Blood pressure indicators are considered the main ones in determining the quality of the cardiovascular system as a whole. Heart rate is equally assessed. With a more in-depth analysis, the doctor is able to characterize the patient’s general health condition and predict risks.
Blood pressure 160/90 mm Hg. Art. in adults this is a borderline indicator. It is certainly considered pathological, since the norm is set at 139 to 89, this is the possible maximum. The question is to determine the degree of development of the process.
In this case we are talking about the second stage of hypertension. Although diastolic (lower) values in the range of 100-110 are typical for it, the assessment, as a general rule, is based on a higher number. That is, by systolic (upper) pressure.
Arterial hypertension of the second degree is already considered developed: the risks of complications, as well as further progression, are high. The prognosis is serious. The outcome can be discussed taking into account the risk (there are 4 forms of such an indicator).
Treatment is carried out under the supervision of a cardiologist throughout life.
Causes
The factors that provoke a gradual or sharp increase in tonometer readings are varied. You need to understand it within the framework of diagnostics.
Physiological
Relatively rare. The duration of the attack (relatively speaking) is determined by the action of the provoking factor.
There are no symptoms at all; slight dizziness or tachycardia is possible. The condition is not dangerous, except in exceptional cases.
Reasons for the development of physiological increases in blood pressure:
- Puberty. Adolescents 12-19 years old suffer from secondary hypertension in approximately 30% of cases. Individual episodes occur in more young people.
The development factor is hormonal changes. Induced juvenile hypertension is unstable.
The tonometer readings can change several times during the day. The blood pressure level can rise above 160 to 90, this is already dangerous.
Despite the naturalness of the changes, their transient nature, you should be regularly monitored by a cardiologist to prevent complications.
- Pregnancy. During gestation, an increase in blood pressure may indicate both a variant of the physiological norm and late toxicosis (eclampsia).
The second is much more dangerous, since 160 to 90 in a woman is the preparatory period and the first alarm bell. Constant monitoring by a doctor is required.
Emergency conditions, such as a sharp jump in blood pressure, pose a danger to the child and mother. There is a risk of death.
- Stress. Both momentary and long-term, for example, against the background of preparation for exams during the session period, etc.
The basis of the condition is the release of adrenal hormones from the blood. Primarily cortisol and adrenaline. Both have a vasoconstrictor effect and stimulate the nervous system.
Blood has to overcome more resistance. Hence the need to intensify cardiac activity to provide tissues with oxygen. Nervous shock plays the same role.
- Physical overload. Usually we are talking about inadequately high mechanical activity.
The phenomenon is typical for amateur athletes, workers whose professional activities involve lifting loads, and others.
The development mechanism is identical to the previous one. The condition worsens as a result of increased cardiac activity.
- Drinking caffeinated drinks. Including tea, energy drinks. Lead to increased vascular tone. The result is a sharp jump in blood pressure within 20-30 minutes.
The action of the active substance is about 2-3 hours. During this entire period the patient is in great danger.
- Alcohol abuse. Alcohol has a paradoxical effect. In the first phase, the effect is vasodilating. There is a drop in blood pressure.
Already after 10-15 minutes the opposite effect is observed. Blood pressure rises, cardiac activity intensifies. A stroke, heart attack, or other emergency condition is possible.
The prospects for such an outcome depend on the characteristics of the patient’s body and resistance to alcohol.
For some, a sip is enough, for others a bottle is not enough to cause a clinically significant increase in blood pressure.
- Smoking. Tobacco products destroy the body more than once. Sometimes this takes ten years.
It has been proven that there is a genetic component that determines the effect of nicotine, tars, and oxides on the body of a particular person.
The body reacts to a powerful stimulus by developing an adaptive mechanism. Over time, this leads not only to persistent, resistant arterial hypertension, but also to multiple cardiac problems, atherosclerosis of the vessels of the lower extremities (surgical departments are literally filled with heavy smokers with developed gangrene).
- Use of oral contraceptives. Young women, wanting to diversify their sex life, take contraceptives.
