Therapeutic strategy
Treatment of renal hypertension, the symptoms of which are similar to hypertension, aims to normalize blood pressure and slow the progression of renal failure, thereby improving the patient’s well-being and increasing life expectancy. Newly diagnosed nephrogenic disease or suspicion of it is a direct indication for hospitalization to clarify the etiological factor of high blood pressure.
Drug treatment
Pharmacotherapy should be selected exclusively by a doctor. Medicines are needed to bring blood pressure back to normal and improve the functional state of the kidneys. Even taking into account the fact that traditional antihypertensive drugs are used to treat pathology, without consulting a nephrologist, taking them with a high degree of probability will not have the desired therapeutic effect. The standard treatment regimen for hypertension of renal origin includes the following groups of drugs:
- beta blockers (Atenolol, Metoprolol, Nebivolol);
- ACE inhibitors (Captopril, Enalapril, Fozinopril);
- diuretics (Furosemide, Indapamide, Spironolactone);
- calcium channel antagonists (Verapomil, Diltiazem, Lacidipine).
Beta blockers neutralize the effects of epinephrine and norepinephrine on special receptors in the heart, resulting in a decrease in heart rate and stabilization of blood pressure. Angiotensin-converting enzyme inhibitors reduce the production of the main mineralocorticosteroid hormone of the adrenal cortex (aldosterone), which prevents an increase in vascular tone.
Hypertensive patients are recommended to take a course of these drugs. The daily dosage is selected individually, taking into account the form of the disease, age and weight of the patient. Thanks to their prolonged action, such tablets allow you to keep your blood pressure under control throughout the day, even with a single dose.
Diuretics utilize excess fluid from the body, preventing the formation of edema, improve kidney function and normalize blood pressure. Calcium antagonists protect the heart muscle from dystrophic changes. For the treatment of nephrogenic hypertension, patients are often prescribed drugs based on Amlodipine. In addition, products of chemical and herbal origin, which are designed to improve the functioning of the organs of the urinary system, provide tangible benefits in the fight against the disease.
Surgical intervention
If a salt-free diet and medication do not bring any results, then it is advisable to think about surgery. Surgical intervention allows you to completely restore vascular patency. Modern clinics are equipped with equipment that allows them to perform high-tech operations with minimal risk to health. The following surgical techniques demonstrate excellent results in the treatment of renal hypertension:
- Percutaneous balloon angioplasty. Using a catheter equipped with a balloon, the specialist straightens the stenotic areas of the arteries. The obvious advantage of this manipulation is the fact that the patient is not under general anesthesia during the operation, and the intervention itself takes very little time. In rare cases, complications occur in the form of rupture of a vessel or exacerbation of bleeding.
- Open angioplasty. The essence of the operation is to remove atherosclerotic plaques and reconstruct the affected area of the renal artery, for which one’s own vessels or prostheses are used. The advantage of the technique is that the patient’s blood flow is completely restored and deposits that provoke an inflammatory reaction are removed. Old age should be considered a contraindication to surgery, since the likelihood of cardiovascular complications is high.
Hypertension and kidneys
When a doctor first diagnoses arterial hypertension or essential hypertension, the question always arises - why hypertension developed, what are its causes. In the vast majority of cases, arterial hypertension is essential, that is, a primary, independent disease with many causative factors, which requires constant treatment. Much less commonly, kidney disease, such as nephritis, causes hypertension. However, even primary (essential) hypertension involves kidney disease, which at the same time suffers from hypertension and maintains high blood pressure numbers.
According to their structure, the kidneys are represented by a tangle of small vessels, surrounded and penetrated by highly organized renal tissue. The kidneys perform several vital functions in the body; disruption of the functioning of these organs leads to serious problems for human health and life. Kidney function is directly related to blood pressure. If we are dealing with long-term untreated hypertension, then detection of kidney damage in this case is almost inevitable.
There is a third option for the relationship between kidney disease and arterial hypertension. There may be two diseases - hypertension and kidney disease, which arise separately, for different reasons, but over time reinforce each other. This effect of hypertension also explains the fact that some of the drugs used to treat arterial hypertension help stop the worsening of kidney disease, sometimes significantly changing the patient's prognosis in a favorable direction.
What is renal pressure
Renal pressure is a diastolic blood pressure indicator, the value of which deviates from the norm as a result of malfunctions in the renal system. The disease is diagnosed in 20-30% of hypertensive patients.
