Irina Ivanova
Hematologist
Higher education:
Hematologist
Samara State Medical University (SamSMU, KMI) Level of education - Specialist 1993-1999
Additional education:
“Hematology”
Russian Medical Academy of Postgraduate Education
Contacts
Vaginal discharge of a bloody type is the monthly norm for every sexually mature woman. If blood begins to flow during the intermenstrual period, then it is worth assuming that the cervix is bleeding, and there are a variety of reasons for this. The occurrence of this phenomenon is most often not the norm, so it is necessary to go to see an experienced specialist as soon as possible. There are several reasons why bleeding occurs; these can be both physiologically natural processes and pathological changes that threaten life. Only a qualified doctor can make a correct diagnosis.
Mechanical damage
Normally, the cervix does not bleed. If discharge appears, you need to immediately determine the reasons for its occurrence. Scanty bloody traces may appear due to mechanical damage to the organ:
- during installation or removal of the fallopian device;
- during abortion;
- when examined on a gynecological chair;
- during sexual intercourse;
- in the case of ultrasound examination with a vaginal probe.
When taking a smear, the cervix rarely bleeds, only if the specialist damages the tissue or walls of the organ. In all of these cases, the blood should clear within a few days. If the discharge does not stop within a week, visit your doctor immediately. It is the gynecologist who must determine whether there is cause for concern.
- Why does erosion bleed during pregnancy?
If the discharge does not appear immediately, but several months after the manipulation (abortion, curettage), this may indicate damage and the development of complications. Through a wound, infections and pathogenic bacteria easily enter the body, causing inflammation, suppuration, and abscess.
Why might the cervix bleed?
Normally, spotting in women of childbearing age appears once a month for several days (menstruation).
If spotting appears between cycles, this indicates some kind of problem.
Read on this topic - What are female discharge: causes and treatment
The causes of cervical bleeding may be:
- trauma to the mucous membrane during sexual intercourse
- after an abortion
- curettage
- after installation of the intrauterine device.
- Or for inflammatory/infectious diseases. Such as staphylococcus, streptococcus, chlamydia, etc.
If bleeding continues for one week after surgical intervention, you should consult a doctor. This may indicate some kind of infection that occurred during the procedure. If there have been no interventions, diseases may be present.
Doctors identify several diseases that can cause cervical bleeding.
Cervical erosion
The most common disease. The cervix bleeds often during examination by an obstetrician-gynecologist.
This happens due to the fact that there are ulcers on the neck, which, with any intervention, begin to bleed.
However, there are cases when erosion bleeds even with the simple secretion of mucus. Erosion appears and spreads with frequent inflammation, infections, and hormonal imbalance.
After cauterization of erosion, bleeding is also possible.
The reasons are:
- Licking the scab. A scab is a film formed after cauterization that protects the wound from infections. This film can thicken and collapse, and after the blood clots break down, the cervix may begin to curve.
- Damage to the scab. The scoop may come off due to heavy lifting or sexual intercourse.
Therefore, after the procedure for 2 months, it is necessary to protect yourself from lifting heavy things and refuse sexual intercourse.
Cervicitis
This is an inflammation of the cervix caused by injuries to the genital organ, pathogenic bacteria and fungi.
Polyps
That is, benign formations. A polyp leads to bleeding when it is large, since wounds and ulcers appear on it, which tear and bleed.
For reference! Even taking a hot bath is enough for the polyp to start bleeding. It also bleeds during sexual intercourse, physical activity, and the use of vaginal suppositories.
Cervical rupture
This is a postpartum injury caused by rapid labor, unqualified medical care, and late first birth.
And rupture also occurs during abortion (when the elasticity of tissues is lost).
Uterine cancer
The most terrible disease, for many people, it sounds like a death sentence. Often, advanced erosions, polyps, and inflammatory processes lead to malignant tumors of the cervix.
Also, the cervix may bleed during pregnancy.
This is caused by hormonal imbalance. In medicine there is such a thing as hormonal erosion.
The body is rebuilt, learning to live differently. However, the woman herself is unlikely to be able to diagnose whether the cervix is bleeding.
Perhaps there are other reasons. Therefore, do not diagnose yourself, but go straight to the doctor!
After a cervical biopsy, i.e. After plucking off living material, discharge is the norm.
However, you need to carefully monitor your condition. Depending on the method of tissue collection, the cervix may bleed for three to five days.
If this period is longer, you need to see a doctor. In this case, a blood clotting disorder is likely. As a result, the vessels located in the cervical cavity bleed.
There is such a procedure as conization of the cervix.
The procedure is an operation in which a cone-shaped portion of the cervix is removed.
The operation is performed as a means of diagnosing cancer, as well as in the treatment of certain female diseases.
After conization, bloody discharge along with mucus will be observed for four months. But bleeding should not be normal.
