0
Author of the article: Marina Dmitrievna
2017.07.17
751
Treatment
Medicine is constantly evolving, and today people who are at risk of death from ventricular arrhythmia have the opportunity to use an implanted cardioverter defibrillator. This surgical method of correcting arrhythmia is very effective and becomes a solution for those who do not respond to drug therapy. Previously, this category of patients was saved only by an automatic external defibrillator; now everyone can literally carry it inside themselves.
What is a cardioverter?
The cardioversion procedure is the provision of assistance to a patient with arrhythmia using electrical impulse therapy. In other words, this is an electrical recharge of the heart muscle, after which ideally sinus (correct) rhythm should be restored. Cardioversion and defibrillation differ from each other in some subtleties, in particular, the presence or absence of synchronization with the heart’s own ventricular contractions. Previously, this type of assistance was provided only using external devices, and the current was supplied to the heart muscle through the muscles of the anterior chest wall. At present, the use of such techniques is also possible with the help of a small device that monitors heart rhythm using implanted electrodes - a cardioverter.
This device is a small device consisting of a microcircuit and a lithium battery, which is sewn under the pectoralis major muscle. The device reads heartbeats using electrodes inserted into the cavity of the right atrium or right ventricle, depending on the type of arrhythmia. That is, such a rhythm “tracking” scheme is similar to a regular cardiogram, but the results of this recording are recorded in the device’s microcircuit. If the rhythm is good, no electrical stimulation is required.
If the patient has a paroxysm of tachyarrhythmia (*a life-threatening attack of palpitations - ed.), the cardioverter detects these disturbances and sends a low-power signal through the electrodes in order to synchronously depolarize all electrically active myocardial cells. An electrical “reboot” of the myocardium occurs, after which the correct rhythm should be restored. Thus, the device operates only “on demand,” that is, when an abnormal heart rhythm requires electrocardioversion.
Typically, the service life of the device is from 5 to 10 years. The equipment is checked at the medical institution where the implantation was performed once every five years. The test is carried out using a computer, which records all the indicators obtained when restoring the normal rhythm.
Device Features
A modern ICD is a system that consists of a device enclosed in a titanium housing and electrodes connected to it and located in the heart chamber. The device is implanted in the right or left subclavian region, and general anesthesia is required. During the implantation operation, after installation of the device, the defibrillation threshold is determined.
The device has a power source, namely a lithium, silver and vanadium battery, as well as a capacitor, resistors, a voltage converter, and a microprocessor. It also has a system for analyzing heart rhythm, releasing a discharge, and a database of information on electrograms of arrhythmic events.
Clinical practice includes the use of atrial and ventricular electrodes with active and passive fixation to provide cardioversion, defibrillation, antibradycardic and antitachycardic pacing. Today, two-chamber, single-chamber systems are used.
Detection of arrhythmias is based on analysis of the frequency of its rhythm, the morphology of the ventricular signal, the ratio of the characteristics of ventricular and atrial activity and the stability of the RR interval. Thanks to these characteristics, the cardioverter-defibrillator can distinguish between supraventricular and ventricular tachyarrhythmias.
The devices have areas for detecting fast and slow VT. When the arrhythmia rate falls into the first zone, the defibrillator is discharged to stop VF or rapid ventricular tachycardia. In another zone, different types of anti-tachycardia ventricular pacing can be performed to suppress arrhythmias. For each area, treatment algorithms and detection parameters are determined in accordance with the characteristics of VT. To install them, a programming device is used. Values may change during follow-up depending on the clinic.
The therapeutic algorithm, which is carried out by the device, is established for each patient individually. It all depends on the person’s condition, how he tolerates clinical tachycardia. For example, if ventricular tachycardia is not fast and hemodynamically insignificant, antitachycardia stimulation with short bursts of pulses with a frequency that is 10-30% higher than the frequency of tachycardia can be successfully used.
If VF or rapid VT develops, the first and foremost action is defibrillation. But the discharge power should be 10 J higher than the intraoperative defibrillation threshold. The aggressiveness of therapy should gradually increase. This means that the discharge power should increase and eventually reach 30 J.
to the point ↑
Indications for cardioverter implantation
The implantation operation must be carried out according to clear indications. In order to determine whether surgery is required, the following criteria must be interpreted by a cardioarrhythmologist:
1. Clinical:
- frequent attacks of tachyarrhythmias, with a ventricular rate of more than 150 per minute,
- loss of consciousness caused by hemodynamically significant tachyarrhythmias,
- the patient has a history of cardiac arrest resulting from ventricular tachycardia, after which the heart was able to be “started” using external defibrillation,
- paroxysmal tachyarrhythmias that are not amenable to drug restoration of rhythm.