The kidneys filter the blood, remove excess fluid, breakdown products and harmful substances that accidentally enter the bloodstream.
Normal and impaired blood supply to the kidney
When the water-electrolyte balance is disturbed and the depressor system is suppressed, the organ begins to function incorrectly: the influx of plasma decreases, water and sodium are retained, causing swelling. Due to excess sodium ions, the walls of the arteries swell. Vessels become more sensitive.
Kidney receptors begin to synthesize an excess amount of the enzyme renin, which is transformed into angiotenis, and then into aldosterone. These elements are responsible for vascular tone, reduce the lumen of the arteries and lead to an increase in pressure.
Normally, lower (renal) pressure is in the range of 60-90 mmHg. Art.
The upper reading of the tonometer should not exceed 140 mmHg. Art. With hypertension of renal origin, blood pressure can increase to 250/150-170 mm Hg. Art.
The difference between is from 100 to 120 units.
The main sign of renal pressure is the ineffectiveness of antihypertensive drugs. This is explained by a specific regulatory mechanism.
Some disorders of the filtering organ can provoke a decrease in the tonometer numbers. But such a symptom is extremely rare.
General characteristics of the pathology
Among hypertensive patients, in 10% of patients, pressure surges are caused precisely by impaired renal function. At risk are people with diseases of the genitourinary system, most of them are men over 30 years old. When measuring indicators above normal, both upper (systolic) and lower (diastolic) pressure are found.
The kidneys filter the blood, regulate the volume of fluid in the body, remove excess sodium ions and cell waste products. Due to the push of blood from the heart there is a powerful flow to the periphery, and when the heart muscle relaxes, the blood returns back. At this moment, filtration occurs through the renal glomeruli. Nephrogenic hypertension begins at the time of deterioration of blood flow in the kidneys and glomerular dysfunction.
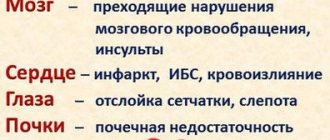
The body delays the removal of sodium salts and fluids, tissue swelling appears, the walls of blood vessels thicken, and due to an excess of secreted enzymes, sclerotic plaques appear in the arteries, narrowing the lumen of blood vessels. The return of blood to the heart weakens, vascular tone deteriorates, as a result of which blood pressure rises and remains at a high level. Long-term fixation at elevated levels (more than 140/90 mm Hg) leads to disruptions in the functioning of the cardiovascular system and to more serious complications.
Classification
Disturbances in the functioning of the renal arteries can occur with almost any kidney disease. However, the modern classification distinguishes 3 main groups.
Renoparenchymatous - the cause is damage to the parenchyma. This is the shell of the organ, consisting of a cortical and medulla layer. Its function is to regulate the accumulation and outflow of fluid. If there are disturbances in its functioning, reverse arterial blood flow appears, swelling occurs, and protein enters the blood and urine.
The following ailments cause diffuse changes in the parenchyma:
- lupus erythematosus, scleroderma and other systemic diseases;
- pyelonephritis and glomerulonephtritis are the most common causes;
- urolithiasis disease;
- renal tuberculosis;
- diabetes;
- both congenital and acquired.
The cause may also be a constantly acting mechanical factor - compression of the urinary tract, for example.
Renovascular - in this case, the cross-section of one or more arteries is reduced by 75%.
Bilateral stenosis - the actual narrowing of the vessel, or stenosis of one organ very quickly causes kidney failure. Fortunately, renovascular hypertension is not common: only 1–5% of all cases. However, it is precisely this that most often leads to the malignant course of the disease.
The causes of renovascular hypertension are:
- atherosclerosis – in 60–85%, especially in the older age group;
- abnormal development of blood vessels; mechanical compression - tumor, hematoma, cyst - lead to the same result.
A distinctive feature of this group is the low effectiveness of antihypertensive drugs even at very high blood pressure.
Mixed - this includes any combination of damage to the parenchyma and blood vessels. The cause may be cysts and tumors, nephroptosis, abnormalities of arterial vessels, and more.
Classification of the disease
There are several types of disease:
- Parenchymatous - occurs in diseases related to disorders of the functional activity of kidney tissue (parenchyma) - with polycystic disease, pyelonephritis, nephropathy, diabetes mellitus, kidney tuberculosis.
