Thrombosis of the hemorrhoid is one of the dangerous complications of hemorrhoids. It is a blockage of a swollen hemorrhoidal vein by a dense, coagulated blood clot. This causes hemodynamic disturbances in the damaged area and severe pain. The disease was assigned an ICD 10 (International Classification of Diseases) code K64 and a marker “hemorrhoids and perianal venous thrombosis.”
Thrombosis of the node in hemorrhoids is a serious complication, which in the absence of medical care can lead to even more dangerous consequences
Causes of thrombosis in hemorrhoids
Thrombosis of the hemorrhoidal node is a common complication of hemorrhoids, which is associated with impaired blood circulation in the anorectal area, the formation of a blood clot (thrombus) in the cavernous plexuses of the rectum.
The patient feels severe pain in the rectum area, not associated with the process of defecation, and a constant sensation of a foreign body in the anus. According to the ICD, hemorrhoidal thrombosis has code K.64.5
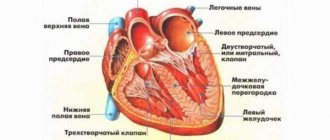
The rectum ampulla is surrounded by venous caverns, which, together with the anal sphincter, prevent the arbitrary release of gases and feces from the anus. These formations are permeated with vessels, which, under the influence of various negative factors, lose their tone. As a result, the blood begins to stagnate, the veins expand and become deformed. This is how hemorrhoidal nodules are formed.
In the process of life, work, and sports, a person’s intra-abdominal pressure changes. Deformed vessels are not able to cope with it, so the body turns on “protection”, turning stagnant blood into a blood clot. This is the main cause of thrombosis or thrombophlebitis. Contribute to the development of pathology:
- hereditary predisposition;
- bad habits;
- alcoholism, diet violations;
- constipation or diarrhea;
- constant lifting of weights;
- physical inactivity;
- "sedentary work;
- chronic inflammation of the pelvic organs;
- pregnancy;
- low temperatures.
Thrombosis of internal hemorrhoids develops due to pinching of the cones by the sphincter and occurs rarely .
Reasons for development
The pathogenesis of thrombus formation is based on the mechanism of emigration of leukocytes to the site of inflammation or damage to the vessel. When rolling (rolling) blood cells over the inflamed area, some of them stick, forming the basis for the formation of a blood clot. At the site of cell accumulation, the concentration of fibrin fibers increases, from which a blood clot is formed.
As the pathological process develops, the clot enlarges, blocking the flow of blood into the thrombosed node and provoking necrosis of the vessel area.
Hemorrhoidal thrombosis can develop for the following reasons:
- Acute hemorrhoids. Exacerbation of varicose veins of hemorrhoidal vessels causes severe pain and spasm of the affected veins. This leads to blood stagnation, the formation of pathological clots and a complete cessation of blood supply to thrombosed nodes. The probability of thrombosis with hemorrhoids is more than 27%. In 17.7% of patients, this pathology develops against the background of an acute form of hemorrhoids.
- Impaired intestinal motility due to poor nutrition. Consuming large amounts of spices, marinades, bitter foods and alcoholic beverages stimulates blood flow to the pelvis and dilation of the anal veins. A lack of plant foods that contain dietary fiber provokes constipation, increased intra-abdominal pressure during bowel movements and the occurrence of venous stagnation. An equally dangerous risk factor is the opposite phenomenon - diarrhea.
- Pregnancy and childbirth. The pressure of an enlarged uterus in the 2-3 trimester of pregnancy causes a disturbance in the outflow of the inferior vena cava, which also affects blood circulation in the rectal vessels. Concomitant hormonal changes provoke a weakening of intestinal motility, and straining during the birth of a child leads to a sharp increase in intra-abdominal pressure and excessive filling of the anal veins. Hemorrhoids and thrombophlebitis of anorectal vessels are common complications of pregnancy and childbirth.
- Damage to the hemorrhoid. Trauma to the node provokes the active release of inflammatory mediators and tissue damage, which causes an influx of immune cells (leukocytes) and blood cells that provide blood clotting (platelets). The risk of a blood clot when a node is injured is higher than against the background of chronic hemorrhoids.
Important information: How to treat hepatic vein (liver) thrombosis and symptoms of Budd-Chiari syndrome
Additional risk factors for the development of pathology are hypothermia of the anorectal area and sedentary work.
What is the danger of thrombophlebitis of hemorrhoidal veins
In ordinary life, it is possible to injure the wall of the external hemorrhoid when performing hygiene procedures. After this, with normal blood clotting, thrombosis of the blood vessels occurs, which stops the bleeding. Then, the blood clot resolves without any consequences. But if thrombus formation occurs without injury, against the background of negative changes in the circulatory system, a condition that is dangerous to human life arises:
- acute thrombosis requiring urgent surgery;
- sepsis;
- atypia with transformation into cancer;
- detachment of a blood clot from the cavity wall with transfer through the bloodstream to the coronaries, cerebral vessels, pulmonary artery and the development of stroke, heart attack, pulmonary embolism.
Each condition can be fatal. That is why any person suffering from hemorrhoidal disease must consult a doctor.
Description of the disease
As the name of the disease suggests, thrombosis of the hemorrhoid does not arise out of thin air: it requires a hemorrhoidal lump and a blood clot in it. In 8 out of 10 cases, the disease is preceded by existing chronic hemorrhoids . Relatively rarely, thrombosis occurs acutely - almost simultaneously with the appearance of the hemorrhoidal lump itself.
The mechanism of development of the disease is as follows:
- In the vein of the perianal region affected by hemorrhoids, as a result of various damaging factors, the integrity of the inner wall of the vessel is disrupted.
- This leads to the risk of bleeding - to prevent it, a blood clot or thrombus is formed in the lumen of the vein, which clogs the gap in the vessel wall.
- The resulting blood clot interferes with normal blood flow in the vein, leading to stagnation of blood in it.
- Swelling and local inflammation occurs around the thrombosed area of the vein .
- Severe pain and discomfort occurs in the anal area, which is not directly related to the size of the blood clot. Even with a small blood clot, the pain will be severe and constant.
- For obvious reasons, a person begins to experience fear of defecation - this leads to constipation, which further increases congestion in the rectal area and aggravates the course of the disease.
- Emptying the bowel after prolonged constipation leads to damage to enlarged and thrombosed hemorrhoids - the pain intensifies.
This vicious circle of pain develops in approximately 30-40% of patients with chronic hemorrhoids.
