Allergic vasculitis is a non-decaying aseptic inflammation of the vascular wall that occurs as a hypersensitive reaction to various toxic and infectious foreign agents.
The dermatological manifestations of this disease are characterized by polymorphism: the rash consists of a wide variety of morphological elements. In addition, the clinical picture may vary in severity. Therefore, it is more correct to perceive allergic vasculitis as a collective name that unites individual diseases. All pathologies of this group can be divided into deep and superficial, depending on which structures are affected by the inflammatory processes.
Allergic vasculitis
Note! Diagnosis and treatment course require an integrated, multidisciplinary, but individual approach. It is important to take into account anamnestic and other diagnostic indicators.
With vasculitis of allergic origin, the pathological process usually involves subcutaneous superficial vessels without involving vessels in the internal organs. This is necessary to differentiate allergic vasculitis from systemic vasculitis.
This immunopathological disease occurs in both female and male people. It is typical for both children and adults. However, accurate epidemiological data are difficult to compile due to clinical and morphological polymorphism. There is a correlation with age, but only in some forms of this group of immunopathologies. For example, Schamberg's dermatosis mainly prevails in males, and Henoch-Schönlein disease (capillary toxicosis, immune microthrombovasculitis) - in adolescents aged about fourteen years.
Etiopathogenesis
Allergic vasculitis belongs to multifactorial pathologies. One of the mechanisms of pathogenesis is based on sensitization (the process of acquiring hypersensitivity to foreign agents) of the body, which can develop in the presence of chronic inflammatory and infectious foci:
- cystitis - inflammation of the bladder;
- tonsillitis - inflammation of the tonsils;
- otitis – inflammation of the middle ear;
- sinusitis - inflammation of the maxillary sinus;
- adnexitis - inflammation of the fallopian tubes;
- pyelonephritis - inflammation of the renal pelvis;
- tuberculosis.
Allergic vasculitis can develop due to taking certain medications or infection
Sensitization can develop against the background of herpetic infections, recurrent acute respiratory viral infections and hepatitis of viral etiology. Patients very often have high levels of antistreptolysin O (produced against the streptococcal antigen-streptolysin antigen) and increased levels of antistaphylococcal hemagglutinins (a substance that causes agglutination - sticking together of red blood cells).
In addition to infectious agents, the pathology is facilitated by the use of certain medications. These include:
- sulfonamides;
- oral contraceptives;
- analgesics;
- barbiturates, etc.
Note! This vascular disease can also be caused by chemicals, such as insecticides or petroleum products.
The cause of the development of this group of diseases can be long-term chronic intoxication and phytoallergens. The risk of disease is increased by intense or prolonged exposure to radiation on the immune system and genetic apparatus.
Factors contributing to the development of the disease may be:
- metabolic system pathologies: for example, diabetes mellitus;
- intraorgan disorders, especially liver disease;
- vascular disorders: varicose veins, hypertension, heart failure.
Various pathologies of internal organs and systems can contribute to the development of the disease.
The complex effect of the above leads to the formation of CECs (complexes consisting of antibodies and antigens that circulate), deposited on the vascular walls and leading to aseptic inflammation. Inflammatory processes increase the permeability of vascular walls. There is a correlation between the severity of the disease and the level of CEC.
Causes
This disease is very dangerous to health and requires immediate treatment, so you need to know its etiology. All age groups are susceptible to the disease, but the symptoms of allergic vasculitis observed in children and adults may differ. In children, skin spots have unclear boundaries and are hemorrhagic in nature. Sometimes different elements of the spot (rash) can merge. The spots that appear on the skin of an adult have clear boundaries.
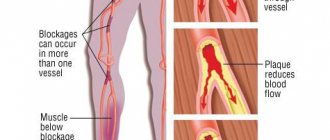
There are the following predisposing factors for toxic-allergic vasculitis:
- Metabolic disorders:
- presence of diabetes mellitus;
- overweight;
- atherosclerosis;
- gout.
- Autoimmune diseases:
- rheumatoid arthritis;
- systemic lupus erythematosus.
- Cardiovascular pathologies:
- heart failure;
- hypertonic disease.
