History of blood transfusion
Since 1926, the National Medical Research Center for Hematology has been operating in Moscow, which is the country's leading scientific center. And the first attempts at donation were recorded in ancient times. But the results were unsuccessful in most cases. There are two reasons:
- At that time it was still impossible to establish the blood type and Rh factor.
- The doctors did not have the necessary equipment and knowledge about transfusiology.
If incompatible blood is transfused, the patient will die. Therefore, now practically no whole blood is administered, but only its components. And this method is safer.
What is the difference between a blood donor and a plasma donor?
As you can see, the process of donating blood plasma is completely different from regular blood donation. A typical blood donation takes about 10 minutes, while plasma donors must be connected to a special machine for 40 minutes.
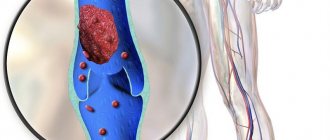
In addition, donating blood plasma may be more dangerous for humans . If plasma is collected using automatic plasmapheresis, it is important that additional substances are introduced into the blood throughout the procedure to reduce its clotting. Plasma contains a lot of platelets, which are responsible for clotting, and if a large number of them are removed at once, the blood can clot - large accumulations of it form in the vessels, and a person’s blood circulation may be impaired.
Therefore, they usually pay more money than for regular blood donation. In Moscow, for every 150 ml of plasma they now pay 1,250 rubles , for 600 ml - 5,000 rubles . For a typical donation of 600 ml of blood they pay less, about 3,600 rubles .
A person can only receive plasma transfusion from a person with the same blood type as him. You can't mix them.
What are the risks for recipients?
The plasma transfusion technique is similar to administering medications through an IV. But here everything is more complicated. This manipulation is the same as living tissue transplantation. The composition of blood includes various components of cells, the harm of which is:
- Molecules.
- Squirrels.
- Foreign antibodies.
Even perfectly matched donor cells are not identical to those of the patient. Therefore, there is a possibility of rejection. And the doctor is responsible for the consequences of a transfusion. Therefore, he must calculate the probability of rejection in advance.
Any intervention is a risk, and the chance of success does not always depend on the correct training and qualifications of the doctor. And during a transfusion, a superficial attitude of medical personnel to work is not allowed. You also can’t rush, and you need to have a certain amount of knowledge. First of all, the doctor must check any other methods. And plasma transfusion is carried out only if it cannot be avoided. And if the patient has contraindications, transfusion is prohibited altogether.
Plasma transfusion - in what cases is it prescribed and how does it happen?
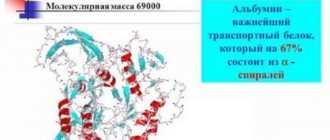
Plasma is a liquid component of blood, rich in biologically active components: proteins, lipids, hormones, enzymes.
Freshly frozen plasmatic fluid is considered the best product due to the fact that it retains the largest number of useful components.
Whereas liquid native, dry lyophilized and antihemophilic plasma somewhat loses the healing characteristics inherent in this component, so they are less in demand.
Blood plasma: why is it transfused?
Transfusion of any type of blood plasma allows you to restore the normal volume of blood circulating in the body, the balance between hydrostatic and colloid-oncotic pressure.
A positive effect from this kind of procedure becomes possible due to the fact that the molecular weight of plasma proteins and the molecular weight of the recipient’s blood are different. In view of this, the permeability of the vessel walls is low, and nutrients are not absorbed; they remain in the bloodstream for a long time.
If a person has acute bleeding, intravenous plasma transfusion is given in a dose of 0.5 l to 2 l. In this case, everything depends on the patient’s blood pressure and the complexity of his disease. In particularly severe situations, it is recommended to combine plasma and red blood cell infusions.
Plasma is infused in a stream or drop, depending on the indications. If microcirculation is impaired, rheopolyglucin or other drugs of this group are added to the plasma.
Terms: Hemotransfusion is an intravascular transfusion of whole blood to a recipient. In fact, it is a complex operation involving the transplantation of living tissue to a person.