Types and degrees of disease
The localization of hemorrhoids with thrombosis is the basis of the classification:
- outer;
- interior;
- combined thrombophlebitis of the node.
The severity of symptoms determines the severity of the pathology:
- first - there are no signs of inflammation of the caverns;
- second - thrombosed nodes of any location give the first symptoms: pain, bruising, swelling of the anus ;
- third - inflammation affects nearby tissues, complications arise.
According to the severity of the process, hemorrhoidal thrombosis is distinguished between acute (complicated) and chronic (recurrent).
How long does it take for a blood clot to dissolve?
Despite the fact that the main pathology (hemorrhoids) takes a long time to treat, the clot in the node resolves within a short period of time (no more than 5 days). This is due to the fact that the formations cut off from the blood supply are quickly replaced by connective tissue.
It is important to take into account that thrombosis of the hemorrhoid quickly resolves only with the timely use of drug therapy. If the disease has reached the third stage and is accompanied by complications, then pain and inflammation may not go away even after the nodes disappear.
Clinical symptoms
The photo shows live external thrombosis of a hemorrhoid.
The very first symptom or sign of hemorrhoidal thrombosis is sudden pain that is accompanied by discomfort in the anorectal area. The nodule formed as a result of thrombosis begins to grow, and the person feels a foreign body in the anus. The nature of the pain changes. If with hemorrhoids of any localization the pain is caused by the act of defecation, then a blood clot in the venous plexus causes constant pain that is not associated with anything.
The clinical picture develops gradually and corresponds to the stages of pathology, which are presented in the table.
| Pathology stage | Symptoms and signs |
| First |
|
| Second |
|
| Third |
|
Types and degrees of thrombosis
Based on the location of the formation of a blood clot, a distinction is made between thrombosis of the external hemorrhoid, if the external cavernous formations are damaged, and thrombosis of the internal hemorrhoid, if platelets accumulate in the veins of the submucosal rectum.
If blood vessels located both below and above the anus are affected, then experts talk about combined thrombophlebitis of hemorrhoids.
The pathological condition develops gradually, this allows us to distinguish three successive stages or degrees in its progression. For ease of gradation, we have presented their distinctive features in the form of an informative table.
| Sign | 1st degree | 2nd degree | 3rd degree |
| Blood clot sizes | Small | Average | Significant size |
| Elasticity of the knot | High degree of elasticity | Medium elastic | Tight |
| Node color | Reddish tint | Dark red or bluish | There are areas that are necrotic or covered with a white coating |
| Severity of pain syndrome | The pain can be tolerated, the discomfort intensifies when touching the node | Severe pain | Unbearable pain |
| Swelling of the perianal area | Not pronounced | The affected node and the area around it are swollen and red | Severe swelling and redness affects the entire anorectal area |
| Inflammation | Virtually absent | The nodes are inflamed | Inflammation covers not only the node, but also the subcutaneous tissue |
| Rectal valve spasm | Absent | Present, but intermittent | Constantly expressed spasm, which only intensifies the pain |
| Bleeding | Absent (possibly due to damage to the unit) | Most often absent | Available |
Possible complications
The progression of thrombophlebitis of hemorrhoids causes a number of complications requiring medical intervention:
- bleeding;
- varicose veins of the anal veins;
- abscess of soft tissues of the perianal area;
- necrosis of thrombosed nodes with symptoms of severe intoxication;
- addition of a secondary infection;
- anal dermatitis;
- postoperative fistulas, suture dehiscence, narrowing of the anus.
Any of the complications requires prompt attention to a specialist.
Causes and risk factors
The immediate cause of hemorrhoidal thrombosis is the formation of a blood clot. Its appearance can be triggered by:
- Pushing during bowel movements, during childbirth, or when lifting heavy objects . As a result of pushing, intra-abdominal pressure increases significantly, which the walls of the vessels may not be able to withstand - they are damaged. As a result of straining during bowel movements, internal hemorrhoids may fall out, which are subsequently pinched by the rectal sphincter and thromboses - this is how internal thrombosis occurs.
- Injuries to the tissues of the anus and rectum during anal sex or the use of sex toys can lead to damage to the walls of blood vessels.
The risk of developing the disease increases many times under the influence of the following factors:
- Hypothermia of the pelvic area, as a result of which the vessels narrow and the outflow of blood from them becomes difficult. As a result of congestion, deformation of the vascular wall can occur.
- Increased intra-abdominal pressure as a result of a hacking cough or in late pregnancy.
- Increased blood clotting, which itself provokes thrombus formation.
- Chronic hemorrhoids.
- Poor nutrition, alcohol abuse.
- Inflammatory and tumor diseases of the pelvic organs.
- Physical inactivity.
Do you know how to treat varicose veins during pregnancy so that they do not develop into thrombosis and cause problems with motherhood? Learn about safe therapy methods. Periarteritis nodosa is one of the little-studied but very dangerous diseases. Find out everything about its timely diagnosis and treatment methods.
Diagnostics
As a rule, an accurate diagnosis of hemorrhoidal vein thrombosis is made quickly, based on a visual examination of the anorectal area, a characteristic clinic. Thrombosis of the external hemorrhoid is localized under the pectineal line; it is inflamed, cyanotic, and painful. Internal - accompanied by a pronounced furrow between the prolapsed node and the swollen skin of the anorectal area. If there is no prolapse, a revision of the rectum is needed, which is carried out under local anesthesia due to unbearable pain.
Laboratory and instrumental methods are used:
- OAC, OAM – assessment of the patient’s general condition;
- coagulogram, electrocoagulography, detailed hemostasiogram - determine signs of hemostasis impairment;
- rectoscopy - for severe pain with suspected cancer, strangulation of a polyp, paraproctitis in the acute phase.
Without an accurate diagnosis, it is impossible to prescribe adequate therapy.
How does acute thrombosis of the external hemorrhoid manifest?
Patients with acute thrombosis of the external hemorrhoid complain of the appearance
protrusions, “bumps” (neoplasms) and/or pain of varying intensity in the anus. The size of the “bump” can range from several millimeters to several centimeters and is often accompanied by swelling of the surrounding tissues (up to the entire circumference of the anal canal). In some patients, the disease proceeds without pain, but most assess the pain as significant or unbearable.
