Cardiovascular diseases are the scourge of modern society. Many people, both old and young, die from them. The statistics are inexorable. There are many reasons for this - poor environment, many stressful situations, unhealthy diet, bad habits, as well as other related diseases. But the big problem is that one disease entails many others, often much more serious. One of these is intestinal infarction. In addition to being a deadly diagnosis, misdiagnosis often results in a very high mortality rate as it is often too late to do anything about it. In today's material we will discuss what an intestinal infarction is, for what reason it occurs, and what treatment is most effective. In addition, we will tell you how you can identify the first signs of intestinal infarction, and also describe the diagnostic methods used. Read the information carefully, it could save the life of you or your loved ones.
Intestinal infarction is often a complication of cardiovascular disease.
What is the disease
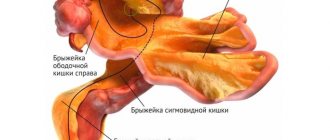
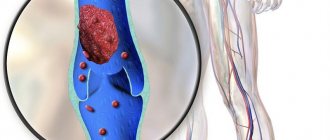
First, let's look at how blood circulation occurs in the small and large intestines. From the aorta, which comes directly from the heart, the so-called mesenteric arteries branch. They are the main blood vessels of the digestive system. In addition to them, the intestine is penetrated by smaller vessels, including veins and capillaries. The blood flowing through them ensures the normal functioning of the small and large intestines. In the presence of cardiovascular diseases or the formation of thrombotic masses in the vessels, partial or complete blockage of the veins and arteries supplying blood to the intestines may occur. If a moment comes when the blood circulation of the vessel is completely stopped, and blood does not flow to a certain part of the intestine, part of its walls will begin to die. This condition is called intestinal infarction. In other words, this is the death of part of the walls of the small and large intestines due to circulatory disorders and thrombosis of the intestinal arteries.
If you do not pay attention to the problem in time, do not make the correct diagnosis and do not take adequate measures, necrosis of the intestinal walls causes peritonitis and its contents enter the abdominal cavity. From now on, the count will go not even by hours, but by minutes. The patient’s life will depend on the qualifications of the medical personnel, but, unfortunately, it often happens that even the most experienced doctor cannot save him. The situation is complicated by the fact that very often the symptoms of intestinal infarction are confused with other surgical diseases, for example, gastric ulcers, and the moment can be hopelessly missed.
Fortunately, it doesn’t just happen, but is a consequence of other serious vascular and heart diseases. Patients after a heart attack, as well as those suffering from atherosclerosis, thrombosis and ischemic vascular diseases are at increased risk. The average age of victims is more than 70 years, but in recent years there have been cases in much younger patients, even younger than 30 years. In the next section, we will look in detail at the reasons why an intestinal infarction may develop.
What is this condition and why is it dangerous?
Intestinal infarction is an acute and life-threatening condition that occurs against the background of circulatory disorders in the main vessels of the organ. Within a few hours after the onset of the disease, necrosis (death) of the tissue of part of the intestine occurs and peritonitis develops - inflammation of the peritoneum.
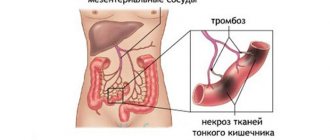
The development of the disease is associated with the characteristics of the intestinal circulatory system. It is carried out due to the vessels of the mesentery - a thin membrane connecting the organ with the posterior wall of the abdominal cavity, and is called mesenteric.
Each part of the intestine is fed by a separate blood vessel and is independent of neighboring areas. Therefore, when it is blocked by a blood clot, part of the intestine is deprived of blood supply and dies. This process is called mesenteric thrombosis.
Until the end of the last century, there were only isolated manifestations of intestinal infarction, while now it accounts for 0.63% of all diseases of the gastrointestinal tract. Older people are most often affected by the disease. More than 60% of them are women. The advanced age of patients and concomitant ailments are problems that arise when deciding on surgical intervention.
Another important task in the successful treatment of the disease is timely and accurate diagnosis. It is almost impossible to do this without special tools. As a result, preparation for surgery takes a long time, during which irreversible processes occur in the intestines, leading to death.
In the International Classification of Diseases (ICD-10), intestinal infarction is coded as K55. 0 and indicates acute vascular diseases of this organ.