Many women have a question about whether the cervix may bleed when taking a smear for examination (for cytology, flora, etc.).
With such a simple and practically painless procedure, the cervix should not bleed. A
if there is such a phenomenon, then it may be a sign of diseases, for example, erosion, polyp, endocervicitis, ureaplasma.
Even a doctor can’t say for sure. We need an examination. A smear test will tell.
Erosion and ectopia
The main cause of background diseases of the cervical uterus is sexually transmitted infections, less often - traumatic (physical) and chemical factors. The result of infection with various STI pathogens is true erosion, which lasts approximately 10-14 days. Erosion is considered a reaction of the cervical epithelium in the form of the formation of a wound that bleeds. The most common causes are chlamydia, genital herpes, myco and ureaplasmosis, gardnerellosis and other opportunistic flora.
Destruction of a section of multilayered squamous epithelium under the influence of bacteria and viruses leads to its necrotic changes and desquamation - desquamation. A bleeding surface is formed.
One of the reasons why a wound appears on the cervix and it begins to bleed is considered to be injury, burn, or disruption of tissue trophism. The decrease in estrogen levels during menopause leads to vaginal dryness, which is a cause of injury. In addition, injuries also occur during rough sexual intercourse and rape. The cause of cervical burns and bleeding is considered to be attempts at self-medication and douching, which destroy the mucous membrane. During the destruction of various pathological formations with the help of liquid nitrogen, radio waves, lasers, and current, a burn scab is formed - this is one of the reasons why it can bleed. Increased bleeding occurs when the burn scab passes away.
As the ulcer heals, ectopia or pseudo-erosion forms. This means that the wound is healed not by flat epithelium, characteristic of the vaginal part of the cervix, but by cylindrical epithelium, which forms the cervical canal. The result of improper healing is ectopia.
In addition, the addition of infectious inflammation to ectopia leads not only to contact discharge containing blood, but also to the formation of purulent discharge from the genital tract. Erosion and ectopia can be asymptomatic.
One of the reasons why the cervix may bleed is ectropion. Often after a difficult birth, as well as with significant interventions, a deformation process - ectropion - can form. The pathology is an inversion of the cervical canal. Being in an unnatural environment, the columnar epithelium is attacked by the acidic environment of the vagina, which leads to tissue destruction and scarring. When contacting the lesion, the cervix bleeds.
After sexual intercourse or gynecological manipulations, the pathological lesion bleeds. Fresh blood is found in small quantities on underwear. The next day, the spotting turns brown and disappears.
Prevention
- timely treatment of hormonal imbalances, infectious diseases and inflammatory processes of the female genital organs;
- healthy lifestyle;
- regular examination by a gynecologist (every six months);
- using contraceptives if pregnancy is not part of your plans (abortion causes serious harm to health);
- careful attention to menstruation (keeping a calendar, which indicates the duration, regularity and abundance of discharge).
If the cervix is bleeding, and this is not related to menstruation, it is imperative to respond to this signal. The delicate organization of a woman’s genitourinary system is susceptible to any changes, and discharge notifies the woman herself of problems.
[31], [32], [33], [34], [35], [36], [37], [38], [39]
Menstrual bleeding is a natural monthly occurrence in the life of every woman of childbearing age. The appearance of other discharge containing streaks of blood indicates the development of dangerous pathologies, therefore such a symptom should be given due attention. Most often, the cause of bleeding is the impact of physical factors: mechanical damage during rough sexual intercourse or when taking a smear from a gynecologist. The unreasonable appearance of discharge is a reason to consult a doctor, because only after diagnosis can the risk of developing dangerous pathologies be eliminated. Find out more about the reasons that can provoke bleeding not related to menstrual bleeding.
Precancerous conditions and cancer
The causes of bleeding caused by precancerous changes are associated with the destruction and damage of capillaries. Dysplasia develops as a result of the pathogenic action of HPV with a high risk of carcinogenesis.
At levels 2 and 3 of dysplasia, contact bleeding occurs.
One of the few reasons why the cervix bleeds is a malignant tumor. Cervical cancer is accompanied by the destruction of blood vessels by a growing tumor, and not by a change in their structure and permeability, so bleeding develops not only upon contact, but also spontaneously. When a large vessel is destroyed, bleeding can be profuse.
Injuries to female genital organs
Situations when organ tissue and epithelium are damaged, resulting in rupture of blood vessels, occur during pathological childbirth:
- narrow pelvis;
- large fruit;
- forceps delivery;
- manual (obstetric) assistance during childbirth.
Unprofessionally placed sutures on the cervix interfere with normal blood circulation and cause changes in the vascular network and nearby tissues. It is possible that the vessels will bleed at the slightest stress - physical, sexual intercourse.