To assess the degree of pain, a special visual analogue scale is used, in which you can independently determine the severity of pain. After all, this is the key point when choosing a treatment method. Surgical treatment will be most effective when the severity of pain is 7 or more points, while for pain up to 4 points, a conservative method of treatment can be considered optimal.
Rice. Visual analogue scale for pain assessment.
Pain usually worsens during bowel movements and/or sitting. The pain and swelling can be severe, even unbearable for several days. The intensity of pain depends on the size of the blood clot and its location in relation to the anal sphincter muscles. In general, manifestations of the disease can persist for several weeks, in exceptional cases longer. Sometimes spontaneous evacuation of a blood clot from a hemorrhoid occurs. This is preceded by necrosis (destruction) of the skin over the thrombus, and the thrombus seems to “fall out” of the node. Externally, this is accompanied by a sensation of a “bursting” ball and the release of a small amount of blood. Usually, after evacuation of the blood clot, the pain and discomfort in the anus gradually decrease. However, necrosis of the mucous membrane above the thrombus does not always end only with the evacuation of the thrombus; necrosis can continue to spread to the hemorrhoid itself and surrounding tissues, which is why this condition requires consultation with a specialist. After acute thrombosis subsides, the patient is most often left with so-called “skin fringes” - excess skin where the thrombosis was. They do not require medical treatment, but may cause cosmetic discomfort.
Modern methods of treatment
How exactly to treat hemorrhoidal thrombosis depends on the location of the pathological process, the stage of the disease, and the degree of severity. A distinction is made between drug therapy and surgical intervention. Sometimes they are combined. Folk recipes are used as background.
Indications for prescribing medications are:
- acute process;
- prevention of complications;
- relapse prevention;
- preparation for surgery;
- postoperative rehabilitation.
Conservative therapy for hemorrhoidal thrombosis is carried out at home: preference is given to tablets, suppositories, ointments, lotions and compresses. Conservative methods of treating thrombosed hemorrhoids do not provide a long-term therapeutic effect, and the risk of relapse is high.
Treatment of thrombosis at home
There are many methods of pain relief. Acute hemorrhoids can be treated with folk remedies only at the beginning of the disease! If thrombosis worsens, immediately contact the clinic! The specialist will make a diagnosis, prescribe appropriate medications and give recommendations on how to treat the disease at any stage of its development. In the first aid kit of a person suffering from hemorrhoids, in case of exacerbation, there should be medicines: “Detralex” and an ointment that relieves inflammation (Trombless, Heparin).
Symptoms, treatment and prevention of hemorrhoidal thrombosis.
Hemorrhoids are considered to be a “sore” that is embarrassing to talk about not only to loved ones, but also to specialists. This is why many people prefer to suffer in silence, seeing a proctologist either with a severe type of illness or with a serious complication.
The most common undesirable consequence is thrombosis of the hemorrhoid, or thrombophlebitis. The pain syndrome in this condition is so pronounced that a person is simply forced to seek medical help.
Pills
They are used as drugs that have a systemic effect, do not irritate the intestines, to dissolve blood clots, normalize microcirculation, and relieve inflammation.
Venotonics
Systemic drugs that increase vascular tone, stimulate the outflow of blood from hemorrhoids, and relieve congestion.
Detralex
Detralex tablets. They are the drug of choice. They act actively at the first signs of the disease. Particularly effective for external hemorrhoids.
| Composition, active substance | Diosmin, hesperidin |
| Mechanism of action of the drug | Detralex:
|
| Indications | Thrombosis of hemorrhoids in external and rectal localization |
| Contraindications | Intolerance to medication ingredients |
| Side effects | Allergization of the body |
| Mode of application | During an exacerbation - 4 days, 6 tablets in two doses, the next three days - 4 tablets. Then, 2 tablets/day until completely absorbed. Course up to 3 months |
| Compatibility with other drugs | No information |
| Use during pregnancy and lactation | Not recommended |
| special instructions | No data |
| Price | From 640 rubles |
Phlebodia 600
Phlebodia 600 capsules. The drug tones the veins, makes them stronger, and balances venous blood flow.
| Composition, active substance | Diosmin |
| Mechanism of action of the drug | Phlebodia 600:
|
| Indications | Thrombosis of any location and form |
| Contraindications | Individual intolerance to ingredients |
| Side effects | Headaches, dyspepsia |
| Mode of application | A couple of tablets with meals to relieve the severity of the process. Then – capsule/day for no more than 3 months |
| Compatibility with other drugs | No data available |
| Use during pregnancy and lactation | By agreement with the doctor |
| special instructions | No data |
| Price | From 850 rubles |
Troxevasin
Troxevasin tablets. Venotonic with antioxidant, anti-inflammatory, angioprotective properties.
| Composition, active substance | Troxerutin |
| Mechanism of action of the drug | Troxevasin:
|
| Indications |
|
| Contraindications | Component intolerance |
| Side effects | Allergization |
| Mode of application | One tablet three times a day for two weeks, until the severity of the process is relieved, then twice a day until the clot is completely absorbed |
| Compatibility with other drugs | Vitamin C enhances the effect of the medicine |
| Use during pregnancy and lactation | From the second trimester after consultation with a doctor |
| special instructions | No |
| Price | From 300 rubles |
Non-steroidal anti-inflammatory drugs (NSAIDs)
Drugs of the NSAID group are indicated for relieving inflammation during thrombosis of external and internal hemorrhoids, and for relieving pain. They are used with caution because they can thin the blood and, in case of overdose, cause bleeding of hemorrhoids.
Diclofenac
Diclofenac tablets. The drug quickly and effectively relieves pain, inflammation, and promotes the resorption of blood clots.
| Composition, active substance | Diclofenac, lidocaine |
| Mechanism of action of the drug | Diclofenac:
|
| Indications |
|
| Contraindications |
|
| Side effects |
|
| Mode of application | One capsule/day after meals until the severity of the process is relieved |
| Compatibility with other drugs | Does not combine with non-narcotic analgesics (Amidopyrine), antiplatelet agents (Cardiomagnyl), increases the toxicity of cytostatics (Methotrexate), reduces the antihypertensive effect of antihypertensive medications (Renitek) |
| Use during pregnancy and lactation | Forbidden |
| special instructions | You cannot drive or operate precision instruments. |
| Price | From 50 rubles |
Nise
Nise tablets. Anti-inflammatory, analgesic mono-drug. Prostaglandin synthesis corrector.
| Composition, active substance | Nimesulide |
| Mechanism of action of the drug | Nise:
|
| Indications |
|
| Contraindications |
|
| Side effects |
|
| Mode of application | 1 piece twice a day, in a minimum short course |
| Compatibility with other drugs | Antiplatelet agents (Cardiomagnyl) enhance their properties in the presence of the drug, diuretics lose their properties. Incompatible with cytostatics (Methotrexate) and sulfonamides (Streptocide) |
| Use during pregnancy and lactation | Contraindicated |
| special instructions | No data |
| Price | From 182 rubles |
Reasons for appearance
Chronic circulatory disorders in the cavernous veins and atrophy of the ligamentous apparatus of the nodes are the main causes of the pathology. Under the influence of these factors, enlarged hemorrhoid cones become displaced and fall out of the anus. Dystrophic processes and a decrease in the density of closure of the anus lead to their further displacement.