- Renovascular - diagnosed when there are changes in blood vessels in patients with atherosclerosis, thrombosis, or disturbances in the functioning of the walls of the renal artery. Increased renal pressure is caused by changes in the lumens of the renal arteries. This type of disease in most cases is detected in young patients under 10 years of age, and is often found in older people.
- Mixed nephrogenic - is a consequence of parenchymal dysfunction of the kidneys in combination with vascular changes.
Arterial hypertension can exist in two forms: benign and malignant. This depends on the rate of development of renal hypertension. Each of them has its own characteristics of the course, symptoms and complications if not treated in a timely manner.
How to diagnose
Diagnostics consists of several stages. First of all, you need to collect anamnestic data (time of onset of the disease, whether there is an effect from medications, whether there is heredity, connection with kidney disease, malignancy of the course). Based on a detailed survey, the origin of hypertension can be assumed.
Correct measurement of blood pressure is important. As a rule, with renal hypertension, a significant increase in numbers is detected, much more than with the usual form of the disease. There is an increase in diastolic pressure and a decrease in pulse pressure. When measuring, it is necessary to take into account the numbers from both the right and left hands. If there is a significant difference between them, then nonspecific aortoarteritis occurs.
Drug treatment
Various pharmaceutical drugs are used to treat renal hypertension. To select an effective treatment regimen, the doctor needs to establish the cause of the pathology. The specialist takes into account the size of glomerular filtration.
Captopril tablets
Therapy is aimed at:
- solving the main problem that negatively affects kidney function;
- pain relief;
- strengthening the body's defenses.
For renal pressure, the following groups of drugs are usually used:
- angiotensin-converting enzyme inhibitors. These include Captopril and Enalapril, Ramipril, Zocardis, Lisinopril;
- angiotensin receptor blockers. These are Losartan, Candesartan, Lorista and Valsartan. Your doctor may prescribe one of these drugs or a combination. The tablets effectively control blood pressure. Lorista-N contains several antihypertensive components that act on a complex of causes of high blood pressure;
- adrenergic blockers . Prazosin, Tamsulosin, Doxazosin, Coronal, Nebivolol, Terazosin effectively lower increased renal pressure. Such tablets are actively used for the secondary development of renal hypertension;
- thiazide diuretics . This group includes Chlorthalidone, Indapamide, Hydrochlorothiazide, Clopamide. They improve well-being by removing excess fluid from the body.
The following combinations are effective:
- diuretics and ACE inhibitors;
- diuretics with beta-blockers;
- calcium antagonists and ACE inhibitors;
- beta-blockers and calcium antagonists (dihydropyridine subgroup);
- diuretics and angiotensin II receptor antagonists.
In the treatment of renal hypertension, several important rules must be followed:
- Do not lower blood pressure sharply. This can cause kidney dysfunction;
- It is worth lowering the pressure slightly, to an acceptable level;
- eliminate factors that worsen the clinical picture and lead to renal failure;
- strengthen renal function.
Therapy is usually long-term, drugs are taken without interruption. If treatment is started in a timely manner, the pressure will normalize and will not lead to the development of complications.
The main danger of the pathology is that it progresses quickly and can affect the heart and brain. Therefore, the disease must be fought as quickly as possible. It happens that. Then hemodialysis, balloon angioplasty, nephrectomy, and donor organ transplantation are performed.
It is prohibited to select medications yourself. This is dangerous with serious complications
It is important to strictly follow all the doctor’s recommendations.
Symptoms of the disease
The complex is formed from the symptoms of hypertension and underlying kidney disease. The manifestation of symptoms depends on the form of the disease: benign develops gradually, malignant develops rapidly.
The first option is characterized by stable blood pressure with a predominant increase in diastolic pressure. Complaints of shortness of breath, loss of strength, discomfort in the heart.
The second option is characterized by increased blood pressure and a sharp weakening of vision (up to its complete loss). This is due to poor blood circulation in the retina. Complaints of acute headache accompanied by vomiting and dizziness.
Typical signs of the pathology are similar to the symptoms of arterial hypertension: dizziness and headaches, panic attacks, decreased brain activity ( memory problems, decreased concentration ).
Renal hypertension usually manifests itself against the background of kidney damage in certain diseases (pyelonephritis, diabetes mellitus, glomerulonephritis), so its symptoms are always associated with the underlying disease.
