Indications for aortofemoral bypass surgery
Aortofemoral bypass surgery is indicated for the following pathological conditions:
- chronic arterial insufficiency caused by occlusion (clogging of the lumen) of the abdominal aorta;
- occlusion of the lumen of the iliac arteries if endovascular intervention is not possible;
- abdominal aortic aneurysm;
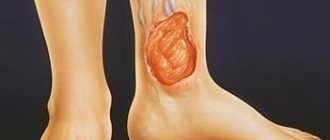
- the presence of non-healing trophic ulcers of the lower extremities;
- impotence of vascular origin.
The operation is aimed at restoring blood flow and eliminating extensive ischemia of the lower extremities, which carries the risk of developing gangrene, amputation and disability of the patient.
Femoral artery replacement can be performed as a treatment method for already developed Leriche syndrome, as well as for prophylactic purposes in the presence of atherosclerosis of the abdominal vessels to prevent complications associated with critical ischemia.
Why is the procedure necessary?
This intervention is prescribed for blockage of both iliac arteries. Allows you to save the lower limbs, improve the quality of life and prevent further complications. Among them, the most common in this situation are impotence, intermittent claudication and absence of pulse in the arteries of the legs. A similar procedure is used when:
- systemic vasculitis;
- obliterating atherosclerosis;
- Takayasu's disease;
- atherosclerosis;
- abdominal aortic aneurysm.
Contraindications and possible complications
Femoral artery bypass surgery is a technically complex and risky surgical procedure that is performed under general anesthesia. For this reason, the procedure has a number of contraindications, the main of which are:
- severe disturbances in cardiac conduction and heart rhythm in the patient;
- suffered a stroke or myocardial infarction in the recent past;
- severe liver and/or kidney dysfunction;
- cardiac ischemia;
- bleeding disorders and other blood diseases;
- the presence of any malignant neoplasms;
- chronic obstructive pulmonary disease in decompensated form;
- anatomically determined inability to access the aorta (for example, in the presence of severe fibrosis of the peritoneal tissue, colostomy, horseshoe kidney).
The operation cannot be performed if the beds of the iliac arteries are severely blocked, and the installation of a shunt will not help normalize blood flow. When, for certain reasons, femoral artery replacement is not possible, endovascular (intravenous) operations are performed, for example, vascular stenting.
Like any other operation of this level of complexity, femoral artery bypass surgery is associated with the risk of complications. One of the most common and completely reversible complications is the accumulation of lymphatic fluid in the area of intervention and severe tissue swelling.
In some cases, fluid removal may be necessary. Typically, swelling goes away within 7-10 days after surgery.
More dangerous complications include:
- development of myocardial infarction or stroke;
- bleeding;
- formation of false aneurysms;
- suppuration of the prosthesis with subsequent development of sepsis;
- occlusion of the vascular prosthesis.
Indications for bypass surgery
There are clear indications for bypass surgery. These include:
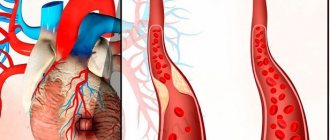
- atherosclerosis (deposition of lipids on the endothelium leads to narrowing of the lumen of the vascular bed);
- coronary heart disease (impaired blood flow in the coronary arteries supplying the heart causes myocardial infarction);
- disturbance of blood flow in the vessels of the brain (changes in the patency of areas of the cerebral vascular network are caused, as a rule, by their obstruction by a blood clot, a detached fatty plaque, or the presence of lipid growths on their walls);
- obesity (people who are overweight tend to have a distended stomach, and stomach bypass surgery helps solve this problem).
The indications for surgery are determined by the surgeon. To do this, he carefully interviews the patient, details all his complaints, and directs him to undergo a full examination. In doubtful cases, the decision is made by a council of surgical specialists.
Preparation for the procedure
To minimize the risks of possible complications, it is necessary to obtain a complete understanding of the patient’s health status, in particular, the state of his cardiovascular system, excretory system, liver and lungs. It is necessary to accurately identify the level of damage to the aorta and iliac arteries, as well as assess the condition of the vessels of the lower extremities. To determine the treatment tactics for pathology, the following diagnostic methods are used:
- physical examination and history taking;
- vascular angiography;
- ultrasound examination of vessels and peritoneal tissues;
- computed tomography using contrast agent;
- MRI of the cardiovascular system.
Based on the data obtained, taking into account the assessment of the patient’s general condition, the tactics of the operation are determined.