Damage to the uterus and cervical vessels most often occurs during abortion, when it is necessary to artificially expand the cervical canal. The surface of the canal is injured, the capillaries burst, and a temporary metabolic disorder occurs in this area, which leads to inflammation.
Menstrual irregularities and pregnancy
Among the many reasons why the cervix bleeds, there is a hormonal imbalance. Menstrual cycles without ovulation, occurring against the background of increased estrogen production and low progesterone levels, lead to dysfunctional bleeding. It may bleed for several months, and profuse bleeding is also typical. This is due to constant estrogen stimulation of the endometrium. Spotting is observed when taking COCs and intrauterine devices.
The cervix may bleed if there is a threat of miscarriage. In this case, both the separation of fresh blood and brown daub are observed. In such situations, it is important not to miss an ectopic pregnancy, in which the same symptoms are observed, as well as severe pain.
After childbirth and surgical interventions, bleeding from the genital tract due to injury. Normally, bleeding gradually weakens and turns into bloody discharge. If bleeding resumes, consult a doctor immediately.
To find the cause of bleeding, ultrasound, extended colposcopy, PCR diagnosis of infections, smear cytology, and blood tests for sex hormones are performed.
Head of the obstetrics and gynecology service at the Medical Center in Kolomenskoye, obstetrician-gynecologist of the highest category, candidate of medical sciences. Area of professional interests: operative gynecology, observation of pregnant women, gynecological endocrinology, reproductive medicine, ultrasound in gynecology, IVF.
What factors can provoke bleeding?
The intensity of cervical bleeding may depend on the nature of the ongoing gynecological disease. The cause of the symptom is often injuries to the cervix, which are obtained in this way:
- having sex with a sexual partner;
- self-examination of the cervix;
- performing ultrasound transvaginally;
- gynecological examination in speculum or bimanual examination.
It is necessary to pay attention to the fact that bleeding from the cervix, which appears as a result of a gynecological examination or having sex, is not the norm. If a small drop appears once, we can talk about accidental damage, but if this is typical for each examination, the patient needs a comprehensive examination.
The intensity of bleeding of the cervix may vary depending on the degree of its damage or the nature of the progress of gynecological pathology. The discharge can be almost transparent, containing streaks of blood, and thick (brown or almost black). Women call them “daubs.” If there is an open, fresh wound on the surface of the cervix, the blood will be a rich scarlet color. The appearance of such a discharge really indicates bleeding resulting from an injury.
In general, bleeding from the cervix in women occurs in the following cases:
- a few days before or after menstruation;
- in the middle of the menstrual cycle;
- during the healing period after surgery;
- after a gynecological examination or sexual intercourse.
The list of main reasons that can provoke bleeding includes:
- taking hormone-containing drugs to prevent unwanted pregnancy;
- intrauterine device;
- hormonal disbalance;
- erosion;
- dysplasia;
- cervical endometriosis;
- myoma;
- papillomas on the cervix;
- adenomyosis;
- polyps of the cervical canal;
- endocervicitis;
- erythroplakia;
- leukoplakia;
- cervical cancer.
Bleeding that occurs during pregnancy indicates a threat of miscarriage or placental abruption. In the early stages, the appearance of non-standard discharge may indicate an ectopic localization of the fertilized egg.
It is impossible to determine the cause of blood discharge from the genital tract on your own. Since such a change is one of the symptoms of dangerous female diseases, the girl should seek medical help as an emergency. After conducting an examination and receiving the results of the required studies, the doctor can give an opinion and answer the question of why you are worried about bleeding that is not related to menstrual bleeding.
| Background and precancerous diseases that can provoke cervical bleeding | |
| Background | Precancerous |
| Ectopia; | |
Erosive lesion (true and false);
Cervicitis.
Condylomas.
The reason for the bleeding is that the violation leads to the destruction of the mucous layer lining the cervix, while the vessels are located close to the surface.
Features of the course of erosion and ectopia of the cervix
The reason for the appearance of erosion and ectopia of the cervix is infectious or traumatic, chemical damage to its mucous membranes. The causative agents of diseases are various sexually transmitted infections. By definition, erosion is a wound on the surface of the cervix that has a tendency to bleed.
The list of main pathogens includes:
- chlamydia;
- herpes;
- mycoplasmosis;
- ureaplasmosis;
- gardnerelez.
When multilayered squamous epithelium is destroyed as a result of increased activity of pathogenic microflora, necrosis of certain foci appears, desquamation occurs, and a bleeding surface forms at the site of the lesion - erosion.
Ectropion
Ectropion is a process of tissue deformation that can form after severe surgery and childbirth. The concept refers to inversion of the cervical canal. It can evert out due to internal ruptures of the cervix. When exposed to an unnatural environment, the columnar epithelium is attacked by the acidic environment of the vagina, which provokes cell destruction and leads to scarring.