Common complaints include:
- pain in the lumbosacral spine;
- frequent urge to urinate;
- double increase in daily urine output;
- periodic increase in temperature;
- fatigue, general malaise.
The disease begins suddenly, the increase in pressure is accompanied by pain in the lumbar region. The tendency to hypertension can be inherited from hypertensive parents. Conventional medications designed to lower blood pressure do not work in such situations.
The clinical picture of PG depends on the degree of change in blood pressure, the initial condition of the kidneys, complications (heart failure, heart attack, damage to the retina and cerebral vessels).
Effect of the adrenal glands on blood pressure
The adrenal cortex plays an extremely important role in the regulation of blood pressure. A large number of hormones responsible for the regulation of blood pressure (catecholamines, aldosterone, glucocorticoids) are produced here.
Hypertension is often based on an excess amount of hormones produced, which determines the specific signs of hypertension and allows the patient to establish the correct diagnosis of the primary disease.
- Patients with pheochromocytoma are characterized by hypertensive crises, constantly elevated blood pressure, sweating, pale skin, interruptions in heart function, a feeling of fear, and tremor of the fingers. The combination of these signs indicates an excess of catecholamines. Hypertension in this case is constant and difficult to treat with medications.
- People suffering from hypercortisolism (Cushing's syndrome) experience a constant increase in blood pressure, excessive fat deposition on the torso and face, often increased blood sugar levels, and a tendency to bone fractures and infertility. Hypertensive crises are rare in people with Cushing's syndrome.
Treatment of kidney pressure
Treatment involves setting two tasks:
- restoration of the functioning of the kidneys and urinary system;
- therapy that eliminates the causes of renal hypertension.
It can be difficult to lower high blood pressure at home, so the doctor prescribes a combination of medications. Depending on the severity of the disease, the doctor prescribes medications from the following groups:
- diuretics, stopping the reabsorption of salts and fluids and accelerating their excretion in the urine;
- substances that reduce calcium absorption to reduce heart muscle tension;
- ACE inhibitors, which block enzymes in the body that cause hypertension;
- beta blockers.
In complex treatment, a hardware phonation procedure is used. The patient is given attachments of a vibroacoustics device, which helps speed up the removal of uric acid from the body, stabilize kidney function and restore blood pressure.
In severe stages of the disease, when folk remedies are not effective, and side symptoms from pills can irreparably harm the body, the doctor decides on surgical intervention. The operation is performed when polycystic disease, oncological tumors and congenital anomalies of the kidney structure are detected.
If a narrowing of the lumen of the adrenal artery is detected, the patient is prescribed balloon angioplasty. Occasionally, with severe damage to the kidney vessels, the surgeon decides to perform a nephrectomy - removal of the kidney. This happens when the disease is in an advanced state, when there is a risk to life.
Doctors confirm that renal hypertension can be cured by supplementing drug therapy with folk remedies:
- bearberry infusion lowers diastolic pressure;
- eating dill seeds cleanses the blood vessels of the kidneys;
- a collection of birch, chamomile, wild pear, cattail and centaury leaves reduces inflammation.
Each recipe must first be agreed with a specialist.
Comprehensive treatment of renal hypertension under the supervision of a physician should be supplemented by a strict diet with a high content of fruits and vegetables, minimizing the amount of salt consumed, avoiding alcohol and increasing physical activity. This will help reduce kidney pressure and avoid irreversible complications for people with severe forms of the disease.
Clinical treatments
Renal arterial hypertension should be strictly controlled by both the doctor and the patient himself to avoid serious consequences. Treatment should be comprehensive, aimed at eliminating the underlying cause of the disease. Drug therapy involves taking diuretics, which promote the process of removing fluid from the body, and adrenergic blockers, designed to expand the lumen of blood vessels and reduce pressure. The patient takes medications at home, but under the strict supervision of the attending physician. Remember, all medications have contraindications and side effects. Before using them, you must read the instructions.
Do not self-medicate. Only a specialist can prescribe appropriate treatment and give recommendations on how to reduce kidney pressure at home. Turning to traditional medicine will not give the desired effect, but it can slightly alleviate the patient’s condition.
You can use the following popular methods:
- Pour 1 tablespoon of clover flowers into 250 ml of boiling water. Leave for an hour. Drink half a glass 3 times a day.
- A decoction of 1 tablespoon of periwinkle leaves and a glass of water, boiled for half an hour, is effective for dilating blood vessels. Use in equal doses throughout the day.