Usually the appointment is carried out without a doctor’s prescription. Dosages are also not observed.
Progestin drugs provoke persistent deviations in hormonal levels and, as a result, chaos in the regulation of vascular tone. Hence the increase in blood pressure over a wide range.
These factors are controllable. That is, the patient is able to correct his condition without the help of a doctor.
However, they do not always end in hypertension.
In the early stages, we are talking about individual episodes of increased blood pressure: there is no provoking factor, and there is no increase in tonometer readings.
Pathological, cardiac factors
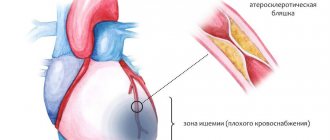
- Atherosclerosis of the aorta, large vessels. As a result of blockage (partial) or stenosis.
It ends with obstruction of patency and intensification of cardiac activity, and without treatment - a heart attack.
The symptoms of a pre-infarction condition are described in detail in this article.
- Congenital and acquired heart defects. More often, valve insufficiency, absent or incomplete functioning of the septa. Recovery is surgical. The effect occurs in 95% of cases; it normalizes the functioning of the muscular organ and lowers blood pressure.
- Inflammatory pathologies of the heart and pericardium. Lead to destruction of cardiac structures or fluid accumulation and compression (tamponade). Treatment is urgent, in a hospital setting, using antibiotics and corticosteroids, as well as special protectors.
- Rheumatism, autoimmune pathologies. Lead to arterial hypertension at advanced stages.
- Having had a heart attack or stroke. Acute nutritional disorder of the myocardium or cerebral tissue, respectively. This is a symptomatic manifestation. Duration - from 3 weeks to 6 months. Intensive antihypertensive therapy under the supervision of a cardiologist is indicated at all times.
Pathological noncardiac causes
- Renal pathologies, including acute or chronic failure, decompensated. Recovery is carried out by a nephrologist. In severe cases, dialysis is indicated, but this is a temporary measure. Neglected situations are eliminated radically by removing the paired organ. If the process affects both kidneys, transplantation is indicated.
- Liver failure. Blood pressure rises to 160-165 to 90-95 or more as a result of organic changes in the organ. The onset of the pathological process is associated with hepatitis or cirrhosis. Extremely rare malignant tumors.
- Endocrine diseases. Hyperthyroidism (excessive production of thyroid hormones), excessive production of cortisol by the adrenal glands. Also background deviations as a result of gynecological diseases.
- Neurogenic conditions, injuries.
160 over 90 is not normal pressure. It indicates a hypertensive process of a certain origin. Natural or not is a diagnostic question. The line between them is minimal, risks are always present.
Increased systolic pressure - what is the danger
Systolic isolated hypertension is a rare disease in which only the upper pressure increases, while the lower pressure is within the acceptable limits established by WHO. Quite often, against this background, there is an increase in such a parameter as pulse pressure.
People in the older age category are most often at risk. This is due to the fact that the older a person becomes, the more intense the aging process occurs. Against this background, structural changes occur in the vessels, and the peripheral nervous system is also affected.
If in addition the patient suffers from vascular atherosclerosis, then the disease is extremely difficult to treat.
According to numerous clinical studies, by the age of 50, the heart undergoes serious changes. Thus, almost everyone experiences an increase in atrial volume, and vascular calcification may also occur. The ability of the kidneys to filter is also noticeably reduced, which leads to disruption of renal blood flow and a decrease in the sensitivity of various receptors.
Very rarely, the disease can be diagnosed at a fairly young age, then most often it is based on a genetic predisposition. To select the correct treatment tactics, systolic hypertension is divided into primary and secondary, which is also called symptomatic.
The secondary form can be diagnosed when:
- Coarctation of the aorta;
- Hemolytic anemia;
- Mitral valve insufficiency;
- Atrioventricular block;
- Thyrotoxicosis.
Almost always, the disease is combined with an increase in heart volume and impaired coronary circulation. In fact, such serious changes in the cardiovascular system are rare.