2. ECG data, Holter monitoring:
- officially registered paroxysms of atrial fibrillation, supraventricular tachycardia, ventricular tachycardia, ventricular fibrillation.
3. Sometimes TPEFI is used to clarify the type of arrhythmia:
- transesophageal electrophysiological study, which allows to provoke and record paroxysmal tachyarrhythmia.
Indications for implantation
Having learned the benefits of a cardioverter-defibrillator, a patient with ventricular tachycardia or other arrhythmias may think that he definitely needs to install such an important device. But it is important to remember that not all people with arrhythmias can and should have such a complex and valuable device implanted. There is a group of indications that the doctor considers when deciding to install an ICD.
There is no need to argue with your doctor if he does not prescribe implantation. Of course, you can consult with several doctors, but in no case should you worry if you have not decided to install a cardioverter-defibrillator. This suggests that there are no serious threats to life, so, on the contrary, you need to be happy, because the body will not experience stress due to another operation.
The results of multicenter studies allowed a joint working group from America more than ten years ago to develop indications for which it is possible and even necessary to implant a device. In fact, there are many indications. They can be divided into several classes.
Class 1 indications:
- Cardiac arrest due to ventricular tachycardia or ventricular fibrillation, and the cardiac arrest must not be due to reversible or non-permanent causes.
- Unexpected persistent ventricular tachycardia, which is associated with organic heart disease.
- Syncope, the origin of which is not established, if an electrophysiological study induces hemodynamically significant ventricular tachycardia or ventricular fibrillation, and treatment with prescribed medications is ineffective or is not tolerated by the patient.
- Unsustainable ventricular tachycardia, which is caused by diseases of the blood vessels, previous myocardial infarction, LV dysfunction and some other conditions.
- Unexpected persistent ventricular tachycardia in patients who do not have organic heart disease and other treatment methods are not applicable.
There are also other classes of indications. These include various conditions, such as cardiac arrest, which is most likely due to ventricular fibrillation, but electrophysiological testing is not possible due to certain medical circumstances.
Also indicated are pronounced signs that are attributed to persistent ventricular tachyarrhythmias in patients on the waiting list for cardiac transplantation. There are other indications that the attending physician knows for sure. At the same time, it is not enough to simply identify from the patient’s words that there is some indication. A thorough examination is necessary to confirm the diagnosis.
to the point ↑
When is surgery contraindicated?
From the cardiovascular system point of view, the only contraindication for surgery is the patient’s presence of slow conduction through the heart muscle (blockade, sinus node dysfunction). That is, in the case when the patient has a rare pulse (less than 30 per minute), accompanied by loss of consciousness, the issue of installing another type of pacemaker - an artificial pacemaker - is decided. Installing a cardioverter in this case is not advisable.
General contraindications include the following conditions:
- Acute infectious diseases,
- Severe somatic diseases in the stage of severe decompensation (diabetes mellitus, bronchial asthma), in this case implantation is possible after the patient can be compensated,
- Exacerbation of chronic diseases (gastric ulcer, pyelonephritis, bronchitis, etc.).
These contraindications are relative, that is, implantation can be carried out, but later.
Indications
Many people who suffer from gastric tachycardia or other types of arrhythmia may want to install such a device, but you need to know about the indications and contraindications for its installation. After all, not all patients can use it. Before recommending implantation of a cardioverter-defibrillator, the doctor evaluates the indications for surgery.
You should not argue with a doctor in cases where he refuses to perform an operation. The argument becomes that there is no serious threat to life from the arrhythmia or that it can be successfully controlled with medications, which means that it is better to simply be glad that the operation will not take place and the body will not endure stress.
Over the years, there have been studies that have grouped indications into categories. If they are present in a person, it is possible, and sometimes even vital, to perform an operation to install a cardioverter-defibrillator.
How is pacemaker implantation performed?
Cardioverter implantation is carried out under X-ray surgical treatment conditions (in the X-ray operating room). After premedication and preparation of the patient using intravenous fentanyl or other antipsychotics, the surgical field is prepared (treatment with antiseptics, administration of subcutaneous anesthetics).
Next,
access is made to the subclavian vein and a conductor (introducer) is inserted into its lumen, into which the cardioverter electrode is inserted.