The patient should stop taking any antiplatelet drugs (drugs that weaken blood clotting) for 7-10 days to reduce the risk of bleeding during surgery. If the patient has a vital need to take such drugs, he is temporarily prescribed direct anticoagulants.
Patient preparation
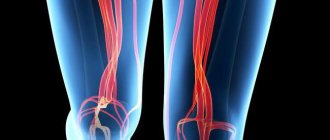
Bypass operations for blood vessels of the lower extremities require preoperative preparation. The doctor prescribes a hardware examination of the state of the circulatory system of the legs. This:
- Duplex scanning to examine the cavities of the veins and arteries, determine the localization of blocked areas of the lower vessels and the speed of blood flow.
- Magnetic resonance angiography for layer-by-layer examination of the lower veins.
- Angiography - the nature of the narrowing of the vein is assessed and a blocked area along the vessel is detected.
Bypass surgery of the heart vessels is preceded by ultrasound of the organ and coronography. An increased risk of postoperative treatment complications is observed in patients with:
- High blood pressure.
- High cholesterol levels.
- Pathology of the heart, lungs, kidneys.
- Diabetes mellitus, etc.
In this case, vein bypass is justified only if there is a threat to the patient’s life. Carrying out a thorough assessment of the condition of the saphenous veins is due to the fact that the period of operation of the shunt and the effectiveness of treatment depend on it. Bypass surgery with an artificial prosthesis is done as a last resort, since reviews from surgeons indicate that half of the veins are clogged after 3 years.
An increased risk of postoperative treatment complications is observed in obese patients.
Progress of aortofemoral bypass surgery
At the preparation stage, premedication is performed, as well as prophylactic administration of antibiotics that suppress the natural saprophytic flora.
To access the aorta, two methods are traditionally used: laparatomy or a retroperitoneal incision according to Rob. The latter method is used most often, as it avoids intestinal injury and reduces the risk of damage to the femoral nerves.
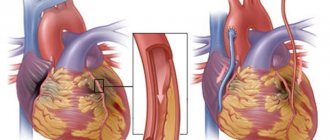
After access to the artery is secured, a shunt made of inert materials is sewn into an area free of atherosclerotic deposits. The diameter of the shunt is selected according to the lumen of the artery. The other end of the shunt is sutured into longitudinal incisions in the femoral artery. If the shunt connects the aorta and one of the femoral arteries, we are talking about aorto-femoral bypass; in the event that the shunt connects the aorta with two femoral arteries at once, the operation is classified as aorto-femoral bifurcation bypass.
What type of surgery can be performed on the femoral artery?
For atherosclerotic lesions of the femoral artery, surgery is recommended in the second and third stages. In such patients:
- the walking distance without pain is less than 250 meters, and with critical blockage it drops to 50 m;
- pain also bothers you at rest, during sleep;
- taking painkillers continues for more than 2 weeks with little effect;
- there are changes on the skin in the form of trophic ulcerative defects.
If you miss the time favorable for surgical treatment, tissue necrosis develops - gangrene with the need for emergency amputation of the limb.
Revascularization (restoration of artery patency) is carried out by performing the following surgical interventions:
- endarterectomy (removal of plaque and inner layer of the wall);
- balloon expansion (dilatation) with stent installation (stenting);
- prosthetics (replacing the affected area with your own vein or an artificial prosthesis);
- shunting (creating a bypass route for tissue nutrition);
- palliative methods (removal of nodes of the sympathetic nervous system, creation of holes in the bone);
- profundoplasty (applying a patch).
We recommend reading the article about femoral artery occlusion. From it you will learn about the causes of pathology and the process of its occurrence, symptoms, methods of diagnosis and treatment. And here is more information about femoral artery aneurysm.
Postoperative period and recovery
For the first 1-2 days the patient is forced to remain motionless, then, if no complications arise, they are allowed to stand up. As a rule, discharge occurs 7-8 days after surgery, and after 14 days the sutures are removed.
During the recovery phase, it is recommended to take medications that help normalize metabolism and reduce cholesterol levels. It is very important to adhere to the principles of a healthy lifestyle: giving up bad habits, excluding foods containing fats, sugar and salt in high doses from the diet.
Prices for aortofemoral bypass surgery
Femoral artery replacement is included in the list of procedures provided for by compulsory medical insurance and is performed free of charge according to a doctor’s indications. But since bypass surgery is a technically very complex operation, not all medical institutions have specialists with sufficient qualifications to perform it. Bypass operations are also performed by medical centers that provide paid services.