In addition to internal changes, hypertension is classified according to other criteria. During the examination, the doctor takes into account the patient’s appearance. The so-called pale form of hypertension is characterized by a decrease in overall body temperature, as well as a change in the color of the skin, which becomes pale. Patients may experience severe weakness and bouts of sweating.
There is also a red form of hypertension. Its main symptom is a sharp increase in blood pressure against the background of darkening of the skin. In some cases, pink migratory spots may appear throughout the body due to dilation of the capillaries.
Home help
An attack of arterial hypertension or an episode of increased pressure is treated with great care. A sharp drop in the tonometer reading can lead to fatal consequences: cardiac arrest, heart attack or stroke.
The algorithm for reducing tonometer readings is as follows:
- Measure blood pressure and heart rate. As the rate increases, the rate of cardiac activity increases. Bradycardia is uncharacteristic and does not occur. Not counting emergency conditions, potentially fatal.
- Open a window or vent to provide fresh air. Excess carbon dioxide in the environment leads to further hypoxia and disruption of cellular respiration. The risk of complications increases.
- Take prescribed medications. If the patient has not yet been to a cardiologist, you can take Capotopril (there are several trade names). This remedy should be in the first aid kit of anyone who is prone to pathologies of the cardiovascular system in general. Quantity - no more than a quarter of a tablet at a time. It is also possible to use a beta blocker (for example, Anaprilin) together. Amount - 25 mg per dose.
- Lie down, calm down. Pay attention to how you feel. If after 30 minutes there is no effect, or even worse, call an ambulance.
Attention:
The use of baths, folk recipes, contrast showers, heating pads, and water procedures is generally strictly prohibited. Such amateur activity will result in at least a hypertensive crisis, and at maximum a dangerous condition with the prospect of death in the short term.
You can reduce the pressure of 160 to 90 on your own, the question is feasibility and safety. Emergency antihypertensive drugs are used. Beta blockers as needed.
What does it mean
What does it mean when the tonometer shows the numbers 160 to 90? The regular appearance of such indicators indicates the transition of hypertension to the second stage. It is important to remember that for representatives of the older age group, blood pressure is 160/90 mmHg. Art. is an acceptable norm.
But only if the condition is not accompanied by the development of a clinical picture typical of hypertension. The reason is the general aging of the entire body and the vascular system in particular. The walls of the blood vessels become less elastic, which leads to an increase in blood pressure (blood pressure).
Important! Women's blood pressure levels are initially lower than men's. Therefore, blood pressure 160/90 is a sure sign of hypertension.
Symptoms and threatening manifestations
Manifestations in women and men are the same, and they can be divided into two groups. The first accompany a person for a certain part of the time. The latter indicate urgent processes and require urgent care in a hospital setting.
Main features:
- Headache. In the parietal, occipital regions, intense in nature. Baling, shooting. Occurs regularly, periods of absence in chronic hypertension stage 2 are relatively short (several days, if you’re lucky - a week). The good or bad news is that the symptom gradually goes away. The heaviness in the head remains, but there is no pain. This is getting used to the new blood pressure. There is nothing good about this. Diagnosis becomes more complicated, tonometer readings stabilize. Coping with such a process is many times more difficult.
- Vertigo. Observed in acute moments. Accompanied by the impossibility of normal orientation in the surrounding space.
- Dyspnea. It occurs as a consequence of impaired gas exchange.
- Tachycardia. Acceleration of cardiac activity. There is no strict determinism, but both phenomena: both pressure and pulse growth are caused by one factor. Therefore they are considered in the system.
- Fainting. In rare cases. Usually at the initial stage of the pathological process or at the time of increasing signs of a hypertensive crisis.
- Noise in the ears, flickering of flies in the field of vision, photopsia, double vision and other manifestations of the sensory organs.
- Nausea and vomiting.
When cardiac problems arise (and sooner or later they become associated), a disturbance in the normal rhythm of the heart occurs, blueness of the skin in the lip area, and pallor of the dermal integument in general.
Symptoms of emergency conditions are more pronounced. If the first group grows gradually, the clinic can develop over the course of months, in this case everything is limited to a few tens of minutes.
- Acute, unbearable headache.