Under X-ray control, the introducer with an electrode inside is brought to the cavity of the right atrium (when installing a single-chamber cardioverter), and then into the cavity of the right ventricle (when installing a two-chamber and three-chamber cardioverter). The electrodes are fixed by “screwing” its tip into the inner lining of the atrium and ventricle. the device itself is sutured under the skin or under the pectoralis major muscle . It is small in size (smaller than the palm of your hand), and after tightening the sutures of the wound, it is almost invisible under the skin. The edges of the postoperative wound are sutured with self-absorbing threads, and wound healing occurs no later than 10-14 days.
The entire procedure takes no more than an hour and, in principle, is painless for the patient.
Living with an ICD
Your ICD. Some facts
- The human heart is a muscle approximately the size of a fist. The heart has a complex electrical system. It produces its own electricity, which causes the heart to contract and relax at the correct rhythm. Thanks to this, the heart muscle is able to pump blood throughout the body.
- For the heart to work properly, the chambers must contract in a coordinated manner and the resting heart rate must be between 60 and 100 beats per minute.
- Electrical signals may be blocked or arrive irregularly. This causes the heart to beat too fast (tachycardia or fibrillation) or too fast (bradycardia).
- Implantable cardioverter defibrillators (ICDs) are miniature computers that fit in the palm of your hand. Typically, they are implanted under the skin in the chest area.
- ICDs help cope with dangerous disorders that result in accelerated rhythm. These disorders occur in the lower chambers of the heart (the ventricles) and are called ventricular tachycardia (VT) and ventricular fibrillation (VF).
- In ventricular fibrillation, the heart beats so fast that it flutters and loses its ability to pump blood. This condition leads to sudden cardiac arrest. If the heart is not immediately made to beat, the person will die.
- If ventricular fibrillation occurs, the ICD can send a shock to the heart muscle to stop the fibrillation or fibrillation muscle contractions.
- ICDs have saved hundreds of thousands of lives and reduced the risk of sudden cardiac arrest for patients.
Living with an ICD
An ICD is a small implantable device that looks similar to a pacemaker (pacemaker). Typically, the ICD fits easily in the palm of your hand. While pacemakers speed up slow heart rates, ICDs are designed to slow down fast rates and provide life-saving therapy when the rate is dangerously fast. ICDs have saved hundreds of thousands of lives and reduced the risk of sudden cardiac arrest for patients.
Why do I need an ICD?
The heart has a complex electrical system. It constantly produces its own electricity, which causes the heart to contract and relax at the correct rhythm. Thanks to this, the heart muscle is able to pump blood throughout the body. Electrical signals may be blocked or arrive irregularly. This causes the heart to beat too fast (tachycardia) or too slow (bradycardia). For the heart to work properly, the chambers must contract in a coordinated manner and the resting heart rate must be between 60 and 100 beats per minute.
ICDs are intended for the treatment of dangerous disorders characterized by accelerated rhythm. These disorders occur in the lower chambers of the heart (the ventricles) and are called ventricular tachycardia (VT) and ventricular fibrillation (VF). If the ventricles fibrillate, they do not contract in a normal rhythm and efficient pumping of blood is impossible. Ventricular fibrillation becomes permanent and effective pumping of blood ceases. Most doctors believe that ventricular fibrillation is a condition in which the heart beats at least 300 beats per minute. If the heart muscle flutters, it is no longer able to pump blood. If in this case measures are not taken immediately, the patient may die.
Typically, ventricular fibrillation leads to sudden cardiac arrest. It should be noted that, if assistance is provided immediately, some people can be brought out of the state of sudden cardiac arrest, despite such a formidable name. Immediate care includes cardiopulmonary resuscitation. Its task is to maintain the blood pumping process. In addition, the erratic electrical activity of the heart should be stopped, the heart's normal rhythm should be restored, and serious complications that occur during periods of significant reduction in blood flow should be prevented. This requires a four to six minute shock from an external defibrillator or implantable cardioverter defibrillator (ICD).
How does an implantable cardioverter defibrillator (ICD) work?
An ICD is a medical device that is implanted in the body to monitor the rhythm of the heart and detect certain types of potentially dangerous rhythm disorders that cause very rapid heartbeats. The ICD is implanted under the skin and connected to one or two electrodes (thin insulated wires) that are placed in or on the heart muscle. Once ventricular fibrillation occurs, the ICD can send a shock to the heart muscle to stop the fibrillation or fibrillary muscle contractions.
How does a shock restore heart rhythm?
The pattern of electrical impulses in the heart is called the heart rhythm. The ICD tracks every beat of your heart. When it senses a dangerously fast rhythm, the ICD delivers an electrical shock. This interrupts the abnormal rhythm pattern and gives the heart the opportunity to restore its normal heart rate.