Serious pathologies
Bloody discharge can be caused by serious diseases, such as inflammation of the cervix (cervicitis). The process can occur due to mechanical injuries or under the influence of infections, fungi, and sexually transmitted bacteria. Sometimes the inflammation goes unnoticed, in other cases it has severe symptoms. The pathology must be treated in any case. Neglected cases lead to infertility and other serious problems in the woman’s reproductive system.
Blood in the vaginal discharge may also appear due to a polyp on the cervix. This is a benign pedunculated tumor. If the polyp is not treated, ulcers appear on its body, which cause bleeding. Also, the compaction can develop into a malignant neoplasm.
When considering the causes of bleeding, we must not forget about erosion. This disease is a sign of serious problems in the female body. Most often, erosion bleeds upon examination; less often, blood appears in normal discharge. Erosion occurs due to sexually transmitted infections, hormonal imbalance, but the most dangerous causative agent of the disease is the human papillomavirus. It also causes cancer of the genital organs. Erosion requires medical treatment, but if therapy is ineffective, the damaged area is removed surgically.
Conditions in which atypical cervical vessels are observed
It has been noticed that with some diseases of the female genital area, the vascular network changes. There are more capillaries, although people do not develop new vessels during their lifetime. Consequently, the appearance of new ones is considered as a pathology requiring observation and treatment.
Precancerous condition in gynecology:
- dysplasia - a change in the structure of the cells of the mucous membrane of the cervix, abnormal functioning;
- leukoplakia - keratinization of the mucous membrane, the formation of a white plate on the cervix with transition to the vaginal part;
- erythroplakia - atrophy of the upper epithelial layer, in which the mucous membrane becomes thinner and blood vessels become visible;
- fibroids - often turns into cancer, the growth of a benign tumor is accompanied by changes in blood vessels, an increase in their number;
- ectropion and erosion quite often turn into dysplasia when nutrition and metabolism are disrupted.
At the slightest suspicion of an abnormal condition of the vessels in the cervix, it is necessary to conduct a more in-depth examination of the female genital organs, establish the cause and draw up a plan for further action.
With tissue proliferation (regeneration, renewal), increased vascular growth is observed. This is explained by the process of restoration of damaged tissues after inflammation.
Most scientists consider changes in the structure of the vessels of the uterus and cervix to be a sign of malignancy (malignant degeneration). They have different forms:
- hairpins;
- commas;
- thickenings in the form of a cut branch;
- a loop;
- corkscrew.
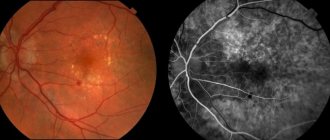
You can see the vessels on the cervix in more detail when exposed to acetic acid. In normal tissue, capillary walls contract. Atypical forms do not react to the stimulus in any way because they have an atrophied muscle layer. Additional examination of the area around the changed arteries is required. Diagnosis involves repeated biopsy sampling for histological analysis and colposcopy with multiple magnification.
Signs of cervicitis
Inflammation of the canal or the outer part of the cervix can manifest itself with the following symptoms:
- copious mucous or purulent discharge (cloudy, yellowish, foamy, mixed with blood), increasing after menstruation;
- dull pain in the lower abdomen and in the sacral area (appears when inflammation spreads to surrounding tissues);
- painful sexual intercourse.
With cervicitis, irritation and itching of the genital organs sometimes appear, which are caused by increased discharge.
The acute process is also characterized by a slight increase in temperature, weakness, and deterioration in general health.
If you notice any of these symptoms, contact your doctor as soon as possible. A specialist will examine you and prescribe the necessary tests.
Reasons for the development of pathology
If the cervix is bleeding, this is an alarming sign that may indicate a dangerous disease.
There should be no bleeding from the cervix. However, there are times when a woman notices a slight discharge of blood outside of menstruation.
The mucous membrane can be injured due to:
- Gynecological examination.
- After sexual intercourse.
- Transvaginal ultrasound examination.
- Installation of the spiral or after its removal.
If the bleeding after the procedures goes away on its own, then there is no need to worry. Blood discharge can be observed during abortion, curettage, or during hysterography.
The cervix may bleed due to the development of certain gynecological diseases, namely:
- Cervicitis. Cervicitis is commonly understood as inflammation of the cervical mucosa. The disease can occur when a fungal or bacterial infection occurs.
- Polyps of the cervical canal. Polyps are classified as benign formations; their development can be asymptomatic and can only be detected during a gynecological examination. In appearance, it is a wart on a stalk. The tumor must be treated, as it may increase in size, resulting in increased bleeding. Polyps can appear due to hormonal imbalance, prolonged stressful situations, and age-related changes. The formation of polyps may be associated with infectious diseases.