- Complete loss of orientation in space.
- Discomfort in the chest. Pressure, radiates to the stomach, back, does not allow normal breathing.
- Severe arrhythmia.
- Paralysis, paresis.
- Facial distortions.
- Speech, vision, hearing impairments.
- Dysuria (lack of urination).
- Frequent syncope.
- Feeling of goosebumps running all over your arms, body, head.
A team of doctors is required to determine the patient's condition and possible transportation to the hospital.
Normal or pathological?
Blood pressure 160/90 mm Hg. Art. Is it the norm or a deviation? Most often, this level of blood pressure is considered by doctors as a pathology and indicates the development of the second degree of hypertension. The condition in this case is accompanied by characteristic symptoms and requires drug treatment.
Sometimes this blood pressure may be normal. This indicator can occur in men over 40 years of age or people with a large physique and tall stature. At the same time, there are no unpleasant manifestations characteristic of hypertension.
Diagnostics
The examination is carried out under the supervision of a group of specialists. The first is a cardiologist. As necessary (to study the origin of arterial hypertension).
List of activities in correct order:
- Oral questioning of the patient and collection of anamnesis. First of all.
- Measurement of pressure and heart rate.
- 24-hour Holter monitoring. The main indicators are recorded for 24 hours. Considered the gold standard, although little is known about etiology.
- Electrocardiography. Assessment of functional deviations. Variants of arrhythmias are possible, from typical sinus tachycardia to ventricular extrasystoles and others.
- Echocardiography. Visual technique. Aimed at identifying organic pathologies and defects. The classic sign of advanced hypertension is left ventricular hypertrophy.
- Load tests. Carefully.
Advanced diagnostics includes blood tests (general, biochemistry, hormones), urine (clinical, according to Zimnitsky).
Also assessment of the neurological status using routine methods, electroencephalography, MRI of the brain (rarely), scintigraphy of the liver, kidneys, and thyroid gland. It is possible to prescribe FVD and X-ray of pulmonary structures.
Treatment
Considered in two planes. When the process occurs naturally, correction of controllable factors is indicated.
The second aspect concerns the etiotropic effect itself - eliminating high blood pressure or the disease that led to the process.
The first point shows a change in lifestyle:
- Refusal of cigarettes, alcohol, especially drugs.
- Complete rest of at least 8 hours per night.
- Normalization of diet. More vitamins, less fatty, fried, no canned and semi-finished products, fast food due to the significant content of sodium compounds, which retain water and negatively affect the kidneys.
- Salt consumption - no more than 5-7 grams per day. You cannot completely abandon it.
- Physical activity is at an adequate level (an hour of walking, maybe a little more every day). No intense exercise, otherwise a stroke is likely.
Attention:
Folk remedies are strictly contraindicated. Thus, recommended herbal remedies based on chokeberry can lead to rupture of a blood vessel in the brain, and decoctions of chamomile, sage, mint, motherwort and valerian are a waste of time. They are not able to correct conditions at an advanced stage. While the patient is brewing tea, the body is degrading.
Another aspect of therapy is addressing the underlying cause. There are different options here.
- Cardiac conditions are treated with conservative methods (the use of ACE inhibitors, beta blockers, calcium antagonists, cardiac glycosides, antiarrhythmic drugs and others), as well as surgical methods (for defects of cardiac structures, the need to install an artificial pacemaker or prosthetics).
- Problems with the endocrine system are solved by taking substitutes or by surgery.
- Nervous pathologies are eliminated with tranquilizers, nootropics and cerebrovascular medications.
There are a lot of options, each clinical case is considered separately.
Blood pressure itself is reduced with the following medications:
- ACE inhibitors. Perindopril and its trade names.
- Beta blockers. Carvedilol, Anaprilin as the safest.
- Calcium antagonists (Diltiazem and Verapamil).
- Centrally acting drugs (Moxonidine).
- Diuretics (Veroshpiron, etc.).
They are usually used in combination. But it is impossible to choose a safe combination on your own. If the pressure rises to 160/90, use Capoten as an emergency.