Cardiac edema is a symptom that accompanies the underlying disease. The observation of these symptoms indicates insufficient work of the heart, its inability to pump the volumes of blood necessary for adequate nutrition of the tissues of the internal organs. [toc]
Swelling is the body's response to heart failure. In most cases, this symptom is observed in elderly patients, which is associated with a decrease in the number of contractions of the organ and the amount of arterial blood ejected. To prevent this condition from developing into a severe form, timely therapy is required.
What are cardiac edema, the mechanism of development
Swelling is the accumulation of physiological fluid in the intercellular space. With cardiovascular diseases, the heart works “to wear out” and cannot cope with the amount of blood that needs to be distributed throughout the body. Due to stagnation processes, the quality of blood changes.
The following are responsible for its structure:
- proteins-albumin and globulins, which retain the liquid part inside the vessels and maintain oncotic pressure;
- glucose and sodium are substances with osmotic properties that draw out fluid;
- hormones (renin, aldosterone, angiotensin, etc.) - increase or decrease the permeability of the vascular walls and lumen.
A change in the ratio of these substances against the background of an increase or decrease in blood pressure (BP) “squeezes” fluid out of the vessels, and it accumulates in soft tissues, in parts of the body located in the lowest areas. During the daytime, swelling due to cardiac pathologies forms on the outer sides of the feet, and at night - on the lower back and buttocks.
Development mechanism
The circulatory system of mammals, which includes humans, consists of 2 circulatory circles - complex systems of all ducts, lymphatics, large and small arteries, veins, capillaries. The large circle provides oxygen supply to peripheral tissues and utilization of carbon dioxide. It begins in the left ventricle and ends in the right atrium.
The pulmonary circulation is called pulmonary. From the right atrium, venous blood enters the pulmonary trunk, which is divided into 2 branches, each of them approaches one part of the lungs (paired organ). There it is saturated with oxygen, returns to the heart, and from there it spreads throughout the body in a large circle. The circulation circles intersect at the heart.
Heart failure (HF) develops gradually. At first, the myocardium does not have time to pump all the blood; it stagnates in the large vessels of the large circle. Their walls are stretched, the pressure increases, and intercellular fluid is squeezed out of the compressed tissues. Organs and tissues do not receive enough oxygen, hypoxia develops. The level of the hormone vasopressin increases, the blood vessels narrow. Because of this, the functioning of the kidneys becomes difficult. Despite the fact that the same amount of free fluid is produced, less urine is excreted. Due to oxygen starvation, the production of substances that increase the permeability of vascular walls is activated.
Attention! Impaired heart function often causes the development of renal, liver or multiple organ failure.
Causes
Cardiac edema does not always occur due to pathologies of the heart or blood vessels. But still, the main factors that trigger the development of cardiac edema are:
- decrease in oncotic pressure;
- hypertension caused by vasoconstriction;
- myocardial failure caused by cardiomyopathy, congenital heart defects, pericarditis;
- development of arrhythmias of various types - tachycardia, bradycardia, angina pectoris;
- inflammation of the heart of infectious etiology;
- myocardial infarction;
- ischemic disease.
Edema of cardiac origin can develop with varicose veins caused by inflammation of the internal walls of blood vessels, with kidney diseases that impair the outflow of urine, liver dysfunction - leading to chronic intoxication of the body. The cause of metabolic disorders can be allergies - acute and chronic, endocrine pathologies, lymphostasis. Therefore, it is necessary to treat cardiac edema only after the etiology of origin has been accurately determined. Symptomatic therapy helps for a short time, and as soon as the therapeutic course ends, the swelling returns again.
Therapy for cardiac edema
Treatment of this disorder requires eliminating not the visible symptoms, but the sources of the lymph flow disturbance. Therapy for heart disease leads to the body independently establishing fluid movement without intensive procedures. For greater effectiveness of therapy, it is necessary to adhere to several restrictions:
- reducing the consumption of salt-containing dishes and preservatives;
- limiting the amount of fluid consumed;
- inclusion of potassium-containing foods in the diet: dried fruits, tomatoes, pumpkin, nuts, etc.
Drug therapy for cardiac edema includes the use of 3 types of drugs: cardiac glycosides; diuretics; angiotensin-converting enzyme inhibitors.
The first category of drugs are components of plant origin that have a stimulating effect on the functioning of the heart muscle. Under the influence of these drugs, the organ performs more work with a reduced number of contractions and less oxygen consumption. Cardiac glycosides include Digoxin, Strophatin, Digitoxin, etc.
Diuretics are mandatory components of the treatment of any disorder associated with moisture stagnation. They have a stimulating effect on kidney function and help accelerate fluid filtration. Certain drugs additionally stabilize the water-electrolyte balance of the blood, which is why necessary elements are removed or retained from the body more quickly. These medications are selected by the attending physician based on the patient’s condition and the degree of swelling. The use of diuretics involves the use of weak components at the initial stage and in small doses, which are gradually reduced.