- Erosion. With erosion, the mucous epithelium of the cervix changes due to mechanical stress or infectious and inflammatory STDs.
Characteristic signs
Vaginal flora smear is an effective diagnosis of gynecological diseases
Bloody discharge from the cervix appears outside of menstruation. They are usually spotty and brown in color. Discharges are observed periodically. In addition, the following symptoms may be observed:
- Discomfort in the lower abdomen.
- Menstrual irregularities.
- Discharge of serous, purulent leucorrhoea.
- Heavy periods.
Pain in the lower abdomen can be of different types: sharp, dull, cutting, pulling. These unpleasant sensations usually appear after sexual intercourse.
If you experience pain in the lower abdomen and spotting from the vagina between periods, then this is a serious reason to contact a gynecologist and undergo an examination.
When contacting a gynecologist with these symptoms, the doctor will conduct an examination using special mirrors. During the examination, the size and shape of the cervix, the presence of deformation, ruptures, etc. are determined. The gynecologist will also take smears for flora and infections.
If necessary, colposcopy is performed. This procedure allows you to study the mucous membrane of the cervix in more detail and collect material for research. The gynecologist may also refer you for an ultrasound examination to exclude or identify tumors, cysts and other formations.
Sources and pathogens
Depending on the cause that provoked the disease, cervicitis is divided into the following types:
- specific: caused by sexually transmitted infections: chlamydia, mycoplasma, trichomonas, gonococci, viruses (herpes, HPV);
- bacterial: develops as a result of changes in the natural microflora of the vagina, as a result of which nonspecific pathogenic microorganisms are activated: staphylococcus, streptococcus, fungi, E. coli;
- traumatic: can be caused by damage to the cervix during childbirth, abortion, curettage;
- atrophic: often a consequence of characteristic changes in the mucosal epithelium during menopause;
- allergic: the main reason is an allergy to spermicides and latex used in the manufacture of condoms.
Each type of cervicitis of the cervix may have its own specific symptoms. Only a doctor can establish a complete picture of this disease after examination and obtaining diagnostic results.
conclusions
A serious disease of the female genital organs can be suspected by changes in the appearance of the blood vessels. A detailed examination is necessary in any case, since the altered structure of the veins may be the result of malignant tissue degeneration.
All iLive content is reviewed by medical experts to ensure it is as accurate and factual as possible.
We have strict sourcing guidelines and only link to reputable sites, academic research institutions and, where possible, proven medical studies. Please note that the numbers in parentheses ([1], [2], etc.) are clickable links to such studies.
If you believe that any of our content is inaccurate, out of date, or otherwise questionable, please select it and press Ctrl + Enter.
When a woman experiences spotting brownish discharge between menstruation or bloody streaks of blood appear in her normal leucorrhoea, this may indicate that the cervix is bleeding. Symptoms of bleeding from the cervix cannot be ignored, since this is a signal of serious processes that can lead to serious consequences in the future.
Atrophic cervicitis
Against the background of declining sexual function and the resulting estrogen deficiency, changes begin in the vaginal epithelium: it becomes thinner and drier. In addition, the acidity of the environment decreases, and the protective functions of the internal microflora are weakened. This leads to the risk of developing various types of inflammation, in particular, the occurrence of atrophic cervicitis.
With this type of disease, a slightly different colposcopic picture is observed:
- The mucosa is thinned, has a pale pink color, and visible petechial vessels (with pinpoint hemorrhages) are visible on it.
- With slight pressure, the vessels begin to bleed.
If the patient exhibits signs of atrophic cervicitis of the cervix, treatment always includes hormone replacement therapy. This method helps to stop the processes of atrophy in cells and restore the function of mucous membranes.
EPIDEMIOLOGY OF CERVICAL CANCER
Lifestyle, bad habits
The first studies on the epidemiology of cervical cancer appeared in the nineteenth century. Rigoni-Stern in 1842 published data based on a study of the death register in Verona from 1760 to 1830. He noticed that cervical cancer was significantly more likely to cause death in married women and widows and was not found in virgins and nuns. This circumstance allowed the scientist to put forward a hypothesis about cervical cancer as an infectious disease. In a study of 13,000 case histories of nuns in Montreal and Quebec, F. Gagnon (1950) noted that cervical cancer was never detected. The author associated these results with the low incidence of inflammatory diseases of the cervix in nuns.
The results of epidemiological studies concerning the role of early onset of sexual activity, early first pregnancy, frequent change of sexual partners, as well as sexually transmitted infectious diseases in the occurrence of cervical cancer have been published. There is now convincing evidence of an increased risk of developing cervical cancer in women who smoke. Some authors (Hellberg, Greenberg, Winkelstein, Brinton) note the relationship of smoking with early onset of sexual activity and frequent changes of sexual partners, others (Hoffman, Sasson) point to the carcinogenic role of nicotine and cotinine contained in tobacco smoke.