- Pour a pinch of white mistletoe into a glass of boiling water, leave for several hours, and strain. Drink a few spoons 3 times a day.
Monitor your condition, systematically measure your blood pressure. If you experience symptoms of renal hypertension, consult your doctor immediately. Only timely measures will help maintain health.
How does pathology develop?
The development mechanism is due to a failure in the basic functions of the kidneys. The main one is filtration ability with the release of water and sodium. Filtration pressure arises due to the fact that there are some differences in the cross-section of the vessel that brings blood and the one that takes it away.
Due to various pathologies in the kidneys, there is a decrease in the normal flow of blood to this organ. Ischemia of the juxto-glomerular apparatus occurs. For this reason, its cellular system undergoes hyperplastic and hypertrophic changes. As a result, a large amount of renin is produced. It combines with a special substance (globulin), angiotensin 1 is formed, from which, as a result of the cleavage of one molecule, angiotensin 2 is obtained.
This compound has a very pronounced vasoconstrictor effect. In parallel with this, a large amount of angiotensin produced induces the production of the hormone aldosterone, which is capable of retaining sodium in the body. Sodium fills the renal arterial vessels, or rather accumulates in their walls, increasing their sensitivity to catecholamine hormones.
Complications of arterial hypertension
An important link in the pathogenesis will be a decrease in the production of angiotensinase by the kidney. In an organ without pathology, it is produced in sufficient quantities and breaks down angiotensin 2, thereby preventing its vasospastic effect. Damage to the kidney tissue leads to a decrease in its effect.
Renal hypertension is also associated with the fact that in diseases the renal medulla secretes few compounds that reduce blood pressure (prostaglandins, kinins). It follows that such a disease occurs due to a decrease in the activity of angiotensinase, the synthesis of prostocyclins and kinins and the activation of the renin-angiotensin-aldosterone system.
What is this
An insidious disease associated with blood pressure exceeding the mercury reading on a tonometer and resulting from any of the kidney dysfunctions is called renal hypertension. Often the disease begins to develop at a young age, which distinguishes it from the classic type of disease. Increasingly, cases of complaints are being recorded from people under 40 years of age.
For the disease to start, it is necessary to have any kidney dysfunction. The kidneys are an organ that helps remove fluid from the body. If for any reason their functioning is disrupted, the blood flow to them decreases, the water in them stagnates, and the result of the malfunction is swelling. Damaged receptors release enzymes that lead to an increase in vascular tension and, as a result, blood pressure. In parallel with this, the production of substances that could reduce tone decreases, and the receptors are subjected to even stronger negative effects.
Causes
The disease is classified into 2 types: renoparenchymal and renovascular. Based on the type of illness, provoking factors are identified.
The causes of diffuse kidney damage (renoparenchymal hypertension) are also divided into groups:
- Anomalies in development. These include hypoplasia (the kidneys are reduced in size from birth), complete and incomplete organ duplication, and cysts.
- Inflammatory process in tissues. This group includes cases of such common diseases as pyelonephritis and glomerulonephritis.
The causes of the renovascular type of disease, or as it is also called in medicine – renovascular hypertension, also have their own sublevels. It is worth noting that in the case of increased blood pressure in children, 90% are diagnosed with renovascular hypertension. In adults, this percentage is slightly lower - 55.
Congenital causes of pathology:
- renal artery stenosis;
- local narrowing of the aortic lumen or a complete break in the isthmus region;
- diffuse and limited protrusion of the wall of the arterial vessel.
Acquired causes contributing to the development of renal hypertension:
- accumulation of cholesterol plaques that narrow or block the lumen;
- acute blockage of the main trunks of the renal artery;
- thickening of the fibrous capsule of the kidney with the degeneration of fiber into fibrous tissue, which is tightly connected to nearby organs;
- external compression of the renal arteries.
Important! Cases have been recorded where specialists diagnosed a mixed form of pathology.
Manifestations
The symptoms of renal hypertension are very varied. In general, the clinical picture consists of symptoms of kidney damage and arterial hypertension. The degree of severity depends on the form of the disease. In case of malignancy, the clinical manifestations are bright, the disease develops quickly. And with a benign form, the manifestations are less pronounced, the dynamics of the disease is gradual.