Blood plasma transfusion: indications
The RLS pharmacological reference book dictates the following indications for transfusion of fresh frozen blood plasma:
- Acute DIC syndrome, which simultaneously complicates the course of shock of various origins, massive transfusion syndrome,
- Severe bleeding, which involves the loss of more than a third of the total blood volume. In this case, a further complication is possible in the form of the same disseminated intravascular coagulation syndrome,
- Pathological changes in the liver and kidneys (conditional indications),
- Overdose of anticoagulants, for example, dicoumarin,
- During a therapeutic plasmapheresis procedure caused by Moschkowitz syndrome, acute poisoning, sepsis,
- Thrombocytopenic purpura,
- Open heart surgery with connection to a heart-lung machine,
- Coagulopathies arising from low concentrations of physiological anticoagulants, etc.
We have reviewed the most common indications for transfusion of fresh frozen plasma. It is not recommended to perform such a procedure to replenish the entire volume of circulating blood. In this case, other methods are used. Plasma transfusions are not prescribed for patients suffering from congestive heart failure.
Fresh frozen blood plasma
Fresh frozen plasma is considered one of the basic components of blood; it is created by rapid freezing after separation of its formed elements. This substance is stored in special plastic containers.
The main disadvantages of using this biomaterial:
- risk of transmitting an infectious disease,
- risk of allergic reactions,
- conflict between the biomaterial of the donor and the recipient (a biological test for compatibility is required before transfusion).
Fresh frozen plasma is produced using two methods:
- plasmapheresis,
- centrifugation.
Plasma is frozen at -20 degrees. It can be used for a year. Only during this time is the preservation of labile factors of the hemostasis system ensured. After the expiration date, plasma is disposed of as biological waste.
Terms: Hemostasis is a system in the human body whose main task is to stop bleeding and dissolve blood clots while maintaining the liquid state of blood in the vessels.
Immediately before the plasma infusion itself, the blood is thawed at a temperature of + 38 degrees. At the same time, fibrin flakes fall out.
This is not a problem, since they will not interfere with the normal flow of blood through plasticizers with filters. Whereas large clots and turbidity of the plasma indicate a low-quality product.
And for doctors, this is a contraindication for its further use, although laboratory assistants may not have identified defects when donating blood and testing.
Important! Due to the fact that such a product can be stored for a long time, doctors try to adhere to the rule of one donor - one recipient.
Plasma proteins are immunogenic. This means that with frequent and large transfusions, the recipient may develop sensitization. This can lead to anaphylactic shock during the next procedure.
This circumstance leads to the fact that doctors try to transfuse plasma according to strict indications. When treating coagulopathies, it is preferable to use cryoprecipate (a protein preparation containing blood clotting factors.
which a person lacks).
When using biomaterial, it is important to follow strict rules: you cannot use the same plasma container for transfusion to several recipients. It is not allowed to re-freeze blood plasma!
Blood plasma transfusion: consequences
Practice shows that most often complications and problems are not expected after blood plasma transfusion. If we look at research, this is less than one percent out of a hundred. However, side effects can cause significant disruptions in the functioning of the entire body and even death.
In view of the fact that blood transfusion with a plasma substitute (plasma) does not provide 100% safety, patients are initially required to consent to such a procedure, making sure to inform them of all the positive aspects, effectiveness and possible alternatives to transfusion.
- Any clinic where plasma transfusions are performed should be equipped with a system that makes it possible to quickly identify and treat side effects that threaten a person’s life. Current federal regulations and guidelines require consistent reporting of such incidents, such as accidents and medical errors.
Acute Adverse Effects
Immunological acute adverse effects include the following:
- Febrile reaction to transfusion. In this case, fever occurs most often. If such a reaction accompanies incompatibility between the blood of the donor and the recipient (hemolysis), then the transfusion must be stopped immediately. If this is a non-hemolytic reaction, then it is not dangerous to human life. This reaction is often accompanied by headache, itching and other manifestations of allergies. Treated with acetaminophen.
- Urticarial rash makes itself felt immediately after plasma transfusion. This is a very common phenomenon, the mechanism of which is closely related to the release of histamine. Most often, doctors in this case write a prescription for the use of the drug Benadryl. And as soon as the rash disappears, we can say that the reaction is over.
- Literally two to three hours after blood plasma transfusion, respiratory distress syndrome, decreased hemoglobin and hypotension may suddenly appear. This indicates the development of acute lung injury. In this case, prompt intervention by doctors is required to organize respiratory support with mechanical ventilation. But there is no need to worry too much; studies have shown that death from this effect occurs in less than ten percent of recipients. The main thing is for the medical staff to get their bearings in a timely manner.