Even in small doses, alcohol can cause hemorrhoids.
Risk factors that can cause inflammation:
- Alcohol and tobacco;
- Heavy physical labor and lifting heavy objects;
- Prolonged sitting position;
- Poor nutrition and obesity;
- Gastrointestinal diseases;
- Pregnancy and childbirth.
Scientists say that inflammation in the anal area can even cause stress!
Most often, the pathology manifests itself during pregnancy and after childbirth, after lifting heavy objects, or after a sedentary profession.
Candles and ointments
Thrombosis of the external hemorrhoid is most effectively treated with ointments or suppositories. The goal of therapy is to relieve pain and dissolve blood clots. It is often combined with tablet medications.
Anticoagulants
The most effective ointments, which are used in the treatment of both external and internal thrombosed hemorrhoids, prevent blood clotting.
Heparin ointment
Heparin ointment. An inexpensive, effective remedy that acts on the blood coagulation system, prevents thrombosis of nodes, has a local anesthetic and anti-inflammatory effect, increases the tone of the veins, and stimulates tissue regeneration.
| Composition, active substance | Heparin, benzocaine, benzyl nicotinate |
| Mechanism of action of the drug | Heparin ointment:
|
| Indications |
|
| Contraindications |
|
| Side effects | Allergy, dyspepsia |
| Mode of application | For external localization of nodes, ointment is applied in a thin layer twice a day, after intimate hygiene. In severe cases, apply a compress. They act rectally using an applicator. Course – about two weeks |
| Compatibility with other drugs | The effect of the drug is enhanced when taken simultaneously with NSAIDs and other anticoagulants |
| Use during pregnancy and lactation | Not recommended |
| special instructions | No |
| Price | From 35 rubles |
Gepatrombin G
Suppositories and ointment Gepatrombin G. The most effective remedy for internal hemorrhoids, resolves already formed blood clots and prevents the formation of new ones.
| Composition, active substance | Heparin, prednisolone, lauromacrogol 600 |
| Mechanism of action of the drug | Heparin G has:
|
| Indications |
|
| Contraindications |
|
| Side effects | Allergy |
| Mode of application | 1 suppository once or twice a day after intimate hygiene of the area, for 15 minutes |
| Compatibility with other drugs | No data |
| Use during pregnancy and lactation | From the second trimester as prescribed by a doctor |
| special instructions | Excess of the drug on the skin causes regeneration to slow down |
| Price | From 170 rubles |
Thrombosis
With hemorrhoids, the walls of blood vessels are damaged. And protective mechanisms include the coagulation system, provoking the formation of blood clots. This phenomenon is called hemorrhoidal thrombosis.
Thrombosis of hemorrhoids can be treated non-surgically.
The conservative method includes the following methods of influence:
- Use of medications
- Strict bed rest
- A diet aimed at relieving constipation and facilitating bowel movements
- Taking laxatives and using enemas
- Cool lotions and compresses, shower of the perineal area, sitz baths with infusions of medicinal herbs
- Wash 3-4 times a day with cool water
- Use of hemorrhoidal suppositories, ointments, creams
Drug treatment of thrombosis is aimed at eliminating symptoms and preventing consequences. To achieve positive results, a specialist can prescribe drugs with analgesic, antiseptic, anti-inflammatory, and astringent effects. Depending on the situation, they can be for topical application, oral administration, subcutaneous, intramuscular or intravenous injection.
To treat phlebothrombosis of the hemorrhoidal plexus, anticoagulants that can dissolve blood clots are used. Also suppositories and ointments based on anti-inflammatory and analgesic ingredients.
If there is a suspicion of thrombosis of the hemorrhoid, treatment should be prescribed by a proctologist.
When hemorrhoids develop, you need to eliminate everything that can cause constipation and diarrhea. During the period of inflammation, you should completely avoid alcohol. Alcohol dilates blood vessels, injuring their walls.
At home, of course, you can slightly reduce the hemorrhoid, but over time it will begin to bother you again. The key to quickly getting rid of the disease is to consult a professional doctor.
THERE ARE CONTRAINDICATIONS CONSULTATION WITH YOUR DOCTOR IS REQUIRED
Author of the article Alexey Alexandrovich Egorov, proctologist
Source: gemorroj03.com
Surgical treatment methods
Radical therapy for hemorrhoidal thrombosis is possible in the third degree of severity of the disease. The operation can be performed for vital reasons, immediately (bleeding, pinched node) or after the severity of the process has been removed. There are two types of surgery: thrombectomy or hemorrhoidectomy according to Milligan-Morgan. Minimally invasive techniques are not used, since thrombosis is a direct contraindication to them.
Thrombectomy
Thrombectomy is used to treat thrombosis of the external hemorrhoid without complications. The essence of the operation is to open a hemorrhoidal cone with a blood clot, remove the blood clot and leave the wound open for independent healing.
Read more: thrombectomy of hemorrhoids, what it is, the likelihood of relapse
An indisputable advantage is the possibility of performing the procedure in pregnant women. In addition, the method is minimally traumatic and wound healing occurs quickly. The downside is the use of thrombectomy only for thrombosis of external hemorrhoids, as well as the risk of relapse due to injury to the walls of the node at the time of surgery.
Hemorrhoidectomy
The operation of hemorrhoidectomy is applicable for acute hemorrhoidal thrombosis, complicated by bleeding, strangulation of the node and in a planned manner. The essence is complete excision of a hemorrhoid of any location. The easiest way is to cut off the affected node from the blood vessels at the base of the leg - this is the Milligan-Morgan method. The operation is performed under general or epidural anesthesia. The completion of the operation can be different:
- without stitching the excised tissue - open hemorrhoidectomy;
- with the wound tightly sutured - a closed version of the Milligan-Morgan operation;
- submucosal removal.
