Coronary artery revascularization
Today, revascularization of the coronary arteries has become a common procedure for cardiac surgeons in specialized centers, and patients are receiving more and more information about these treatment methods. Myocardial revascularization methods significantly reduce mortality from cardiovascular diseases and allow patients to return to their previous, full life without heart pain and restrictions.
Therapists, cardiologists, and angiosurgeons have complete information about these methods of treating cardiovascular pathology, but not all patients understand what the term “coronary revascularization” entails. Many patients who are indicated for the use of one or another method of this surgical intervention refuse it, fearing unreasonable complications. Most often, such fears arise due to an incomplete understanding of the essence of the manipulation, which, due to lack of time or for other reasons, doctors do not always clearly explain.
Indeed, it is quite difficult to explain the progress of a surgical intervention to a person who is not medically savvy, but we will try to “chew” and “sort out” all the information regarding myocardial revascularization. Namely, we will touch on the definition of terminology, indications and methods of manipulation, and also consider promising, developing methods of revascularization of the coronary arteries.
We encrypt the terms
Coronary arteries of the heart
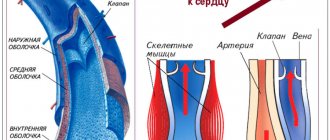
The human heart is supplied with blood by arteries called coronary arteries. It is thanks to them that the myocardium receives a sufficient amount of nutrients and oxygen. But for various reasons, coronary arteries can become narrowed, blocked, or collapsed. The most common cause of narrowing is an atherosclerotic plaque. In this case, the myocardium experiences a lack of the oxygen it needs, and oxygen cardiac “Hunger” develops - ischemia.
All medical methods of treating this condition are aimed at eliminating oxygen “hunger” of the heart or ischemia, restoring the lumen of the artery and, as a result, normalizing blood circulation, metabolism and oxygen saturation. This is done using medications, and if there is no effect from them, or for certain indications, surgical intervention. Myocardial revascularization is the restoration of blood supply to the heart muscle, which suffers from oxygen deficiency, through surgery.
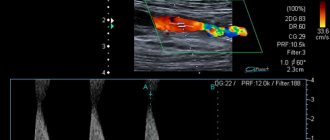
Impaired blood flow in the coronary arteries
If we analyze the Latin term “revascularization” by its composition, its meaning inherent in the word itself becomes clear. The prefix “re-” means repetition, the resumption of a previously performed action, “vas” means vessel in Latin. During revascularization, blood flow in the coronary arteries is restored; this is done by the doctor surgically, either by acting on the lumen of the artery itself, or by acting in “bypass” ways (as if turning off the affected area of the vessel from the blood flow, by applying bypass anastomoses from other vessels).
The choice of surgical technique depends on the specific pathology for the individual patient. Some are indicated for coronary stenting, and for others, transmyocardial laser revascularization of the myocardium. These are just a few methods related to our topic. And the most well-known among patients, one of the most frequently performed methods of myocardial revascularization with excellent long-term results and an excellent postoperative prognosis, is coronary artery bypass grafting.
Shock wave therapy
This surgical method is also experimental. The so-called “acoustic wave” directed at the heart stimulates the growth of new arteries and capillaries in the myocardium in a poorly supplied area of the myocardium.
Shock wave therapy is absolutely painless and bloodless. Currently, this technique is practically not used. This is due to the lack of specific information about treatment results and patient reviews.
Coronary myocardial revascularization eliminates only the consequences of the disease, but not its cause. If you neglect proper nutrition and continue to eat fatty and sweet foods, new complications of atherosclerosis will develop, even more severe and life-threatening.
Coronary artery bypass grafting
Direct revascularization (Coronary artery bypass grafting)
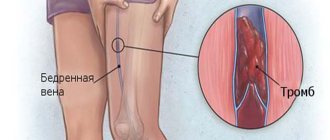
This method is a type of direct revascularization, since coronary artery bypass grafting creates an anastomosis or connection between the aorta and the coronary artery below the site of its narrowing. The graft is the saphenous femoral vein. The doctor will recommend CABG to those patients who have angina pectoris of at least class III, IV, which is not amenable to conservative treatment, limits the patient’s motor activity and significantly impairs his quality of life.