- Acute hemolysis occurs due to inconsistency in the identification of the recipient's blood plasma, in other words, due to personnel error. The complexity of this effect lies in the fact that clinical indications may remain unexpressed, accompanied exclusively by anemia (delayed hemolysis). Whereas complications occur in the case of concomitant aggravating factors: acute renal failure, shock, arterial hypotension, poor blood clotting.
Important! If a person is under anesthesia or has fallen into a coma, a sign of hemolysis is internal bleeding for unknown reasons from the injection site.
In this case, doctors will definitely use active hydration and prescribe vasoactive drugs.
- Anaphylaxis most often makes itself felt in the first minute of a blood transfusion. Clinical picture: respiratory distress, shock, hypotension, edema. This is a very dangerous phenomenon that requires emergency intervention from specialists. Here everything needs to be done to support a person’s respiratory function, including administering adrenaline, so all drugs must be at hand.
Non-immunological complications include:
- Volume overload (hypervolemia). If the volume of transfused plasma is incorrectly calculated, the load on the heart increases. The volume of intravascular fluid increases unnecessarily. Treated with diuretics.
Symptoms of hypervolemia: severe shortness of breath, hypertension and even tachycardia. Most often it manifests itself six hours after a blood plasma transfusion.
Chemical effects include: citrate intoxication, hypothermia, hyperkalemia, coagulopathy, etc.
What is the blood plasma transfusion technique?
Indications for transfusion of blood plasma and all its physiological components are determined exclusively by the attending physician on the basis of previously conducted laboratory, physical and instrumental studies.
It is important to understand that there is no standard and established scheme for the treatment and diagnosis of diseases in this case. For each person, the consequences and the transfusion itself proceed individually, depending on the body’s reaction to what is happening.
In any case, this is a significant burden on him.
Frequently asked questions regarding various blood transfusion techniques can be found in the guidelines.
What is indirect and direct blood transfusion?
Indirect blood transfusion is used most often. It is administered directly into a vein using a disposable bottle with a filter. In this case, the technology for filling a disposable system must be described in the manufacturer’s instructions.
In medical practice, other ways of introducing plasma are used: not only into a vein, but also intra-arterially, intra-aortically and intraosseously.
It all depends on what result you want to achieve, and whether it is even possible to provide plasma transfusion.
Direct blood transfusion does not imply its stabilization and preservation. In this case, the procedure is performed directly from the donor to the recipient. In this case, only whole blood transfusion is possible. Blood can only be administered intravenously; no other options are suggested.
But direct blood transfusion is performed without the use of filters. This means that the patient faces a high risk of getting a blood clot that formed during the procedure. Consequently, thromboembolism may develop.
That is why direct blood transfusion is performed only in emergency cases. And medical personnel resort to this type of procedure extremely rarely. In such a situation, it is better to resort to a transfusion of freshly prepared warm blood. This reduces the risk of contracting a serious disease, and the effect will be even better.
Loading…
Source: https://dlja-pohudenija.ru/serdcze/analiz-krovi/osobennosti-perelivaniya-plazmy-i-pokazaniya-k-proczedure
In what cases is transfusion necessary?
Manipulation has a specific purpose. Most often, donor material is needed to replenish blood reserves in case of large blood loss. Blood transfusion is also an effective way to increase platelet counts if a person suffers from poor clotting. There are certain indications for manipulation:
- Severe anemia.
- Life-threatening blood loss.
- State of shock.
Surgical intervention is required, in which there is a possibility of large blood loss or devices that create artificial circulation will be used (for example, vascular surgery, heart surgery).
But also the cause of transfusion can be:
- Poisoning the body with chemicals.
- Sepsis.
- Diseases associated with blood.
Oncology clinic in Moscow
Oncology clinic in Moscow ¦ BLOOD TRANSFUSION FOR CANCER PATIENTS ¦ Plasma transfusion
Transfusion of blood and its components
Transfusion of blood and its components is most often carried out in very severe diseases, when it is necessary to compensate for the lost volume of blood or the deficiency of any of its fractions, including formed elements and proteins.
Until now, under the blood is an effective remedy that cannot be replaced by anything, since there are no medicinal analogues that can duplicate its functions, at least partially.
For this reason, every large hospital has a supply of donor blood and its individual components, which are used according to appropriate indications.
Blood transfusion at the European Clinic
In the European Clinic of Surgery and Oncology, transfusions of blood and its individual components occur quite often, since there are patients with severe somatic and oncological pathologies and their condition requires replacement of the volume of blood and its formed elements.