The effect of inhibitors is aimed at increasing the properties of diuretics and reducing the production of angiotensin-converting enzyme, which has a constricting effect on blood vessels. They have a beneficial effect on the functioning of the heart, normalizing blood circulation. The drugs in this group are Enalapril, Quinapril, Lisinopril, Fozinopril, etc.
In addition to the use of the presented group of medications, therapy for edema includes taking special medications to eliminate the specific cause of heart failure and compliance with preventive measures.
Characteristic signs of edema caused by disruption of the cardiovascular system
Unlike the accumulation of fluid in soft tissues caused by impaired kidney function, cardiac edema does not appear in the morning, but in the evening. They are usually symmetrical and rise from above - they first appear on the back of the foot, then move to the ankles. If treatment is not started on time, they rise to the hips and grab onto the buttocks. In severe cases, fluid accumulates in the abdominal cavity (ascites accompanies 5% of cases of heart failure).
Attention! Uneven swelling of the lower extremities in cardiac pathologies is explained by the development of varicose veins. These pathologies often occur simultaneously.
Swelling due to heart disease increases in the evening. During the day you have to be in a horizontal position, intercellular fluid accumulates below under the influence of gravity. The heart is not able to pump the entire volume of blood, it stagnates in large veins, the vessels dilate, and the general condition worsens.
The main symptom of cardiac edema is a decrease in body temperature in the area of swelling. Stagnant processes disrupt intercellular metabolism, the supply of oxygen decreases, and oxidation processes slow down. Your feet begin to freeze and “goosebumps” appear on them.
Interesting! Edema during inflammatory processes is hot to the touch, kidney edema feels the same as the surrounding tissue.
Due to the above changes - metabolic disorders, hypoxia - the color of the skin changes. At first it turns pale, then acquires a bluish tint, and later - bluish-violet. Another characteristic feature is density. The skin on top is stretched. If you press on the affected area with your fingers, a hole remains that does not smooth out for a long time. In this case, the patient does not experience pain - sensitivity decreases due to atrophy of nerve endings.
“Cardiac edema” appears gradually; its origin is indicated by a slow increase. First, small portions of venous blood stagnate, which, under the influence of gravity, “drain” into the lower extremities, dilating the vessels and squeezing out the intercellular fluid. It is difficult to get rid of swelling - diuretics, rubbing, poultices, compresses do not help. On the contrary, they can lead to formations increasing in size. Edema subsides only when the pumping function of the heart is restored.
Stagnation of intercellular fluid is not the only symptom of heart failure. Other organic disorders also indicate pathology of the heart muscles:
- Shortness of breath is a disruption of the breathing rhythm that worsens with physical exertion. When the speed of blood movement in the systemic circulation decreases, its passage through the small circulation slows down. Patients complain of the inability to take a deep breath and lack of air.
- Weakness and dizziness appear due to hypoxia. When blood flow slows, not enough oxygen reaches the muscles and brain. Weakness increases, it becomes difficult to concentrate, memory functions and coordination abilities are impaired. These symptoms occur earlier than edema of cardiac origin.
- Cyanosis - the skin first becomes pale and then turns blue. This happens because there is not enough oxygen in the arterial blood. The capillaries suffer the most. If they are close to the surface of the epithelium, the face appears “transparent”.
- Heart pain is first localized on the left side of the chest (the most severe manifestations in coronary artery disease). Then they radiate to the left shoulder, to the right hypochondrium. If the right ventricle of the heart cannot cope with the load due to pathological changes, blood stagnation occurs in the portal vein. It receives blood from the liver after filtration. Blood accumulates, stretching the liver capsule, which puts pressure on surrounding tissues.
Another sign of heart failure is the “Hippocratic” or “drum” fingers. With chronic respiratory and heart failure, the shape of the nail phalanges of the fingers change - they thicken and become dull. Both upper limbs are affected simultaneously. If you begin treatment of cardiac edema at the first signs of illness, the development of severe symptoms can be prevented.
Mechanism of occurrence
The disorder is based on changes in speed and efficiency of blood flow in the large and small circles.
The result of a decrease in myocardial contractility is a slow movement of connective tissue.
Stagnation in the veins leads to an increase in pressure and the release of the liquid fraction, plasma, into the intercellular space.
At its core, edema is an increase in the volume of soft tissue for a specified reason. Since the force of gravity acts strictly vertically, from top to bottom, the legs are the first to suffer.
As the pathological process progresses, the condition worsens, but this takes time. On average, the development of a complex disease takes from 2 to 6-7 years.
Peripheral edema also forms as a result of the further development of secondary pathological processes. Like kidney failure, liver dysfunction.
It is problematic to distinguish conditions from each other, especially in the later stages of cardiac decompensation.
The intensity of the symptom becomes higher, which indicates continued progression. Diagnostic measures, multiple ones, put an end to the question.
Diagnostics
Even after the patient has voiced complaints, assessing the clinical picture, the origin of the swelling cannot be determined. Diagnostic measures begin with standard examinations: blood pressure monitoring; blood donation - a detailed analysis for cholesterol, thyroid hormones; Analysis of urine. During the examination, the doctor conducts a physical examination - using a phonendoscope, he listens to the heartbeat and lung sounds. If previously percussion was mandatory - the boundaries of organs were determined using palpation, now patients are referred for ultrasound.