Prices depend on many factors, including the location of the institution, and range from 45 to 200 thousand rubles.
Bifurcation aortofemoral bypass (ABBS)
Department of Vascular and Endocrine Surgery
Bifurcation aortofemoral replacement or bypass surgery is a surgical procedure to restore blood supply to the lower extremities. It consists of installing a prosthesis (shunt) between the femoral arteries and the aorta, bypassing the blocked segment. Bifurcation aortofemoral bypass (ABBS) is performed when there is blockage of the terminal aorta and/or iliac arteries.
The operation is performed under general anesthesia. If it is placed parallel to the affected vessels, then this is a bypass. If it completely replaces clogged arteries, then this is prosthetics.
Indications:
1. Aneurysm of the infrarenal aorta more than 40 mm in diameter.
2. Rupture of an aneurysm of the infrarenal aorta.
3. Occlusive lesions of the infrarenal aorta, main arteries with chronic ischemia of the lower extremities 2B, 3, 4 degrees (according to Fontaine - A.V. Pokrovsky).
Indications for simultaneous interventions on the aortofemoral and femoropopliteal segments:
1. Small diameter of the deep femoral artery (less than 3 mm).
Complications after aortofemoral reconstructive surgery
Long-term results of patency of aortofemoral transplants vary over a very wide range. Primary 5-year patency ranges from 70% to 90%. According to Nevelsteen et. al., after 10 years, a good result was observed in 58% of patients with II degree of ischemia and in 46% with III and IV degrees of ischemia, and the cumulative patency of the grafts was 74%. Down et al. summarizing the experience of 1748 operations in the aortofemoral zone, revealed that after 5 years the cumulative patency of the grafts was 80%, and after 10 years more than 70%. Obviously, the difference in the results cited by the authors is due to both the frequency of involvement of the femoral-popliteal segment in the process, the initial degree of ischemia, and the duration of observation of the operated patients. At the same time, the use of various synthetic prostheses does not have a statistically significant difference in the long-term results of aortofemoral reconstructions.
The choice of type of surgical intervention, according to some authors, affects long-term results. Thus, a number of researchers believe that aortofemoral bypass surgery is accompanied by fewer late complications. Other researchers, on the contrary, have noted that the incidence of late reocclusion is lower after aortic resection with replacement. However, most surgeons did not note statistically significant differences in the frequency of “late” reocclusions after aortofemoral bypass surgery and aortic replacement. Most authors believe that even with unilateral occlusions of the aortoiliac segment, it is advisable to perform aortobifemoral bypass surgery. At the same time, Van der Akker et al. estimates that 34% of all patients with aortofemoral lesions require unilateral reconstructions. However, long-term results do not differ from aortofemoral bypass surgery and only 6% of patients require surgery on the contralateral side. Long-term results were better in patients operated on in stage II B degree of ischemia. Almost unanimous opinion is expressed by the majority of researchers regarding the influence of patency of the distal arterial bed on long-term results. According to some researchers, with a patent femoral-popliteal segment, primary and secondary patency was 10-15% higher than in patients with combined lesions of the aorto-femoral and femoral-popliteal segment, starting from 4-5 years. According to I.I. Zatevakhina et al. in cases of outflow only through the deep femoral artery, the latter is occluded more often than when blood flow is maintained through both femoral arteries.
The anatomical and functional state of the deep femoral artery and the degree of development of collaterals in the popliteal artery play a great role in the occurrence of thrombotic complications. With developed collaterals, up to 87% of patients in the long term after aorto-deep-femoral bypass surgery report good results, which may not differ statistically significantly from the results obtained in patients with patent femoral-popliteal segments.
According to various researchers, from 5 to 20% of patients who have undergone aortofemoral reconstructions require a second stage of femoropopliteal or femoro-tibial bypass surgery. According to the observations of Harris et al. of 106 patients with combined lesions of the aortofemoral and femoropopliteal segment, 20% of patients required a second stage of surgery. The author notes the best results when performing direct revascularization of the popliteal artery. Cumulative patency in the first group of patients reached 98%, and in the second group only 69%. At the same time, in patients who underwent simultaneous reconstruction of the femoral-popliteal segment, mortality was almost 2 times higher than in patients with isolated aorto-femoral bypass surgery.