Causes of intestinal infarction
The most important causes of intestinal infarction are thrombotic formations in blood vessels. Blood stops flowing into the vessels as soon as the lumen of the vessel closes. The intestinal wall does not receive the necessary nutrition, after which its parts die. But thrombosis also occurs due to very specific reasons. Among them are the following:
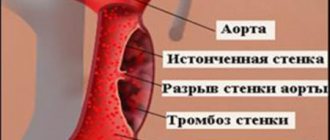
- Vascular atherosclerosis. Cholesterol plaques form on the walls of blood vessels. If treatment is not started in time, they may become more numerous, and after they rupture, blood clots form, which can block blood flow. If they form in the mesenteric arteries leading to the intestines, they can provoke intestinal infarction. When a blood clot breaks away from the wall, thromboembolism occurs, as a result of which death can occur in just a few minutes, and the mortality rate is almost 100%.
- High blood pressure. It is not a direct cause of intestinal infarction, but it provokes the formation of atherosclerotic plaques that develop into blood clots.
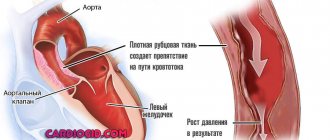
- Heart defects. They cause impaired blood flow in the chambers of the heart, resulting in the formation of thrombotic clots that can block the lumen of the intestinal arteries.
- Rheumatism is an inflammation of the connective tissue of the heart, which further contributes to the formation of thrombotic masses.
- Myocardial infarction is a rupture of the heart muscle, as a result of which thrombotic clots form and spread throughout the body.
- Endocarditis and obliterating endarteritis.
- Varicose veins and thrombophlebitis are the formation of blood clots on the walls of blood vessels, as a result of which their lumen decreases. Under favorable conditions, it can be complicated by intestinal infarction.
- Blood poisoning. Harmful substances contained in the blood contribute to the formation and accumulation of plaques and blood clots and their clogging of the lumen of blood vessels.
- Condition after surgery or complicated childbirth. Any surgical intervention always carries an increased risk of blood clots.
- Taking hormonal contraceptives by women. Although quite rare, they belong to a high-risk group. Such drugs can contribute to the occurrence of thrombophlebitis and even lead to thromboembolism.
- Injuries resulting in damage to large blood vessels. The stronger the damage, the greater the risk of complications in the form of blood clots.
Prevention of myocardial infarction
Prevention of certain complications during myocardial infarction is intended to prevent adverse outcomes and improve treatment results.
Bed rest can lead to pulmonary embolism in a third of patients. The most physiological way of prevention is early activation. If the course of the disease allows, then after 2 days of bed rest, independent visits to the toilet are allowed while using anticoagulant drugs.
Up to 50% of patients die from ventricular fibrillation in the first hours of the disease. Methods for predicting it are unreliable. Prophylactic administration of magnesium preparations reduces the likelihood of developing ventricular arrhythmia by two times, and mortality by three times.
A significant reduction in the risk of recurrent myocardial infarction can be achieved by quitting smoking and correcting arterial hypertension to 140/90 mm Hg. Art. and a decrease in blood cholesterol levels to 5 mmol/l.
Complications accompanying acute myocardial infarction are not inevitable. Many can be prevented or their negative impact can be reduced. It is very important for the outcome of the disease to comply with medical prescriptions and avoid a sedentary lifestyle, as well as excessive activity, and getting rid of bad habits.
For information on rehabilitation and prevention of secondary attacks of MI, watch this video:
Course of the disease
Experts distinguish three stages of intestinal infarction: ischemic, infarct stage and peritonitis. Let's look at each of them in more detail.
- Ischemic. At this stage, there is a predisposition to poor circulation, as well as blockage of blood vessels. If you notice the problem at this stage, you can avoid serious consequences.
- Stage of heart attack. At this stage, part of the large or small intestine dies. The destructive process continues even after blood flow is restored. The protective properties of the intestinal wall gradually decrease, and intestinal bacteria begin to penetrate into the abdominal cavity.
- Peritonitis. The most difficult stage, life is no longer counted by hours, but by minutes. The intestinal tissue disintegrates, and all its contents penetrate into the abdominal cavity, causing very severe inflammation and serious infection.