Very often there are situations when there are no other alternatives and a transfusion can not only save a life, but also quickly improve the patient’s well-being.
The combination of traditional and advanced methods of influencing pathology allows doctors at the European Clinic to achieve excellent results in treating patients and improving their general condition.
| European Oncology Clinic Request for consultation and treatment +7(925)191-50-55 Moscow, Dukhovskoy lane, 22b |
Blood plasma
Plasma is obtained from whole blood by centrifugation or plasmapheresis, which removes the formed elements of blood: red blood cells, white blood cells, platelets.
The difference between plasma and serum is that plasma contains the anticoagulant sodium citrate, which prevents the formation of fibrin clot and the loss of certain proteins.
Naturally, plasma, unlike serum, contains fibrin, antihemophilic globulin and other factors.
Blood plasma is often used for diagnostic purposes, for example, in bacteriological studies to test microbial coagulase, or in determining the clotting ability of blood to initiate thrombus formation.
From the same volume of blood, different volumes of plasma and serum are obtained: the plasma content is approximately 10% higher than the serum due to the fact that the process of fibrin formation binds part of the fluid.
How is blood plasma used?
Blood plasma is used for transfusions for various pathological conditions. It contains a large amount of nutrients, coagulation factors, elements of the anticoagulant system, enzymes, hormones, immunoglobulins, antibodies and other components.
Doctors prefer to use frozen plasma rather than lyophilized or native plasma.
During storage and lyophilization, the breakdown of proteins is much more intense than during freezing, which makes the plasma not so effective, because some of the active components no longer work.
Frozen plasma is stored for a year at -45ºС, after which it is disposed of as biological waste.
If there is a need for plasma transfusion, it is carefully thawed and warmed to +38ºС.
In this case, fibrin flakes may fall out. If they are not very large, then they are not paid attention to, since there are filters in the plasma transfusion system. If large flakes or films are formed, then such plasma is disposed of.
An important role in the choice of plasma for transfusion is played by the antigenic compatibility of the donor material with the recipient's body.
Antibodies can destroy red blood cells, and, in addition, plasma proteins are quite immunogenic and can provoke anaphylactic shock, which, as a rule, manifests itself in the first minutes of plasma transfusion.
Indications for plasma transfusion
Disseminated intravascular coagulation is an indication for plasma transfusion. With this disease, generalized activation of the coagulation system occurs as a result of the release of a large amount of thromboplastin into the bloodstream.
As a result of this process, the proteins of the coagulation system are depleted and numerous hemorrhages and a tendency to bleed are observed; in severe cases, hypotension and a state of shock develop.
Plasma transfusion allows one to replenish coagulation factors, as well as normalize the content of anti-coagulation proteins.
In general, normal plasma restores the disturbed hemostatic balance. In case of chronic disseminated vascular coagulation, plasma is supplemented with substances that prevent coagulation.
Blood plasma is often used for acute blood loss, and its volume makes up about a third of all infusion solutions.
The value of plasma is to maintain normal oncotic pressure inside the vessels and counteract hydrostatic pressure. In addition, the blood plasma contains iron transport proteins (transferrin, ferritin), which help restore hemoglobin levels.
With serious liver diseases and the development of liver failure, the content of coagulation factors and other proteins synthesized in this organ drops sharply, which provokes bleeding, hemorrhages, and hematomas.
To avoid major complications, the lack of these factors is compensated for by blood plasma components.
For blood clotting disorders of various etiologies, plasma transfusions can be used. Sometimes the cause is coagulopathy, dicoumarin overdose, or thrombocytopenic purpura. In all these cases, plasma proteins help restore physiological hemostasis.
Complications and contraindications for plasma transfusion
Despite the fact that all donor material is tested for major infectious agents, sometimes a complication of plasma transfusion can be bacterial or viral infection.
For example, if the recipient’s body did not have the Epstein-Barr virus, then transfusion of components with this virus can provoke infectious mononucleosis.
In cases of heart failure (for example, after a myocardial infarction), plasma transfusion can lead to an increase in circulating blood volume and increased workload on the heart. For this reason, these patients are given plasma slowly under cardiac monitoring.
If the plasma contains high titers of anti-erythrocyte antibodies, its administration can provoke hemolysis of red blood cells and kidney problems. The development of anaphylactic shock is possible, since plasma proteins can be immunogenic for the recipient's body.
