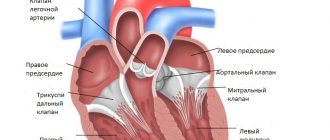
The valvular apparatus of the heart consists of four components, among which the mitral valve is of particular importance. Hemodynamics in the systemic circulation depend on the quality of its work. If mitral valve disease is determined, treatment is required, mainly surgically, which improves the quality and length of life of the patient.
The mitral valve (MK, mitral valve) is also known as the bicuspid valve or left atrioventricular valve. It is a heart valve with two leaflets, which is located between the left atrium and the left ventricle. The mitral valve along with the tricuspid valve are known as atrioventricular valves because they lie between the atria and ventricles of the heart.
Under normal conditions, blood flows through the open mitral valve during diastole with contraction of the left atrium. The MV closes during systole with contraction of the left ventricle.
The flow of blood through the systemic circulation, through which oxygen and nutrients flow to most of the organs and systems of the body, depends on the work of the MK. If there is any abnormality, blood may flow backward through the valve leaflets (mitral regurgitation) or the heart valve may be so narrowed (mitral stenosis) that it is difficult for blood to flow from the atrium to the ventricle. Rheumatic heart disease often affects the mitral valve; which may also prolapse with age or be affected by infective endocarditis.
Video: Mitral valve of the heart
What it is?
Left valve prolapse, or mitral valve prolapse, or bicuspid valve prolapse (BVP) is a disease accompanied by dysfunction of the valve located between the left atrium and the ventricle.
Normally, when the atrium contracts, the valve opens and blood flows into the ventricle. The valve then closes and the ventricle contracts, releasing blood into the aorta. With some pathology of connective tissue or changes in the heart muscle, a disturbance in the structure of the mitral valve occurs, which leads to “bending” of its valves into the cavity of the left atrium during contraction of the left ventricle, and part of the blood flows back into the atrium. The severity of this pathology is judged by the magnitude of the reverse flow.
It is believed that this disorder is most often observed in young people, but data from the Framingham study showed that there is no significant difference in the incidence of this disease depending on gender and in different age groups. In the case of a small return of blood (regurgitation), it is not clinically felt and does not require treatment. In rare cases, the amount of reverse blood flow is large and correction of the defect is required, including surgical intervention.
Anatomy
The heart can be imagined as a kind of pump that forces blood to circulate through the vessels of the whole body. This movement of fluid becomes possible by maintaining the pressure in the cavity of the heart and the work of the muscular apparatus of the organ at the proper level. The human heart consists of four cavities called chambers (two ventricles and two atria). The chambers are limited from each other by special “doors”, or valves, each of which consists of two or three doors. Thanks to this anatomical structure of the main motor of the human body, every cell of the human body is supplied with oxygen and nutrients.
There are four valves in the heart:
- Mitral. It separates the cavity of the left atrium and the ventricle and consists of two valves - anterior and posterior. Prolapse of the anterior valve leaflet is much more common than the posterior one. Special threads called chords are attached to each of the valves. They provide contact between the valve and muscle fibers, which are called papillary or papillary muscles. For the full functioning of this anatomical formation, the joint coordinated work of all components is necessary. During cardiac contraction - systole - the cavity of the muscular cardiac ventricle decreases, and accordingly the pressure in it increases. In this case, the papillary muscles are activated, which close the exit of blood back into the left atrium, from where it flows out of the pulmonary circulation, enriched with oxygen, and, accordingly, the blood enters the aorta and then, through arterial vessels, is delivered to all organs and tissues.
- Tricuspid (three-leaf) valve. It consists of three doors. Located between the right atrium and ventricle.
- Aortic valve. As described above, it is located between the left ventricle and the aorta and does not allow blood to return to the left ventricle. During systole, it opens, releasing arterial blood into the aorta under high pressure, and during diastole, it is closed, preventing blood from flowing back to the heart.
- Pulmonary valve. It is located between the right ventricle and the pulmonary artery. Similar to the aortic valve, it prevents blood from returning to the heart (right ventricle) during diastole.