- Liver disease or other associated pathologies:
- inflammatory bowel diseases;
- cirrhosis of the liver;
- malignant tumor;
- HIV – immunodeficiency virus, etc.
The following causes of allergic vasculitis are identified:
- Infectious nature:
- viral flora (herpes, influenza, hepatitis A, B, C);
- bacterial flora (mycobacterium tuberculosis, ẞ - group A hemolytic streptococcus, Staphylococcus aureus, leprosy);
- fungal diseases (candida).
- Exposure to allergens obtained from food - gluten, dairy proteins.
- The body's reaction to drugs:
- vitamin complexes;
- insulin use;
- antibacterial drugs (sulfonamides, penicillins, streptomycin);
- oral contraceptives;
- streptokinase, etc.
- Exposure to chemical compounds – household chemicals, insecticidal preparations, oil refining substances.
Classification
Rheumatology (a field of medicine that studies pathologies that systemically or locally affect connective tissue) classifies vasculitis according to the size of the vessels affected. The systematics depends on how deep the vessel affected by the pathology is located, what is the size of its lumen; area of blood supply and blood flow. The disease is divided into two forms.
- Superficial allergic vasculitis.
- Deep allergic vasculitis.
There are two types of allergic vasculitis
Superficial allergic vasculitis
In the superficial form, small vessels located in the skin are mainly affected. The following vasculitis are superficial:
- nodular necrotic. A more typical course is chronic, accompanied by general symptoms. Erythematous spots with small hemorrhages and nodes appear. It should be differentiated from a form of skin tuberculosis, which is characterized by papules and necrotic lesions;
- hemosiderosis;
- Ruiter's arteriolitis;
- leukoclastic microbial (erythematous-hemorrhagic spots against the background of exacerbation of chronic infections);
- smallpox-like parapsoriasis (nodules turn into ulcers with a necrotic center; accompanied by lymphadenitis and fever);
- hemorrhagic, accompanied by hemorrhage.
Hemosiderosis
Hemosiderin is a pigment formed during the breakdown of hemoglobin. Hemosiderosis includes allergic vasculitis, which is characterized by the deposition of hemosiderin on the vascular walls. On the skin of the distal parts of the extremities, characteristic petechial elements, telangiectasias, and small dark yellow spots appear, accompanied by intense itching. In some cases, trophic ulcers form. General symptoms usually do not accompany the main clinical picture.
Manifestations of hemosiderosis
The group of hemosideroses includes:
- Milian's white atrophy (depigmented areas of skin atrophy with a hemosiderotic rim against the background of varicose veins and chronic capillaries; risk factors: pregnancy, gynecological disorders, hemodynamic changes);
- itchy purpura (characterized by scaly erythema and pigmentation, intense itching, pronounced dermatological picture - increased lichenification);
- Majocchi's disease;
- pigmented purpuric lichenoid dermatitis (polymorphic bilateral rashes);
- Schamberg's disease;
Schamberg's disease
- arcuate Touraine's purpura with vascular ectasia (pigmentation and telangiectasia - dilation of skin vessels, in the form of semi-arches on the legs);
- orthostatic (correlates with age, associated with hemodynamic disturbances in the great vessels, characterized by erythematous-squamous lesions in the area of the lower extremities and pelvis);
- pigmented angiodermitis purpurosa (purple spots appear as a complication of varicose veins);
- senile (the result of degeneration of structural proteins).
Important! It is necessary to differentiate vasculitis of the hemosiderosis group with lichen planus (a disease of unknown etiology, characterized by pinkish itchy nodules), toxicerma (acute skin inflammation), atopic dermatitis (allergic skin inflammation) and eczema (blistering itchy rash).
Hemorrhagic vasculitis (Henoch-Schönlein disease)
With Henoch-Schönlein disease, not only the subcutaneous vessels are affected, but also the circulatory system of the internal organs. Microthrombosis is characteristic, accompanying non-infectious vascular inflammation. Depending on the pathogenesis, the following types of pathology are distinguished.