Immediately after the transfusion, a skin rash, as a reaction to increased histamine levels, and a fever are likely to occur. The latter can be provoked, among other things, by hemolysis of red blood cells and then the transfusion is stopped.
A severe complication of plasma transfusion is respiratory distress syndrome, in which blood pressure and hemoglobin drop: this indicates damage to the lung tissue and requires resuscitation measures and artificial ventilation.
Despite the dangers that blood and plasma transfusions pose, the potential benefits for human health and life in certain conditions are very great and can literally snatch the patient from the clutches of death.
Strict adherence to indications and identification of contraindications, compliance with instructions and professional standards allows you to minimize the risks associated with this procedure.
| European Oncology Clinic Request for consultation and treatment +7(925)191-50-55 Moscow, Dukhovskoy lane, 22b |
| Indications for blood transfusion |
| Plasma transfusion |
| Red blood cell transfusion |
| Platelet transfusion |
| Leukocyte transfusion |
+7(925)191-50-55 — European treatment protocols in Moscow
REQUEST TO THE CLINIC
Transfusion for children
Blood transfusion has no age restrictions. If necessary, manipulation can also be prescribed for newborns. The indications for transfusion for children are the same. Blood transfusion is an excellent solution if a dangerous disease progresses rapidly. Transfusion in newborns can be caused by the following reasons:
- Jaundice.
- The liver or spleen is enlarged.
- It is necessary to increase the number of red blood cells.
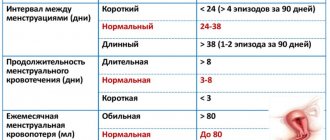
The main argument for carrying out the manipulation is the bilirubin level. For example, if in a child it exceeds 50 µmol/l (umbilical cord materials are taken for testing), it is necessary to carefully monitor the child, since this is considered a violation. You may need donor material in the future. But not only the bilirubin level itself plays a key role, but also how quickly it accumulates. If it is higher than normal, blood transfusion is necessary.
10.3. Features of leukocyte concentrate transfusion
Leukocytes are transfused, if possible, immediately, but no later than 24 hours after receipt. To achieve a therapeutic effect, leukocyte transfusions must be daily, for at least 4-6 days in a row, provided there is no restoration of granulocytopoiesis or adverse reactions. The leukocyte concentrate is transfused through a conventional device for intravenous transfusion of blood and its components with a filter.
Pre-transfusion testing of leukocyte concentrate is similar to that for blood gas carrier transfusions. Compatibility with ABO and Rh systems is required. Histoleukocyte antigen (HLA) matching provides a better response to transfusion, especially in patients with identified HLA antibodies.
When should you not give a blood transfusion?
Preparation is an important stage of manipulation. There are some restrictions when blood transfusion becomes prohibited. For example:
- Myocardial infarction.
- Coronary heart disease.
- Heart failure.
- Congenital heart defect.
- Problems with cerebral circulation.
- Bacterial endocarditis.
- Pulmonary edema.
- Hypertension.
- Thromboembolic syndrome.
- Exacerbation of glomerulonephritis.
- Liver or kidney failure.
- Asthma.
- Allergy to many irritants.
But sometimes transfusion of plasma to a patient is the only possible way to save the patient, so some contraindications may not be taken into account. But first it is necessary to check the compatibility of the tissues of the donor and recipient, so a number of tests are taken. Diagnostics are also carried out before plasma transfusion.
Fresh frozen blood plasma
Fresh frozen plasma is considered one of the basic components of blood; it is created by rapid freezing after separation of its formed elements. This substance is stored in special plastic containers.
The main disadvantages of using this biomaterial:
- risk of transmitting an infectious disease,
- risk of allergic reactions,
- conflict between the biomaterial of the donor and the recipient (a biological test for compatibility is required before transfusion).
Fresh frozen plasma is produced using two methods:
- plasmapheresis,
- centrifugation.
Plasma is frozen at -20 degrees. It can be used for a year. Only during this time is the preservation of labile factors of the hemostasis system ensured. After the expiration date, plasma is disposed of as biological waste.
Terms: Hemostasis is a system in the human body whose main task is to stop bleeding and dissolve blood clots while maintaining the liquid state of blood in the vessels.