Coronary vessels with stenosis of more than 50%, as well as narrowing of more than 1 mm, are also subject to surgery. But the final decision to undergo coronary artery bypass grafting or not for a particular patient is made by the vascular surgeon only after conducting the “gold standard” of coronary artery disease - coronary angiography. If this diagnostic study reveals a pronounced narrowing of the main trunk of the coronary artery, an occlusive lesion, or a significant narrowing of 2-3 large arteries supplying blood to the heart muscle, there will be surgery.
Heart failure
Contraindications: congestive heart failure, a pronounced decrease in the functioning of the left ventricle when its ejection fraction is 25% or less. There are also relative reasons that may be contraindications to surgery: oncology, renal failure, lung diseases. In these cases, the doctor weighs the risks and benefits of intervention on the heart vessels, and makes his verdict in each case individually.
And the benefits of CABG are very significant: after the operation, the life expectancy of patients increases significantly, the quality of life increases significantly, and the risk of developing a heart attack decreases. If the doctor recommended this method of treatment to you, having carefully analyzed the history of your disease and assessed all the pros and cons, if you are confident in the doctor’s competence, then you should not be afraid of the operation or postpone it without significant reasons. Perhaps this treatment method will help you feel the taste of life again, forget about heartache and feel like a healthy person.
Indications
Restorative interventions on cardiac vessels are complex surgical procedures that are performed according to certain indications:
- angina pectoris of I-IV functional class with a defect of one stem or two or more coronary arteries, a proven area of ischemia of more than 10% of the myocardial mass;
- unstable angina - an acute condition with impaired blood circulation in one of the areas of the myocardium without the development of necrosis (infarction);
- early phase of myocardial infarction (with ST segment elevation - urgent indication, without elevation - after assessment on the GRACE scale);
- severe stenosis of the only remaining coronary artery (more than 50%);
- low tolerance to physical activity with the development of shortness of breath against the background of a decrease in the lumen of one of the arteries by more than 50%.
Depending on the clinical picture and characteristics of the course of the disease in each individual patient, the need for revascularization is determined by the attending physician.
Transluminal balloon angioplasty
Balloon angioplasty
An unprepared person will hardly be able to pronounce this method of treatment the first time; it is enough to remember that this method is one of the varieties of methods for revascularization of coronary vessels. Its essence is as follows: a catheter is inserted into the lumen of the affected vessel through the artery of the thigh or shoulder, the catheter with a balloon is advanced to the site of narrowing and the narrowed area is expanded 2-3 times by dosed inflation of the balloon.
Indications for the balloon angioplasty method are the same as for the previous surgical intervention. But the effect of the method is best if angioplasty is performed when the patient has 1-2 vessels affected and there is no involvement of the main trunk of the left coronary artery. It is worth noting that patients with angioplasty, according to medical observations, more often have to undergo repeated surgery than patients with bypass surgery. In 20-25% of patients, repeated stenoses of the same arteries are possible.
Types of surgical revascularization
Arteriotomy
Arteriotomy is the classic type of surgical revascularization. It involves external opening of the vessel and removal of the blood clot that has blocked the lumen. Arteriotomy operations have been carried out since 1912, when material for suturing blood vessels was first used.
Endarterectomy
Since the 40s of the last century, operations called endarterectomies have been carried out. Here we are talking about surgically “releasing” a blocked artery so that it is possible to get to the site of the blockage, excise the artery and remove the clot without serious surgical damage to the patient’s external tissues.
Removing a blood clot using a balloon catheter
Since the 60s, another improved technique has appeared: removing the blood clot using a balloon catheter. Such a catheter is brought to the thrombus “from the inside,” along the lumen of the artery. At the site of blockage, the balloon inflates and “releases” the clot. It is pulled to the place where it is most convenient to excise the artery without causing much damage to the patient’s external tissues. This is where the blood clot is removed.
Difficulties in carrying out such operations were due to the lack of “internal review”. Surgeons were forced to act by touch. There was a risk of incomplete and incorrect removal of the blood clot, with damage to the vessel, etc.
Currently, operations are not performed blindly, but under detailed radiological control. In addition, an additional tool is used - a cord inserted centrally along the lumen. It serves to guide the movement of the catheter through the vessel and more accurately remove the blood clot to the place where it will be cut out.