Specific examinations during initial treatment:
- ultrasound - to exclude pathological changes in the kidneys and liver;
- electrocardiography - detects disturbances in pulse rhythm and hypertrophy of the cardiac ventricles;
- donate blood for atrial natriuretic hormone - a marker of heart failure;
- radiography - prescribed to patients with severe edema.
A set of diagnostic procedures is prescribed to each patient separately. To exclude kidney or liver dysfunction, a biochemistry test is prescribed. During it, the following indicators are determined: bilirubin, ALT, ACaT, prothrombin index, urea, creatinine. Perhaps they will give you a referral for an MRI or CT scan.
Interesting! Sometimes a specific diagnostic measure is carried out - the Kaufman experiment. It can be used to determine which organ dysfunction is associated with the appearance of swelling. The procedure is still popular among doctors working in medical institutions that are not equipped with expensive equipment.
The patient is asked to drink 400-500 ml of water every hour for 3 hours. Then he is laid down with a cushion placed under his legs so that they are above the level of the heart. You need to walk or stand for another 2 hours. Urinalysis is performed periodically. The dynamics of blood circulation in heart failure are determined by the density of the sample. If in the first the density is normal, in the second - after the patient was lying down, it is low, and in the third - when the patient was walking - the highest, the diagnosis of HF is confirmed. In decompensated heart failure, the Kaufman method is dangerous to use.
Signs
Often people do not realize that the cause of leg swelling is a problem with the heart. Therefore, they do not take any action for a long time, and the disease, meanwhile, progresses. Swelling in the legs due to heart failure has characteristic symptoms that differ from similar manifestations of kidney or liver diseases:
- In the initial form, the disease affects the lower part of the leg - the foot swells.
- Symmetrical appearance (on both legs).
- The lower limbs become elastic to the touch.
- After pressing with a finger, a slowly disappearing hole remains.
- Possible liver enlargement.
- A severe form of the disease is accompanied by swelling in other parts of the body. New symptoms arise - tachycardia, shortness of breath, pale skin, chronic fatigue.
If swelling of the legs appears, similar to a symptom of heart failure, you should immediately go to the doctor and start treatment. Timely help will save you from dire consequences such as heart attack or stroke.
Treatment
If the diagnosis is established and the accumulation of extracellular fluid in the soft tissues causes cardiac dysfunction, complex therapy is necessary. When the process grows rapidly and appears as a complication after infectious diseases, the patient is offered hospitalization. Treatment at home is allowed for relapses of chronic heart failure, or for patients with moderate edema. Treatment is aimed at eliminating or bringing into remission the underlying disease. To get rid of edema, symptomatic therapy may be required. In addition, the patient will have to adhere to a special diet for a long time.
Basic treatment
Therapy and additional measures depend on the stage of the disease. On the first stage, it is enough to support yourself once every six months with the help of medications - the complex is clarified by a cardiologist. No adjustment of the daily routine is required, since symptoms appear only during intense physical activity.
At the second stage A (II-A), when blood circulation in the small circle is impaired, the skin already turns pale and the lips turn blue. In this case, it is recommended to go to the hospital at least once a year. A special diet is required, and physical activity will have to be limited. At stage B (II-B), with circulatory disorders in the large and small circles, patients already complain of chest pain. They need to adjust their daily routine, switch to a special diet, and limit physical activity. They may be declared incapacitated.
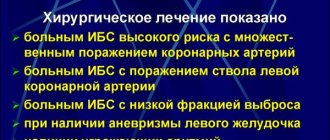
At the third stage, patients are given disability. The underlying disease is usually accompanied by renal and liver failure, liver cirrhosis, and diffuse pneumosclerosis. It is impossible to stop the final stage with conservative therapy. Stabilization is possible only through surgical intervention, provided that the pathological changes in the internal organs have not reached the terminal stage.
Due to the rapid deterioration of the condition, treatment for heart failure should be started early. To bring the condition into remission, the following may be prescribed:
- ACE inhibitors. This group includes: Lisinopril, Ramipril, Captopril, Enalapril and the like. These drugs stop the degradation of the myocardial structure.
- Beta blockers - Atenolol, Bisoprolol, Anaprilin. They stop tachycardia and reduce myocardial oxygen demand.
- Cardiac glycosides - often Digoxin. Increase blood flow, enhancing contractility.
- Diuretics - Hypothiazide, Furosemide, Lasix. Medicines eliminate swelling.
- Preparations with potassium and magnesium - Asparkam, Panangin, Kudesan. If you do not replenish the reserve of minerals that are removed along with the intercellular fluid, you will not be able to stabilize your heart rate.
- Statins - Atorvastatin, Livazo, Crestor, Rosuvastatin. They are necessary for ischemic disease.
- Indirect anticoagulants - Heparin, Venolife, Warfarin. Reduce blood clotting and prevent the formation of blood clots.