Normally, the work of the heart can be represented as follows. In the lungs, the blood is enriched with oxygen and enters the heart, or rather its left atrium (it has thin muscle walls and is only a “reservoir”). From the left atrium it pours into the left ventricle (represented by a “powerful muscle” capable of pushing out the entire incoming volume of blood), from where during systole it spreads through the aorta to all organs of the systemic circulation (liver, brain, limbs and others). Having transferred oxygen to the cells, the blood takes up carbon dioxide and returns to the heart, this time to the right atrium. From its cavity, fluid enters the right ventricle and, during systole, is expelled into the pulmonary artery and then into the lungs (pulmonary circulation). The cycle repeats.
What is prolapse and why is it dangerous? This is a state of inadequate functioning of the valve apparatus, in which, during muscle contraction, the blood outflow pathways are not completely closed, and, therefore, part of the blood returns back to the heart during systole. So, with mitral valve prolapse, the fluid during systole partially enters the aorta, and partially from the ventricle is pushed back into the atrium. This return of blood is called regurgitation. Usually, with pathology of the mitral valve, the changes are insignificant, so this condition is often considered as a normal variant.
Antiphase is an ultrasound of the heart, what does it mean?
Hello. Please help me figure it out. My son is 17 years old. The doctor heard a murmur in his heart and sent him for an ultrasound. We got the following results. EchoCG. Conclusion. Bicuspid aortic valve. The valve flaps are sealed.
Cardiac cavities: dimensions within the age norm. Contractility is preserved. Mitral valve prolapse, art. 1, with slight regurgitation. Regurgitation on the tricuspid valve, stage 1.
How serious is this? What do we have to do? Thank you.
Good afternoon. Please comment on the child's echocardiography. Aorta 0.1 cm. Opening amplitude 8 mm. Left atrium - 14mm. The mitral valve is normal. There is an antiphase. There is no prolapse. Interventricular septum: diastole – 4 mm, systole – 3 mm. Posterior wall of the left ventricle: diastole – 3 mm, systole 4 mm. Overall contractility: EF 67%. UO 18ml. FU 38%.
Right ventricle - 8mm. Pulmonary artery 10mm. Interatrial septum: defect with a diameter of 8 mm with left-right shunting. The interventricular septum is normal. There is no free fluid in the pericardial cavity. An additional chord is visualized in the cavity of the left ventricle. Conclusion: congenital heart defect: ASD. Dilatation of the pancreas. Moderate valvular stenosis of the pulmonary artery.
Hello. Please look at the results of the heart ultrasound. Aorta: the lumen of the aortic root is 40 mm, the walls are thickened and dense. The aortic valve leaflets are thickened, dense, calcified (++). In systole, the divergence of the leaflets is 18 mm. The anteroposterior size of the left atrium is 40 mm. Right atrium 31x45. EDD of the right ventricle 35 mm. EF 63%. ESD of the left ventricle 50. ESD of the left ventricle 32.
MZhP 10 mm. The movement of the IVS is without any peculiarities. ZSLZh 10 mm. The movement of the LV is without any peculiarities. Mitral valve: the movement of the leaflets in diastole is multidirectional. The mitral valve leaflets are compacted, changed, calcified (+). Peak E = peak A. The movement of the mitral valve is M-shaped.
The blood flow velocity at the aorta is 110, at the level of the MV - 80, the tricuspid valve - 50, and the pulmonary artery -100. The cavities of the heart are not dilated. Regurgitation: aortic 1-2 degrees, mitral 1-2 degrees. Calcification of the aortic valve - grade 2, mitral valve - grade 1. Diastolic function is impaired. No violations of local and global contractility were detected. I am 69 years old.
I have atherosclerosis of the cervical arteries; with prolonged physical activity, pain appears in the heart area. What is this connected with?
Good afternoon. Please explain the results of the heart ultrasound. Left atrium 31 mm. The aorta at the level of the sinuses of Valsalva is 41 mm, the ascending aorta is 39 mm. The divergence of the aortic valve leaflets is 17 mm. Right ventricle 33 mm. The outflow tract of the right ventricle is 27 mm.