Often, in addition to removing the blood clot, it is necessary to perform other actions to clean the vessel: remove liming elements, etc. Detection of liming sites makes it possible to clarify the question of the origin of the disease. It becomes clear that thrombosis is its root cause.
Stenting
Stages of arterial stenting surgery
This is a minimally invasive intervention consisting of installing a stent - a mesh that is inserted into the affected vessel and straightens, creating a metal frame and shaping the desired diameter for the vessel. The method is less traumatic; the stent installation process occurs under X-ray control. This intervention can be performed already at the stage of coronary angiography; it is relatively safe, low-traumatic, and is performed under local anesthesia.
Coronary atherectomy
Catheter cutting atherectomy
A method based on the removal of atherosclerotic “plaque” from the lumen of the vessel using a special catheter. An atherectomy catheter is a device that relieves stenosis by cutting away the plaque with a sharp knife and then removing the cut mass. The peculiarity of the manipulation is that it can only be carried out in arteries with a lumen of 3 mm or more (this is due to the size of the catheter), and these are only large, main vessels. The method is relevant only for narrowing due to atherosclerosis.
Alternative techniques for surgical revascularization
Modern medicine has various means of minimally invasive revascularization. They are alternatives to classical surgical methods of excision of arteries (arteriectomy) - but are by no means methods of alternative medicine. These means have been adopted by official medicine, which today practically no longer gives preference to the classical means of vascular surgery.
Modern minimally invasive techniques are commonly called endovascular surgery. She is given preference. Endovascular surgery meets the interests of patients: the treatment is less painful, less traumatic, and postoperative rehabilitation is faster. The only question is whether this or that surgical clinic has equipment for minimally invasive endovascular operations and therapeutic actions, and whether its staff has the necessary experience.
Endovascular procedures involve the use of vascular catheters placed along the internal lumen of the artery not through an external incision, but through small “punctures” made in the shallowest areas of the artery (for example, in the groin). Attachments on catheters make it possible not only to catch a blood clot to remove it out, but also to expand the vessel from the inside (balloon dilatation) and implant a stent (a vascular frame that prevents its narrowing).
The modern technique of interventional thrombolysis (chemical decomposition of a blood clot) is based on the catheter administration of decomposing substances that treat the body of the blood clot. If the position of the blockage site is sufficiently “convenient,” substances for thrombolysis (streptokinase, urokinase, rt-PA drug) can be administered directly at the site where the artery is punctured.
Thrombectomy immediately frees the internal lumen of the artery. This means that blood flow is immediately restored. It takes time for the blood clot to chemically break down. Therefore, thrombolysis can be performed when the artery is not completely blocked. Or with simultaneous bypass of the blocked area (establishment of temporary bypass blood flow).
Laser methods
Laser revascularization
Laser revascularization is a new method; it has been used quite recently and at this stage is more of an experimental method. The meaning of laser myocardial revascularization is that a light guide is inserted into the coronary vessel and, using laser energy, the atherosclerotic “plaque” is removed without damaging the vessel wall. This improves coronary circulation.
Transmyocardial laser revascularization is indicated for patients with multiple coronary lesions when CABG or stenting is not possible. In addition to the emergence of new vascular communications, under the influence of the laser, myocardial axons are destroyed, which causes a weakening of pain impulses in the patient. Laser therapy methods require further study and development; perhaps they are the future of cardiac surgery, and they will not be inferior to direct methods of revascularization, and in some ways will surpass them.
answers to some questions / 2. circulatory diseases / 16. myocardial revascularization
Myocardial revascularization
general information
Myocardial revascularization
– a broad concept that includes both CABG surgery and various types of PCI on the coronary arteries.