Efficiency reaches 98%, the risk of relapse is reduced to zero. In case of inflammation of the perirectal tissue, additional manipulations may be required, for example, drainage of the anorectal area to reduce the inflammatory infiltrate.
Treatment of thrombosis of hemorrhoids
Conservative treatment is carried out in two directions: etiotropic (eliminating the cause of thrombosis) and symptomatic (relieving the patient’s suffering, improving his general condition). The following groups of drugs are used:
- painkillers - applied topically already at the examination stage, since palpation of hemorrhoids is often difficult due to severe pain. Later they can be prescribed in the form of systemic drugs;
- anti-inflammatory – reduce tissue damage by inflammatory agents, relieve pain and swelling. The bioavailability of drugs at the site of inflammation is ensured by topical medications - rectal suppositories (suppositories), ointments, microenemas;
- fibrinolytics (drugs that reduce blood viscosity) - necessary to thin a dense clot and normalize blood circulation;
- phlebotonics – improve the tone of the veins, helps reduce venous stagnation;
- angioprotectors – protect the inner lining of blood vessels from damage, preventing the formation of new blood clots;
- antispasmodics – relax the muscular lining of blood vessels and sphincters, prevent pinching of the node and eliminate discomfort;
- drugs that improve the functions of the gastrointestinal tract (motility stimulants, laxatives) are prescribed as maintenance therapy, facilitate bowel movements, and prevent tissue injury from dense feces.
Depending on which hemorrhoids are damaged, thrombosis of internal and external hemorrhoids is distinguished. They differ in diagnostic methods and approach to treatment, but both forms are equally dangerous to the patient’s health.
With proper treatment, the blood clot dissolves, blood circulation is normalized - perianal thrombosis quickly passes as soon as its immediate cause is eliminated. Conservative treatment does not require hospitalization and can be carried out at home.
In cases where conservative therapy is ineffective, surgical intervention is resorted to. It consists of removing the hemorrhoidal node along with the surrounding tissues and feeding vessels. The volume depends on the scale of the lesion - it can be a small operation performed under local anesthesia on an outpatient basis, or a large-scale intervention with excision of a large volume of tissue.
Thrombosis of the node at a late stage requires surgical treatment, the purpose of which is to prevent the development of necrosis
During the Milligan-Morgan operation for excision of hemorrhoids, a long recovery period follows. The operation using the Longo method is less traumatic, but requires special equipment, materials and highly qualified surgeons. It has high efficiency, a shorter rehabilitation period and excellent reviews from both doctors and patients.
After recovery, the patient must adhere to the basic rules of prevention: follow a diet, avoid excessive physical activity, heavy lifting, and a sedentary lifestyle. Otherwise, a relapse of the disease cannot be ruled out.
Folk remedies
How quickly hemorrhoidal thrombosis goes away depends on how well the treatment package is selected. One of the components of combination therapy for thrombosed hemorrhoids is folk recipes. But it is important to understand that it is impossible to cure thrombophlebitis of the rectal veins only with folk remedies. Moreover, failure to consult a doctor can have unpredictable consequences.
Baths
For thrombosis, the most popular methods of alternative medicine are sitz baths with medicinal herbs:
- baths with a decoction of water pepper, which contains tannins, rutin, quercetin, and organic acids. A handful of herbs is poured into 2 liters of hot water, boiled for a quarter of an hour, left for 20 minutes, filtered, poured into a basin, 0.5 liters of boiling milk is added, sat down so that the hemorrhoids are covered with the solution, the procedure is done at night for a month;
- cold sitz baths from horse chestnut decoction - crush 50 g of branches, pour in a liter of water, simmer for 5 minutes, cool, pour into a basin that already contains 2 liters of cool water, sit for 15 minutes so that the water covers the nodes or irritated anorectum region;
- warm baths from birch leaves - pour a handful of leaves with a liter of boiling water, leave for half an hour, filter, pour into a basin with 2 liters of clean warm water, sit for half an hour so that the anorectal area is covered with the solution;
- sow thistle - the plant is used for thrombosis of the node: a handful of sow thistle is poured into a liter of water and boiled for a minute, then the decoction cools, wrapped in a warm blanket, it is filtered, used for cool baths for 20 minutes, three times a week, for a month;
- sitz bath with aloe juice - juice from several leaves of the plant is dissolved in cool water (2 liters), sit in a basin for 15 minutes so that the thrombosed nodes are covered with the solution (this procedure is effective in the early stages of thrombosis).
Lotions, compresses
Procedures are used to relieve inflammation, painful nodes, and resolve blood clots:
- the easiest way is lotions with strong black tea, which have an astringent effect and contain tannin and tannins;
- disinfect the anorectal area in case of thrombosis using a lotion with a solution of potassium permanganate;
- aloe leaves should be put in the refrigerator for a day (ideally, they should be stored for a week in a dark, cool place), the plant leaf is washed, dried, cut and applied with the sticky side to the node, left until all the juice is absorbed, change the leaf three times/ day during the week;
- horse chestnut flowers are crushed, wrapped in gauze and applied to the site of thrombosis, this relieves pain and inflammation;
- if the thrombosed nodes are injured and begin to heal, then take horse chestnut and rowan flowers in equal parts, add one part of arnica, mix everything, then pour 5 g of the collection with a glass of boiling water, leave for an hour, filter, apply a napkin soaked in this solution to the nodes, for a few minutes. Repeat the action until the pain subsides and bleeding disappears;
- prepare a decoction of quince flowers, pomegranate, blackberry leaves, strawberries - they all have an astringent effect in the form of lotions;
- Compresses made from raw potatoes are effective: the tuber is grated, wrapped in gauze, and applied to the site with the blood clot for half an hour;
- mint, oak and alder bark, chamomile, cucumber lashes, grape leaves are mixed in equal proportions, a concentrated decoction is prepared, sterile gauze is soaked in the medicine, and applied to thrombosed hemorrhoids.
If we are talking about rectal thrombosis, instead of napkins or gauze, use cotton swabs, which are soaked in decoctions and administered rectally.
Decoctions can be drunk internally, herbs are brewed like tea and have a good effect on the gastrointestinal tract.
Homemade candles
The most effective are suppositories made from raw potatoes, which are cut from the middle of the tuber, lubricated with olive oil, and administered rectally for pain in the first stages of hemorrhoidal thrombosis. According to patient reviews, suppositories have a mild, quick pain-relieving effect.