The movement of the mitral valve leaflets is multidirectional. MZhP 8mm. The amplitude of the IVS is 3 mm. Posterior wall of the left ventricle 11mm; the amplitude of the left ventricle is 5 mm. ESD 65mm ESD 48mm EDV 225 ml ESD 112 ml Ejection fraction 50% Dopplerography Regurgitation on the LA 2nd stage. at a speed of 1.1 m/sec. Gradient - 4.6 mm Hg. Art.
Left ventricular diastolic dysfunction. Conclusion: the left and right parts of the heart are enlarged. The aorta and valves are sealed. PA valve insufficiency, stage 1. Hypokinesia of the LV walls. Myocardial contractility is reduced. Type 1 LV diastolic dysfunction.
I have diabetes and sometimes have tachycardia. How is your heart condition?
Hello. Irina, 55 years old. For several months I have been worried about severe shortness of breath, and with minimal exercise I feel very bad. I did an ultrasound of the heart and got the following result: Irregular rhythm 78 beats/min. Congenital heart defect. ASD 7-8 mm with blood discharge from left to right with signs of hemodynamic overload of the right heart.
Dilation of the right heart. Pulmonary hypertension stage 1. Aortic insufficiency of the 1st degree. Consolidation of the aorta and aortic valve. Tricuspid regurgitation grade 2-3. Compaction of the mitral ring. Mitral regurgitation grade 2-3.
Do these changes require surgical treatment? Is surgery performed at this age? Thank you.
Hello. Please decipher the results of the ultrasound of the heart. Left atrium - 37 mm, right atrium - 48 mm, right ventricle - 28 mm, anterior wall of the right ventricle - 5 mm. Aorta: the diameter of the aorta at the level of the leaflets is 27 mm, the leaflets of the aortic valve are somewhat compacted, the divergence of the leaflets is 18 mm, Pg max is 9 mm, V max is 1.
5 m/sec, 1st degree regurgitation, T1/2 regurgitation flow - 51 ms. Mitral valve: leaflets are sealed, peak A: Vmax - 0.5 m/sec, peak E: Vmax - 1.1 m/sec, Pg max - 5 mm. RT, regurgitation - 1-2 degrees, mitral orifice area - 4.8 cm2, T 1/2 pressure gradient - 42 ms, E/a - 2.2, IVRT - 62 ms, DT - 132 ms.
Left ventricle: ESD - 65 mm, EDV - 207 ml, ESR - 51 mm, ESV - 115 ml, stroke volume - 94 ml, heart rate - 94, ejection fraction - 45%, shortening index - 22%, local contractility - not impaired . MZhP: MZhP syst. — 11 mm, IVS dia. — 10 mm, syst. excursion of the IVS - 2 mm, TZSLZh diast. — 12 mm, TZSLZh syst.
- 14 mm, systolic excursion of the posterior wall of the LV - 4 mm. Tricuspid valve: leaflets – no changes, regurgitation – 1st degree, Pg max – 2.2 mm. Pulmonary valve: leaflets - without features, pulmonary trunk - 24 mm - at the upper limit of normal, Vmax - 0.98 m/sec, Pg max - 3.
6 mm, 1st degree regurgitation, collapse of the IVC on inspiration - less than 50%, signs of pulmonary hypertension, systolic pressure in the PA - 30 mm Hg. Art.
Good afternoon. Please look at the ultrasound of the heart. Are the results normal? There is no dilatation of the heart cavities. EDR of the left ventricle is 3.5 cm, anterior-posterior size of the left atrium is 2.3 cm. There is no myocardial hypertrophy. TZSLZH - 0.7 cm. The aorta is not dilated and is mobile.
Pulmonary artery: no changes. Valvular apparatus: slight prolapse of the anterior valvular leaflet into the cavity of the left atrium in systole up to 0.2 cm - within the physiological norm. Left ventricular ejection fraction 65%. There is no myocardial asynergia.
Doppler analysis: without features.
Hello. Anastasia, 48 years old. Please evaluate the results of EchoCG. Over the last month my blood pressure has started to rise. Could this be related to changes on EchoCG? What treatment is required? How dangerous? Thank you. Results of Doppler echocardiography Left atrium: 32 mm.