As symptomatic therapy, the following are used: peripheral vasodilators (Prazosin, Sodium nitroprusside) to relieve anginal pain; non-glycoside inotropic stimulants (Adrenaline, Dobutamine) - for hypotension. It is possible to prescribe other medications based on the clinical picture.
Attention! Treatment is carried out under the supervision of a doctor. It may be necessary to adjust the dosage or change the therapeutic regimen.
ethnoscience
When connecting recipes made from medicinal plants, you must consult your doctor. Herbal decoctions and infusions are not always combined with pharmacological drugs.
Most often used:
- Viburnum berries, which increase urine flow. Fresh (or dried) fruits, 1 tsp, brew with 1 glass of boiling water, boil for 10 minutes. The infusion is diluted with honey. You can take up to 3 glasses per day.
- Wormwood is useful for tachycardia, shortness of breath, angina pectoris. Drink 45 ml per day, in equal portions, 30 minutes before meals. To prepare the decoction 2 tbsp. l. pour 0.5 liters of water, boil for 15 minutes, let stand, filter, bring to the original volume.
- Stinging nettle normalizes blood circulation. To make an infusion, dried plant materials are brewed like strong tea, at the rate of 1 tbsp. l. per glass of boiling water. Drink instead of tea, morning and evening.
- Vitamin tea to replenish vitamin and mineral reserves. Mix equal amounts of rosehip and red rowan berries. It’s better to brew it in a thermos and drink it like compote or fruit drink. It is better to sweeten with acacia or buckwheat honey.
- Parsley seeds have a pronounced diuretic effect. Leave for at least 10 hours in a thermos, pour 1 tsp. seeds with a glass of cold water. Everyone drinks in equal portions every day at equal amounts of time.
- Asparagus improves metabolic processes in the myocardium. The plant is dried entirely, a saturated infusion is brewed in a thermos - 3 tbsp. l. for 250 ml of boiling water. After 2 hours, filter. Drink 1 tbsp. l. every hour for 3-5 days.
- The diuretic mixture is made up of 1 part horsetail, 2 parts knotweed, 3 hawthorn flowers. Brew with hot water: 1 tbsp. l.—1 glass. You need to drink before 13.00, a few sips each time.
- Lily of the valley - the plant contains cardiac glycosides. This natural raw material is poisonous, so before introducing the infusion into a therapeutic course, you must consult a cardiologist. The action is pronounced. The infusion is brewed at the rate of: 1 tsp. - 200 ml of boiling water. Take half a tablespoon 3 times a day.
- The soothing collection reduces the load on the heart muscle. Mix 3 parts of valerian roots, the same amount of peppermint, 4 parts of lemon balm. Brew like tea, take half a glass in the morning and before bed.
- Mint has a calming effect. Brew in the morning, drink half a glass in the morning.
- To stimulate blood circulation in the lower extremities, it is recommended to do foot baths. Nettle - preferably fresh, crushed, infused 2-3 handfuls in 1.5 liters of boiling water for 15 minutes. Cool to 45-50°C, lower your legs for 10 minutes.
In folk recipes they often give the recommendation: “brew it like tea.” It is implied that you need to pour 1 tbsp. l. vegetable raw materials 250 ml (glass) of boiling water and leave covered for 15-20 minutes.
Attention! The duration of the treatment course with medicinal infusions and decoctions is no longer than 1.5-2 months, unless otherwise recommended. Baths can be done once every 2 days up to 7-8 months.
Nutrition
It is recommended to adhere to diet No. 10 according to Pevzner. Avoid salt and reduce its content to a minimum, adding it to ready-made dishes. Reduce calories by reducing the content of carbohydrates and fats. Cooking technology: stewing, boiling, baking in foil, steaming. Daily calorie content - 2500 kcal.
You need to limit: coffee, strong tea, oils - butter and vegetable, green peas, white cabbage, radishes, carbonated drinks, tart vegetables - onions and garlic. It is allowed to eat herring, but first soak it in milk. Prohibited: smoked meats, canned food, chocolate, offal, strong broths, mushrooms, fish.
Allowed:
- bread is not rich;
- baked goods - with bran;
- soups - with unsaturated broths, milk;
- lean meat and fish;
- eggs - no more than 3 pcs. in Week;
- vegetables - potatoes, tomatoes, cucumbers, beets, zucchini, carrots;
- cereals and pasta;
- milk and fermented milk products;
- sweet fruits - peaches, pears, plums;
- berry desserts are better - jam, mousses, marshmallows, marmalade;
- drinks - teas: weak black or fruit, compotes, fruit drinks, juices.
You need to eat in small portions, 5-6 times a day, not forgetting about foods rich in potassium - baked potatoes, bananas, raisins, buckwheat porridge. During treatment with diuretics, nuts, seeds, and grapes are added to the diet. It is better to replace salt with soy sauce or lemon juice.
Approximate daily menu for edema:
- Breakfast - semolina porridge, bread with cream cheese, tea with milk.
- Snack - dried fruits, no more than a handful.
- Lunch - pureed potato and cauliflower soup with sour cream, steamed turkey with potatoes, fruit compote.