Immediately before the plasma infusion itself, the blood is thawed at a temperature of + 38 degrees. At the same time, fibrin flakes fall out. This is not a problem, since they will not interfere with the normal flow of blood through plasticizers with filters. Whereas large clots and turbidity of the plasma indicate a low-quality product. And for doctors, this is a contraindication for its further use, although laboratory assistants may not have identified defects when donating blood and testing.
Important! Due to the fact that such a product can be stored for a long time, doctors try to adhere to the rule of one donor - one recipient.
Plasma proteins are immunogenic. This means that with frequent and large transfusions, the recipient may develop sensitization. This can lead to anaphylactic shock during the next procedure. This circumstance leads to the fact that doctors try to transfuse plasma according to strict indications. When treating coagulopathies, it is preferable to use cryoprecipate (a protein drug containing blood clotting factors that a person lacks).
When using biomaterial, it is important to follow strict rules: you cannot use the same plasma container for transfusion to several recipients. It is not allowed to re-freeze blood plasma!
Donated blood for people with allergies
If a person often experiences allergic reactions, there are some rules for transfusion. First, it is necessary to carry out desensitizing therapy. To do this, the following drugs are administered intravenously:
- Suprastin.
- Calcium chloride.
- Pipolfen.
The drugs are antihistamines, but in many cases hormonal drugs are also needed. To test for allergies to donor biomaterial, a small amount of material is injected into the patient. The emphasis is not on quantity, but on the quality of blood. Only those substances that are necessary for the patient are retained in the plasma. And the volume of fluid can be replenished using blood substitutes.
Can blood plasma transfusion cure coronavirus?
Typically, vaccination involves the introduction into the body of weakened or killed microorganisms (viruses) intended to create stable immunity to possible future infectious diseases - that is, to release antibodies.
But what to do if a vaccine has not yet been developed for a particular virus? Yes, we are talking about coronavirus now. In this case, scientists have developed a treatment method called blood plasma transfusion.
To do this, plasma is taken from those people who have already had coronavirus, and then transfused into patients to produce antibodies against this infection. How does it work, and why does blood plasma have such miraculous properties?
Blood plasma is the key to treating many diseases
What is human blood plasma
Plasma is the liquid part of the blood; it consists of 90% water, as well as proteins, fats, carbohydrates, vitamins and clotting substances.
Scientifically speaking, plasma is the intercellular substance of the liquid tissue of blood.
To obtain it, healthcare workers use special equipment that separates the plasma from other blood particles, including red blood cells. Therefore, plasma is not red like blood, but has a yellowish tint.
The plasma separated from the red blood cells is subsequently used for transfusion, and the red blood cells are returned to the donor. This process is called plasmapheresis.
Blood plasma (yellow) has separated from red blood cells and other particles (red). The yellow part is transfused to the patient, the red part is returned to the donor
Plasma is used to treat many viruses, including coronavirus
Suppose a person became infected with coronavirus, and his immunity turned out to be so strong that he was able to overcome the infection (with the help of medications).
The virus was defeated due to the fact that the immune system released many antibodies SPECIFICALLY against this infection.
Antibodies already know what to do with a virus of this type, and if the person gets sick again (if there is one), the person will be able to overcome the coronavirus faster.
To help other people with less strong immunity, blood plasma is taken has had coronavirus
This plasma, as we remember, contains various substances, platelets for healing and... the very antibodies that the donor’s immunity developed. After entering the body of a sick person, antibodies begin to kill the coronavirus , since they have already had such experience.
Simply put, more experienced reinforcements in the form of special forces came to the aid of the “soldiers” of the patient’s body.
https://www.youtube.com/watch?v=7-OooQyN7bQ
Due to the fact that the patient himself also produces antibodies to this virus, albeit more slowly, through joint efforts they manage to defeat the infection. In fact, human blood plasma is the very vaccine that helps in the fight against coronavirus. But there is very little of it, since not everyone wants to become plasma donors .
The first people to think about plasma transfusions were South Korea, where the COVID-19 outbreak occurred shortly after China. Back in February 2020, the first trials of treating coronavirus with blood plasma transfusions were conducted there, and they were completed successfully. The patients have recovered. Together with quarantine measures in the country, it was possible to suppress the epidemic of a dangerous virus.
To better understand the benefits of plasma transfusion, read what happens in the body when it is attacked by coronavirus.
Not long ago, other countries, including Russia, began to adopt this practice. In Moscow, points have already been set up to donate blood plasma, which is taken from those who have already recovered from coronavirus.