Left ventricle: EDR 51 mm, ESR 27 mm Ejection fraction: 75% Mitral valve: leaflets are sealed, posterior leaflet is sclerotic. Calcinosis 0-1. Physiological regurgitation. Aorta The aortic valve leaflets are sealed. There is no regurgitation. Calcinosis 0-1. Aorta at the level of the sinuses of Valsalva: 32. Right ventricle: normal.
Right atrium: normal. Pulmonary valve: valve leaflets are sealed. Regurgitation is minimal. Tricuspid valve: minimal regurgitation. IVS thickness (diastole): 9.6 LVSD thickness (diastole): 9.6 CONCLUSION: Sclerotic changes in the walls of the mitral and aortic valves.
Calcification of the mitral valve, aortic valve 0-1. Violation of diastolic function of the left ventricle by Doppler method.
Hello. Dmitry, 41 years old. Please explain the results of the heart ultrasound. How dangerous is the mitral valve condition? Thank you. Left ventricle: contractility is preserved, the cavity is not expanded.
CSR 31 mm SV 72 ml CDR 48 mm EF 65% CSR 41 mm EDV 108 IVS 11, bases up to 14 mm ZSLZH 10 mm Mitral valve: valve leaflets are sealed, movement is multidirectional. Mitral area. holes saved.
Transmitral flow is changed peak E Question asked April 19, 2012 Ultrasound of the heart
Source: https://ogomeopatii.ru/protivofaza-est-uzi-serdca-chto-oznachaet/
Classification
Mitral valve prolapse can be:
- Primary. Associated with connective tissue weakness, which occurs with congenital connective tissue diseases and is often transmitted genetically. With this form of pathology, the mitral valve leaflets are stretched, and the retaining leaflets of the chord are lengthened. As a result of these violations, when the valve closes, the flaps protrude and cannot close tightly. Congenital prolapse in most cases does not affect the functioning of the heart, but is often combined with vegetative-vascular dystonia - the cause of symptoms that patients associate with heart pathology (periodically occurring functional pain in the chest, cardiac arrhythmias).
- Secondary (acquired). Develops in various heart diseases that cause disruption of the structure of the valve leaflets or chords. In many cases, prolapse is provoked by rheumatic heart disease (an inflammatory disease of the connective tissue of an infectious-allergic nature), undifferentiated connective tissue dysplasia, Ehlers-Danlos and Marfan diseases (genetic diseases), etc. In the secondary form of mitral valve prolapse, pain that passes after taking nitroglycerin is observed, interruptions in heart function, shortness of breath after exercise and other symptoms. If the cardiac chords rupture as a result of a chest injury, emergency medical attention is required (the rupture is accompanied by a cough, during which foamy pink sputum is released).
Primary prolapse, depending on the presence/absence of noise during auscultation, is divided into:
- The “silent” form, in which symptoms are absent or scanty, and noises and “clicks” typical for prolapse are not heard. Detected only by echocardiography.
- Auscultatory form, which, when auscultated, is manifested by characteristic auscultatory and phonocardiographic “clicks” and noises.
Depending on the severity of the sagging of the valves, mitral valve prolapse is distinguished:
- I degree - the doors bend by 3-6 mm;
- II degree - there is a deflection of up to 9 mm;
- III degree - the sashes bend by more than 9 mm.
The presence of regurgitation and the degree of its severity are taken into account separately:
- I degree – regurgitation is mild;
- II degree – moderately severe regurgitation is observed;
- III degree - there is pronounced regurgitation;
- IV degree – regurgitation is severe.
Valvular structure of the heart
The human heart consists of several sections, which are separated by special partitions - valves. Everyone knows that the task of the heart is to transport blood to all tissues and organs, as well as enrich it with oxygen and nutrients. By contracting in jerks, this most important organ causes the blood to move. In this case, it first enters some sections, “chambers,” of the heart, and then flows from there into the central bloodstream.
Valve structure
Valves play the role of peculiar partitions that allow blood to pass in one direction, but prevent it from returning back. Several such “septa” take part in the work of the heart - the aortic, tricuspid, mitral and separately the pulmonary valve. The mitral valve of the heart is a very important part of this system. A failure in the performance of its functions immediately affects the functioning of the entire body.
Reasons for development
Mitral valve prolapse is not an independent disease. It is a syndrome that occurs in numerous diseases. Depending on the etiology, secondary MVP is distinguished - it occurs as a result of other pathologies, and primary - it is also congenital or idiopathic.