The most well-known and widespread is balloon angioplasty, which can be combined with other effects on an atherosclerotic coronary artery: installation of a metal frame - an endoprosthesis (stent), burning out the plaque with a laser, destroying the plaque with a rapidly rotating drill and cutting off the plaque with a special atherotomy catheter. Revascularization, like pharmacotherapy, has 2 goals: improving the prognosis (prevention of MI and VS, reducing or completely eliminating symptoms. The main factors that determine the choice of treatment method are individual cardiovascular risk and severity of symptoms. Coronary artery bypass grafting There are two
indications
for CABG
: improved prognosis (reduced mortality; reduction in the risk of developing MI has not been convincingly proven) and reduced symptoms. In terms of its effect on prognosis, CABG surgery did not reveal any advantages over pharmacotherapy in low-risk patients (annual mortality less than 1%). According to meta- analysis, CABG improved the prognosis only in the average and high risk groups, however, in the average risk group, the 5-year mortality rate during drug therapy was 13.9%, and the annual mortality rate was 2.8%, which is high by modern standards
. Studies have established anatomical changes in the coronary arteries, in which CABG can improve the prognosis
: - significant stenosis of the main trunk of the left coronary artery;
- significant proximal stenosis of the 3 main coronary arteries; - significant stenosis of 2 main coronary arteries, including severe stenosis of the proximal part of the left anterior descending coronary artery. The criterion for significant stenosis in these studies was narrowing of the main coronary arteries ≥ 70% and the main trunk of the left coronary artery ≥ 50%. For left ventricular dysfunction, surgical treatment has advantages over pharmacotherapy (European Coronary Artery, North American CASS). Surgery has been shown to reduce symptoms and myocardial ischemia and improve the quality of life of patients with Std. These effects are observed more often than improvement in prognosis. The risks and benefits of surgery should be carefully weighed in low-risk patients in whom the goal is only to relieve symptoms. Perioperative mortality in CABG is, on average, 1-4%. In the last 20 years, the standard has been to bypass the left anterior descending artery with the left internal mammary artery and use the saphenous vein to bypass other arteries. However, stenosis of venous shunts remains a problem. Large studies have shown that the use of the left internal mammary artery for CABG improves survival and reduces the incidence of late MI, recurrent angina, and the need for repeat coronary artery interventions. Experience has been gained in using the radial artery. In this case, the rate of maintaining arterial patency exceeds 90% within 3 years. In patients suffering from serious concomitant diseases, it is advisable to perform minimally invasive interventions without cardiopulmonary bypass, which can lead to a decrease in perioperative mortality and the risk of complications. However, randomized studies have now been completed, which have shown no difference in the outcomes of minimally invasive interventions and standard operations during the first 3 years. Another randomized study with angiographic control after 3-6 months showed a decrease in the rate of bypass patency after minimally invasive surgery (90 vs. 98%). Percutaneous interventions on the coronary arteries
Coronary angioplasty with stenting in patients with CTS and suitable anatomy of the coronary arteries allows dilatation of one or more vessels with a high probability of restoring their patency and an acceptable risk.
The risk of death after conventional angioplasty is about 0.3-1%. According to the AVERT study, in patients with StES who belong to the low-risk group, lipid-lowering therapy is not inferior to PCI on the coronary arteries in the prevention of ischemic outcomes. However, PCI provides a more pronounced clinical antianginal effect. According to the COURAGE study, the odds of death and nonfatal myocardial infarction at 4.6 years of follow-up were no different between patients who initially underwent coronary angioplasty with stenting and those who subsequently received aggressive medical therapy. Vascular stenting and the use of drug-eluting stents
A meta-analysis of 29 studies in 9918 patients found no difference in mortality or incidence of myocardial infarction after coronary artery stenting and standard balloon angioplasty.
However, stenting leads to a decrease in the incidence of restenosis and the need for repeated interventions on the coronary arteries. According to randomized trials (RAVEL), drug-eluting stents (paclitaxel, sirolimus, everolimus) significantly improve treatment outcomes and reduce the risk of restenosis and adverse outcomes, including the need for repeat revascularization of the target artery. Indications for revascularization
Candidates for myocardial revascularization are patients who have indications for coronary angiography.
Additional indications are the following: - drug therapy does not provide satisfactory control of symptoms; — non-invasive methods demonstrate the presence of a widespread ischemic zone; — high probability of success with an acceptable risk of postoperative complications; — the patient prefers invasive treatment and has full information about the risks associated with the intervention. It is not appropriate to recommend invasive treatment in patients whose risk of perioperative death exceeds the estimated annual mortality rate. The choice of revascularization method is based on the following factors: - the risk of complications and death after the intervention; — probability of success, including the technical feasibility of performing angioplasty or CABG; — risk of restenosis or occlusion of the shunt; — completeness of revascularization; - presence of diabetes mellitus; — experience of a medical institution; - the patient's desire. Contraindications to myocardial revascularization
- Patients with stenosis of one or two coronary arteries without significant proximal narrowing of the anterior descending artery, who have mild or no symptoms of angina and have not received adequate drug therapy. In such cases, invasive intervention is not advisable, as well as in the absence of signs of myocardial ischemia during noninvasive tests or in the presence of limited areas of ischemia of viable myocardium. — Borderline stenosis (50-70%) of the coronary arteries (except for the main trunk of the left artery) and the absence of signs of myocardial ischemia during non-invasive examination. — Insignificant stenosis of the coronary arteries (less than 50%). - High risk of complications or death (possible mortality - more than 10-15%), except in cases where it is offset by the expected significant improvement in survival or quality of life.