What other therapy does an ICD perform?
Defibrillation is the most important function that an ICD performs. Some ICDs are also capable of performing low-energy therapy to treat less severe rhythm disorders. This type of therapy is called anti-tachycardia pacing (ATP). In addition, an ICD can stimulate the heart in the same way as a pacemaker. These devices not only help maintain your heart rate, but also store a lot of information about your heart. The collected information can be obtained by the attending physician. They will help the doctor program the device so that the therapy performed best suits your condition.
What sensations accompany the discharge?
Different people perceive shock differently, so the experience of an ICD shock varies greatly. Some people don't even feel it. Some people experience moderate intensity sensations. Others describe the shock as a shock to the chest. Although the shock may cause discomfort, it means that the ICD has responded to a very dangerous heart rhythm disorder.
How often will I receive a shock?
It depends on the characteristics of the patient. Some people live for years with an implanted ICD and have never received a shock. Others receive shocks more often. It is not unusual for ICD patients to receive one or two shocks over many years. Ask your doctor about what to prepare for, but keep in mind that even he is not able to absolutely accurately predict what kind of therapy you will need.
What to do after the discharge?
The best thing is to find a place where you can sit down and catch your breath. Very soon the normal heart rate will be restored. You may feel slightly dizzy or disorientated for a short time. Do not worry. Some patients require only a few minutes to recover, while others require several hours. Most doctors ask patients to contact them after shock. The attending physician may ask you to come to him after the discharge for control. Because your healthcare provider is aware of your clinical condition, it is best to contact your healthcare provider for instructions about post-shock behavior.
How will the ICD “understand” that a shock is not needed if the heart is beating rapidly for a natural reason?
Any person leading an active life will experience tachycardia under stress. This is fine. After stopping physical activity, a healthy heart gradually restores its normal rhythm of contractions.
Most modern ICDs are capable of distinguishing natural from pathological tachycardia. Medically speaking, a fast heart rate caused by exercise differs from a potentially dangerous fast heart rate in the area where electrical impulses are generated in the heart. During physical activity, a healthy heart generates electrical impulses in its upper chambers. After this, the impulses are transmitted along the conduction pathways of the heart to the lower chambers, causing them to contract. Dangerously fast rhythms originate in the ventricles. To distinguish between these pulses, ICDs use formulas called “discriminators.”
How is an ICD implanted?
Generally, cardiac device implantation does not require general anesthesia. Usually, pain relief while maintaining consciousness is sufficient for implantation. You will receive medication to help you relax, but during the procedure you will remain aware of everything that is happening and will be able to hear and even talk to the doctor and nurses. Several medications will be administered when the incision is made. Although the local anesthetic will prevent severe pain, you may feel some pressure when the device is implanted.
What to expect during ICD implantation surgery?
First, the doctor will make a small incision in the upper chest and find a vein. A small puncture will be made in the vein, and then long flexible wires will be passed through the vein into the heart. The operating team monitors the progress of the electrode using a high-mounted monitor called a fluoroscope. The monitor shows a moving image in the X-ray part of the spectrum. Often the placement of the electrodes is the longest part of the operation. Once the electrodes are placed, your doctor will check them to make sure the electrodes are positioned optimally to deliver energy to the heart.
Once the electrodes are placed, your doctor will connect you to the implantable device. Then the doctor, separating the skin and underlying tissue from the underlying muscle, will form a “pocket.” Once the ICD is connected to the leads, it is placed in a pocket. After placing the device, the doctor will stitch the incision.
After the incision has healed, many people barely notice the small scar and slight protrusion. However, if the patient is short or thin, the device may protrude a little more. If you are concerned about how you will look after surgery, discuss this with your doctor. Sometimes the device can be placed in another place where it will not be so noticeable.
The length of surgery depends on the type of device being implanted, as well as your anatomy and the time spent determining the optimal position of the electrodes. Typically, ICD implantation lasts several hours.
What to expect after surgery?
Immediately after surgery, you will be taken to the intensive care unit. You may experience increased sensitivity at the implantation site for some time. You will stay in the hospital for anywhere from several hours to several days. Discuss the specifics of your case with your doctor.
During the postoperative period, carefully follow all instructions from your doctor. First, be sure to report any redness, tenderness, or tenderness near the implant site. If you notice redness or tenderness around your scar after leaving the hospital, contact your doctor immediately without waiting for your appointment.
How long will the recovery period last?