The benign form has a fairly stable pressure, while both diastolic and systolic increases. Although a little more diastolic. The patient is concerned about fatigue, weakness, shortness of breath, headache, pain in the heart area.
But the malignant type of renal hypertension is characterized by a large increase in pressure and a decrease in visual acuity due to impaired blood supply to the retina. I am worried about a severe headache, dizziness, and vomiting may occur.
Common signs for both forms are attacks of palpitations, panic, and decreased cognitive function (the person does not learn material well and does not remember many things). The patient is constantly plagued by headaches and dizziness.
Since renal hypertension is always associated with kidney pathology, in addition to high blood pressure, there are also symptoms from the kidneys:
- pain in the lumbar region;
- increased urge to urinate;
- increase in the volume of urine excreted;
- Sometimes your body temperature may rise.
Signs of the kidneys depend on the genesis of the disease (pyelonephritis, diabetes mellitus)
An important feature that unites all types of the disease under discussion is refractoriness to various groups of antihypertensive drugs. It is important to note that the severity of the clinic is directly dependent on concomitant diseases (heart failure, heart attack)
Hypertension develops in stages
Symptoms of renal hypertension
Symptoms of renal hypertension:
- high renal and cardiac pressure;
- severe headaches;
- increase in heart rate;
- fatigue in the absence of strenuous activity;
- eye hemorrhages;
- retinal damage;
- swelling of the optic nerve;
- black spots before the eyes;
- blurred vision, loss of focus;
- swelling of the limbs;
- lower back pain;
- sudden pressure surges.
If these symptoms appear, you should not postpone your visit to the doctor. During the examination, a specialist may detect noise in the arteries. With renal arterial hypertension, pressure readings in each arm will be different, and a urine test will show the presence of protein.
There are two forms of arterial hypertension of renal origin: malignant and benign. They can be distinguished by their characteristic symptoms:
- malignant hypertension develops quickly: the lower pressure jumps sharply to 120 mmHg, leveling off with the upper one; the patient’s vision suffers, severe pain appears in the back of the head, dizziness, and vomiting occur;
- benign hypertension develops gradually: pressure increases evenly, but it is not possible to bring it down with antihypertensive drugs; there is pain in the frontal lobe, lethargy, difficulty breathing, the heart beats faster, pulsation is heard with pain in the sternum.
Severe headaches may be a sign of illness
Causes and mechanism of development
There are quite a lot of factors affecting the condition and functioning of the cardiovascular system.
Most of them can lead to an increase or decrease in blood pressure. In relation to renal hypertension, there are 3 main causes:
- Retention of sodium and water ions is a common mechanism for the formation of hypertension when parenchyma is damaged. With an increase in the amount of incoming blood, it ultimately leads to impaired filtration and a kind of internal edema. The volume of extracellular fluid increases, which provokes an increase in blood pressure. Sodium ions are retained along with water.
In response, the production of digitalis-like factor increases, which reduces sodium reabsorption. But with kidney disease, the hormone is produced too actively, which leads to vascular hypertonicity and, accordingly, increases blood pressure.
- Activation of the RAAS renin-angiotensin-aldosterone system. Renin is one of the hormones that promotes the breakdown of protein, and in itself does not affect the condition of blood vessels. However, as the arteries narrow, renin production increases.
The hormone reacts with α-2-globulin, together with which it forms an extremely active substance - angiotensin-II. The latter significantly increases blood pressure and provokes increased synthesis of aldosterone.
general information
Renal hypertension is a kidney disease that occurs for various reasons (depending on classification). Nominally, hypertension is an increase in pressure that occurs in the kidneys and leads to disruption of the blood filtration process.
If we consider the disease in more detail, we can see that it often develops against the background of another disease and occurs as a complication:
- renal artery stenosis;
- pyelonephritis;
- glomerular nephritis;
- diabetic nephropathy;
- nephropathy in pregnant women.
The essence of the problem is that the level of pressure in the organs increases, this leads to the development of pathological changes, the growth of fibrous tissue, and inflammation. Polycystic disease often leads to this disease.
However, an increase in pressure can be caused by other factors; it often occurs due to pathological changes, developmental anomalies of a congenital or acquired nature.
Principle of disease development:
- large vessels of the kidneys narrow;
- due to what the glomeruli are affected;
- pathological processes occur;
- the first signs of the disease appear.
