- In what cases can we talk about hypertension?
- Why does blood pressure rise?
- What does this mean?
- What causes the pathology?
- How does hypertension manifest?
- Additional examination
- Principles of therapy
- Choosing your due date
- Prevention options
Changes in the body of a pregnant woman normally lead to a decrease in blood pressure.
Under the influence of placental estrogens and progesterones, blood vessels lose sensitivity to the hormone angiotensin-II. They are in an expanded state, their resistance to blood flow decreases. This is necessary for normal growth of placental vessels and provision of nutrition to the fetus. Therefore, in the first trimester, the pressure decreases from the original by 5-15 mm Hg. Art., falls a little more in the second. And in the third there is a return to the physiological norm. But in some women, conception occurs against the background of high blood pressure or hypertension occurs during pregnancy. This condition is dangerous for the mother and the fetus.
In what cases can we talk about hypertension?
In pregnant women, arterial hypertension is diagnosed in 4-8% of all pregnancies. Despite such a small percentage of the disease, it ranks second among the causes of maternal mortality. Therefore, the disease must be detected and treated promptly.
If pressure above normal was determined during a single measurement, then this does not mean anything. For diagnosis, several conditions must be met:
- Increase in blood pressure to 140/90 mm Hg. Art. and higher.
- Increase in indicators in comparison with the period before pregnancy: systolic by 25 mm Hg. Art., diastolic - by 15 mm Hg. Art.
- Changes are determined by two consecutive measurements, between which at least 4 hours have passed.
- Single-time increased diastolic pressure above 110 mm Hg. Art.
Hypertension in pregnant women proceeds in stages similar to conventional hypertension:
- Stage 1 – pressure from 140/90 to 159/99 mm Hg. Art.;
- Stage 2 – blood pressure from 160/100 to 179/109 mm Hg. Art.;
- Stage 3 – blood pressure from 180/110 or more.
According to classification, pathology can be of several types. Depending on the date of appearance:
- Hypertension that existed before pregnancy - the woman was diagnosed with hypertension or the first signs appeared before the 20th week of gestation, symptoms of this form persist more than 42 days after birth.
- Gestational hypertension - initially normal blood pressure after 20 weeks rises to significant levels above normal.
- Preeclampsia is a combination of high blood pressure and protein in the urine.
- Existing hypertension in combination with proteinuria and gestational hypertension - the pregnant woman was diagnosed, but after 20 weeks the symptoms begin to increase, protein appears in the urine.
- Unclassifiable hypertension due to lack of information.
The course of the disease is gradual. At the initial stage, there is no damage to target organs. As the condition progresses, pathological changes in the kidneys are observed, up to renal failure. Signs of ischemia increase in the heart, angina pectoris and heart failure develop. Damage to the blood vessels of the brain, retina, and the development of atherosclerosis of the carotid arteries are also possible.
Stages
Gestational hypertension, information about which can be found in ICD 10, has several stages of development. It can occur in degrees:
- Light;
- Average;
- Heavy.
The severity of hypertension in expectant mothers is usually determined by the level of blood pressure and the amount of protein present in the urine. Additionally, doctors include two life-threatening conditions in the classification of pathology:
- Eclampsia. Characterized by loss of creation and convulsions. With this complication, the probability of survival of patients is very low;
- Preeclampsia. It is observed with high blood pressure readings on the tonometer, as well as with convulsive readiness. The patient develops severe headaches and constantly feels dry in the mouth. The picture of the disease is complemented by darkening in the eyes and the appearance of flickering goosebumps.
In some countries, both conditions are included in the description of moderate and severe preeclampsia.
Why does blood pressure rise?
It is generally accepted that initially any hypertension has neurotic causes. This is a deep neurosis that leads to disruption of the regulation of blood vessels. The development of pathology is aggravated by existing diseases of the blood vessels, brain, and kidneys in the past. The situation is aggravated by excess weight, excessive consumption of table salt, smoking and alcohol.
The development mechanism is associated with a physiological increase in the volume of circulating blood. If there is a lack of placental 17-hydroxyprogesterone, then the high sensitivity of the vessels to the hormone vasopressin remains, they easily go into a state of spasm, which entails an increase in pressure.
Changes in the heart (hypertrophy) are aimed at compensating for the condition of hypertension, but this leads to even greater deterioration. The vessels of the kidneys are gradually affected, which further perpetuates the pathology.