Recommendations for myocardial revascularization to improve the prognosis in patients with stable angina (EOC, 2006)
Class I:
— CABG with severe stenosis of the main trunk of the left coronary artery or significant narrowing of the proximal segment of the left descending and circumflex coronary arteries (A);
— CABG for severe proximal stenosis of the 3 main coronary arteries, especially in patients with reduced left ventricular function or rapidly occurring or widespread reversible myocardial ischemia during functional tests (A); — CABG for stenosis of one or two coronary arteries, in combination with a pronounced narrowing of the proximal part of the left anterior descending artery and reversible myocardial ischemia in non-invasive studies (A); — CABG for severe coronary artery stenosis, combined with impaired left ventricular function and the presence of viable myocardium according to non-invasive tests (B). Class II a:
- CABG for stenosis of one or two coronary arteries without pronounced narrowing of the left anterior descending artery in patients who have suffered sudden death or persistent ventricular tachycardia (B); — CABG for severe stenosis of 3 coronary arteries in patients with diabetes mellitus, in whom signs of reversible myocardial ischemia are determined during functional tests (C); - percutaneous intervention or CABG in patients with signs of reversible myocardial ischemia identified using functional tests or frequent episodes of ischemia during daily activities (C).
Recommendations for myocardial revascularization to reduce symptoms in patients with stable angina (EOC, 2006)
Class I:
— CABG for multivessel disease (if technically possible) in patients with moderate or severe symptoms that cannot be controlled with drug therapy, if the risk of surgery does not outweigh its possible benefit (A);
- percutaneous intervention for stenosis of one coronary artery (if technically possible) in patients with moderate or severe symptoms that cannot be controlled with drug therapy, if the risk of intervention does not outweigh its possible benefit (A); - percutaneous intervention for multivessel disease (if it is technically possible and there are no anatomical risk factors) in patients with moderate or severe symptoms that cannot be controlled with drug therapy, if the risk of intervention does not outweigh its possible benefit (A). Class II a:
- percutaneous intervention for stenosis of one coronary artery (if technically possible) in patients with mild or moderately severe symptoms that are unacceptable to them, if the risk of intervention does not outweigh its possible benefit (A);
— CABG for stenosis of one coronary artery (if technically possible) in patients with moderate or severe symptoms that cannot be controlled with drug therapy, if the risk of surgery does not outweigh its possible benefit (A); — CABG for stenosis of several coronary arteries (if technically possible) in patients with mild or moderately severe symptoms that are unacceptable to them, if the risk of surgery does not outweigh its possible benefit (A); - percutaneous intervention for stenosis of several coronary arteries (if technically possible) in patients with mild or moderately severe symptoms that are unacceptable for them, if the risk of intervention does not outweigh its possible benefit (A). Class II b:
- CABG for stenosis of one coronary artery (if technically possible) in patients with mild or moderate symptoms that are unacceptable to them, if the risk of surgery does not exceed the estimated annual mortality (B).
Sexual activity
Sexual intercourse can trigger the development of angina, so you can take nitroglycerin before it. Phosphodiesterase inhibitors (sildenafil, tadafil and vardenafil) used to treat sexual dysfunction should not be used in combination with long-acting nitrates.
Modern non-drug methods for the treatment of stable angina
Enhanced external counterpulsation
Enhanced external counterpulsation (EECP) is an auxiliary method of treating refractory angina, which consists of sequentially pumping air into cuffs placed on the lower extremities.
