not always indicate that it is tetralogy of Fallot.
In addition to performing an ultrasound of the heart, the defect can be identified using genetic testing. Such screening is mandatory for a period of about 4 months. Moreover, in 35% of pathology detections, it can be combined with diseases resulting from chromosome disorders, for example, Down syndrome.
When diagnosing Fallot's defect, echocardiography is also performed, which helps to make the most accurate diagnosis, especially if it is in infants. The echocardiogram result determines the subsequent treatment strategy.
Color Doppler ultrasound, in turn, determines the direction of blood flow.
Auscultation helps to listen to systolic murmurs located in the left edge of the chest. The apex beat of the heart is usually weak and can be palpated in the 4th-5th intercostal space. And also by auscultation it is possible to determine the transmitting pulsation located in the epigastric region.
An x-ray is also one of the important components of a comprehensive analysis, since x-rays can reveal signs of a specific form of the disease. In this way, important radiological signs can be determined: displacement of the aorta, location of the septum conus and the condition of other organs.
How is the treatment carried out?
The choice of the most effective treatment depends on the specific type of Fallot's disease.
| Type | Treatment methods | |
| Embryological | Economical | Resection of the conus arteriosus |
| Hypertrophic | Massive | |
| Tubular | Conservative method of palliative plastic surgery | |
| Multicomponent | Surgery to correct stenosis |
In this case, the use of glycosides is contraindicated for the patient, as they can provoke an attack. Radical correction using surgical methods, in turn, is most often carried out in case of a multicomponent type of disease or complications.
Help during a seizure
With this diagnosis, patients at the cyanotic stage can sometimes develop heart failure. This happens due to frequent dyspnea-cyanotic attacks.
If an attack occurs, proceed as follows:
- lay the patient on his side, bend his legs to his stomach or squat;
- provide oxygen;
- give an injection or drip with morphine;
- if no improvement is observed, an injection of sodium bicarbonate is given;
- for convulsions, hydroxybutyrate is administered.
The dosage of medications should be prescribed by the doctor who is seeing the patient.
Surgery
In most cases, radical correction is chosen as treatment, otherwise the prognosis is quite disappointing: without treatment, the disease in severe form is fatal for children under the age of one year.
In pediatrics, the disease itself is an indication for surgery, unless the child has a contraindication in the form of pulmonary hypertension or other exceptional factors.
Surgical intervention occurs as follows:
- first close the hole in the septum;
- then, depending on the severity of the disease, part/all of the heart muscle on the right side is removed, the valve is adjusted/replaced, or a shunt is installed between the heart and the vessels connecting to the lungs.
In 80% of cases, surgical interventions for this pathology are successful. There are also cases when it is necessary to carry out not one, but several operations. After this, the patient should undergo regular follow-up.
The price of a particular operation depends on its complexity and whether subsequent intervention will be necessary. On average in Moscow, its cost varies from 132,000 to 200,000 rubles.
Forecast for future life
On average, life expectancy with such a diagnosis in a mild form is up to 12 years, if the patient does not undergo surgery, regardless of when the diagnosis was made.
And only 5% of people with a mild form of the defect, who had it in childhood, but were not operated on, survive to the age of 40 years. An adult who underwent surgery as a child should be constantly monitored by specialists and take maintenance medications.
Even during surgery, there is a possibility of a sudden stroke, which threatens the patient’s life and in some cases can be fatal.
Specialists who studied pathology identified the following pattern: the earlier the surgical intervention was performed, the greater the likelihood of a positive outcome. Dmitrieva Yulia (Sych) – In 2014, she graduated with honors from Saratov State Medical University named after V. I. Razumovsky. Currently working as a cardiologist at the 8th City Clinical Hospital in the 1st clinic.
Source: https://infoserdce.com/serdce/chto-takoe-tetrada-fallo/
Clinical recommendations and prognosis
With timely detection of the defect and its prompt treatment, the prognosis is favorable . Otherwise, patients suddenly die in childhood or adolescence from acute heart failure.
With this diagnosis, it is important for parents to take all possible measures:
- Active and round-the-clock monitoring of the child.
- Registration of the child and regular examination by a therapist, cardiologist, or cardiac surgeon.
- Avoid intense physical activity, stress, hypothermia, and active sports.
- Healthy eating.
- Planning with a cardiac surgeon the time for surgical intervention (this is the only effective method of treating the defect). The operation "valvotomy" is an expansion of the pulmonary artery trunk in combination with closure of the atrial septal defect.
- Perform surgery as early as possible.
- Monitoring the child in the postoperative period and ensuring quick and comfortable adaptation for him.
There is no specific prevention for this disease. As with other congenital defects, the best preventive measure is a healthy pregnancy and an undisturbed heredity .
Patients with an already identified defect, even after a successful operation, must be constantly monitored by a cardiologist, avoid high physical activity and try not to get sick.
Fallot's triad is undoubtedly dangerous, but not hopeless. Doctors know how to do everything possible so that a child with such a heart defect can live a full life - you just need to contact them in time and entrust them with the life of your baby!
Pentade of Fallot: characteristics and treatment
This disease is a combination of 5 symptoms:
- PA stenosis;
- dextroposition of the aorta;
- IVS defect;
- MP defect;
- right ventricular hypertrophy.
Heart rhythm disturbances due to illness
In other words, the pentade of Fallot is the same tetralogy of Fallot, but with the addition of one more sign - a violation of the integrity of the interatrial septum. Significant defects in this area are extremely rare. Most often, doctors note incomplete closure of the hole. It develops due to incomplete formation of the valve. The disease is characterized by the release of blood in small quantities through a loosely fitting valve of the oval opening.
Due to differences in blood ejection vectors, a person experiences pronounced hypoxemia. But it also happens that the splash goes in the direction from left to right. This means that there is an extra load on the right ventricle, which somewhat compensates for the symptom.
Clinical studies are carried out exactly the same as with tetrad. The doctor makes a conclusion only after performing cardiac probing and a procedure called angiocardiography.
Defects in adults
Drug treatment is ineffective, so doctors perform operations. Both pentad and tetralogy of Fallot are treated in the same way, but there is one caveat - doctors need to restore the integrity of the MPP. The prognosis for people suffering from the disease is not very favorable. However, it is more positive than with tetrad. This is due to compensation of arterial hypoxemia. The earlier radical intervention is performed, the greater complications can be avoided, but the life expectancy of patients with such defects rarely exceeds 40 years.