- Afternoon snack - biscuits with rosehip infusion.
- Dinner - stewed fish with carrot puree or sweet pilaf, tea with milk.
- At night - kefir or yogurt.
In case of severe heart failure and severe edema, it is better to adhere to the Karel diet. The daily diet is divided into 8-10 meals. For 3 days, limit yourself to 800 ml of warm milk and 100 ml of rosehip decoction in equal portions. For another 3 days, 200 g of semolina with milk and 50 g of bread and butter are introduced into the menu.
The next cycle, also designed for 3 days - 700 g of milk, 150 g of bread (uneaten), 200 g of puree from permitted vegetables, butter - a piece of 50 g, 2 eggs. In the future, they switch to the Pevzner diet. Such unloading, when the condition worsens, helps to quickly get rid of swelling.
Therapy
Timely medical intervention helps to overcome the pathology completely. Excess fluid is removed from the body, facilitating the functioning of all its systems. In addition, patients with heart failure should monitor their diet. Drink minimal fluids.
Diet
For patients suffering from heart failure, in the early stages of the onset of swelling, a gentle diet No. 10 is prescribed. Its fundamental principles are:
- Reducing calorie content of food.
- Reducing salt intake (up to 3 g per day).
- Reducing portions.
Features of diet No. 10
Meals should be divided, at least five meals per day. Dishes enriched with fats and carbohydrates are excluded from the diet. It is recommended not to fry food, but to bake, stew or boil it. The menu should be dominated by protein dishes of animal and plant origin.
Rye bread, baked goods with bran, dairy, vegetable and fruit soups are allowed. In limited quantities - various cereals, sweet fruits. You need to eat more vegetables and greens. Sweets allowed: jam, marshmallows, marmalade, various berry and fruit mousses. In total, no more than 2500 kilocalories are allowed per day.
In the later stages of the disease, the patient is prescribed the Carrel diet. It is more strict and makes it possible to effectively remove fluid from the body, eliminate swelling and shortness of breath. The diet is divided into several stages:
During the first three days, the patient drinks warm milk, and at the end of the last day - rosehip decoction. Meals should be small meals, at least eight times a day.- Over the next two to three days, solid food is added to the diet. You are allowed to eat a piece of rye bread, a plate of semolina porridge with butter.
- During the sixth to ninth day of the diet, vegetable puree with butter and two boiled eggs are added.
- During the tenth to sixteenth days, the amount of solid food increases.
The daily fluid intake in the later stages of the diet should not exceed 1-1.2 liters. You should try to drink more fruit infusions.
Conservative treatment
When noticeable swelling of the legs occurs, adequate treatment is prescribed that can completely eliminate the pathology. In simple cases and in the absence of contraindications, the doctor prescribes the following diuretics:
- Furosemide.
- Lasix.
- Hypothiazide.
- Indapamide.
- Veroshpiron.
- Spironolactone.
To strengthen the walls of venous vessels, it is recommended to take the following medications:
- Aescusan.
- Troxevasin.
- Detralex.
- Normoven.
The following medications are suitable to reduce blood viscosity:
- Cardiomagnyl.
- Lospirin.
- Aspecard.
- Aspirin.
To restore lost potassium ions take:
- Panangin.
- Asparkam.
In severe cases of the disease, the patient is admitted to the hospital. Initially, a potassium-polarizing mixture is injected intravenously. It helps improve the condition of the cardiovascular system. IVs are prohibited. Administration of the drug through droppers can only aggravate the patient’s already serious condition and lead to pulmonary edema.
After a few days, if the patient's blood pressure is stable, he is given diuretics. If the pressure is low or high, therapy is carried out aimed at stabilizing it.
Possible complications
Swelling, which appears occasionally after excessive physical exertion, stress, debilitating diseases and as a consequence of complications, is not dangerous. But if they persist for more than 2 weeks, occur periodically, and are accompanied by shortness of breath and weakness, there is reason to consult a doctor.
The symptom indicates a circulatory disorder, which, in the future, can not only aggravate heart failure, but also provoke the development of liver and kidney failure. The swelling itself has a negative impact. Stagnation of blood in the lower extremities, squeezes out intercellular fluid, disrupts metabolic processes in epithelial tissues.
Complications that can develop due to neglect of one’s own health:
- lymphadenoma (swelling of the lower extremities) - stimulate the formation of trophic ulcers, areas appear where nutrients do not flow, phlegmon and areas of necrosis appear;
- hydrothorax - fluid accumulates in the pleural cavity;
- ascites - intercellular tissue accumulates in the abdominal cavity;
- hydropericardium - transudate flows down the pericardial sac, pericardium (the condition is called cardiac dropsy).
Surgical intervention against the background of heart failure is difficult. The prognosis for recovery depends on the underlying disease that caused the swelling. If heart disease begins to be treated at the first signs, then the puffiness quickly disappears. But it is impossible to judge that the disease was defeated by the disappearance of swelling. This does not affect the final forecast.
Prevention and general recommendations
Effective means aimed at reducing swelling are various baths of medicinal herbs and massage of the limbs. It is recommended to make compresses from grated potatoes. Since cardiac edema accompanies a person for a long time, great attention should be paid to preventive measures.