Quite often, idiopathic MVP is detected in children and adolescents. It appears due to congenital connective tissue dysplasia. As a result of this disease, other disorders in the structure of the valve apparatus may develop, for example:
- lengthening or shortening of the cardiac chords;
- improper attachment of the chords to the valve flaps;
- presence of additional chords;
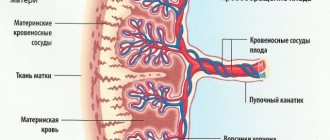
As a result of structural changes in the connective tissue, degenerative processes occur in the valve leaflets, and they become more pliable. Because of this, the valve cannot withstand the pressure created by the left ventricle and bends towards the left atrium. Connective tissue dysplasia can occur for various reasons that affect the child in the womb, among them the following:
- Acute respiratory viral infections during pregnancy.
- The presence of occupational hazards in a woman.
- Preeclampsia.
- The influence of environmental factors on the mother during pregnancy.
- Excessive stress on the body of a pregnant woman.
In approximately 20% of cases, congenital MVP is transmitted through the maternal line. In addition, mitral valve prolapse occurs in other hereditary diseases, such as:
- Morphan's syndrome.
- Arachnodactyly.
- Elastic pseudoxanthoma.
- Osteogenesis imperfecta.
- Ehlers-Danlos syndrome.
Secondary MVP (or acquired) can occur as a result of certain diseases. The most common causes of this pathological condition are:
- Cardiac ischemia.
- Rheumatism.
- Hyperthyroidism.
- Chest injuries.
- Hypertrophic cardiomyopathy.
- Systemic lupus erythematosus.
- Myocardial dystrophy.
- Myocarditis.
Prolapse in this case occurs due to damage to the valve leaflets, papillary muscles, chordae or disturbances in the function and structure of the myocardium. Also, an important role in the mechanism of development of MVP is played by disturbances in the functioning of the autonomic nervous system, deficiency of micro- and macroelements (especially Magnesium) and metabolic pathology.
Another cause of secondary prolapse is aortic valve stenosis. As a result of this acquired defect, the opening of the aortic valve narrows, and blood cannot fully pass through it. This creates excess pressure in the left ventricle, which in turn presses on the bicuspid valve. If there is a fact of prolonged existence of excess pressure, then the mitral valve leaflets begin to bend towards the left atrium, and prolapse occurs.
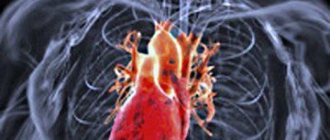
Basic pathologies and methods of their diagnosis
The main causes of acquired MV defects: rheumatic and atherosclerotic lesions, age-related and degenerative changes, consequences of infective inflammatory endocarditis against the background of sepsis. These diseases lead to narrowing and disruption of the functioning of the atrioventricular opening, the development of insufficiency or stenosis. Complex combined defects often appear as a consequence of severe rheumatic disease.
Common mitral valve diseases
MV prolapse – (protrusion or sagging) of the valves into the atrium cavity during systolic contraction. The defect is more common in newborns, with peak detection occurring between the ages of 5-15 years.
It can be primary (of unknown origin) or secondary - the result of an inflammatory process or injury to the sternum, more often in athletes. Connective tissue dysplasia indicates an inherited genetic disease.
The violation is characterized by:
- Regurgitation of the bicuspid mitral valve disrupts blood flow, which is manifested by the development of pulmonary hypertension (increased pressure in the vessels of the lungs) and decreased levels in the peripheral arteries.
- Clinical symptoms depend on the degree of prolapse and the cause of the defect.
- In the initial stages, the condition may worsen minimally, most often when playing sports.
- The progression of regurgitation is indicated by increasing weakness and dizziness, headaches, and loss of consciousness. Shortness of breath, difficulty breathing at the slightest exertion, and a feeling of lack of air are often troubling.
- There is a high risk of developing arrhythmia and cardiac arrest.
Symptoms of mitral valve prolapse
The severity of symptoms of mitral valve prolapse varies from minimal to significant and is determined by the degree of connective tissue dysplasia, the presence of regurgitation, and autonomic abnormalities. Some patients do not have any complaints, and mitral valve prolapse is an incidental finding on echocardiography.