Because every patient is different, it will be difficult to accurately determine the length of the recovery period in your specific case. Follow your doctor's instructions carefully. For some time after surgery, your usual activities will be limited. Once your recovery period is complete, your doctor will be your best source of advice on how to resume your normal lifestyle.
What are the risks of using an ICD?
Your doctor is the best person to tell you about the risks of using an ICD. Do not forget to ask him all the questions you have and share all your doubts. A small number of patients with ICDs develop complications related to the implantation procedure. These complications include infection, a reaction to drugs used during surgery or to the device itself, blood loss, or damage to a blood vessel, heart wall, or other organs.
After the operation, you will experience some discomfort and loss of strength. Once you recover, you will feel better. However, some patients continue to experience discomfort at the ICD implantation site. If you also feel discomfort, tell your doctor about it. After ICD implantation, it is important to take certain precautions. You can safely use most appliances that are in working order and properly grounded, but you should avoid strong magnetic fields, including MRI devices. Your doctor will discuss any necessary precautions with you. In addition, you should carefully read all brochures supplied with your product, paying particular attention to the “Caution” and “Attention” sections. These sections contain important safety information.
ICD therapy may not stop the arrhythmia. Moreover, there is a possibility that therapy will make it worse. However, in an attempt to control the arrhythmia, the ICD will deliver more intensive therapy. There is a small risk that the ICD may fail to deliver needed therapy or provide therapy when it is not needed. An ICD does not always eliminate all symptoms of an arrhythmia. You may continue to feel dizzy or faint.
How often should I visit my doctor after implantation?
For routine check-ups, you will need to see a cardiologist or GP regularly. Immediately after surgery, you may need to visit your doctor several times. All of these visits are very important because they will allow the doctor to ensure that the implanted device is functioning correctly. The necessary adjustments are made painlessly in the doctor's office using a desktop computer called a programmer. Your doctor will also check whether your incision is healing. After this, you will visit your doctor regularly for follow-up examinations. Your doctor will advise you how often to do them. If the situation is stable, your doctor may suggest that you visit him once or twice a year or after you receive a shock. Your doctor may also need to see you if your family or GP has any concerns.
If many changes were made during your visit to the doctor, you may need to make your next visit a shorter period of time to ensure that the changes are effective and that there are no problems associated with them.
How is the inspection carried out?
The follow-up examination is absolutely painless and usually takes less than half an hour. During the examination, the doctor or nurse will place a sensor on the area of skin located over the implanted device. This sensor is similar in size and shape to a TV remote control.
Some devices do not require a sensor because they transmit information remotely. The device reports battery status information to the programmer, performs other system checks, and reports your heart rate information accumulated since your previous health check. If you have experienced a shock or therapy in the past time, the programmer will receive this information.
If necessary, the doctor can change some device settings to optimize therapy. For these reasons, it is very important that you follow your follow-up inspection schedule.
How will the doctor replace the battery in my device?
Implanted devices are powered by special batteries that are designed to last for a long time. These batteries do not die suddenly like flashlight batteries, but provide multiple warnings that the end of their life is approaching. Monitoring the condition of the batteries by the attending physician is part of the routine follow-up examination. Most devices' batteries last between three and six years, although this depends on the device and how often it sends electrical impulses to the heart. Once the device warns that the battery is low, your healthcare provider will schedule a replacement. Implantable devices are sealed, so batteries cannot be replaced. Instead, the doctor implants a new device. As a rule, this operation takes less time than the first one, since the doctor only needs to connect the new device to the existing cardiac electrodes.
Will an implantable device change my life?
You can live longer, healthier, more productive and happier. After surgery, you should limit your exercise for a while. Make sure you carefully follow all your doctor's instructions. Very soon you will be able to do everything you did before, and even more.
Should I stay away from devices like microwaves, magnets, and strobe lights?
Implantable devices cannot be damaged by working appliances such as microwave ovens, electric blankets, and most power tools. Using electric arc welding equipment or working with vehicle ignition systems will also not cause harm to the ICD. However, they may cause short-term interference with the proper operation of the device. Some medical equipment may also interfere with ICD operation. If you experience dizziness or palpitations (fast, irregular heartbeats), simply turn off the electrical equipment or move away from it. After this, the implanted device will restore normal functioning. If you must use equipment that may cause EMF, consult your healthcare professional. You can also request instructions from the equipment manufacturer.
Will medical equipment interfere with my ICD?