The second important prognostic indicator of long-term patency of aortofemoral grafts is the age of the operated patients. Most authors note a higher incidence of thrombotic complications in patients operated on before the age of 45 years. According to Munro et al. The 3-year cumulative patency rate is as high as 65%, 23% of patients experience limb loss, and thrombotic complications occur in 51% of patients. Particularly attractive are the data that did not reveal statistically significant differences in cumulative patency in patients with atherosclerotic occlusions under the age of 50 and after 50 years. According to a number of authors, 4-year patency in patients under 40 years of age was 89%; however, the authors included in the sample only 56 patients with localized lesions of the aortofemoral segment, while 39 patients with widespread atherosclerosis were not included in the analysis.
Long-term results of reconstructions in men and women, according to most researchers, are not statistically significantly different.
Over the past 30 years, the causes of late thrombotic complications have been analyzed in the literature. Most researchers identify three main reasons for the development of thrombosis: progression of the underlying disease, changes in the prosthesis itself, and errors in both technical and tactical plans.
The most common cause of thrombotic complications is the progression of atherosclerosis, more often in the distal part, preventing the outflow of blood, and less often in the proximal direction, which leads to a decrease in volumetric blood flow through the aorta and branches of the prosthesis.
The second most common factor causing thrombosis is anastomotic stenosis, which is called “anastomotic restenosis” in the literature. Some authors attribute the development of restenosis to complications associated with the use of synthetic prostheses. Indeed, when using synthetic materials, the incidence of restenosis is higher than when using an autovein; however, it is known that the development of restenosis also occurs when using an autovein.
The third factor includes tactical and technical errors leading to the occurrence of thrombotic complications: uncorrected stenosis of the proximal or distal segment, the imposition of a low proximal anastomosis in the area most susceptible to atherosclerosis, leaving kinks and excess vascular prostheses, performing operations in the inadequate condition of the distal arterial bed ). According to I.I. Zatevakhina et al., about one third of long-term complications are caused by errors in both technical and tactical plans.
Another frequent complication after reconstructive operations is the development of false aneurysms of distal anastomoses, according to the literature, the frequency of which ranges from 3.2% to 13.3%. False aneurysms of the proximal anastomosis are less common, the incidence of their development ranges from 0.6% to 4.8%. The timing of the occurrence of false aneurysms is different and ranges from 6 months to 20 years after surgery. Most often, false aneurysms appear within 4 to 6 years after surgery. The difference in the frequency of detection of false aneurysms is largely due to the methods of their diagnosis. Thus, with targeted ultrasound examination of distal anastomotic zones, the incidence of false aneurysms was 13.3%, and in almost 50% of patients they were asymptomatic and were detected during control ultrasound scanning.
False aneurysms of distal anastomoses account for about 6% of all late thrombotic complications.
Other causes involved in the development of thrombotic complications, such as extravasal compression, compression of the branch of the prosthesis by the sigmoid colon or inguinal ligament, fibrous periprosthetic ring, certainly occur, but in a very limited proportion of patients and in clinical practice they are of rather theoretical interest.
At the same time, dehydration of the body, which occurs with the development of dehydration due to the consumption of large amounts of alcohol, can cause the development of thrombosis even in the absence of the three main reasons mentioned.
Vascular thrombosis can also occur against the background of increased blood clotting or antithrombin deficiency. These disorders can be observed in hematological or oncological diseases, as well as as a manifestation of an infectious process. They account for about 4% in the structure of thrombosis.
The causes of late reocclusions cannot always be identified. According to available observations, the timing of their development is of some importance. According to some authors, atherosclerotic restenosis and reocclusion occur no less than 3-5 years after primary surgical interventions. Meanwhile, tactical and technical errors appear much earlier and are accompanied by the occurrence of reocclusions in the next 1-2 years. However, it is not always possible to establish a clear relationship between the timing and cause of reocclusions.
According to most authors, reocclusions in 50-80% of cases occur in the next two years after surgical interventions. So, I.I. Zatevakhin et al. note that in 54.8% of patients, reocclusions occurred in the first two years after primary operations, while in the next three years their frequency decreased, increasing again after a 5-year period. According to Wilson et al., 79% of thromboses occur in the first 5 years. In 50% of cases, the cause of thrombotic complications is the progression of atherosclerosis in the distal direction. According to I.I. Zatevakhin et al., in patients after aortofemoral bypass surgery, obstruction in the femoropopliteal segment occurs almost 4 times more often than in the aortic segment.
In recent years, ultrasound methods have become widely used in the diagnosis of late thrombosis and anastomotic stenosis.