In children with primary mitral valve prolapse, umbilical and inguinal hernias, hip dysplasia, joint hypermobility, scoliosis, flat feet, chest deformity, myopia, strabismus, nephroptosis, varicocele are often detected, indicating a disorder in the development of connective tissue structures. Many children are predisposed to frequent colds, sore throats, and exacerbations of chronic tonsillitis.
Quite often, mitral valve prolapse is accompanied by symptoms of neurocirculatory dystonia: cardialgia, tachycardia and interruptions in heart function, dizziness and fainting, vegetative crises, excessive sweating, nausea, a feeling of a “lump in the throat” and lack of air, migraine-like headaches. With significant hemodynamic disturbances, shortness of breath and increased fatigue occur. The course of mitral valve prolapse is characterized by affective disorders: depressive states, senestopathies, asthenic symptom complex (asthenia).
Clinical manifestations of secondary mitral valve prolapse are combined with symptoms of the underlying disease (rheumatic carditis, congenital heart defects, Marfan syndrome, etc.). Possible complications of mitral valve prolapse include life-threatening arrhythmias, infective endocarditis, thromboembolic syndrome (including stroke, pulmonary embolism), and sudden death.
Prolapse in childhood
In childhood, MV prolapse occurs much more often than in adults. This is evidenced by statistical data based on the results of ongoing research. It is noted that in adolescence, MVP is diagnosed twice as often in girls. Children's complaints are of the same type. Basically, this is an acute lack of air, heaviness in the heart and chest pain.
The most common diagnosis is grade 1 anterior leaflet prolapse. It was detected in 86% of examined children. Stage 2 disease occurs in only 11.5%. MVP III and IV with degree regurgitation are very rare, occurring in no more than 1 child out of 100.
Symptoms of MVP manifest themselves differently in children. Some people practically do not feel abnormal heart function. In others it manifests itself quite strongly.
- Thus, chest pain is experienced by almost 30% of adolescent children who have been diagnosed with MVC (mitral valve prolapse). It is caused by various reasons, among which the most common are the following:
- chords that are too tight;
- emotional stress or physical stress leading to tachycardia;
- oxygen starvation.
- The same number of children experience heart palpitations.
- Often teenagers who spend a lot of time at the computer, preferring mental activity to physical activity, are prone to fatigue. They often experience shortness of breath during physical education classes or when doing physical work.
- Children diagnosed with MVP often exhibit neuropsychological symptoms. They are prone to frequent mood swings, aggressiveness, and nervous breakdowns. Under emotional stress, they may experience short-term fainting.
During the examination of the patient, the cardiologist uses various diagnostic tests, through which the most accurate picture of MVP is revealed. The diagnosis is established when noises are detected during auscultation: holosystolic, isolated late systolic or in combination with clicks, isolated clicks (clicks).
Heart valve prolapse in childhood often develops due to a lack of magnesium ions. Magnesium deficiency disrupts the process of collagen production by fibroblasts. Along with a decrease in magnesium content in the blood and tissues, there is an increase in beta-endorphin and an imbalance in electrolyte balance. It has been noted that children diagnosed with MVP are underweight (inappropriate for height). Many of them have myopathy, flat feet, scoliosis, poor development of muscle tissue, and poor appetite.
It is recommended to treat MVP with a high degree of regurgitation in children and adolescents, taking into account their age group, gender and heredity. Based on the severity of the clinical manifestations of the disease, a treatment method is selected and medications are prescribed.
But the main emphasis is on changing the child’s living conditions. Their mental load needs to be adjusted. It must alternate with physical exercise. Children should visit a physical therapy room, where a qualified specialist will select the optimal set of exercises, taking into account the individual characteristics of the course of the disease. Swimming lessons are recommended.
With metabolic changes in the heart muscle
Why is mitral valve prolapse dangerous?