Narrowing of large arteries and damage to the glomeruli leads to disruption of the filtration functions of organs. Against this background, various problems appear: the level of protein in the blood increases, the kidneys cannot fully perform their functions.
This leads to toxic damage to the body, and gradually, as the disease progresses, acute or chronic renal and heart failure develops.
Causes, symptoms and specifics of renal hypertension
When certain diseases occur, physiological mechanisms are disrupted, and a persistent increase in blood pressure occurs.
Pathologies that can cause secondary renal hypertension include the following:
- chronic or acute inflammatory processes in the renal filter system;
- polycystic kidney disease;
- tuberculous contamination of renal tissue;
- hydronephrosis;
- amyloidosis;
- disturbances in the functioning of the renal tissue caused by compression of the parenchyma by the enlarged uterus of the fetus in women;
- congenital or acquired narrowing of the renal arteries;
- general systemic connective tissue pathologies.
The specificity of renal hypertension is associated with the mechanism of its occurrence; due to water retention in the body, not only the afterload on the myocardium increases, but also the preload, which is manifested by an increase in not only systolic, but also diastolic pressure. In parallel, the presence of pain in the lumbar region is usually observed, which is associated with the primary disease that caused the development of hypertension.
Renal arterial hypertension has characteristic symptoms
There are both specific and nonspecific clinical manifestations of this disease. Common ones include:
- decreased performance;
- the appearance of constant headache;
- increase in heart rate;
- the appearance of excessive swelling of the lower extremities and face;
- bluish coloration of peripheral tissues, redness of the sclera;
- increased irritability.
More specific symptoms of renal hypertension include:
- increase in systolic and diastolic blood pressure indicators;
- the appearance of pain in the lumbar region;
- decrease in daily urine output;
- temperature increase;
- visual impairment;
- noise during auscultation in the projection area of the branch of the renal arteries;
- the presence of different blood pressure indicators on the right and left limbs.
Diagnostics
Doctors with extensive experience can identify renal hypertension in the initial stages. Qualified specialists have the opportunity not only to timely diagnose the syndrome of renal arterial hypertension, but also to select a set of medicinal measures that can relieve the main symptoms of the disease and stop pressure surges.
To make a differential diagnosis of renal hypertension, it is necessary to constantly monitor blood pressure levels over a long period of time. If within 30 days, when measuring blood pressure, a reading of 140/90 mm Hg is detected. Art., the diagnosis is confirmed. In the presence of pronounced pathologies in the activity of the kidneys, renal hypertension is diagnosed. If the disease is detected, it is necessary to carry out comprehensive treatment of renal hypertension.
To confirm the diagnosis, the following studies are performed:
- Analysis of urine.
- Ultrasound of the kidneys.
- Urography.
- Scintigraphy.
- Angiography.
- MRI and CT.
- Biopsy.
Diagnosis and treatment of hypertension
The main diagnostic signs are the condition of the left ventricle and fundus, diastolic pressure indicators.
Making a diagnosis requires an examination that can reveal all these signs, as well as other manifestations of the underlying disease and the consequences of hypertension.
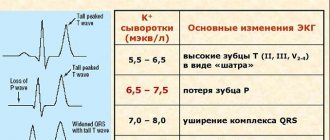
The patient undergoes an ECG, ultrasound of the heart, is examined by an ophthalmologist, and tests are taken. Pressure indicators must be monitored over time in order to have an idea of how persistent hypertension has become and what the systolic and diastolic pressure numbers are. The kidneys, adrenal glands, aorta, and renal arteries are subject to examination. It is necessary to determine the amount of sodium and potassium and hormones in the blood and urine. Methods such as x-rays with radioisotopes and vascular angiography are used.
Clinical signs
- Murmurs in the area of the arteries of the kidneys;
- Some protein in urine;
- Decrease in specific gravity of urine;
- Asymmetry of pressure indicators on the left and right hands;
- Increased size of the left ventricle.
The reason for prescribing an examination, as a rule, is an increase in blood pressure. In this case, there may be accompanying symptoms, but they may not be present for some time. It is necessary to monitor blood pressure at different times, with different loads and in different positions of the patient’s body.
When hypertension is detected, other studies are prescribed that will present a picture of the state of the kidneys, their function, and will allow us to assess the condition of the blood vessels and how they work.
Once diagnosed, treatment should not be delayed. It depends on the severity and extent of the lesions, on the general condition of the patient and his individual characteristics.