Causes of hypertension in pregnant women
Cardiologists believe that the main factor provoking the occurrence of pathology is stress. Hypertension in pregnant women appears as a result of emotional shocks, mental and mental overload. They lead to the occurrence of neurocirculatory dystonia (NCD).
The majority of cardiologists' patients have previously experienced increased blood pressure (episodically or systematically). Even if high blood pressure values were not recorded in the medical record, the doctor makes a conclusion about the existence of pathology based on the woman’s interview. In this case, arterial hypertension and pregnancy are phenomena not directly related to each other.
The presence of concomitant diseases, which sometimes are not even identified at the time of the first visits to the obstetrician-gynecologist, can also provoke the disease. Therefore, when a combination such as hypertension and pregnancy occurs, treatment is carried out taking into account concomitant diseases. Among such pathologies are disorders of the endocrine system (thyrotoxicosis, diabetes mellitus), problems with the kidneys, and respiratory system organs.
In addition, other factors that cause hypertension during pregnancy play an important role. As a result of the changes occurring in a woman’s body, the load on the circulatory system increases, which cannot always cope. Blood pressure rises due to the following reasons:
- insufficient increase in vascular volume;
- compression exerted by the growing uterus on the diaphragm;
- increased blood volume in a pregnant woman;
- the occurrence of placental circulation;
- changes in the position of the heart inside the chest;
- high levels of hormones;
- late gestosis.
Hypertension in pregnant women can also threaten if a woman decides to become a mother already in adulthood - after 30-35 years - or when she is very young. Carrying several babies and a large volume of amniotic fluid can also cause high blood pressure.
What does this mean?
Hypertension and pregnancy are a dangerous combination. With high pressure, the lumen of blood vessels narrows. In this case, already in the early stages of pregnancy, blood flow in the placenta is disrupted. The fetus does not receive enough nutrition and oxygen, its development slows down and, according to ultrasound results, does not correspond to the term. In some cases, disruption of blood flow ends with spontaneous termination of gestation at an early stage.
At a later stage, generalized vasospasm can lead to abruption of a normally located placenta. In most cases, with such a development of events, the child cannot be saved.
High blood pressure can develop into full-fledged gestosis. At the same time, swelling of varying degrees of severity occurs, and protein appears in the urine. The disease can progress and lead to preeclampsia or eclampsia - the appearance of seizures and loss of consciousness, even to coma.
Changes in the placenta with this pathology form placental insufficiency, which is manifested by impaired supply of nutrients, fetal hypoxia, delayed fetal development and, in severe cases, death.
Diagnostics
It can sometimes be difficult to determine whether elevated blood pressure detected during pregnancy is due to chronic hypertension or gestational hypertension, especially if there are no recorded blood pressure values during the first half of pregnancy. Clinical characteristics obtained from history, physical examination, and some laboratory tests can be used to clarify the diagnosis. When assessing the mother, the well-being of the fetus must also be considered.
Preeclampsia rarely occurs before the third trimester, and a diagnosis of severe hypertension or preeclampsia in the first or early second trimester requires the exclusion of gestational trophoblastic disease and/or molar pregnancy. Mild swelling of the lower extremities is common in normal pregnancies, but rapidly increasing or independent swelling may indicate the development of preeclampsia. However, edema is no longer part of the diagnostic criteria for preeclampsia.
New attacks during pregnancy suggest preeclampsia-eclampsia, but primary neurological disorders should be excluded.
Belgium has introduced first trimester screening to identify women at risk of developing preeclampsia or gestational hypertension. The screening algorithm uses a combination of maternal variables, including mean arterial pressure, uterine artery pulsatility index, pregnancy-related plasma protein-A, and placental growth factor. The algorithm was particularly effective in predicting early preeclampsia.
What causes the pathology?
Chronic hypertension during pregnancy can be either a primary disease or secondary to the pathology of other organs. Then it is called symptomatic.
The following reasons lead to an increase in blood pressure during pregnancy:
- existing hypertension (90% of cases);
- kidney pathologies: glomerulonephritis, pyelonephritis, polycystic disease, kidney infarction, diabetic damage, nephrosclerosis;
- diseases of the endocrine system: acromegaly, hypothyroidism, pheochromocytoma, hypercortisolism, Itsenko-Cushing's disease, thyrotoxicosis;
- vascular pathologies: coarctation of the aorta, aortic valve insufficiency, arteriosclerosis, periarteritis nodosa;
- neurogenic and psychogenic causes: stress and nervous strain, hypothalamic syndrome;
- gestosis.