Are complications possible and what are the dangers of mitral valve prolapse? Despite the fact that in most cases there is mitral valve prolapse with minor regurgitation, which does not require special therapy, there is still a risk of complications. Complications are quite rare (only 2-4%) and include the following life-threatening conditions that require treatment in a specialized hospital:
- Acute mitral regurgitation is a condition that usually occurs as a result of rupture of the chordae tendineae due to chest injuries. It is characterized by the formation of a “dangling” valve, that is, the valve is not held by the chords, and its valves are in free movement, not performing their functions. Clinically, a picture of pulmonary edema appears - severe shortness of breath at rest, especially in the lying position; forced sitting position (orthopnea), bubbling breathing; congestive wheezing in the lungs.
- Bacterial endocarditis is a disease in which microorganisms that have broken into the blood from a source of infection in the human body settle on the inner wall of the heart. Most often, endocarditis with damage to the heart valves develops after a sore throat in children, and the presence of initially altered valves can serve as an additional factor in the development of this disease. Two to three weeks after the infection, the patient develops repeated fever, chills, there may be a rash, an enlarged spleen, cyanosis (blue coloration of the skin). This is a serious disease that leads to the development of heart defects, gross deformation of the heart valves with dysfunction of the cardiovascular system. Prevention of bacterial endocarditis is timely sanitation of acute and chronic foci of infection (carious teeth, diseases of the ENT organs - adenoids, chronic inflammation of the tonsils), as well as prophylactic use of antibiotics during procedures such as tooth extraction, removal of tonsils.
- Sudden cardiac death is a serious complication, apparently characterized by the occurrence of idiopathic (sudden, causeless) ventricular fibrillation, which is a fatal arrhythmia.
Despite the fact that mitral valve prolapse rarely has a malignant course and causes severe complications, this disease still requires constant medical supervision and monitoring. Do not neglect your doctor’s recommendations and undergo regular check-ups with a cardiologist. Such measures will help you prevent the progression of this disease, and you will maintain your health and ability to work.
Diagnostics
Detection of MVP often occurs accidentally, and at any age, which, as already noted earlier, is accompanied by a cardiac ultrasound procedure. This method is the most effective in diagnosing mitral valve prolapse, because its use determines the possibility of identifying a specific degree of prolapse in combination with the amount of regurgitation accompanying the pathology.
- Mitral valve prolapse of the 1st degree determines the relevance for the patient of the variant of its manifestation in such a variant in which the bulging of the valves is insignificant (within 5 millimeters).
- Mitral valve prolapse of the 2nd degree determines the relevance of the bulging of the leaflets within no more than 9 millimeters.
- Mitral valve prolapse of the 3rd degree indicates protrusion of the leaflets of 10 millimeters or more.
It should be noted that in this version of dividing pathology into degrees, the degree of regurgitation is not taken into account, due to which now these degrees are not the basis for the subsequent determination of the prognosis for the patient and, accordingly, for the prescription of treatment. Thus, the degree of mitral valve insufficiency is determined on the basis of regurgitation, which is displayed to the greatest extent during ultrasound.
As additional diagnostic measures to determine the characteristics of the heart, an ECG procedure, as well as a Holter ECG, can be prescribed. Thanks to the ECG, it is possible to study changes relevant to the functioning of the heart based on the impact caused by mitral valve prolapse, while the Holter ECG allows recording of data relevant to the functioning of the heart within a period of 24 hours. Mostly, the congenital form of prolapse does not interfere with the functioning of the heart; accordingly, there is no special need for additional diagnostic measures due to the practical absence of detection of certain abnormalities in them.
Diagnostic methods
To identify mitral regurgitation, pay attention to the medical examination data:
- cardiac hump (due to expansion and thickening of the wall of the left ventricle);
- the apical impulse is strengthened in the 5th intercostal space;
- pulsation is determined at the rib angle;
- the boundaries of the heart are expanded;
- the first sound at the apex is weak or absent, systolic murmur;
- the second tone is accentuated on the pulmonary artery, split.
Instrumental diagnostic data helps detect the following deviations:
- FCG – confirms changes in tones and the presence of noise;
- ECG - hypertrophy of the left and then the right ventricle;
- X-ray – enlarged left arches, triangular heart, congestion in the lungs;
- Ultrasound with Doppler sonography is the main method for determining the degree of regurgitation and mitral regurgitation.