Table. Types of hemorrhagic vasculitis.
| View | Description |
| Abdominal | It is characterized by sudden intense pain in the abdominal cavity and bleeding of the intestinal tract. |
| Skin-articular | The rash consists of erythematous spots accompanied by small local hemorrhages. Skin manifestations are accompanied by inflammation of the joints - arthritis. |
| Renal | Clinical picture of acute or chronic glomerulonephritis (diffuse, bilateral inflammation of the kidneys, which mainly affects the glomeruli). |
| Lightning Necrotic | Systemic damage to several internal organs is typical: the myocardium, joints, and functional units of the kidneys. Manifested by bleeding from the gastrointestinal tract and nasal cavity. |
| Mixed | Manifestations of different types may occur simultaneously. |
Manifestations of Henoch-Schönlein disease
Capillarotoxicosis should be distinguished from dermatitis caused by medications, as well as non-hemorrhagic syndrome.
Ruiter's arteriolitis
This form is characterized by morphological polymorphism: the rash is a collection of blisters, papules, abscesses, vesicles, telangiectasias, as well as necrotic and ulcerated areas. Accompanied by general symptoms:
- headaches and arthralgia;
- low-grade fever - temperature in the range of 37 - 37.9 degrees;
- inflammatory changes in the elements forming the joint.
According to the nature of the main elements of the rash, arteriolitis is classified into:
- hemorrhagic;
- nodular-necrotic;
- polymorphonodular.
Manifestations of Ruiter's arteriolitis
The reaction is most often acute and occurs instantly. The rash can manifest itself in different ways (purpura, eczema, urticaria, etc.) and is accompanied by a worsening of the patient’s symptoms (burning of the affected areas, damage to the central nervous system; arthralgia, myalgia). With repeated exposure to an allergen, the rash most often appears in the same place, but the appearance of new lesions is also possible. The rash can occur not only on the epidermis, but also on the mucous membranes. Severe forms are possible: Steven-Johnson syndrome (acute bullous toxic-allergic disease) and Lyell syndrome (toxic necrolysis of the epidermis).
Deep allergic vasculitis
Deep vasculitis is accompanied by damage to larger vessels. Erythema nodosum is a deep form of vasculitis. This pathology is distinguished by the appearance of dense nodules as the main morphological element, which most often form in the area of the legs. Erythema can occur in both chronic and acute forms. In both cases, the patient's condition worsens, bilateral arthralgia and arthritis occur.
With deep allergic vasculitis, larger vessels are affected
Disease development process
If the basis of allergic vasculitis is an allergy, then the onset of the disease is considered to be the moment when the body begins to interact with some substance that is perceived by the immune system as an irritant.
After this contact, immunity provokes the appearance of immunoglobulins, which are specific antibodies.
Then the process of disease development begins, which consists of several points:
- After the initial production of antibodies, they remain in the blood until the body encounters the same allergen. And after the allergenic substance re-penetrates the blood, it binds with antibodies, resulting in the formation of immune complexes that form a connection with the cell membranes of blood vessels.
- Allergic inflammation begins, which damages and destroys vascular walls. And the degree of vascular damage depends on how pronounced and widespread the inflammatory process is.
- After damage, the vascular wall begins to allow both the liquid blood part and cell elements (erythrocytes, leukocytes, platelets) to pass through. We can say that small and large hemorrhages occur around the vessels.
- Hemorrhages lead to the onset of inflammatory processes and the formation of various symptoms. The causes of the disease depend on which part of the body the vessels are affected.
Allergies can affect the walls of both blood vessels and arteries. The rate of destruction of the vessel wall depends on its thickness and the diameter of the vessel.
Skin blood vessels are more affected by allergies. In addition to blood vessels, internal organs are also affected.
Children's forms
In children, allergic vasculitis initiates much more acutely and is more severe. Elements of the rash may generalize. Inflammatory reactions become more intense. The general condition of the child worsens. Noted:
- general fatigue and lethargy;
- sudden weight loss
- heat;
- dyspeptic symptoms (for example, nausea);
- pain localized in the epigastrium and intestinal area;
- pain in the intestines:
- arthralgia.
In children, this pathology is more acute.
Note! The disease is much more severe if the immunopathological process has affected internal organs. For the childhood form, relapses are more common. In children, periarteritis nodosa and hemorrhagic immune microthrombovasculitis usually occur.