When using Doppler ultrasound, it is possible to diagnose relapse of limb ischemia even before the development of thrombosis of vascular prostheses and to suspect the presence of stenosis. The disadvantages of Doppler ultrasound include the inability to accurately localize and assess the degree of the stenotic process. According to I.I. Zatevakhina, the insufficient information content of the method was also noted in the acute course of recurrent ischemia. Thus, in 75% of patients with thrombosis of vascular grafts and clinical symptoms of acute limb ischemia, the arteries of the leg were not located. While in more than half of the patients the tibial arteries were patent during the operation.
More accurate information is provided by duplex scanning, which makes it possible to determine the percentage of stenosis, as well as to carry out long-term dynamic monitoring of patients with functioning transplants and assess the degree of progression of the atherosclerotic process. It has been established that with stenoses of the distal anastomoses of more than 60%, the peak frequency increases and the frequency spectrum expands.
According to some researchers, during X-ray contrast studies in patients with thrombotic complications, it is not always possible to obtain the distal arterial bed when it is patent.
Despite this, angiographic examination remains an important method in the diagnosis of thrombotic complications, since the information obtained allows us to judge the causes of reocclusion.
| < Previous | Next > |
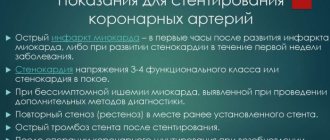
Cardiac ischemia
It is caused by a narrowing of the lumen of the coronary vessels, which leads to insufficient oxygen supply to the heart muscle. In such a situation, complaints often arise of pain behind the sternum or in the left half of the chest, the so-called. angina pectoris, or angina pectoris. In such cases, diagnostic procedures are indicated, the main one of which is coronary angiography (CAG). Based on the results of this study, a decision is made on further treatment directly during coronary angiography. In some cases, it is possible to widen the narrowed area using balloon angioplasty and insertion of a stent, however, in most cases, coronary artery bypass grafting (CABG) surgery is necessary. Timely coronary bypass surgery prevents irreversible changes in the heart muscle, in many cases improves myocardial contractility and increases the quality and length of life.
This operation lasts on average 3-4 hours. It is carried out mainly using a heart-lung machine (CPB). In some cases, this operation is possible on a beating heart. The decision on how to perform coronary artery bypass grafting is made individually, depending on the type and severity of damage to the coronary vessels and the need for simultaneous additional surgery (replacement or reconstruction of one of the valves, removal of an aneurysm, etc.).
The advantages of coronary bypass surgery without an infrared apparatus are:
- absence of traumatic damage to blood cells;
- shorter duration of the operation;
- rapid postoperative rehabilitation;
- no complications associated with cardiopulmonary bypass.
How to prepare
Before the procedure, you must undergo an examination. This will allow you to determine the exact degree of stenosis. In this case, both standard and specific studies are prescribed. Their list includes:
- blood test (for general indicators, for HIV, for markers of hepatitis C and B, for coagulation, for syphilis);
- urine analysis for general indicators; duplex color scanning;
- X-ray contrast angiography;
- Magnetic resonance imaging;
- plethysmography (assessment of arterial blood flow);
- ankle-brachial index (an indicator of damage to the arteries of the legs);
- coronary angiography;
- Cardiography (ECG).
In addition, other types of examinations may be needed, depending on the presence of certain diseases. This approach gives a detailed picture of the preoperative state of the body and allows you to correct some aspects in advance. 7 days before the intervention, stop taking certain medications, 2-3 days before - alcohol and tobacco, 1 - food. Before the operation, an enema cleansing of the intestines is performed.
Main stages of bypass surgery
A small incision is made in the coronary artery below the site of stenosis.
If the radial artery or vein was used, then one end is sutured into the incision, and the other into the aorta.
If the intrathoracic artery was used, then its end is sutured into the incision of the coronary artery, and the second end already extends from one of the branches of the aorta.
General provisions
It is possible to use various conduits. Complete autoarterial revascularization has advantages in long-term follow-up.
The operation is performed under artificial circulation or on a beating heart.
Access to the heart through median sternotomy or minimally invasive techniques.
Your attending surgeon will tell you more about all this.
End of operation
Once the anastomoses are formed, blood begins to flow into areas of the myocardium that have suffered from a lack of oxygen and nutrients. In case of multi-vessel disease, bypass surgery of several arteries of the heart is performed. At the end of the operation, the sternum is closed with wire sutures that remain permanently. The soft tissue is sutured and the patient is transported to the intensive care unit for further observation and awakening.