If after this set of studies it is not possible to confirm the diagnosis or it is necessary to choose the optimal type of surgical treatment, then probing of the cavities and contrast ventriculography may be prescribed.
How to treat mitral valve prolapse?
Treatment of acquired MVP in most cases is carried out in a cardiology hospital. The patient is recommended to adhere to bed or semi-bed rest, give up bad habits and follow a diet.
For rheumatic, i.e. infectious cause of the development of this heart defect, the patient is prescribed a course of antibacterial therapy to eliminate rheumatic carditis. For this purpose, antibiotics from the penicillin group are used (Billin, Vancomycin, etc.). If significant blood regurgitation and arrhythmia are detected in a patient, other medications may be prescribed, the action of which will be aimed at eliminating symptoms (diuretics, antiarrhythmics, hypotensives, etc.). The complex of therapy and dosage of drugs in such cases can only be selected individually. In the same way, the question of the possible need for surgical treatment is resolved.
To treat MVP, which was caused by cardiac pathologies, medications used to treat the underlying disease are used. This therapy is aimed at normalizing blood circulation and eliminating arterial hypertension and arrhythmias, and if drug treatment is ineffective, the patient may be recommended surgical intervention aimed at eliminating the mitral valve defect.
Particular attention is paid to cases of MVP that were caused by chest trauma. After correcting the condition with medication, patients undergo surgery to stabilize the mitral valve. Such patients require hospitalization and careful monitoring. If a cough with pink sputum appears, medical attention should be provided immediately, because any delay can lead to death.
Symptoms of pathology
Mild regurgitation is not clinically apparent because the left ventricular myocardium has sufficient strength to compensate for the slight increase in volume. With a decrease in the contractility of the left half of the heart, the stage of subcompensation begins. During this period, patients begin to complain of:
- labored breathing;
- fatigue;
- rapid pulse and heartbeat;
- pain in the heart area;
- persistent cough with bloody sputum.
After the addition of circulatory failure in the systemic circle, attacks of suffocation, swelling of the legs appear, the liver enlarges, the veins of the neck become overfilled, and fluid accumulates in the abdominal and pleural cavity. When the recurrent nerve is compressed by an enlarged atrium or trunk of the pulmonary artery, the voice becomes hoarse or disappears. Almost half of patients experience atrial fibrillation.
Forecast for life
The prognosis for life is favorable. Complications rarely develop, and the patient’s quality of life does not suffer. However, the patient is contraindicated from engaging in certain sports (jumping, karate), as well as professions that overload the cardiovascular system (divers, pilots).
Regarding military service, we can say that, according to orders, suitability for military service is decided individually for each patient by a military medical commission. So, if a young man has mitral valve prolapse without regurgitation or with regurgitation of the 1st degree, then the patient is fit for service. If there is regurgitation of the 2nd degree, then the patient is conditionally fit (in peacetime he will not be called up). If there is grade 3 regurgitation, arrhythmias or heart failure of functional class 11 or higher, military service is contraindicated.
Thus, most often a patient with mitral valve prolapse with a favorable course and in the absence of complications can serve in the army.
The main causes of shortness of breath Rheumatism of the joints Endocarditis Pericarditis Cardiac arrhythmia Cardiac myocarditis
Learning to speak correctly
Diagnosis name
There are times when we, having misheard or misread medical terms, remember them with errors. The end result is that humans develop diseases, just like animals. Although the culprit may be the harmless attribution of an extra ending. Do not confuse the concept of mitral valve endocardiosis. Mitral valve endocardiosis occurs in dogs and has nothing to do with the human body.
Sometimes, not knowing medical terms, the patient can get a little confused. Therefore, one of the causes of damage to the valve apparatus is not endocarditis of the mitral valve, but endocarditis. I would also like to draw attention to such a concept as mitral valve prolapse. Prolapse cannot be collapse. These terms should not be confused. Prolapse is a condition of the mitral valve when its leaflets, for various reasons, bend into the cavity of the right atrium.
Collapse means “fallen” in Latin. This term is found in medicine when it comes to vascular insufficiency - vascular collapse, collaptoid state. When we talk about collapsed lung, this means a condition where this organ is in a collapsed state due to the accumulation of air or gas between the membranes that enclose the lung.