Chronic cervicitis
If the acute process is not treated, then the disease takes a chronic form within a month. At the same time, the woman may have the feeling that “everything has passed”: the discharge has become less or disappeared completely, the pain has subsided. Such patients often come to us. After a detailed interview, it is possible to find out that some time ago there was clearly acute cervicitis, the treatment of which the woman prescribed for herself. Result: the disease did not go away, but hid, and at the first “convenient” opportunity it made itself felt. Such cases may include weakened immunity, overwork, and stress. Discharge and genital irritation appear again, and sometimes there is a burning sensation when urinating.
With old inflammation, the cervix looks hyperemic, somewhat swollen and thickened. Sometimes a doctor discovers chronic cervicitis during pregnancy, and then the main task is to choose a treatment tactic that will reduce the risk of miscarriage, but will not harm the fetus.
Diagnostics
The doctor detects visual signs of cervicitis already during the examination. To clarify the diagnosis, colposcopy is performed. If cervicitis has developed, the following picture is observed during the study:
- Hyperemia of the cervical mucosa is clearly expressed (there are areas of redness).
- Dotted inclusions or reddish spots with unclear outlines are noticeable, which, after wetting with a vinegar solution, turn pale and become clearer.
- Spots of various shapes are visible, protruding above the surface of the surrounding tissue.
- Redness around the cervical canal and a slight protrusion of the mucous membrane are detected.
In addition to colposcopy, histological and cytological research methods are used for differentiated diagnosis of cervicitis. As a rule, anti-inflammatory therapy is prescribed before the Pap test and biopsy. Goal: to increase the reliability of diagnostic results so as not to miss the onset of cell mutation.
Frequent consequences of cervicitis are erosion of the cervix, spread of infection to internal organs, and transition of the disease to a protracted form. The only way to avoid this is to treat the disease when the first signs appear.
The doctor draws up a treatment regimen immediately after receiving the test results. External methods include treating the affected area with brilliant green, hydrogen peroxide, and silver nitrate solution. Antibiotics are selected according to the sensitivity of pathogens to them.
In chronic cases, a complex of vitamins and immunostrengthening agents is prescribed. If the disease is caused by viruses, antiviral drugs and cytostatics are included in the therapeutic regimen.
If you suspect you have cervicitis, you should not use folk remedies, especially on your own. The doctor may prescribe douching with medicinal decoctions, but only as an auxiliary type of treatment that complements the complex of basic measures.
In our clinic, laser method and radio wave therapy are effectively used to combat cervicitis. If there are specific infections, the partner should also undergo treatment at the same time.
The criterion for cure is the disappearance of external signs, “clean” smear tests. The result is monitored one and three weeks after completion of the course of therapy.
In order not to jeopardize your health, infectious diseases should be treated in a timely manner. And to detect them, visit a gynecologist annually and immediately make an appointment if alarming symptoms appear. In our Center you will always be provided with comprehensive assistance for any type of pathology, using the latest diagnostic and treatment methods. Come to us for preventive examinations and if you have possible signs of cervicitis, trust your health to experienced doctors.
Colposcopy
Colposcopic examination, first proposed in 1924 by H. Hinselmann, consists of examining the cervical mucosa using a binocular magnifier equipped with a lighting system and color filters. The improvement and development of devices and colposcopic technology has led to the emergence of many of its varieties:
- Simple colposcopy - examination of the vaginal part of the cervix using a colposcope;
- Extended colposcopy associated with the use of a 3% solution of acetic acid (when treated with it, spasm of the subepithelial vessels occurs and swelling of the mucosa, which promotes better visibility), as well as Lugol's solution (pathological areas, the epithelium of which is deprived of glycogen, do not turn brown, which allows you to determine the boundaries of the lesion).
Basic principles of treating a bleeding cervix
To choose a treatment method, doctors should determine why the cervix is bleeding. Various diagnostic methods are used for this. The most common solution is an ultrasound, examination in a gynecological chair, and a blood test for hormones. Each case will require its own group of drugs:
- If the cause of bleeding is infectious cervicitis, the gynecologist will prescribe antibiotics. Most often, women are advised to take Ceftriaxone, Erythromycin, Ofloxacin.
- For non-infectious inflammation - vaginal suppositories that have an antifungal, antiviral and antimicrobial effect, namely Diflucan, Terzhinan.
- In cases where bleeding is caused by erosion, modern methods of surgical intervention are used (cryodestruction, laser, radio wave exposure). At the same time, the following drugs are prescribed - Depantol, Hexicon.
- Polyps cannot be treated with medication; they cannot be reabsorbed. They need to be removed only mechanically. The operation is performed after menstruation; the patient should first take antibacterial drugs.