Performing an operation
Depending on the examination data obtained, the doctor chooses the method of performing the operation. To do this, he assesses the general condition of the patient and the degree of atherosclerotic lesions of the lower limb, the threat of gangrene, the possibility of using general anesthesia, a contrast agent, and subsequent long-term therapy with anticoagulants.
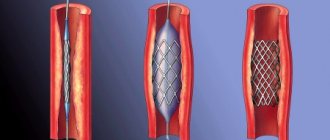
Dilatation with stenting
Indicated for local narrowing of the femoral artery or for its blockage. It is performed intravascularly under radiographic control. A balloon is inserted through a puncture of the vessel, which expands at the site of stenosis and crushes the cholesterol plaque. A mesh tube made of metal wire (stent) is installed in the problem segment to prevent the vessel from blocking.
Prosthetics
It is performed under general anesthesia with open access. Part of the femoral artery is removed, and a section of the great saphenous vein is sutured into the site of the defect. In this case, it is necessary to take into account the direction of its valves; they should not interfere with the movement of blood. In some cases, an artificial vascular graft may be necessary.
Thrombembolectomy
Indicated when a blood clot or part of a cholesterol plaque is detected that has blocked the femoral artery. The operation can be performed using an indirect method - the blood clot is removed from the vessel using a special grip.
With direct arteriotomy, the vessel is cut, and a probe with a balloon at the end (Fogarty type) is inserted into it. It moves beyond the blockage, and then the balloon is inflated, and the catheter, along with the thrombotic masses or embolus, is removed. After complete cleansing, a vascular suture is placed on the artery.
Endarterectomy
Used for atherosclerotic lesions of the femoral artery. The obstructing (clogging) plaque is excised along with part of the inner lining of the vessel. With open access, the operation is performed under visual control. With the semi-closed method, a small incision is made on the affected segment of the artery, surgical instruments are inserted into it, and atheromatous masses are removed.
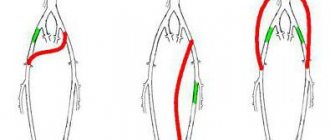
Bypass operations
They involve creating a bypass route for the blood supply to the lower limb. During the operation, the patent sections of the femoral and popliteal arteries are connected using the patient's own vein or a vascular prosthesis. The operation is performed under general anesthesia or spinal anesthesia.
If the surgical risk of traditional operations is high, the surgeon can build a long tunnel under the patient’s skin from the subclavian artery to the femoral artery (in the upper third of the thigh). In these places, the vascular prosthesis is connected to the isolated vessels, and it is sutured on the skin of the chest, abdominal wall and in the groin area to prevent displacement and twisting.
Rehabilitation period
Typically, patients remain on a ventilator for some time after CABG. After restoration of independent breathing, it is necessary to combat congestion in the lungs: rubber balls (or special devices) are well suited for this, which the patient inflates 10-20 times a day, thereby ventilating and straightening the lungs.
The next task is the treatment and dressing of wounds of the sternum and legs. After 7-14 days, the skin wounds heal and the patient is allowed to shower.
During CABG surgery, the sternum is dissected, which is then secured with metal sutures, since it is a very massive bone and bears a large load. For faster healing, it is necessary to provide her with rest; for this purpose, special medical bandages are used. You can do without a corset, however, there are cases when the sutures cut through in operated patients and the sternum diverged, as a result of which repeated operations were performed, although not such large ones. Therefore, patients are recommended to purchase and use a chest bandage.
The next stage of rehabilitation is an increase in motor activity. After the operation, when angina is no longer a concern, the doctor prescribes how to increase the pace. Usually they start by walking along the corridor up to 1000 meters per day, and gradually increase the load. Over time, the motor mode is not limited. After discharge from the hospital, it is advisable to go to a sanatorium for final recovery.
2-3 months after surgery, it is recommended to conduct a VEM or Treadmill stress test in order to assess how passable the new bypass paths are and how well the myocardium is supplied with oxygen. If there is no pain or changes on the ECG during the test, then recovery is considered successful.
In case of violation or cessation of medicinal, dietary and physical measures during the recovery period, recurrence of plaques is possible, and re-operation may be refused. In some cases, new narrowings may be stented.
Risks and complications
- postoperative bleeding;
- inflammatory process of a postoperative wound;
- respiratory complications;
- heart rhythm disturbances;
- pain associated with nerve fibers, muscle spasm or dislocation of costal cartilage;
- encephalopathy;
- cardiac weakness, perioperative myocardial damage, stroke, death.
Anyone can calculate the risk of surgery using the international table for calculating the risk of cardiac surgery EuroSCORE II, which takes a few minutes.