Risk factors:
- hereditary predisposition to diseases that contribute to the formation of angiological, cardiac, and immunological pathologies;
- recurrent infections;
- hyperergy to allergens;
- vaccination;
- helminthiasis;
- hypothermia.
Forms of pathology can develop as a result of decreased immunity.
In what cases can you think about allergic vasculitis?
Allergic vasculitis may be suspected in patients with the symptoms described above under the following circumstances:
- if the patient has an allergic history (it is known that he is allergic to some substances or foods);
- if the fact of the patient’s contact with a substance to which he is allergic is clearly established;
- if the disease occurs immediately after such contact or shortly after it.
Many types of rashes described with allergic vasculitis can also appear with other diseases of an infectious or autoimmune nature. To confirm the allergic nature of vasculitis, complex immunological methods are used to show the presence of antibodies to the allergen in the patient’s blood.
↑ Return to contents
Diagnostics
If the clinical picture is typical, you should seek professional help. This pathology is a field of rheumatology. Diagnosis is difficult due to the polymorphism of morphological elements and the severity of the clinical picture, as well as the diversity of forms included in this group of pathologies. Attention is paid to collecting anamnesis, features of the clinical picture, age, and the nature of the clinic. Laboratory tests and skin biopsy are performed, followed by histological analysis. Using laboratory tests, the amount of CEC and ASL-O (antistreptolysin O) is determined; conduct biochemical functional studies of the liver, blood and urine tests; determine blood glucose levels.
Diagnosis of vasculitis must be comprehensive
The histological picture shows swelling and enlargement of the endothelium, which narrows the lumen. The walls are infiltrated with leukocytes. There may be hemosiderin deposits on the walls. RIF - immunofluorescence reaction - reveals deposits of complexes on the wall of affected vessels. Bacteriological examination of biological material (for example, depending on the suspicion of a lesion, smear, saliva, etc.), PCR (polymerase chain reaction), RPR (Rapid-plasma-reagin) test and phthisiological examination (phthisiology is a clinical discipline of medicine, which studies the etiopathogenesis of tuberculosis) are necessary to accurately determine the foci of infection.
To determine the causes of pathology and develop a course of therapy, detailed multidisciplinary diagnostics is necessary.
Diagnosis must be multidisciplinary, since the pathology affects the vascular system. Additionally, you may need consultations with an angiosurgeon and phlebologist (phlebology is a branch of medicine that studies the function and structure of veins), as well as a cardiologist. It may be necessary to perform ultrasound dopplerography (ultrasound Dopplerography), angio- and electrocardiography. The inclusion of other specialists depends on the extent of the process to internal organs.
UZGD
Forecast
There are many types of vasculitis, but overall the condition is rare. If you have angiitis, the prognosis depends on:
- Vasculitis type;
- What parts of the body are affected;
- How quickly the condition worsens;
- The seriousness and severity of your condition.
The disease responds well to treatment if it is started in a timely manner. In some cases, vasculitis may go into remission. “Remission” means “reduction, weakening” of the ongoing disease process, but it can also return at any time.
Sometimes vasculitis is chronic (long-lasting) and does not go into remission. Long-term medication treatment can often control the signs and symptoms of chronic vasculitis.
It is rare, but it happens that angiitis does not respond well to treatment, which can lead to disability and even death.
Much is still unknown about vasculitis. However, scientists continue to study what this disease is and its different types, causes and treatments.
Treatment
For medicinal purposes, it is first necessary to reduce the risk of further contact of allergens with the body. Therapy is carried out with antiallergenic drugs: antihistamines and desensitizing agents, as well as calcium supplements. In severe cases, cytostatics and glucocorticoids are used, as well as extracorporeal hemocorrection.
- Hemosorption is a method of extrarenal dialysis. Toxic substances come into contact with the adsorbent and are absorbed or enter into a chemical reaction. Using this method allows you to remove CEC and toxic substances from the blood.
- Plasmapheresis is a method of extracorporeal hemocorrection, which consists of collecting blood, centrifuging (dividing a heterogeneous substance into fractions by density using centrifugal force) of biological fluid and removing plasma with pathogenic substances. Using this method allows you to remove part of the plasma with toxins, antigens, etc. The patient is injected with his own mass enriched with red blood cells and platelets.