Symptoms of the disease
It is more difficult to correctly identify the symptoms of intestinal infarction. When it happens, you must immediately call an ambulance. But how can you understand that this is exactly the case and not something else, less serious? Let's look at what symptoms are characteristic of an intestinal infarction.
- Severe abdominal pain with no clear localization. At first it is expressed in short attacks, after which it is felt throughout the abdomen and lasts continuously. It intensifies so much over time that even narcotic painkillers do not help get rid of it.
- The patient unconsciously tries to take a position in which the pain does not cause him severe discomfort. It may be different for everyone, but usually it is lying on your side with your knees pulled up to your chest.
- Frequent loose or pasty stools, often containing mucus and blood.
- Nausea and vomiting, also with bloody impurities.
- Reduced blood pressure in the later stages of the development of the disease, since at the very beginning it is most often standard or even slightly elevated.
- Pallor of the visible mucous membrane due to blood loss.
- Bloating and severe hardening of the abdomen.
- Positive Shchetkin-Blumberg symptom. A qualified specialist can identify it. Its essence is to press the palm of your hand on the anterior abdominal wall, and then sharply release it. With an intestinal infarction, the pain becomes several times more intense.
Manifestations of intestinal necrosis
The disease usually begins suddenly, and the nonspecificity of clinical signs does not allow all patients to make an accurate diagnosis at the initial stage. If the blood flow in the intestinal arteries has already been disrupted for some time against the background of atherosclerosis and periodic spasms, then discomfort in the abdomen is a familiar sensation for the patient. If pain appears against this background, the patient will not always immediately seek help, even if the pain is quite intense.
Symptoms of intestinal ischemia begin with abdominal pain - intense, in the form of contractions, which by the end of the first period of the disease becomes constant and severe. If the small intestine is affected, the pain is localized mainly near the navel; with ischemia of the colon (ascending, transverse, descending) - on the right or left in the abdomen. Complaints of nausea, stool instability, and vomiting are possible. The examination data does not correspond to the clinic, and with severe pain, the abdomen remains relaxed and soft, palpation does not cause increased pain.
Symptoms of intestinal infarction appear after the first period, approximately six hours after the cessation of blood circulation in the arteries or veins. At the same time, the pain intensifies, and symptoms of intoxication appear. In acute thrombosis or embolism, signs of necrosis develop rapidly, starting with intense pain in the abdomen.
The progression of intestinal gangrene and the addition of inflammation of the peritoneum (peritonitis) leads to a sharp deterioration in the patient’s condition:
- The skin is pale and dry, the tongue is covered with a white coating, dry;
- Severe anxiety appears, possibly psychomotor agitation, which is then replaced by apathy and the patient’s indifference to what is happening (areactive peritonitis);
- The pain weakens and may disappear completely, which is associated with total necrosis and death of nerve endings, and therefore this is considered an extremely unfavorable sign;
- The abdomen is initially soft, then gradually swells as intestinal atony worsens and peristalsis ceases.
The Kadjan-Mondor symptom will be specific for intestinal gangrene: when palpating the abdomen, a cylindrical formation of dense consistency is revealed, painful, difficult to displace. This is a fragment of the intestine with the mesentery, which has undergone edema.
A few hours after the onset of ischemia, fluid may appear in the abdomen (ascites); when inflammation occurs, they speak of ascites-peritonitis.
In case of a small intestinal infarction due to blockage of the superior mesenteric artery, vomiting mixed with blood and bile is among the symptoms. As it progresses, the contents of the stomach become fecal in nature.
Damage to the inferior mesenteric artery and gangrene of the thick section can manifest as blood in the stool, which is sometimes excreted copiously unchanged.
In the terminal stage of intestinal infarction, the patient's condition becomes critical. The pain weakens or stops completely, feces and gases do not pass away, intestinal obstruction develops, and severe intoxication is expressed, the patient is apathetic and indifferent, weak, does not show complaints not because of their absence, but due to the severity of the condition. Convulsions and coma are possible. Peritonitis begins 12-14 hours after the vessel is closed, death occurs within the first two days.
Even if you start treatment in the last stage of intestinal infarction, the effect is hardly possible. Irreversible changes in the abdominal cavity doom the patient to death.
Chronic intestinal ischemia may precede acute forms of damage. Its most common cause is atherosclerosis of the aorta, celiac trunk or mesenteric arteries, which provokes a lack of blood flow to the intestines.