Conservative treatment
This method of treatment is the main one. Its goal is, if possible, to get rid of the underlying disease and maintain or restore kidney function. One of the methods of therapy is diet. This may be sufficient for the treatment of transient hypertension.
Diet features
The so-called table No. 7 is prescribed, the main limitations of which are a decrease in the amount of salt and protein. A gradual replacement of animal proteins with plant proteins is provided. The main limitation concerns sodium and products containing it. It is necessary to strictly limit salt, do not add salt to dishes during cooking, exclude canned foods, smoked foods, hard cheeses, sauerkraut, and rye bread.
Other treatments
If diet is not enough, then medications are prescribed:
Stories from our readers “I was able to cure my KIDNEYS with the help of a simple remedy, which I learned about from an article by a UROLOGIST with 24 years of experience, Pushkar D.Yu...” Elena Mikhailova, Crimea Read more »
- Diuretics;
- Adrenergic blockers;
- Antihypertensive drugs.
Treatment with a vibroacoustic device can be effective. This method is called phonation of the kidneys, that is, treatment with sound microvibrations. If it is possible to restore kidney function, then blood pressure normalizes.
When the disease develops to the terminal stage and the patient has chronic renal failure, he needs hemodialysis, otherwise poisoning of the body with metabolic products occurs.
Surgical treatment is prescribed for urolithiasis, as well as irreversible changes in the kidneys and the possibility of transplantation. Another surgical method is used to eliminate it - balloon angioplasty. As a result of its use, a special balloon is inserted into the narrowed area of the vessel, which is inflated to the required size and supports the walls, ensuring normal lumen of the vessel.
With timely treatment, blood pressure can be corrected: it can be reduced and stabilized. This will definitely bring positive results, as damaging factors will go away. The general condition and well-being of the patient will improve.
Diagnostic measures
To prescribe the correct treatment, the doctor must conduct a comprehensive examination of the body, taking into account the nature of the disease and the individual characteristics of the body. It is important to identify the cause of high blood pressure, because it is not always a consequence of kidney disease.
Diagnosis of renal hypertension includes the following procedures:
- Urine and blood tests.
An increased content of protein, as well as leukocytes and erythrocytes, may indicate the presence of a disease, even if there is no increase in pressure yet. Laboratory diagnostic methods make it possible to determine the level of microelements, especially potassium and sodium.
- Fundus examination.
Arterial hypertension affects the condition of the fundus. The central artery narrows and hemorrhage may occur. A disruption in the blood supply to the optic nerve leads to retinal edema. Vision deteriorates. With primary hypertension, visual impairment is usually not observed.
- Ultrasound examination of the kidneys.
When performing an ultrasound, the doctor examines the structure of the walls of the arteries, determines whether they are affected, how effective the blood supply to the organ is, and whether the patient has a tumor.
- Renography of the kidneys (x-ray method of studying the kidneys using radioactive components);
One of the most objective diagnostic methods that allows you to determine how the kidneys cope with their functional load. Helps identify organ pathologies in the early stages of disease development.
- Survey and excretory urography of the kidneys
The general condition of the kidneys is examined and their excretory function is analyzed.
These methods are contraindicated in patients with liver and kidney failure.
- Vascular angiography
As a result of this study, the location where the pathology exists, as well as its size and degree of development, is determined. The method is used to make an accurate diagnosis.
A comprehensive diagnosis of the disease also includes studies of the functioning of other organs: the heart, lungs, blood vessels, and organs of the genitourinary system. The doctor pays attention to pressure readings and its duration. If a patient’s blood pressure remains at least 140-90 for several weeks, a diagnosis of hypertension should be considered. If abnormalities in the functioning of the kidneys are detected, a diagnosis of renal hypertension is made.
Tired of fighting kidney disease?
SWELLING of the face and legs, PAIN in the lower back, CONSTANT weakness and fatigue, painful urination? If you have these symptoms, there is a 95% chance of kidney disease.
If you care about your health , then read the opinion of a urologist with 24 years of experience. In his article he talks about RENON DUO capsules.
This is a fast-acting German remedy for kidney restoration, which has been used all over the world for many years. The uniqueness of the drug lies in:
- Eliminates the cause of pain and brings the kidneys to their original state.
- German capsules eliminate pain already during the first course of use and help to completely cure the disease.
- There are no side effects and no allergic reactions.