Infectious foci are sanitized. Systemic antibacterial therapy is used. As external agents, ointments containing clostridiopeptidase (an enzyme that catalyzes the hydrolytic cleavage of peptides), troxerutin (venotonic, antioxidant), cattle blood extract, chloramphenicol (an antibiotic), etc. are used. Local anti-inflammatory agents and dressings with dimethyl sulfoxide, as well as magnetic therapy and ultraphonophoresis is used for articular manifestations of the disease.
Treatment can be done with medications, diet, plasmapheresis, etc.
During exacerbations of the disease, bed rest is strictly indicated. Allergens should be excluded from the diet. Fatty, salty and fried foods should be limited. The diet must be enriched with foods containing protein and vitamins. Requires drinking plenty of fluids for detoxification. In severe cases, saline solution and the necessary medications are administered parenterally.
Drugs are used that increase vascular tone and reduce the permeability of vessel walls and thrombus formation.
Ascorbic acid and flavonoids, which have antioxidant properties, strengthen the walls of blood vessels and improve immunity.
For rapid healing, topical medications are used.
Note! Treatment of such pathology is always complex and individual.
Signs of damage or inflammation of internal organs
Symptoms of inflammation and subsequent damage to internal organs in allergic vasculitis can appear both before and after the rash occurs. But in the first case, they only complicate the diagnosis of the disease and can send the doctor down the wrong path. That is why you should be attentive to the manifestations of the disease and describe to the doctor in as much detail as possible the symptoms that worry the patient:
- Joint damage - swelling, hematomas (occur under the skin) and pain in the joint area. Most often, the knees and ankles are affected; less often, symptoms disturb the elbow and shoulder areas.
- Damage to one or both kidneys - lower back pain will be the most striking symptoms; urine tests show the presence of proteins and red blood cells in it. In the absence of proper treatment, renal failure and primary urinary syndrome develop.
- Damage to the central nervous system is a cerebral hemorrhage, which is difficult to diagnose and requires consultation with a neurologist.
- Damage to the heart or heart muscle - angina pectoris, arrhythmia, pressure drops, heart failure, stroke and heart attack develop.
- Damage to the secondary digestive organs and gastrointestinal tract - the main symptoms are nausea (vomiting), thick bloody streaks in the daily stool, spasmodic paroxysmal or acute pain in the stomach. Children and adolescents are more susceptible to this vasculitis than adults.
The symptoms described above may be supplemented by general malaise. The patient feels weakness, chills, surges in pressure and temperature, and appetite is significantly reduced.
▲
Prevention
To prevent vasculitis of allergic origin, it is necessary to avoid hypothermia and decreased immunity. Particular vigilance is required for children, since childhood forms of this group of pathologies are severe. Vaccination should be carried out only after prior consultation with a doctor, especially in cases where the family history is complicated by vascular and cardiac pathologies.
To avoid the development of such a pathology, you need to carefully monitor your health and promptly treat any ailments that arise.
You should avoid contact with potential allergens and improve your lifestyle. Proper nutrition will improve your immunity. It is important to treat infectious diseases promptly. Helminth infections should be treated promptly and adequately. If the development of such a disease is suspected, treatment measures are aimed at eliminating the underlying cause. If rashes appear and the patient’s general condition worsens, it is necessary to seek medical help.
Hemorrhagic vasculitis. Schonlein-Genyukh disease
Hemorrhagic vasculitis (vasculitis haemorrhagica) usually manifests itself as rashes, numerous small spots on large areas of the skin, accompanied by itching and burning, as well as deep swelling of the dermis and, in some cases, hemorrhages. Such symptoms are usually found with simple purpura, one of the variants of hemorrhagic vasculitis. Rheumatic purpura, in addition to skin lesions, affects large joints, for example, modifications of the knee joints. The abdominal type of hemorrhagic vasculitis manifests itself in the form of acute disorders of the gastrointestinal tract with the possible subsequent occurrence of nephritis. The abdominal type often occurs in childhood and adolescence.