Although medical equipment generally does not interfere with ICD function, some devices can interfere with its function. Before you undergo any medical, including dental, procedure or test, such as electrosurgery, electrocautery, lithotripsy, or radiation therapy, tell your healthcare provider that you have an ICD implant.
Even with the ICD turned off, any diathermy is contraindicated for you. This procedure can damage the tissue around the implanted leads or permanently damage the ICD. Try to stay away from transcutaneous neuro- and myostimulation (TENS) devices. They may interfere with the operation of the ICD. Magnetic resonance imaging (MRI) scanners can seriously damage the ICD. When approaching or standing in the MRI room, the ICD may not function properly.
Can I use a mobile phone?
Mobile phones that send electromagnetic pulses can interfere with the normal functioning of the device. However, you can minimize the risk by taking simple precautions, such as not carrying your phone in your chest pocket above the ICD and keeping the device near the ear farthest from the ICD. ICDs contain special filters that protect devices from interference generated by mobile phones.
Will my iPod® or other portable media player affect the performance of my ICD?
There is no evidence that a portable media player such as an iPod or MP3 interferes with the normal functioning of the devices.
When can I resume physical activity?
Ask your doctor if you can resume physical activity. It is important to avoid shock to the area of the implanted device. So it's best to avoid contact sports like football. Otherwise, the device or electrodes may be damaged. After implantation, you may have more energy. Many people believe that by reducing the severity of symptoms, strength increases.
Can I do activities that require intense physical activity, such as hiking, skiing, or jogging?
It is best to always discuss your plans with your doctor. The doctor will give you advice about intense physical activity based on knowledge of your capabilities and condition. If the sport you play involves stress on your arm or chest (such as swimming or golf), you may want to discuss your pre-implant exercise with your doctor. This may influence the choice of device type and implantation site.
Is sex safe for me?
Typically, the implanted device does not have a negative impact on the patient's sex life except for a short period of hospital stay and recovery. However, it is important to follow your doctor's instructions about resuming physical activity.
Will I be able to drive a car?
Talk to your doctor about this. Keep in mind that although an ICD can stop fast heartbeats, it may not be able to prevent symptoms associated with the rhythm (such as dizziness and fainting). Before driving again, discuss the advisability of doing so with your doctor.
Can I travel?
Your doctor will best answer this question. Many ICD patients find that with a little more care and planning, they can enjoy traveling to many parts of the world. It always makes sense to plan your route carefully and leave a copy of the program with your loved ones. Just in case of difficulties along the way.
Will airport security systems affect the performance of my device?
Many patients are concerned about the security systems used at airports. They worry in vain. Indeed, security rules at airports have become stricter, but having an implanted device will not bring any additional inconvenience. It is best to go through the airport metal detector at normal speed. If an alarm sounds (which is completely optional), this only means that the system has detected the presence of metal in the implanted device.
Please present your patient card for screening. Ask for a manual search.
A security officer may use a hand-held metal detector. In this case, be sure to inform the supervisor that this procedure must be performed quickly and the sensor should not be held over the implanted device for more than a second.
What else should I know about traveling if I have an implanted device?
When traveling, be sure to carry important medical information with you, such as the names and dosages of medications, the name and telephone number of your doctor, and emergency medical care information. Also ask your healthcare provider for a copy of the most recent printout of the programmer test data and settings made during the last test. If you are traveling to a country that speaks Spanish, French or German, your doctor may be able to give you a printout in the appropriate language. (Some devices may soon be able to print in Italian, Japanese and Chinese.) Carry enough medications with you. If you are traveling by train or plane, keep some of your medications in your carry-on luggage and some in your suitcase.
Finally, let the attendants know if you have special dietary needs and develop healthy eating habits while on the road.
Do I need to take medications after ICD implantation?
Ask your doctor this question. Typically, an implanted device does not replace medications. Instead, the drugs and the implanted device work together. However, your doctor may adjust the dose.
Are there any food restrictions?
In general, to keep your heart healthy, doctors recommend eating foods that are low in sodium, fat, and sugar and rich in fiber and carbohydrates.
Are there complications after surgery?
Due to the fact that implantation is an operation with low surgical stress (there is no large incision, no long intervention and no large blood loss), postoperative risks are no more than 3% of all those operated on. However, this small proportion of patients may develop complications, but these unpleasant phenomena can occur after any operation. These include thromboembolic and infectious (inflammation of the wound edges) complications, as well as bleeding in patients with disorders of the blood coagulation system.
Prevention of complications includes early activation of the patient, careful treatment and timely change of dressing on the postoperative wound, as well as a comprehensive examination of the patient before surgery (in particular, a blood test for coagulation with the determination of specific indicators - INR, APTT, VSC, PTI, PTT).