The entire process is synchronized with the ECG. During diastole, the cuffs inflate sequentially and rapidly from the lower legs to the thighs and buttocks. This leads to an increase in diastolic and coronary perfusion pressure and increased blood supply to the myocardium. Instant pumping of air from the cuffs at the beginning of ventricular contraction (systole) reduces vascular resistance and relieves the work of the heart (reduces afterload). The long-term effects of the procedures are an increase in oxygen delivery and a decrease in myocardial oxygen demand, and the end result is an increase in coronary perfusion pressure and collateral blood flow, an increase in nitric oxide production, an increase in angiogenesis and, in general, a decrease in angina. Contraindications to the method include: decompensated chronic heart failure, severe pathology of the heart valve apparatus, severe uncontrolled arterial hypertension (BP above 180/110 mm Hg), malignant arrhythmias, severe pathology of peripheral vessels, severe varicose veins with the presence of trophic ulcers, high pulmonary hypertension, aneurysm and thrombosis of various parts of the aorta. In a randomized, placebo-controlled, multicenter study, external (external) counterpulsation reduced the frequency of angina attacks and increased the time of exercise before the onset of angina. The study involved 142 patients with refractory angina and a positive stress test. The course of treatment is 35 sessions, each lasting 1 hour. Active treatment group – 75 people, cuff pressure – 300 mm Hg, 4-7 sessions per week. Placebo group – 67 people, cuff pressure – 75 mm Hg. In an international study of 978 patients with refractory angina of class III-IV, using this technique, an improvement in the condition of one class was observed in 81% of patients, and the quality of life of patients significantly improved. The clinical effects of the course of EECP procedures included: reduction in the frequency of angina attacks, increased exercise tolerance, improved blood supply to the ischemic area of the myocardium according to myocardial radionuclide scintigraphy with thallium. Recently, evidence has been accumulating on the positive effect of EECP on improving vascular endothelial function and reducing the aggression of atherosclerosis. Cardiac shock wave therapy (SWT) Shock wave therapy
(SWT) is a new technology that allows non-invasively to improve the blood supply to the myocardium in the ischemic zone due to the formation of new capillaries.
The principle of shockwave therapy is based on the mechanical effect on the ischemic myocardium by the energy of an acoustic wave. At the same time, a number of vasoactive substances are released in the affected area, including nitric oxide and vascular endothelial growth factor, promoting vasodilation and neoangiogenesis. However, the effectiveness of shockwave therapy has been demonstrated only in pilot studies, so the pronounced positive dynamics of clinical manifestations of angina pectoris and objective indicators of myocardial perfusion require confirmation in large randomized studies. Transmyocardial laser revascularization (TMLR)
One of the new methods of surgical treatment of severe angina is transmyocardial laser therapy. This method has been officially used in the United States since 1998. In Russia, a number of leading cardiology clinics have also begun to actively use transmyocardial laser therapy over the past 3-4 years. The effectiveness of the method is associated with improved blood supply to the myocardium due to the flow of blood from the LV cavity through the newly formed 20-40 channels with a diameter of 1 mm. A number of studies (BELTEF, PACIFIC) indicate significant positive effects of this technique (increased exercise tolerance, decreased angina class). TMLR is performed during thoracotomy, either simultaneously with CABG or as an independent procedure. The TMLR method is quite effective; it reduces the FC of angina pectoris, improves perfusion, function and metabolism of the LV myocardium. Improved perfusion is observed only in laser irradiated areas in the presence of viable myocardium. The results of a 5-year observation of 80 patients with severe refractory angina showed that in 20%, after TMLR using a high-energy CO2 laser, angina completely disappeared, and in approximately 90% of patients with coronary artery disease, the functional state decreased by one class, according to the Canadian classification. However, surgery-related mortality is 5-10%, and additional 1-year mortality is another 10%.