Doctors prefer suppositories made from natural propolis. You can add pine resin to it, heat the mixture in a water bath, then add a few drops of natural oil. Cool. Suppositories are made in small sizes and carefully inserted into the rectum, which helps dissolve blood clots, normalizes blood circulation, relieves inflammation, pain, swelling, and heals damaged tissue. Propolis suppositories are antioxidants and antiseptics.
In addition, you can use:
- ice suppositories with a decoction of medicinal herbs are an effective pain reliever and stops the worm (minus – temporary effect);
- a candle made of beets or garlic, inserted into the rectum at night, relieves inflammation during thrombosis, disinfects the anorectal area;
- candles made from honey in vegetable oil, frozen in the refrigerator, have analgesic, anti-inflammatory, and disinfectant properties.
Ointments
Therapy for hemorrhoidal thrombosis is carried out using homemade ointments that relieve pain, inflammation, stimulate blood flow in the anorectal area, and wound healing:
- ointment with propolis - most loved by patients and doctors; to prepare it, animal fat is heated to room temperature and propolis is added in equal parts, then the mixture is applied to the thrombosed node overnight, and washed off in running water in the morning;
- soft butter is mixed with honey, the mixture is applied in a similar way;
- fresh cabbage is boiled in milk, cooled, crushed together with bran to a homogeneous mass, which is applied to the nodes;
- birch tar is mixed with animal fat in equal proportions and applied to the thrombosed node (tar is a strong allergen, so an allergy test is needed before application);
- tar can be mixed with Vaseline (1:10), infuse the mixture, apply to the nodes after intimate hygiene.
Hirudotherapy is effective for hemorrhoidal thrombus. A leech is planted on each affected node, which sucks out the blood; the node decreases in size, dries out and falls off.
Features of treatment
Thrombosis therapy is prescribed taking into account the severity of the disease.
At stages 1 and 2, drug treatment is indicated, aimed at reducing inflammation, dissolving a blood clot, relieving acute pain and preventing the development of complications. If conservative methods do not give the desired result, stage 3 of the disease is recorded: urgent surgical intervention is required. The doctor removes the blood clot or completely excises the thrombosed node.
Drug treatment
In the conservative treatment of thrombophlebitis, restriction of physical activity is prescribed: you cannot lift weights, engage in strength sports, or spend a lot of time in a sitting position. You should also follow a gentle diet: exclude fatty, fried foods, hot spices, alcoholic drinks from the diet, and add more foods rich in plant fiber. A proper diet normalizes bowel movements and helps get rid of constipation.
To restore blood circulation, patients are prescribed anticoagulants in the form of ointments for external use or rectal suppositories.
Usually the doctor recommends dressings with Heparin ointment, Troxevasin, Hepatothrombin. For internal thrombosis, suppositories are used: Anestezol, Ultraproct, Papaverine, Nigepan.
To relieve pain, reduce inflammation, and swelling, non-steroidal anti-inflammatory drugs are prescribed: Diclofenac, Ibuprofen, Nurofen. Venotonics strengthen the walls of blood vessels, reduce the risk of bleeding, and improve the trophism of ulcerated areas with node necrosis. For the treatment of thrombosis, Ginkor gel, Lyoton, Detralex capsules, Phlebodia are used.
If inflammation of the subcutaneous tissue is present, Heparin is combined with the use of anti-inflammatory ointments: Levosin, Levomekol, Manifed.
Novocaine blockades, cryotherapy, and lotions with Dimexide help to get rid of intense pain due to thrombosis. If tissue infection occurs, a course of antibacterial therapy is carried out, and the cones are treated locally with ointments with corticosteroids. Antispasmodics (No-shpa, Papaverine) are necessary to relax the anal sphincter and reduce pain.
Due to the increase in hemorrhoidal, swollen nodes during thrombosis, feces may be retained in the intestinal cavity, which aggravates the course of the disease and intensifies the inflammatory process. The patient undergoes sanitation of the perineum, and is given cleansing and laxative enemas with vaseline oil.
Physiotherapeutic procedures provide a good therapeutic effect. For thrombosis of the venous nodes of the anus, UHF, darsonvalization, electromagnetic therapy, and laser treatment are performed.
Surgery
The indication for surgical intervention is the chronic course of thrombosis, stage 3 of the disease and the ineffectiveness of drug therapy. Urgent surgery is performed in case of intense bleeding or necrosis of hemorrhoids.
Treatment is performed in several ways:
- Thrombectomy is the removal of a blood clot that has caused a blockage in a vessel. The procedure is performed under local anesthesia, the doctor dissects the lump and removes the clot.
- Complete resection of the venous compaction eliminates the cause of thrombosis and avoids repeated relapses. Hemorrhoidectomy is performed by ligating or excision of nodes: the doctor uses a regular scalpel, laser or electrocoagulation to ligate pathological tissues.
The operation is performed on an outpatient basis and does not require hospitalization of the patient. Sometimes after surgical treatment bleeding occurs and a narrowing (stricture) of the anus develops. After thrombectomy, re-exacerbation of thrombosis is possible.
During the recovery period, nitroglycerin cream 0.2% is used to relieve pain: the drug relieves sphincter spasms.
Analgesics, NSAIDs and sitz baths are also prescribed.
First aid at home
In case of inflammation of hemorrhoids and subacute thrombosis, a person must observe bed rest, a milk-vegetable diet, and take laxatives for painless bowel movements.
You should not try to set prolapsed hemorrhoids on your own! Such manipulations can provoke the development of bleeding, damage to the rectal mucosa and necrosis of a large area.
To relieve pain from thrombosis, reduce redness and swelling, compresses with lead water, 2% sodium bicarbonate solution or witch hazel are applied to the perianal area. The lotions are changed every 30 minutes.
After 1–2 days, when the inflammation subsides, you can take warm baths with soda and potassium permanganate at home. The water should not be hot, otherwise the pathological process may resume.
Can it be cured with folk remedies?
Alternative medicine recipes can be used to treat thrombosis only at an early stage of the disease as an addition to medications. You should first consult your doctor.
- Warm sitz baths with the addition of a decoction of chamomile, sage, St. John's wort, peppermint, and eucalyptus help relieve pain, reduce inflammation and burning in the anus. Herbs normalize blood circulation, accelerate tissue regeneration, and have an antiseptic effect. The healing solution can also be used for external compresses.