Hypertension carries risks of damage to the kidneys, heart and brain, and impaired fetal development. But it itself can be a consequence of pathology of internal organs.
Treatment
Treatment of arterial hypertension during pregnancy in the event of preeclampsia and eclampsia is discussed in detail in the relevant articles (follow the links).
Treatment of arterial hypertension during lactation
Approved drugs
The following antihypertensive drugs are approved for the treatment of hypertension during lactation:
It is also possible to take diuretics (hydrochlorothiazide, chlorthalidone, furosemide, torsemide) and the β-blocker prazosin, but there are indications that all of them, when used in high doses, can reduce the formation of breast milk. The issue of the safety of using nifedipine and verapamil during lactation continues to be discussed (a number of experts consider their use possible, especially during hypertensive crises, but manufacturing companies mention lactation as a contraindication).
Prohibited drugs
Breastfeeding women should not be advised to take:
- methyldopa,
- indapamide,
- amiloride,
- spironolactone,
- eplerenone,
- amlodipine,
- lercanidipine,
- all sartans.
How does hypertension manifest?
Physiologically, pressure during pregnancy naturally decreases during the first two trimesters, and only by the time of birth it returns to its normal state. But with existing hypertension, pressure can behave differently. In some cases, it decreases and stabilizes. But the condition may also worsen - increased blood pressure, swelling and proteinuria.
When visiting a doctor, women may complain of increased fatigue and headaches. Sometimes the following symptoms bother you:
- sleep disorders;
- rapid heartbeat, which is felt independently;
- dizziness;
- coldness of hands and feet;
- chest pain;
- dyspnea;
- blurred vision in the form of flickering spots before the eyes, blurred vision;
- noise or ringing in the ears;
- paresthesia in the form of a feeling of “crawling goosebumps”;
- unmotivated feeling of anxiety;
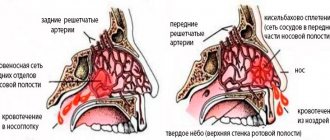
- nosebleeds;
- rarely – thirst, frequent night urination.
Initially, the pressure increases periodically, but gradually, with increasing severity, hypertension becomes permanent.
Preeclampsia and its classification
Most often, blood pressure begins to increase after 20 weeks of pregnancy. The earlier high blood pressure is first detected, the more malignant the disease becomes. Preeclampsia can occur either with isolated hypertension or with the addition of proteinuria (protein in the urine) and dropsy (edema). According to the classification, gestosis is:
- mild;
- moderate;
- severe.
The severity of gestosis is determined depending on pressure levels and protein levels in the urine. In our classification of gestosis, two most dangerous conditions are separately distinguished:
- Preeclampsia - convulsive readiness with high blood pressure and protein levels. A woman complains of a headache, dry mouth, flashing spots or darkening in the eyes.
- Eclampsia - loss of consciousness, convulsions and a high degree of death in the patient.
In the American classification, these concepts are included in the moderate and severe degrees of gestosis. Depending on the severity of gestosis and the duration of its course, pregnancy management tactics and the method of delivery are determined.
Risk groups for the development of gestosis
- Women with extragenital (not related to the genital organs) pathology. This includes pathology of the cardiovascular system, existing hypertension, kidney disease, obesity, and diabetes. In this case, gestosis is called combined.
- Women who have had gestosis in previous pregnancies.
- Pregnant women with pathological weight gain (more than 12 kg during pregnancy).
- Pregnant women under 18 years of age or over 35 years of age.
Causes of gestosis
Where and why such a severe complication of pregnancy occurs, no one knows for sure. Scientists around the world are trying to figure out the cause of gestosis and ways to treat or prevent it. The main theories include:
- Autoimmune response. The fetus is a half-foreign object for the mother, no matter how sad it may sound. The mother's body tries to get rid of the fetus by triggering immune defense mechanisms and producing antibodies to the kidneys, placenta and other organs of the fetus. These antibodies partially damage the mother's body.
- Genetic theory assumes that a woman has a special gene responsible for the development of gestosis. This theory may explain why mothers with preeclampsia give birth to daughters who later repeat this situation .
- The placental theory is the most common. When the embryo is implanted and the placenta develops at this site, special trophoblast cells migrate into the spiral arteries of the uterus and beyond. If this process is disrupted, the walls of the blood vessels are not rebuilt properly, and their inner lining is damaged during pregnancy. This triggers the process of vasospasm and the release of active substances - thromboxane, prostacyclin and others. These vasoactive substances further spasm and damage blood vessels. The vicious circle closes.