How to get rid of cardiac edema? It is recommended to undergo regular medical examinations, adhere to a special diet, get rid of bad habits, and try to minimize exposure to stressful situations. In emergency situations, the hormone adrenaline is released into the body. In response to this, the heart begins to work with redoubled force, and vasospasm occurs. The load on organs in such a situation increases significantly. Smoking and alcohol lead to the development of vascular atherosclerosis and provoke the formation of renal and cardiac edema.
An important condition for prevention is the treatment of somatic diseases: anemia, fever, diabetes, respiratory diseases. Dental tonsillitis is a dangerous disease. The infection enters the bloodstream, resulting in endocarditis, an inflammation of the heart muscle. Untreated tonsillitis can cause heart failure at a young age.
Galina Polovnikova / author of the article
I write articles in various areas that, to one degree or another, affect such a disease as edema.
Prevention
When cardiac-type swellings appear, measures must be taken to prevent the development of the underlying disease.
- Reduce the amount of salt in your diet, avoid spicy and spicy foods.
- Increase the consumption of fresh vegetables, fruits, drinks - except alcohol, sweet tonics and strong coffee
- Increase physical activity, do foot massages, baths - including contrast ones. Make time for walking.
- Eat a healthy diet and avoid weight gain.
- Quit smoking and alcohol.
Diet
This is an important part of complex therapy, since it is impossible to relieve swelling without following a diet. What to do to effectively combat edema? Here are some rules:
- Reduce the amount of water consumed. This includes first courses, juices, milk porridges, and other foods with a high liquid content. Excess water in the body puts a strain on the diseased heart, causing the formation of edema. The total volume of clean water (including food) should not exceed one and a half liters. If the patient's specific situation requires it, the doctor prescribes an even stricter restriction.
- Eat often, but in small portions. The best option is 5-6 times a day. Overeating is unacceptable. The interval between the last meal and sleep should be at least 4 hours. This diet creates conditions for rapid digestion and absorption of nutrients.
- Minimize salt intake. The ideal option is to completely exclude it from the diet. If desired, you can replace it with a little lemon juice while cooking. Salt directly affects fluid stagnation in the body. The heart becomes weaker, and the swelling increases.
- Avoid fried, smoked and fatty foods. They also tend to increase swelling. Cook food in healthy ways - boil in water or steam, bake in the oven without adding oil. This applies to both vegetable and meat dishes.
- Balance your diet. It is necessary to reduce the level of fat consumed, but proteins and carbohydrates must be supplied to the body in sufficient quantities, not lower than the daily norm - 2500 kcal. Regular consumption of foods rich in vitamins and minerals (fresh vegetables, fruits, herbs) will have a beneficial effect on the entire body.
To make it clearer how to treat swelling in heart failure by adjusting the diet, let’s combine an approximate list of healthy and harmful foods into one table.
| Can | It is forbidden |
| Lean meat (chicken, beef, veal). | Processed meat products (sausage, frankfurters, ham), lard, pork, goose. |
| Dairy and vegetable soups. | Fatty broths. |
| Lean fish (not salted). | Canned food (meat, fish), salted and smoked fish. |
| Stale or dried bread, crackers. | Fresh baked goods (bread, pancakes, pancakes). |
| Boiled eggs. | Fried eggs. |
| Cereals, pasta | Legumes (peas, soybeans, beans) |
| Fermented milk products (cheese, cottage cheese, kefir). | Salty cheeses (brynza), cream, sour cream. |
| Vanillin, cinnamon. | Hot spices. |
| Vegetable oil. | Animal fats, margarine. |
| Marshmallow, mousse, jelly, marshmallow. | Chocolate, desserts with rich cream. |
| Fresh fruits and vegetables (just don’t overuse them), boiled or baked. | Salted, pickled vegetables, nuts, mushrooms, spinach, radishes, radishes. |
| Juice, compote, weak tea. | Caffeinated drinks (coffee, cocoa, strong tea), alcohol, lemonade. |
The timing of the diet is determined by the doctor. It is usually recommended to adhere to dietary restrictions during the period of treatment for swelling, as well as for the first time after it (about a month).
Complications and prognosis
The progression of cardiac edema over 1-2 weeks and refusal to visit a medical facility leads to impaired blood circulation and tissue trophism, and their further necrosis.
In the absence of therapy, trophic ulcers, lymphedema, ascites, anasarca, and fluid accumulation in the lungs may occur. Dangerous pathologies cause the death of the patient.
If all the recommendations of the cardiologist are followed, the treatment of the primary disease (and elimination of the syndrome) is successful.
What is “cardiac edema” and when does it occur?
There are many heart diseases. This includes coronary heart disease, in which a section of the heart muscle is insufficiently supplied with blood, and heart defects, when one of the openings - between the atrium and the ventricle, or between the ventricle and the vessels coming from it - becomes either too narrow or, conversely, widens. Heart diseases also include cardiomyopathy, in which the normal structure of the myocardium is disrupted for unknown reasons, myocardial dystrophy, hypertension and others.