- For internal thrombosis and bleeding, it is useful to use raw potato suppositories. Before insertion into the anus, the suppository must be lubricated with sunflower or sea buckthorn oil.
- One of the effective folk remedies that can treat thrombosis is natural propolis. Small suppositories are made from it and carefully inserted into the anus. The bee product helps dissolve blood clots, normalizes blood circulation, relieves inflammation, pain, swelling, heals damaged tissue, and acts as an antiseptic and antioxidant.
Home recipes should not be used at an advanced stage of thrombosis.
In such cases, it is necessary to urgently start using medications or perform surgical removal of the nodes.
Diet
Nutrition for hemorrhoidal thrombosis is an integral part of the overall complex treatment. The antithrombotic diet has several features:
- at the time of exacerbation of hemorrhoids, patients are limited in the amount of liquid they drink per day: the usual drinking ration is halved;
- Products containing vitamin K and C are prohibited for consumption: tomatoes, currants, all citrus fruits, liver, cabbage increase blood clotting, provoking the formation of more and more blood clots;
- during the period of remission - regular meals, fractional meals, in small portions (palm size), dishes are steamed;
- Smoking and alcohol are strictly prohibited during any period of illness.
Nutrition directly affects the patient’s recovery rate after surgery.
The table shows permitted and prohibited products for everyone who suffers from hemorrhoids of any location with a history of node thrombosis.
| Recommended | Prohibited |
| Porridge | Fried, spicy, fatty foods, smoked foods, canned food, marinades |
| Fiber from vegetables and fruits | Rich broths |
| Dairy products | Salt (no more than 20 g/day) |
| Vegetable soups | Strong coffee, tea |
| Omelette | Legumes |
| Grape | |
| Soda | |
| Sweets |
Choice of treatment tactics
There are 2 methods of treatment - conservative and surgical. Conservative treatment is used for grades 1 and 2 . It consists of following a diet, taking medications orally and local treatment.
The diet consists of normalizing the activity of the digestive tract by consuming enough dietary fiber per day. These include: bran from wheat, oats, seaweed, flax seeds, vegetables and fruits.
Meals should be at least 4-5 times a day in small portions. It is necessary to exclude the intake of fatty, fried, spicy foods, and alcohol.
Local treatment - lotions moistened with antiseptic solutions (furacillin, potassium permanganate).
Drug treatment:
- Elimination of pain syndrome - Proctosan, Aurobin, Ultraproct, Relief and other drugs.
- Anticoagulants – Heparin ointment, Troxerutin.
- Phlebotonics – Detralex.
- Anti-inflammatory therapy - Diclofenac, Indomethacin.
- For bleeding, local hemostatic drugs are indicated - Phenylephrine, sodium alginate.
Surgical treatment is prescribed for stage 3 thrombosis . An operation is performed to excise the hemorrhoid and remove the blood clot - thrombectomy. In severe cases, the node itself is removed - hemorrhoidectomy.
Prevention measures
Prevention of thrombosis in hemorrhoids consists, first of all, in excluding from the diet foods that cause constipation (smoked meats, spicy foods, alcohol, etc.). If you limit the pressure of feces on the nodes, you can avoid the formation of unwanted blood clots. But, without treating the hemorrhoids themselves, the risk of blood clots still remains - it is recommended to make every effort to get rid of the primary disease.
In addition, as a preventative measure, doctors advise moderating physical activity and not pushing too hard during bowel movements. If you really can’t go to the toilet, it’s better to take a mild laxative. Among folk recipes, a glass of boiled milk with 1 tablespoon of honey will cope with this task.
Conclusion
Thrombosis of the hemorrhoidal node is expressed in severe pain and swelling in the rectal area. Often the patient experiences a spasm of the anal sphincter, which creates additional difficulties with bowel movements. Treatment with herbs, tablets and ointments will help cope with the disease. But if bleeding and periodic exacerbation of the disease are observed, surgery cannot be avoided. Still, the best treatment option is to eliminate the root cause. It is hemorrhoids that need to be fought in order to stop the occurrence of complications.
Degrees of hemorrhoids, symptoms
Degrees of hemorrhoids photos in women
Hemorrhoids have an acute and chronic course. As mentioned above, hemorrhoids are classified by location. There is a clinical classification according to severity.
Mild degree
It manifests itself as moderate inflammation; thrombosis and other complications usually do not occur. Moderate arterial bleeding occurs and pain appears. The stool is usually preserved, and the process does not affect the regularity of bowel movements.
In the event that hemorrhoids fall out, they can easily reset themselves. Apart from local manifestations, there are no other complaints and general health does not suffer.
Average degree
The symptoms described above are accompanied by swelling of the formed nodes. They become inflamed. If the knot falls out, it cannot be set on its own - this must be done, literally, “with your own hands.”
There are frequent and severe thromboses and bleeding. Defecation becomes very painful, and there is a tendency to constipation, often of a psychological nature.
General symptoms appear that indicate the severity of the condition: low fever, the appearance of lethargy and weakness, decreased appetite, increased nervousness, poor sleep, fear of defecation, and even a conscious refusal to eat so as not to go to the toilet.
- At this stage, the patient’s whole life comes down to a painful wait for the next bowel movement, which is perceived as torture.
Severe degree
At this stage of the disease, the picture of progressive complications comes to the fore. The dropped nodes cannot be set back in any way. They become necrotic and suppurate. The skin of the anal area is sharply swollen.
The temperature is high, pain occurs in the perineum and even in the abdomen. There is no way to empty your bowels on your own. An increase in intra-abdominal pressure can lead to intestinal rupture, peritonitis, and intestinal obstruction.
In addition to this classification, not only the severity, but also the stages of the disease are important for the diagnosis and choice of treatment tactics for hemorrhoids:
- The first degree is characterized by the presence of collapsed nodes.
When you strain, they increase sharply, like berries, and bleeding appears, often in the form of scarlet streaks in the feces. The rectal sphincter retains its function. Exacerbation occurs 2-3 times in a whole year, when anal itching and episodes of inflammation occur.
- The second stage is characterized by the appearance of node thrombosis, which will be discussed below.
The nodes are adjusted only by hand, which differentiates the stages. Bleeding and pain are intense and regular, but there is no general anemia in the patient. Often before bleeding there is an attack of anal itching. Exacerbations occur every month. The rectal sphincter is weakened, but it still holds the intestinal contents well.