Treatment of gestational hypertension
In most cases, high blood pressure goes away on its own after termination of pregnancy in one way or another (artificial or spontaneous childbirth, cesarean section or late miscarriage).
Despite this, both pre-existing hypertension and newly emerging gestosis are subject to treatment during pregnancy.
The main groups of drugs for the treatment of gestosis:
- Antioxidant complex vitamins: A, E, C, as well as omega-three fatty acids.
- Magnesium preparations, both in the form of prophylactic administration, and magnesium sulfate (magnesium), used for emergency care.
- Herbal sedatives: valerian, motherwort, mint, as well as combined drugs such as Sedavit, Relaxil, Persen.
- Antispasmodics – no-shpa, papaverine, drotaverine.
- Central alpha agonists: methyldopa preparations - Dopegit, Dopanol. They are the drugs of choice for lowering blood pressure during pregnancy .
- Beta-blockers: metoprolol, atenolol. Appointed in case of ineffectiveness of previous groups.
- Calcium antagonists: nifedipine, nimodipine are prescribed to pregnant women as a last resort, in the absence of effect from methyldopa or beta-blockers. Most often used in emergency care for high blood pressure.
Here, in fact, are all the blood pressure medications approved for use in pregnant women. Prescribing other drugs is risky, since there has not been sufficient research on their safety for the fetus.
Drug treatment of gestosis must be combined with diet, fasting days, salt restriction, sleep and rest patterns.
Additional examination
It would be right to find out, even when planning a pregnancy, whether there are prerequisites for an increase in blood pressure. Those who come to the doctor after receiving a positive pregnancy test need to remember whether there were episodes of increased blood pressure before gestation or during a previous pregnancy. This data is necessary for the doctor to assign a risk group, to plan further management of pregnancy and carry out the necessary diagnostics, and determine methods of prevention.
Data is needed on the expectant mother's smoking habit, existing diabetes mellitus, overweight or diagnosed obesity, and blood lipid imbalance. What matters is the presence of cardiovascular diseases in young relatives and death from them at a young age.
Arterial hypertension is a therapeutic pathology, so the gynecologist conducts examination and treatment of such women together with a therapist.
Be sure to clarify the time of onset of complaints, whether they grew gradually or appeared suddenly, and correlate this with the duration of pregnancy. Particular attention is paid to the weight of the expectant mother. A body mass index of more than 27 significantly increases the risk of developing hypertension. Therefore, even before pregnancy, it is recommended to lose at least 10% of weight for those who exceed this figure.
The following tests may be used during the examination:
- Auscultation and palpation of the carotid arteries - allows you to identify their narrowing;
- examination and auscultation of the heart and lungs may reveal signs of left ventricular hypertrophy or cardiac decompensation;
- Palpation of the kidneys allows in some cases to identify cystic changes;
- Be sure to examine the thyroid gland for enlargement.
If there are neurological symptoms, then they check for stability in the Romberg position.
Clinical guidelines for hypertension in pregnant women include multiple blood pressure measurements when making a diagnosis. It needs to be done in several ways:
- on two hands, and compare the result obtained;
- in a lying position, and then standing;
- examine the pulse in the femoral arteries and the pressure in the lower extremities once.
If, when moving from a horizontal to a vertical position, diastolic pressure increases, then this speaks in favor of hypertension. A decrease in this indicator is symptomatic hypertension.
Diagnostics includes mandatory examination methods and additional ones, which are used in case of disease progression or treatment failure. The following methods are mandatory:
- clinical blood test (general indicators, hemoglobin);
- biochemical blood test: glucose, protein and its fractions, liver enzymes, basic electrolytes (potassium, calcium, chlorine, sodium);
- general urinalysis, the presence of glucose, red blood cells, as well as daily protein content;
- ECG.
All women have their blood pressure measured at every doctor's visit. On the eve of the visit, the pregnant woman must undergo a general urine test.
Additional methods are prescribed selectively depending on the clinical picture, as well as the suspected cause of increased pressure:
- urine tests according to Nechiporenko and Zimnitsky;
- Ultrasound of the kidneys;
- blood lipid profile;
- determination of aldosterone, renin, blood sodium and potassium ratio;
- urine test for 17-ketosteroids;
- blood for adrenocorticotropic hormone and 17-hydroxycorticosteroids;
- Ultrasound of the heart;
- consultation with an ophthalmologist and examination of the fundus vessels;
- 24-hour blood pressure monitoring;
- urine test for bacteria.