In addition to these general complications, in occasional cases, premature failure of the device is possible - failure of the pacemaker. Due to the fact that modern devices rarely fail, the risks of such complications are minimized.
general information
The implanted device operates autonomously for a long time, but battery life depends on many factors. To summarize, the device will work for about 4-6 years, after which the battery will need to be replaced.
People who have an ICD should be aware that interference occurs from operating electronic devices, and they can also damage the defibrillator. Modern mechanisms are equipped with additional protection against waves and interference, but you should still be careful.
It is better to refuse to carry a phone near the mechanism; talking on a mobile phone is allowed if you put it to your right ear, away from the ICD. In stores, you need to walk near security counters as always, but do not touch them. If an ICD is installed, patients do not have to go through security counters at airports; the main thing is to carry a special ID.
If surgical interventions or tomography are carried out throughout life, then the doctor must be informed about the mechanism, because medical equipment can malfunction.
Complications without surgery
Despite the fact that some patients have a small risk of the complications listed above, the adverse consequences of tachyarrhythmias without implantation are much more common. The most dangerous of them is sudden cardiac death due to developed ventricular fibrillation. Therefore, if the arrhythmologist has identified clear indications for implantation in the patient, it is necessary to carry out this operation as early as possible.
What to do if you feel a cardioverter-defibrillator shock
Shock therapy with a cardioverter-defibrillator is a reason to make an appointment with an arrhythmologist to test the ICD, with the exception of patients connected to a remote monitoring system, when the patient’s condition during shock and the operation of the device are assessed remotely by a doctor. Shock can be motivated, this means that there was a life-threatening tachycardia, which the device cured.
In this case, a visit to the doctor will help assess the need to change antiarrhythmic therapy. Shock may be unmotivated, which means that shock occurred without the presence of life-threatening tachycardia. The reasons may be violations in the integrity of the electrodes, external electrical interference, or misperception of atrial tachycardia as ventricular tachycardia. In this case, during a visit to the doctor, the exact cause of shock will be determined and, if possible, eliminated.
How does life change after cardioverter implantation?
In general, lifestyle after cardioverter implantation requires minor correction, which is usually recommended for all patients with pathology of the heart and blood vessels. This is especially true for persons with organic heart pathology that has caused rhythm disturbances (coronary artery disease, previous heart attacks, heart defects, etc.). This requires restriction of physical activity (exclusion of professional sports), nutrition correction (exclusion of unhealthy foods) and elimination of bad habits.
As for ability to work, patients can engage in their usual work activities, as long as they do not involve working with electrical appliances, night work, or remote or long-term business trips. In principle, the patient’s ability to work after implantation is not impaired.
But as for disability , the following nuances should be noted. According to the Decree of the Government of the Russian Federation “On approval of the regulations on conducting a military medical examination”, in particular, on the basis of Art. 44, implantation of a cardioverter implies coronary heart disease with significant dysfunction. But in practice, everything happens completely differently. In order to receive disability after surgery, the patient must be examined by the ITU bureau, which takes into account the main disorders of the heart, including those in connection with the underlying disease. That is, the patient will be assigned a disability group, most likely, on the basis of organic pathology of the myocardium, which resulted in complete or partial loss of ability to work.
Among the main prohibitions after installing the device, the following can be noted:
- It is forbidden to perform MRI, and if this study is necessary, CT is performed,
- it is prohibited to perform lithotripsy (crushing stones in the gall bladder or urinary tract) without changing the cardioverter settings,
- perform surgery using electrocoagulation of tissues without appropriate adjustment of the cardioverter,
- Prolonged work with electrical appliances is prohibited,
- Carrying a mobile device in breast pockets is prohibited.
A patient with an installed cardioverter should visit a cardioarrhythmologist annually in a medical facility that has a computer capable of reading data from the device. Repeated implantation with complete replacement of the device is possible after 5-10 years, depending on the service life of the battery in the cardioverter.
What to expect after ICD implantation, are there any risks and possible complications?
for the first 1-3 days after surgery . During this period of time, the doctor once again checks the quality of operation of the installed device and monitors the general condition of the patient.
If conventional surgical sutures were used to close the wound, they are removed 10 days after ICD implantation.
Swelling and pain in the area of the device for the first couple of days are quite normal. Mild analgesics may be prescribed to relieve pain.
Discomfort associated with the introduction of a foreign body will be present for the first 2 months , especially when raising the arm. However, over time, a person gets used to the cardiac defibrillator and does not feel its presence.