- The third stage is characterized by unpleasant “surprises”.
As soon as you stand up, strain, lift a small weight or engage in physical labor, the nodes begin to fall out. They have to be manually adjusted, but they bleed almost constantly and the patient may develop severe anemia, with pallor and shortness of breath.
In this case, a gaping of the anal sphincter occurs; it is no longer able to hold feces. The inability to retain feces and gases completely depresses the patient and leads him to isolation from others and severe depression.
General signs
There is also a staged pattern in the appearance of signs of formation and prolapse of hemorrhoids.
At the beginning, patients have a feeling of itching and a foreign object in the anus, after eating spicy foods, alcohol, or physical labor. Then, after several months or even years, scarlet bleeding appears, from droplets to copious amounts, in a trickle, covering the feces from the outside and not mixing with feces.
Before bleeding, itching appears in the anal area. In the later stages of the disease, the main complaints are prolapse of hemorrhoids, thrombosis and other inflammatory processes.
It must be said that outside the period of defecation, pain practically does not bother patients. Pain in hemorrhoids, one way or another, is always associated with the act of defecation.
Symptoms and signs of pathology
Hemorrhoids can be easily treated in the initial stages. But, unfortunately, many people neglect the help of doctors, as a result of which complications typical for the disease develop. One such complication is hemorrhoidal thrombosis.
Thrombosis of hemorrhoids is always accompanied by severe symptoms. Clinical manifestations of the disease are visible to the naked eye.
The main symptoms of thrombosis of hemorrhoids are:
- Pain in the anus, which becomes more intense with an upright position of the body, movements, and after going to the toilet. An important diagnostic criterion is the sudden onset of pain, which then does not go away.
- Feeling of a foreign object in the rectum.
- Itching near the anus.
- Inflammation and swelling of the tissues of the perianal area.
- Hemorrhoidal bumps are firm to the touch and painful.
- Discharge of bloody and mucous masses from the rectum appears when the disease is severe.
Symptoms worsen and increase as the disease progresses.
Diagnosis of thrombosis
Usually the disease has such characteristic symptoms that additional diagnostics are not required
- interview and examination of a specialist - coloproctologist;
- rectal examination;
- anoscopy.
It is usually not possible to palpate (feel) the rectum, since this manipulation will be quite painful for a person.
Due to the acute and pronounced symptoms, thrombosis of the hemorrhoidal node is diagnosed quite easily and quickly. For this purpose, three types of research are used: visual, digital and instrumental.
Upon visual inspection, you can see enlarged external nodes that have a purple or bluish color, often covered with a whitish coating. If the doctor notices black areas, this indicates necrosis of hemorrhoids - tissue death. The area around the thrombosed nodes is swollen and red, and bleeding may be observed.
With a digital examination, the doctor examines the density of the nodes. As a rule, thrombosed nodes are dense to the touch and do not collapse when pressure is applied to them. In case of internal thrombosis, after a digital examination, blood remains on the glove. There is increased sphincter tone.
If thrombosed nodes fall out, a digital examination can only be done with pain relief, since the procedure is painful for the patient, and sphincter spasm does not allow the doctor to fully examine the affected area.
The last stage of diagnosis is instrumental examination (rectoscopy). It is carried out using a rectoscope (rectal mirror). Instrumental diagnostics gives the doctor the opportunity to differentiate pathology.
In cases of severe pain, rectoscopy is also performed under local anesthesia.
It usually takes a doctor a little time to make a diagnosis, since the signs of hemorrhoids are very bright and noticeable during a routine examination of the patient. But the doctor will definitely question the patient in detail about his complaints about his health and clarify the presence of concomitant and chronic pathologies. Next, an external and rectal examination will be required.
IMPORTANT. If the pathology is at the second or third stage, it is almost impossible to examine the patient without causing him pain. Therefore, a specialist may prescribe an examination under local anesthesia in a hospital setting.
If a more detailed examination is necessary, the purpose of which is to clarify the stage and degree of development of the pathology, the doctor prescribes rectoscopy. This is an examination in which the rectum is examined with a special instrument that helps determine the presence of thrombosis even at its early stage.
If a more detailed examination is necessary, the purpose of which is to clarify the stage and degree of development of the pathology, the doctor prescribes rectoscopy
Clinical tests are also important: a urine and blood test will help establish an overall picture of the patient’s well-being and determine the level of platelets responsible for blood clotting.
Diagnosis of the disease is not difficult for a qualified specialist. The following diagnostic procedures may be required:
- Study of anamnesis. The doctor pays attention to the presence of chronic hemorrhoids and factors that contribute to increased intra-abdominal pressure (childbirth, heavy physical labor).
- Visual and digital inspection. The latter may be difficult due to pain and spasm of the anal sphincter. In this case, local anesthesia may be required.
- Instrumental examination using a rectal speculum or rectoscope. This is necessary for the detection of internal thrombosed nodes, differential diagnosis of thrombosis from cancer, anal fissures, rectal polyps and paraproctitis.
- Laboratory blood test to evaluate its coagulation system (hemostasiogram).
To make a diagnosis of external thrombosis of the hemorrhoid, the proctologist must:
- conduct a survey - from it the doctor will find out whether you have previously had attacks of hemorrhoids;
- inspect the affected area;
- if possible, palpate, but often this is not possible due to severe pain;
- - will prescribe a rectoscopy - an instrumental examination of the rectum, which will help to accurately determine the presence of thrombosis. It is carried out using an anesthetic;
- - will write out a referral for a blood test to determine anemia;
- - prescribe a blood clotting test.
Forecasts and preventive measures
The outcome of the disease is favorable if it is not advanced, the necessary therapeutic measures are taken, and treatment is carried out under the supervision of a qualified proctologist.
How quickly does hemorrhoidal thrombosis go away? The disease of the first degree can go away on its own in a few weeks, but you should not rely on this - it is better to see a doctor on time and cure the disease without exposing yourself to the risk of serious complications.
Prevention of thrombosis is the avoidance of risk factors for the disease . In particular, it is necessary to lead a healthy and active lifestyle, avoid hypothermia, eat right, and learn how to properly empty the intestines (without straining or constipation).
Thrombosis of hemorrhoids lies in wait for almost 40% of patients with chronic hemorrhoids, and for some it can occur suddenly - after childbirth or heavy physical labor.
There is nothing shameful in this disease to hide it until it becomes unbearable: the sooner treatment is started, the sooner the disease will be defeated!