Sometimes women prefer traditional medicine rather than drug treatment. Herbs and mixtures can have a positive effect on the body and reduce symptoms, but they can only be used after consulting a doctor. Herbal medicine involves tamponing. A tampon is moistened in the prepared solutions and inserted into the vagina. For erosion, nettle juice is effective; for inflammation, flax or eucalyptus oil.
Diagnosis of bleeding from the cervix
Diagnosis of bleeding from the cervix includes:
- Carrying out an examination using special mirrors, with the help of which it will be possible to determine the size and shape of the cervix, the presence of deformation and tears, and the condition of the mucous membrane.
- Analysis of smears for flora and cancer cells, analysis for infections.
- Examination of the cervix using a colposcope. Dysplasia and early forms of cancer are characterized by changes that are not detectable during a routine examination, but they are detected using a colposcope. A colposcope makes it possible to examine the mucous membrane under multiple magnification, and samples - to find abnormalities and accurately collect material for cytological analysis.
- Cytological examination is often used as a method of instrumental diagnosis. During it, smears taken from the surface of the cervical canal are examined under a microscope for the presence of cancer cells. The analysis allows diagnosing cancer with up to 95% accuracy. Inflammatory processes in the cervix can create difficulties for cytologists when carrying out differential diagnosis. Cytology results due to inflammation may interfere with the detection of cancer cells if bacterial flora and leukocytes predominate in the material, and there are minimal or no epithelial cells. If inflammation is detected, you first need to eliminate it, and only then carry out a cytological analysis.
- An ultrasound examination will determine the presence of a cyst, fibroid, or tumor.
- Blood test for hormones.
[19], [20], [21], [22]
What do we have to do?
First of all, if a woman’s cervix begins to bleed, she needs to see a doctor to identify the causes and make a diagnosis. Depending on this, the doctor recommends/prescribes one or another treatment. The erosion needs to be cauterized. However, this is not recommended for those who have not given birth. For this, there are less radical traditional medicines:
- Sea buckthorn oil tampons.
- Aloe juice tampons.
- Spinning with herbs.
- Candles.
Polyps must be removed. Treat inflammation. The main thing is not to start the problem. Timely diagnosis means good health in the future.
Treatment
Transient bleeding from the cervix does not require treatment; it goes away on its own. Chronic diseases are subject to special treatment.
The tactics of the treatment approach differ for different pathologies. Before prescribing appropriate therapy, the gynecologist conducts a comprehensive examination.
Table. Treatment regimens for cervical diseases.
| Disease | Treatment tactics |
| Polyp | The bleeding polyp is removed through surgery. The operation is performed in a clinic setting. Anesthesia is used as a method of pain relief. The polyp is cut off from the mucous membrane, the damaged area is cauterized. A few hours later the woman is allowed to go home. |
| Erosion | For cervical erosion, treatment is carried out in several ways, depending on the severity of the pathological process. For minor erosion, medications are used - suppositories and vaginal gels containing panthenol. If the erosion is large, surgical treatment is used. Erosion is cauterized with a coagulator, laser, or cryodestruction is used |
| Cancer | Treatment of malignant tumors of the cervix is carried out jointly by gynecologists and oncologists. Treatment tactics depend on the stage of cancer. In most cases, surgery is used to remove the cervix and the entire uterus. After surgery, radiation therapy or chemotherapy is prescribed |
Emergency treatment is indicated if a woman’s cervix bleeds during pregnancy. In this case, the woman is taken to the gynecological department and the issue of maintaining or terminating the pregnancy is decided.
Menopausal bleeding due to dry mucous membranes is treated with replacement therapy. A woman is prescribed estrogen preparations in the form of tablets for oral administration or topical agents. With their constant use, the mucous membrane is restored and bleeding stops.
Treatment with folk remedies is symptomatic and does not replace the main therapy prescribed by a doctor. With the help of folk remedies it is impossible to cure a polyp, erosion, and even more so cancer. They are used to temporarily stop bleeding from the genital tract.
For this purpose, the following means are used:
- infusion of water pepper;
- nettle decoction;
- burnet decoction.
The drugs are taken orally. It is not recommended to use folk remedies in the form of baths or douches, as this contributes to even greater damage to the mucous membrane.
Prevention of cervical pathologies
Refusal of treatment may worsen the situation. The disease will progress, leading to problems conceiving a child and even the development of a malignant neoplasm.
To prevent the appearance of bloody discharge from the vagina and cervix, you must follow simple recommendations:
- systematically visit a doctor every six months;
- pay attention to genital hygiene;
- exclude mechanical injury;
- avoid unprotected sex, use contraceptives;
- keep a menstruation calendar, monitor the intensity and timing of discharge.