They pay money for this, but it seems to me that the feeling that by doing this you may be saving someone’s life is much more valuable. Share in our Telegram chat whether you would become a plasma donor and why.
At the time of writing this article, 3 people in Moscow have recovered from coronavirus thanks to blood plasma transfusions.
How is blood plasma obtained?
To obtain it, blood plasma donors . Previously, blood was spun in a centrifuge at high speeds, as a result of which only 250-300 ml of plasma was obtained from 500 ml of blood collected. This method is not the most effective, since in this case it is impossible to return red blood cells and some other useful substances back to the donor.
A centrifuge in which the blood is accelerated, and the plasma itself is released to the top, and the red blood cells remain in the sediment
And scientists have developed a method of automatic plasmapheresis , which is now widely used in medicine. Donating blood plasma takes about 40 minutes .
- First, blood is drawn from the donor;
- Then, using a special device (“bell”), the plasma is separated. From 350 ml of blood, 230 ml of blood plasma is obtained;
- The cellular components of the blood, including red blood cells, are returned to the collection device and returned to the donor. In essence, a reverse blood transfusion occurs, but without plasma;
- To compensate for the donor's fluid loss, he is additionally injected with a portion of saline solution.
A machine that separates plasma from the blood and returns red blood cells to the donor
Plasma obtained from blood is frozen at –30 °C for 1 hour. Otherwise, it will lose its properties.
What is the difference between a blood donor and a plasma donor?
As you can see, the process of donating blood plasma is completely different from regular blood donation. A typical blood donation takes about 10 minutes, while plasma donors must be connected to a special machine for 40 minutes.
In addition, donating blood plasma may be more dangerous for humans .
If plasma is collected using automatic plasmapheresis, it is important that additional substances are introduced into the blood throughout the procedure to reduce its clotting.
Plasma contains a lot of platelets, which are responsible for clotting, and if a large number of them are removed at once, the blood can clot - large accumulations of it form in the vessels, and a person’s blood circulation may be impaired.
Therefore, they usually pay more money than for regular blood donation. In Moscow, for every 150 ml of plasma they now pay 1,250 rubles , for 600 ml - 5,000 rubles . For a typical donation of 600 ml of blood they pay less, about 3,600 rubles .
A person can only receive plasma transfusion from a person with the same blood type as him. You can't mix them.
Why is blood plasma transfused?
In fact, plasma is mostly transfused not to fight coronavirus (this is only now the case), but for blood clotting disorders or if a person has lost too much blood.
In this case, a loading dose of platelets will help not only restore coagulation, but also help to heal even serious wounds faster.
Plasma transfusion is much more effective than whole blood transfusion, since only those substances that are necessary can be sent to a person.
In addition, blood plasma is used to create medicines. Many tablets contain it, including those prescribed for the treatment of immune deficiency, neurological, infectious and autoimmune diseases, heart failure and others. Every year, doctors are finding new possibilities for using plasma.
Collected blood plasma is stored for 3 years at temperatures below –30 °C.
Ideas that blood has almost magical properties existed at the dawn of modern society. Therefore, some experiments in this area are still ongoing, and, as we see, they are very successful.
Source: https://Hi-News.ru/eto-interesno/mozhet-li-perelivanie-plazmy-krovi-vylechit-koronavirus.html
Biomaterials for transfusion
- For transfusion can be used:
- Whole blood (rarely used).
- Red blood cells with a minimal number of platelets and leukocytes.
- Platelets (they can be stored for no more than 3 days).
- Fresh frozen plasma transfusion. It is suitable for burns, tetanus or staphylococcal infections.
- Components necessary to improve clotting.
Whole blood is rarely administered because so much biological material is needed and the risk of rejection is very high. And in most cases, the patient only needs the missing components, so there is no point in transplanting foreign cells into him. Whole blood may be suitable for heart surgery or if severe blood loss has occurred.
There are also several methods of transfusion:
- Replenishment of necessary blood components by administering them intravenously.
- Exchange transfusion. When part of the patient's blood needs to be replaced with donor materials. This method is suitable for renal failure, intoxication or hemolysis. Most often, fresh frozen plasma is used as the material.
- Autohemotransfusion. This method involves injecting the patient with his own blood. Fluid can be collected if there is bleeding. It is cleaned and stored. This method of transfusion is relevant if the blood type is rare and it is impossible to find a donor.