What they all have in common is that, in the absence of adequate treatment, they lead to overload of the heart muscle and myocardium. This is called heart failure. When it develops gradually and affects the right ventricle, edema forms. They are called edema in right ventricular heart failure.
“Simply”, in case of uncomplicated heart disease, fluid will not accumulate in the skin. This will happen only in the case when the right ventricle, working with a large circle of blood circulation, is unable to pump a standard volume of blood and begins to “leave” it in the vessels.
General swelling
General edema, depending on the causes of occurrence, is divided into:
- Heartfelt
- Renal
- Hypooncotic of alimentary origin
- Hepatic
- Myxedematous
Cardiac edema
Edema of a patient with a disease of the cardiovascular system is a sign of right ventricular failure and venous stagnation in the systemic circulation.
The mechanism of occurrence of cardiac
edema:
- A decrease in the contractility of the right ventricle leads to an increase in hydrostatic pressure in the veins of the systemic circulation, as a result of which the liquid part of the blood along the hydrostatic pressure gradient goes beyond the vascular bed into the tissue. The volume of circulating blood decreases, hypovolemia develops.
- In response to hypovolemia, hormonal mechanisms are activated: the production of ADH in the pituitary gland and aldosterone in the adrenal glands, which leads to increased reabsorption of sodium and water in the renal tubules and worsening edema.
- Due to hypovolemia, renal blood flow decreases, irritation of the JGA occurs, activation of the RAAS (primary hyperaldosteronism) aggravates the retention of sodium and water in the body.
- Hypovolemia and venous hypertension in the systemic circle lead to tissue hypoxia, resulting in increased capillary permeability.
- Prolonged venous congestion in the liver leads to a disruption of its neutralizing function, as a result of which excess aldosterone does not have time to be neutralized in the liver (secondary hyperaldosteronism).
In the later stages of heart failure, the liver loses the ability to synthesize albumin, which leads to a decrease in the oncotic pressure of the blood and worsening edema up to the development of anasarca, that is, the accumulation of fluid not only in the subcutaneous fatty tissue, but also in the cavities.
Clinical characteristics
cardiac edema:
- appear or intensify in the evening, disappear or decrease in the morning.
- appear first on the back of the feet, ankles (in bedridden patients - on the sacrum), then spread to the legs and thighs, symmetrical
- cyanotic – accompanied by acrocyanosis; with prolonged stagnation in the systemic circulation they become “colored”, which is due to diapedesis of erythrocytes, the formation and gradual breakdown of hemosiderin.
- dense, the hole does not straighten out for a long time when pressed.
- cold
- with prolonged existence, edema can be accompanied by trophic disorders - trophic ulcers appear, and secondary infection may occur.
Renal edema
According to pathogenesis (according to the triggering mechanism), edema in kidney diseases is divided into:
-nephritic
-nephrotic
-retention
Nephritic edema.
The cause of nephritic edema is acute glomerulonephritis and proliferative variants of chronic glomerulonephritis.
Mechanism of nephritic edema:
- With allergic-inflammatory damage to the nephron glomeruli, compression of the renal vessels occurs with inflammatory edema. Impaired blood supply to the kidneys causes irritation of the juxtaglomerular apparatus, increasing the release of renin. The latter stimulates the adrenal glands, which begin to intensively secrete aldosterone.
This leads to sodium retention in the body
, irritation of tissue osmoreceptors, resulting in
increased ADH secretion
. An increase in the amount of the latter leads to an increase in the reabsorption of water by the renal tubules, and water begins to accumulate in the tissues.A compensatory reaction to hypernatremia is the redistribution of sodium with its transition from the vascular space to the extravascular space. Thus, tissue hypernatriosis is formed, leading to an increase in the osmolarity of the interstitial tissue and an increase in Pt, this leads to the transition of water into the interstitial space.
This process is observed in all parts of the body, but loose hydrophilic areas of fiber swell more. This explains the localization of edema.
- The pathogenic agent acts on the basement membrane of the renal glomeruli and changes its structure so that the membrane proteins become antigenically foreign to the body’s own.
In this regard, antibodies begin to be produced against them, which in turn affect vascular membranes in general, since the latter contain antigens that are common to the antigens of the glomerular membranes.
Thus, in the body as a whole, the permeability of vascular membranes increases and the membrane factor is included in nephritic edema - systemic capillaritis develops.
Clinical characteristics:
nephritic edema is localized on the face, dense, motionless, more pronounced in the morning, decreases or disappears in the evening.
Nephrotic edema.
Causes of nephrotic edema: non-proliferative variants of chronic glomerulonephritis (small process podocyte disease, membranous nephropathy, focal segmental glomerulosclerosis), renal amyloidosis, diabetic nephropathy, renal vein thrombosis.
Mechanism of nephrotic edema:
The main mechanism of their development is hypo-oncotic.
- An increase in protein filtration and a decrease in its reabsorption in nephrotic syndrome lead to massive proteinuria, resulting in the development of hypoproteinemia with a decrease in blood oncotic pressure. This, in turn, causes fluid to escape along the oncotic pressure gradient into the tissue - edema develops.