Myocardial revascularization is a broad concept that includes both CABG surgery and various types of TKA. The most well-known and widespread is BAP, which can be combined with other effects on an atherosclerotic coronary artery: installation of a metal frame - an endoprosthesis (stent), burning out the plaque with a laser, destroying the plaque with a rapidly rotating drill and cutting off the plaque with a special atherotomy catheter. The immediate clinical effectiveness of TKA is quite high - angina attacks stop, LV contractile function improves. However, despite the simplicity and obvious feasibility of restoring coronary blood flow using TKA, the issue of preventing relapse of the disease as a result of the development of restenosis, which occurs in 32-40% of patients within 6 months after the intervention, remains unresolved. The indication for TKA is, as a rule, severe angina pectoris with damage to one or more coronary arteries, which is difficult to respond to antianginal therapy, and non-invasive tests indicate an unfavorable prognosis of the natural course of the disease. When determining the timing of intervention, the profession and wishes of the patient should be taken into account. Stenoses must be accessible to catheter technology, and occlusions must be less than 3 months old. In case of severe damage to the main trunk of the left coronary artery, surgical treatment is preferable, although in some cases TKA and stenting of the affected artery are possible. When comparing the results of drug treatment and TKA, the latter has an advantage in effectiveness in the immediate post-procedure period; With long periods of observation, the differences disappear. Coronary artery bypass grafting using venous and arterial grafts has become quite widespread. Low mortality rates, high clinical effectiveness and increased life expectancy of patients indicate the advantage of CABG over drug treatment, especially in multivessel lesions. When comparing TKA and CABG, identical clinical results are noted, but the surgical method has an advantage in patients with diabetes and in people with serious heart rhythm disturbances. TKA cannot be performed in a number of cases due to limited technical capabilities and anatomical features - extensive arterial occlusions, severe calcification. A differentiated approach to prescribing a particular treatment method allows you to achieve better final results. Despite the expansion of possibilities for drug treatment of patients with coronary artery disease, the introduction into clinical practice of TKA with stenting of the coronary arteries, and surgical methods of myocardial revascularization remain the most radical method of treating coronary artery disease. Indications for surgical myocardial revascularization - CABG - are determined by the severity of clinical angina (FC III-IV) and segmental narrowing of the lumen of the coronary arteries >70%. Indications for surgery can be determined only on the basis of the results of CAG and ventriculography, taking into account clinical examination data. The main coronary arteries and their large first-order branches are subject to bypass surgery. A previous MI is not a contraindication to surgery, and if post-infarction angina persists, it is recommended to perform the intervention without waiting 4-6 months, as is customary when the course of the post-infarction period is favorable. The amount of myocardial revascularization is determined by the number of diseased arteries supplying blood to the viable myocardium. Each ischemic area of the myocardium must be revascularized. It is not advisable to restore blood supply in the area of post-infarction cardiosclerosis. Currently, there is a definite tendency to bypass the maximum possible number of coronary arteries using autoarteries. For this purpose, the internal mammary arteries, radial arteries, right gastroepiploic and inferior epigastric arteries are used. Despite the quite satisfactory results of CABG, angina returns in 20-25% of patients within 8-10 years. Such patients are considered candidates for reoperation. More often, the return of angina is caused by the progression of coronary sclerosis and damage to autovenous shunts, which leads to stenosis and obliteration of their lumen. Shunts in patients with risk factors are especially susceptible to this process: hypertension, diabetes, hypercholesterolemia, smoking, obesity. Indications for CABG are: ✓ severe disabling or quality-altering angina (FC III-IV), not amenable to maximum drug therapy; ✓ results of non-invasive studies, in which there is low tolerance to FN and a pronounced ischemic reaction to the ECG, in the presence of functionally significant (≥70%) stenoses of one or more coronary arteries; ✓ stenosis of the main trunk of the left coronary artery ≥50%. When deciding on surgery, factors such as the presence and severity of concomitant diseases, age, social activity of the patient and his mood for surgical treatment are important. Reports in recent years about successful surgical treatment of coronary artery disease in patients with renal failure, cancer, and severe diabetes have shown that in such situations in each case it is necessary to carefully compare the possible risk and the expected effectiveness of the operation. Advanced age in itself is not a contraindication to surgery, but elderly patients with a complex of concomitant diseases are at significantly greater risk. Many social and psychological factors can cause patients to categorically refuse surgery. The presence of hemodynamically significant lesions of the main trunk of the left coronary artery, proximal narrowing in all three main coronary vessels, or other changes involving the proximal anterior descending coronary artery suggests a positive decision on the issue of surgery. Under the above conditions, patients even with a mild clinical picture of coronary artery disease may have incomparably better prospects with surgical rather than drug treatment. Significant impairment of LV function - EF 25 mm Hg, in the presence of clinically manifested HF, significantly worsens the prognosis of both surgical and drug treatment, but is currently not considered an absolute contraindication to surgical intervention
Source: https://venus-med.ru/cardial/103-revaskulyarizaciya-miocarda.html