A thin white scar forms at the site of the incision.
Possible exacerbations:
- Infection of the surgical site.
- Bleeding from the area where the ICD was placed.
- Poor tolerance of anesthetics used during manipulation.
- Damage to a nerve root, heart wall, or blood vessel.
- Entry of air into the pleural cavity.
Other likely consequences:
- Sending impulses that are not needed . This is especially true for young patients: their excessive physical activity increases the heart rate, which leads to unnecessary discharges. This phenomenon is usually accompanied by pain in the sternum and can cause damage to the organ. In such cases, you should consult a doctor: he will reconfigure the device or prescribe certain medications: Sotalol, Amiodarone, beta blockers, etc.
- Absence of impulses in case of cardiac arrhythmia . The reason for this lies in the malfunction of the stimulator - it needs to be changed or adjusted.
In addition, in order to protect the device from malfunction, it is necessary to avoid prolonged contact with devices that produce magnetic fields.
Examples of such devices are:
- Mobile/cell phones, MP3 players. If they are turned on, they should not be carried in a pocket in close proximity to the ICD.
- Microwave.
- Electric generators.
- Welders.
- Metal detectors. Before undergoing them, it is necessary to inform the personnel that there is a cardioverter-defibrillator in the body. You can pass through such detectors, but you should not sit near them or linger in the opening.
- Magnetic resonance tomographs.
The patient can confirm that an ICD is implanted into the body using a special certificate card , which must be given to him by a doctor. You must carry this card with you at all times.
Remote monitoring of patients with cardioverter-defibrillators
Almost all manufacturers of cardioverter defibrillators have remote monitoring systems. Two systems are registered in Russia today: Homemonitoring from Biotronic, and Carelink from Medtronic. The essence of the systems is that the patient is given a device that is placed next to the patient’s bed, where the patient sleeps at night.
And at certain intervals, the device wirelessly connects to the cardioverter-defibrillator and reads data, including information about the episodes of arrhythmia, shock therapy, electrode parameters, and battery charge. This information is sent via cellular communication to the hospital server.
The doctor evaluates this information and, if necessary, contacts the patient and calls him for testing or consultation. Remote monitoring systems allow early diagnosis of disturbances in the operation of the cardioverter-defibrillator. On the other hand, such systems can reduce unnecessary patient visits to the clinic.
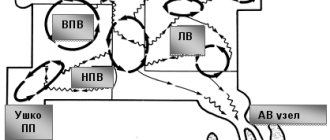
Single-chamber pacemaker
A single-chamber stimulator uses a single endocardial lead placed in either the right atrium or right ventricle to stimulate the cardiac chamber (atrium or ventricle).
Isolated atrial stimulation is used in cases where the generation of sinus rhythm (SSRS) is impaired while the atrioventricular junction (atrioventricular node) is functioning intact. In this case, cardiac pacing completely or partially replaces the function of sinus rhythm.
Ventricular stimulation is used if the patient has a permanent form of atrial fibrillation or transient atrioventricular blockade of the sinus rhythm into the ventricles occurs. In rare cases, it can be implanted with complete atrioventricular block.
Differences between a cardioverter-defibrillator and a pacemaker.
A cardioverter defibrillator is very similar to a pacemaker. But in the case of a cardioverter-defibrillator, it has the additional function of delivering a powerful electrical discharge - a shock, designed specifically to stop life-threatening arrhythmias. A pacemaker sends low-amplitude electrical impulses to the heart, which cause the heart to contract. The purpose of a pacemaker is to prevent your heart rate from becoming too low. A cardioverter-defibrillator, of course, can perform the function of a conventional pacemaker, but its main feature is the ability to generate high-energy impulses - shocks.
Dual chamber pacemaker
A dual-chamber pacemaker uses two endocardial leads to pace the right atrium and right ventricle. The electrodes are placed in the appropriate areas, thereby stimulating two chambers of the heart at once.
Dual-chamber stimulators are used to synchronize the atria and ventricles in cases of impaired atrioventricular conduction (AV junction dysfunction), which makes the heart rhythm closest to natural.
Both single-chamber and dual-chamber pacemakers can be equipped with a frequency adaptation function. The frequency adaptation function is used to increase the heart rate if one’s own, natural rhythm cannot respond by increasing the frequency to physical activity or to the emotional state of a person.
Frequency adaptation is marked with the Latin letter R. In single-chamber stimulators the designation SR is used, in dual-chamber stimulators - DR.