- BCC decreases, which leads to increased production of ADH and aldosterone, activation of the RAAS, and this in turn leads to fluid retention and aggravates the formation of edema.
Clinical characteristics:
nephrotic edema is massive, soft, mobile, combined with the simultaneous accumulation of transudate in the pleural cavities, in the pericardium, in the abdominal cavity with the development of manasarca.
Differences between renal edema and cardiac edema.
Renal edema differs from cardiac edema in a number of features:
- renal edema usually appears on the face, and cardiac edema on the legs; this difference is especially characteristic of nephritic edema.
- In case of heart failure, swelling in the legs usually appears or intensifies in the evening, and disappears or decreases overnight. Edema with glomerulonephritis (nephritic, on the contrary, is more pronounced after sleep, and goes away or decreases during the day: at night, edematous fluid stagnates in the subcutaneous tissue of the eyelids due to the lack of blinking, while during the day, muscle contractions during blinking contribute to its better outflow through the lymphatic pathways.
- The skin over cardiac edema is cyanotic, cold with brown induration. The skin of kidney patients above the edema is pale.
- Renal edema is soft, mobile (especially nephrotic), and cardiac edema is dense.
Retention edema
in kidney diseases, they occur when urine production by the kidneys ceases or sharply decreases (anuria), which is observed in patients with acute renal failure, as well as in the terminal stage of chronic renal failure.
At the same time, a decrease in glomerular filtration acquires significance only in the presence of other prerequisites for the development of edema, and not as an independent factor.
Thus, in severe renal failure with a sharp impairment of filtration, swelling is often absent or even disappears if it existed before.
Source: //studfile.net/preview/6066110/page:2/
Pathology therapy
The goal of treatment is to relieve the underlying disease. The most effective method of suppressing pathology is complex therapy, including taking medications and using folk remedies.
Self-medication for cardiac edema is prohibited. Only the attending physician can select the optimal treatment plan for the patient.
Drug treatment
The use of 6 groups of drugs helps restore the functionality of the myocardium and eliminate blood stagnation:
- Beta blockers that equalize the work of the heart, reducing the muscle's need for oxygen (Nebilet, Corvitol).
- ACE inhibitors (angiotensin-converting enzyme), helping to reduce high blood pressure, stopping the progression of changes in the myocardium - Enalapril, Ramipril. If a patient taking the listed drugs develops a paroxysmal cough, the treatment regimen is adjusted: the treatment uses drugs that block angiotensin receptors - Losartan, Valsartan.
- Cardiac glycosides that improve tissue nutrition and increase blood flow (Strophanthin, Digoxin).
- Antiarrhythmic medical products. Their list includes various groups of drugs. The choice is made after determining the type of arrhythmia.
- Medicines that improve myocardial trophism (Vazonit, Cardonat).
- Diuretics - diuretics.
Let's look at the last category in more detail.
Diuretics
The group combines several types of drugs that reduce the amount of fluid through a complex effect on the body. The list of mechanisms of their work:
- decreased reabsorption of salts and water;
- an increase in the volume of substances excreted in urine;
- increasing the rate of urine formation.
Veroshpiron, Furosemide, Torameside, Piretanide are used to treat swelling of the legs in heart failure.
A side effect of diuretic therapy is a decrease in the level of potassium ions in the blood (hypokalemia). Taking these tablets should be combined with medications that replenish lost vitamins and minerals. Panangin is usually prescribed to restore balance.
Diet
Following a special diet allows you to control the amount of fluid and nutrients entering the body.
Severe swelling of the legs helps to remove table No. 10, a characteristic feature of which is the reduction of daily consumed carbohydrates and fats. Basic rules of a therapeutic diet:
- limiting the amount of salt used for cooking;
- excluding strong tea, chocolate, coffee, beans, mushrooms and cabbage from the menu;
- saturating the diet with fruits, seafood, vegetables;
- refusal of alcohol, as well as spicy and fried foods.
The number of meals per day increases to 6 times. Patients are advised to consume vegetarian soups, boiled lean meat, milk, cereals, salads, and compotes. The total energy value of products cannot exceed 2600 kcal.
Free liquid should be present in a volume of no more than 1200 ml.
It is recommended to have dinner no later than 3 hours before going to bed.
The tenth table helps reduce the load on the gastrointestinal tract, heart and blood vessels;
stabilizes metabolism, improves blood circulation.
Daily routine and lifestyle
Maintaining a healthy lifestyle, physical and mental rest helps combat edema of cardiac origin.
The patient should avoid:
- increased loads;
- stress;
- long continuous activity.
In the morning it is recommended to take a contrast shower, during the day - take short walks, in the evening - use foot baths with various decoctions of raw medicinal herbs, and do a massage.
When working sedentarily, it is necessary to change your position at least once every 30 minutes and perform exercises to restore blood circulation.
You should get at least 9 hours of sleep at night.
Folk remedies
Alternative medicine recipes will help consolidate the results of drug therapy and reduce swelling at home.