How to donate plasma for coronavirus patients
Convalescent plasma is not yet widely available. In many cities of Russia they are starting to collect it. The first procurement centers were organized in Moscow, after the release of the order of the Department of Health No. 325 of 04/01/2020. According to this order, the chief doctors of hospitals where care is provided to patients with COVID-19 are required to provide information about convalescents who could become donors. They are interviewed and invited to visit a plasma collection point no earlier than 2 weeks after discharge.
The donor movement is expanding throughout Russia. The Chelyabinsk Regional Blood Transfusion Station began collecting blood from convalescent donors in May 2020. The Adyghe Republican Blood Transfusion Station also invites those who have recovered and are ready to become donors. The Clinical Hospital on Yauza (Moscow) offers to donate blood.
The resulting plasma can be used by the donor himself in case of re-infection - its shelf life is 2 years. Phone numbers of reception points in different cities of Russia can be found on the Internet.
There are many more requests from clinics than there is prepared plasma, since there are not enough donors. One dose can help a small number of patients, but during an epidemic, plasma from several hundred thousand donors is needed. Organizing a collection during strict self-isolation is not easy, and not every convalescent can be encouraged to donate.
Where to donate blood plasma after coronavirus?
The place to donate blood is the nearest blood transfusion station .
If we talk about Moscow, work on the preparation and storage of fresh frozen plasma from convalescent donors is carried out at the Blood Center named after. OK. Gavrilov and the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky.
In Minsk, in addition to blood transfusion stations, the Republican Scientific and Practical Center for Transfusiology collects plasma.
Anyone who has been ill and wants to donate blood should contact these institutions.
How to donate plasma for coronavirus
Plasma is collected by plasmapheresis , in which whole blood is separated into plasma and cellular blood elements. Blood is taken from the donor so that it does not clot and is stable; an anticoagulant . The device separates plasma from cellular components, which are returned to the donor’s bloodstream.
The process lasts 30-40 minutes, during which time the donor donates 650 ml of plasma. If the procedure is poorly tolerated, the amount is reduced to 400 ml. At the end of the procedure, the volume of the collected plasma is replenished with a colloidal solution. After completion of the procedure, the donor is provided with breakfast and is observed for 30-40 minutes, after which he can be free. It is mandatory to measure blood pressure during and after the procedure, an ECG is performed and blood oxygen saturation is determined.
Undesirable reactions are possible during the procedure, but they are rare:
- When inserting a venous catheter, bleeding sometimes occurs.
- There may be a decrease in calcium levels in the donor's blood, which can cause muscle spasms and heart rhythm disturbances . This is due to the fact that the collected donor blood is treated with a citrate anticoagulant to prevent clotting in the machine system. The cellular elements returned to the donor also contain an anticoagulant, which can slightly reduce calcium levels.
- After replenishing the donor's plasma with a colloidal solution, blood clotting factors and immunoglobulins are slightly reduced.
Plasma taken from a donor after testing and processing (a process called pathogen reduction , which is carried out with Methylene blue , ultraviolet irradiation, Riboflavin or amotosalen ) can be urgently transferred within a day without freezing to the clinic that made the request. If this is not necessary, it is frozen and issued upon request as planned. All doses are stored in freezers, transported in compliance with the rules, and before use they are thawed in centers and hospitals using special equipment.
Requirements for plasma donors during coronavirus
According to Order No. 325 of Moscow, a person who meets the following requirements can become a plasma donor for the treatment of coronavirus:
- Previous COVID-19 disease of mild or moderate severity, the fact of which must be confirmed by discharge from the hospital.
- Complete recovery 14 days or more before donation. This is confirmed by negative results of nasopharyngeal swabs or PCR. You need to undergo PCR diagnostics twice and get a negative result.
- A certain level of SARS-CoV-2 neutralizing antibody titers is greater than 1:320.
- Negative tests for HIV and hepatitis .
- Normal biochemical and clinical blood test .
- Age over 18 years.
- No ARVI at the time of blood donation.
- Weight not less than 50 kg.
- There are no general contraindications to blood collection.
On the day of delivery, rapid testing for immunoglobulins M and G to the SARS-CoV-2 virus. This is important for assessing the level of neutralizing antibodies, since not every person who has recovered has a sufficient level of antibodies to become a donor.
Many people have a question: are payments to donors made and in what amount? The Moscow Department of Health announced payments: for every 150 ml the payment is 1,250 rubles, and if the donor donated 600 ml, 5,000 rubles are paid.