The condition of the fetus is monitored using ultrasound and Dopplerography of the vessels of the placenta and fetoplacental complex.
Treatment of deviation
Arterial hypertension in pregnant women requires prompt relief of symptoms and prevention of possible complications. Usually, medications (hypotensive drugs) are used as a last resort if the disease is at stage 3. Medicines prescribed by a specialist must be taken regularly to prevent sudden increases in blood pressure. In addition, treatment for the expectant mother includes:
- conversations with a psychologist;
- proper nutrition;
- yoga or fitness courses for pregnant women;
- regular walks in the fresh air;
- physiotherapeutic treatment;
- body weight control.
Only a doctor can prescribe treatment on an individual basis. Taking therapeutic measures on your own is dangerous.
The development of a clear symptom complex and complications can be prevented. Typically, pregnant women with arterial hypertension are advised to avoid stressful situations and also take one tablet of acetylsalicylic acid per day. The medication does not harm the health of either the expectant mother or the baby and supports the vascular system. In addition, vitamin complexes also have a good effect.
Principles of therapy
During pregnancy, treatment for hypertension is aimed at reducing the risk of complications for the mother and premature birth.
With a slight increase in blood pressure, treatment can be done on an outpatient basis, but always with periodic visits to the doctor. The absolute indication for hospitalization is a rise in blood pressure of more than 30 mmHg. Art. or the appearance of symptoms of involvement in the pathology of the central nervous system.
If the disease is detected for the first time, hospitalization is recommended to clarify the diagnosis and in-depth examination. This will also make it possible to determine how great the risk is of progression of the condition, its transition to gestosis or the occurrence of pregnancy complications. Pregnant women who are undergoing outpatient treatment are hospitalized, but without positive dynamics.
Recommendations for hypertension in pregnant women include three treatment options:
- Non-drug treatment.
- Drug therapy.
- Combating complications.
Non-drug treatment
The technique is used for all pregnant women diagnosed with hypertension. Arterial hypertension is primarily a psychosomatic disease, a long-term neurosis. Therefore, it is necessary to create conditions in which there will be the least amount of stressful situations.
What should those who are at home do? You need to evenly distribute your daily routine, leaving time for daytime rest, or better yet, short sleep. In the evening, going to bed should also be no later than 22:00. Reduce time spent at the computer and watching TV, eliminate programs that make you nervous. It is also necessary to distance yourself as much as possible from all life situations that can provoke nervous tension, or try to change your attitude towards them from a sharp emotional one to a neutral one.
Additionally, reasonable physical activity is required. This could be walking in the fresh air, swimming or special gymnastics for pregnant women.
Both in the hospital and at home, changes in the nature of nutrition are provided. It is recommended to eat frequent small meals 5 times a day, with the last meal no later than 3 hours before bedtime. Limit table salt intake to 4 g per day. It’s best to cook food without it, and add a little salt directly on your plate. For overweight women, the amount of fat and simple carbohydrates is limited. All pregnant women are recommended to increase the proportion of vegetables and fruits, grains, and fermented milk products in their diet.
For those undergoing outpatient or inpatient treatment, physiotherapeutic treatment may be prescribed:
- electrosleep;
- hyperbaric oxygen therapy;
- inductothermy on the feet and legs;
- diathermy of the kidney area.
Additionally, psychotherapeutic treatment and improvement of the general emotional state are necessary.
Treatment with medications
Tablets under certain conditions:
- pressure rises higher than 130/90-100 mm Hg. Art.;
- systolic pressure increased by more than 30 units from normal for a woman or diastolic pressure by more than 15 mm Hg. Art.;
- regardless of blood pressure indicators in the presence of signs of gestosis or pathology of the fetoplacental system.
Treatment of pregnant women is associated with the danger of drugs affecting the fetus, therefore drugs are selected in minimal dosages that can be used as monotherapy. Taking pills should be regular, regardless of the tonometer readings. Sometimes, having decided that the measurement results and general well-being are satisfactory, women voluntarily decide to stop taking medications. This threatens sudden jumps in blood pressure, which can lead to premature birth and fetal death.