If you are attentive to your health and sensitive to alarming symptoms, you can avoid the appearance of serious pathologies and prolong the youth and health of the female body. Also for these purposes, it is recommended to review your diet, engage in moderate physical activity, and lead an active lifestyle.
Surgical manipulation, the essence of which is curettage (or scraping) of the functional layer of the uterine mucosa.
Curettage of the uterine cavity is a surgical procedure, the essence of which is to scrape out (or scrape off) the functional layer of the uterine mucosa. The term RDV (“separate diagnostic curettage”) is also used - it is called separate because it is carried out in stages - first the cervical canal is scraped, and then (a separate manipulation) - the uterus itself; It is called diagnostic because the resulting scraping will be sent for histological examination to establish an accurate diagnosis.
During the curettage process, only the top layer of the endometrium is removed, so the uterine mucosa is subsequently restored.
The scraped material is sent for histological examination. This eliminates the possibility that the disease is malignant. This is the main purpose of curettage performed for diagnostic purposes.
Decoding the results
Deciphering a smear for cytology allows us to draw conclusions about the degree of cleanliness of the vagina and the presence of pathologies in a woman.
In total there are 4 degrees of purity:
- First degree. Rarely seen. The smear reveals exclusively rod flora, a small amount of squamous epithelium and single leukocytes.
- Second degree. A common study finding found among healthy women. In the flora in the cytology smear there are squamous epithelial cells, single cocci and other non-pathogenic microorganisms.
- Third degree. This degree of purity means the initial stage of the inflammatory process. Detected inflammation in a cytology smear requires the start of other diagnostic studies to find the root cause of the problem. The smear contains polymorphic rod flora, neutrophilic leukocytes, granulocytes and glandular epithelium; in addition, the results of cytology of a smear from the cervical canal can reveal yeast fungi with a tendency to multiply and be active.
- Fourth degree. The inflammatory process is pronounced. Coccal and bacillary-coccal flora predominate. This research result requires an urgent search for the causative agent of infection and appropriate treatment.
READ MORE: Cytology interpretation of the analysis is normal
Doctors often talk about the fifth degree of purity, the result of which is a harbinger of an oncological process in the woman’s genital area, since in this case a large number of atypical cells are detected in the smear.
! See a doctor immediately if...!
- you very quickly stopped bleeding from the vagina and began to experience abdominal pain;
- your temperature has risen above 38°C;
- you have severe abdominal pain that does not go away after taking painkillers;
- you experience heavy vaginal bleeding that quickly fills your sanitary pads and does not stop for several hours;
- you have copious, foul-smelling vaginal discharge;
- your health suddenly deteriorates, you feel dizzy, weak or lost consciousness.
Distinctive symptoms of bleeding during cervical erosion
The following characteristic signs will help to suspect pathology:
- Bloody discharge is weak, spotting, moderate;
- The color of the discharge is scarlet, brown, pale pink;
- Bloody discharge can almost always be associated with one or another effect on the cervix (sex, gynecological examination, use of tampons, etc.);
- Bleeding occurs outside of the menstrual cycle;
- The discharge stops on its own within a few hours;
- Pain is not typical, itching and burning are absent.
The picture shows the characteristic features of discharge in the presence of erosion.
For your information
Cervical erosion is not capable of causing heavy and prolonged bleeding. Severe bleeding in diseases of the cervix may be associated with pathology of the blood coagulation system, and also indicate malignant degeneration.
Typical bleeding from erosion can be seen by the appearance of brown or scarlet spots on the laundry. In such a situation, regular panty liners are sufficient; no additional measures are required. If the bleeding does not stop or gets worse during the day, you should see a doctor as soon as possible.
It is also useful to read: Cryotherapy for cervical pathologies (including erosion)
Preparation for the procedure
- Examination and consultation with a gynecologist.
- General blood analysis.
- Coagulogram (assessment of the blood coagulation system).
- ECG.
- Tests for hepatitis B and C, RW (syphilis) and HIV.
- Vaginal smear (there should be no signs of inflammation).
2 weeks before your curettage: Stop taking any medications or dietary supplements (including herbal supplements) that you have not previously discussed with your doctor who will be performing the curettage. Some medications can change blood clotting and increase the risk of bleeding. If you are taking medications for a serious illness (for example, hypertension, arrhythmia, epilepsy), do not stop treatment, but be sure to tell your doctor about the medications you are taking.
2-3 days before curettage:
- Avoid sexual intercourse.
- Do not douche and refuse to use any intimate hygiene products. To toilet the genitals, use only warm water.
- Stop using any medications in the form of vaginal suppositories, tablets, or sprays unless their use has been discussed with your doctor in advance.
- On the eve of curettage, refrain from eating and drinking 8-12 hours before the procedure. This is necessary for safe anesthesia.
Diagnostic curettage is performed before menstruation, a few days before its onset.