Chronic intestinal ischemia is manifested by periodic cramping pain in the abdomen, which appears or intensifies after eating, which is why over time the patient begins to limit himself in nutrition and loses weight.
Impaired passage of contents through the intestines is accompanied by malabsorption, vitamin deficiency, and metabolic disorders. Patients complain of prolonged constipation, which is followed by diarrhea. Lack of blood flow causes a decrease in intestinal motor activity, stool stagnates - constipation occurs. Fermentation of feces provokes periodic diarrhea and bloating.
Low awareness of doctors in the field of identifying mesenteric thrombosis at the prehospital stage significantly affects the results of treatment, which is delayed due to the lack of a correct diagnosis. Another reason for late diagnosis may be the lack of technical capabilities in the hospital itself, because not everywhere there are conditions for urgent angiography, and not every hospital can even boast of having a working CT machine.
It is possible to suspect an infarction of the intestine by the presence of a compacted painful conglomerate in the abdomen, the presence of increased peristaltic sounds, or detection of areas of distended intestine by percussion by a characteristic ringing sound. Ultrasound, X-ray, angiography, and laparoscopy can be used to confirm the diagnosis.
Diagnosis of intestinal infarction
Considering the mortal danger of the condition, it is necessary to establish the correct diagnosis extremely quickly and accurately. Any delay could cost the patient's life. So, what diagnostic methods will help identify intestinal infarction? The first step is to test for the presence of the Shchetkin-Blumberg symptom. If the fears are confirmed, the patient is immediately sent for emergency surgery. If in doubt, the following diagnostic measures can be carried out:
- Clinical blood test. With intestinal infarction, the level of leukocytes and ESR (erythrocyte sedimentation rate) increase. An increase in these parameters indicates the development of inflammation in the patient’s body.
- Angiography. A special substance is injected into the blood vessels, which helps to see the condition of the bloodstream on an x-ray. Ideally, all vessels should be clearly visible, since the injected substance is X-ray contrast. In places where intestinal infarction develops, there will be no contrast.
- Laparoscopy. Under anesthesia, a special tube with a flashlight and a camera is inserted through small incisions in the abdominal cavity. The surgeon will see the condition of the intestines and intestinal vessels on a special monitor.
- Laparotomy. It differs from laparoscopy in that a longer incision is made in the middle part of the peritoneum.
Treatment methods
If thrombosis in a patient leads to intestinal infarction, the only effective treatment is emergency hospitalization and surgery. During the operation, part of the dead intestine is removed from the patient (intestinal resection), if possible, the blood clot that has blocked the vessel is eliminated, and the volume of lost blood is replenished. In no case should you delay the operation, because if the intervention is delayed for more than a day, with a high degree of probability the patient will no longer be able to be saved. The consequences will be dire. If the operation is successful, the patient will need lifelong care. In addition, he will have to administer proteins, fats and carbohydrates intravenously, since most of the intestine, which feeds the body with all its nutrients, may be removed. It will also be necessary to use drugs to reduce the level of thrombotic masses in the blood, and to constantly monitor blood clotting.
Forecast
Most patients have a poor prognosis for recovery and life. Good results can be obtained only when intensive therapy is started in the first 3 to 5 hours from the moment of decreased blood flow through the mesenteric vessels. Even after a successful operation, many patients become disabled.
Intestinal infarction occurs when tissue nutrition is disrupted due to limited blood flow through the mesenteric vessels . This can be caused by: blood clot formation, embolic blockage, spasm or low blood pressure. A typical sign of the disease is severe pain with a soft and painless abdominal wall. An urgent instrumental examination is required to make a diagnosis.
The most informative methods are tomography and angiography, but with the help of conventional ultrasound, you can determine treatment tactics. Medicines are effective in the first hours at the stage of reversible lesions; in the future, only surgery can help. Due to late detection, the prognosis is poor in most patients.
cardiobook.ru
Prevention and prognosis
With intestinal infarction, the prognosis of the disease is most often unfavorable, since in most cases it cannot be detected in a timely manner. When the disease reaches the stage of peritonitis, it is already too late to save the patient. As a preventive measure, it is recommended to lead a healthy lifestyle, monitor your diet, and if you have heart diseases, engage in high-quality and timely treatment.