Do not use or use as a last resort for health reasons:
- ACE blockers: Captopril, Lisinopril, Enalapril;
- angiotensin receptor antagonists: Valsartan, Losartan, Eprosartan;
- diuretics: Lasix, Hydrochlorothiazide, Indapamide, Mannitol, Spironolactone.
Preference is given to long-acting drugs. In case of ineffectiveness, combination therapy with several drugs may be used.
Drugs for the treatment of hypertension in pregnant women belong to several groups of antihypertensive drugs:
Atenolol is on the list of approved drugs, but it is used very rarely, because There is evidence that it causes fetal growth retardation. The choice of a specific drug depends on the severity of hypertension:
- 1-2 degrees - Methyldopa is considered the first-line drug, 2 lines - Labetolol, Pindolol, Oxprenolol, Nifedipine;
- Stage 3 – 1st line drug – Hydralazine or Labetolol are used intravenously, or Nifedipine is prescribed to be taken every 3 hours.
In some situations, the listed methods are ineffective, and there is a need to prescribe slow calcium channel blockers. This is possible if the benefits outweigh the risks of their use.
Additionally, treatment is aimed at correcting feto-placental insufficiency. They use agents that normalize vascular tone, improve metabolism and microcirculation in the placenta.
Treatment of complications
If gestational complications develop, treatment methods depend on the duration of pregnancy. In the first trimester, it is necessary to prevent the threat of its interruption. Therefore, sedative therapy, antispasmodics and progesterone treatment (Duphaston, Utrozhestan) are prescribed.
In the second and third trimester, correction of placental insufficiency is necessary. Therefore, drugs are prescribed that improve microcirculation, metabolism in the placenta (Pentoxifylline, Phlebodia), hepatoprotectors (Essentiale), antioxidants (vitamins A, E, C). Treatment is carried out against the background of antihypertensive therapy. If necessary, infusion therapy and detoxification are carried out.
Complications
Gestational hypertension requires consideration of several complications that affect different organ systems.
Life-threatening complications of preeclampsia
The overlap of preeclamptic disorders with hypertension during pregnancy can lead to severe complications for the mother:
- eclamptic seizures;
- intracerebral hemorrhage;
- pulmonary edema (due to capillary leakage, myocardial dysfunction, excessive intravenous fluid administration);
- acute renal failure (due to vasospasm, acute tubular necrosis [ATN], or renal cortical necrosis) with proteinuria greater than 4–5 g/day;
- HELLP syndrome (microangiopathic hemolysis, elevated liver enzymes and thrombocytopenia [platelets <100/µL]);
- liver swelling with or without dysfunction;
- liver infarction, rupture and subcapsular hematoma (which can lead to massive internal bleeding and shock);
- DIC syndrome.
Fetal complications include placental abruption, intrauterine growth restriction, preterm birth, and intrauterine fetal death.
Choosing your due date
Maintaining pregnancy directly depends on the effectiveness of the treatment. If blood pressure is well controlled, it is possible to extend gestation until the fetus reaches term. Childbirth is carried out under strict monitoring of the condition of the mother and fetus and against the background of antihypertensive therapy.
Premature birth is necessary in the following situations:
- treatment-resistant severe hypertension;
- worsening of the fetus;
- serious complications of hypertension: heart attack, stroke, retinal detachment;
- severe forms of gestosis: preeclampsia, eclampsia, HELLP syndrome;
- premature detachment of a normally located placenta.
Natural birth is preferred; amniotomy is performed at an early stage. Pain relief and careful blood pressure monitoring are mandatory. In the postpartum period, there is a high risk of bleeding, so the administration of uterotonics (Oxytocin) is necessary.
Prevention options
It is not always possible to avoid hypertension during pregnancy, but you can reduce the risk of its development. To do this, you need to plan your pregnancy. Overweight women are advised to adopt a healthy diet to gradually lose weight. But you can’t use strict diets or fasting. After them, in most cases, the extra pounds return.
If you have diseases of the kidneys, thyroid gland, heart, or diabetes, it is necessary to stabilize the condition and select adequate therapy that will minimize the possibility of worsening the condition during pregnancy.
Women who are diagnosed with hypertension while carrying a child are recommended to be hospitalized three times during pregnancy to clarify the condition and correct the therapy.
It is important to remember about non-drug methods that are used for any form of hypertension. With a slight increase in pressure and no complications, they are sufficient to stabilize the condition. In other cases, you must strictly follow the doctor's recommendations.