Myocardial contractility decreases when metabolic processes in the heart are disrupted. A decrease in myocardial contractility can occur for various reasons. The degree of reduction in myocardial contractility can only be assessed indirectly.
Sometimes, when assessing myocardial contractility, doctors note that the heart, even under heavy loads, does not increase its activity or does so to an insufficient extent.
For example, if an athlete exposes himself to excessive physical activity for a long time, depleting the body, over time he may experience a decrease in myocardial contractile function.
For some time, contractility will be maintained due to the use of available internal energy resources. When the cause of a decrease in the contractility of the heart is a serious illness, the situation becomes more serious and requires increased attention.
If you are interested in the question of determining normokinesis of myocardial contractility, only a doctor can explain what it is. The heart muscle has the ability, if necessary, to increase blood circulation volume by 3-6 times. This can be achieved by increasing the number of heartbeats.
The reason for the decrease in contractility is physical overexertion of a person for a long period of time.
Also, impaired contractility can develop with increased metabolism in the body due to hyperthyroidism.
To improve myocardial contractility, drugs are prescribed that improve blood microcirculation and drugs that regulate metabolism in the heart.
Impact of changes in myocardial contractile function
The contractile function of the heart is the main one in its activity as a pump, which is carried out on the basis of the coordination of individual muscle cells.
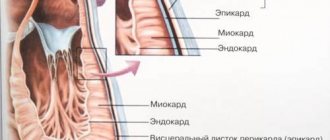
The conversion of chemical energy into mechanical energy occurs in sarcomeres (functional units of the contractile myocardium). Each muscle fiber of the contractile myocardium consists of 200-500 contractile protein structures - myofibrils.
The myocardium consists of two types of cells connected to each other through so-called intercalary signs. Most of the muscle cells of the heart perform a contractile function and are called contractile cells - cardiomyocytes.
If the contractility of the left ventricular myocardium is reduced
Ventricular preload is the diastolic blood volume, which depends to a certain extent on end-diastolic pressure and myocardial compliance.
During systole, the state of the myocardium depends on the ability to contract and the magnitude of the afterload. In the presence of symptoms of insufficient myocardial contractility, a relationship appears between cardiac output and vascular resistance.
Myocardial contractility (contractility) is the property of myocardial fibers to change the force of their contractions.
Features of the myocardium
The myocardium has a number of physical and physiological properties that allow it to ensure the full functioning of the cardiovascular system. These features of the heart muscle make it possible not only to maintain blood circulation, ensuring a continuous flow of blood from the ventricles into the lumen of the aorta and pulmonary trunk, but also to carry out compensatory and adaptive reactions, ensuring the body’s adaptation to increased stress.
The physiological properties of the myocardium are determined by its extensibility and elasticity.
The extensibility of the heart muscle ensures its ability to significantly increase its own length without damaging or disrupting its structure. For reference. The strength of further myocardial contractions during systole (contraction of the heart muscle, ending with the expulsion of blood from the cavities of the ventricles) depends on the degree of myocardial extensibility during diastole (relaxation of the heart muscle).
The elastic properties of the myocardium ensure its ability to return to its original shape and position after the effect of deforming forces (contraction, relaxation) ends.
Also, the ability of the heart muscle to develop strength during myocardial contraction and perform work during systole plays an important role in maintaining adequate cardiac activity.
For reference. Physiological characteristics are manifested by excitability, contractility of the myocardium, its conductivity and automaticity.
What is myocardial contractility?
Cardiac contractility is one of the physiological properties of the heart muscle, which realizes the pumping function of the heart due to the ability of the myocardium to contract during systole (leading to the expulsion of blood from the ventricles into the aorta and pulmonary trunk (TP)) and relax during diastole.
Important. Myocardial contractility is distinguished by a clear sequence that maintains the rhythm and continuity of heart contractions.
First, the contraction of the atrial muscles occurs, and then the papillary muscles and the subendocardial layer of the ventricular muscles. Further, the contraction spreads to the entire inner layer of the ventricular muscles. This ensures a full systole and allows you to maintain a continuous ejection of blood from the ventricles into the aorta and LS.
The contractility of the myocardium is also supported by:
- excitability, the ability to generate an action potential (get excited) in response to stimuli;
- conductivity, that is, the ability to conduct the generated action potential.
Cardiac contractility also depends on the automatism of the heart muscle, manifested by the independent generation of action potentials (excitations). Thanks to this feature of the myocardium, even a denervated heart is able to contract for some time.
What determines the contractility of the heart muscle?
Attention. Myocardial contractility (MC) can be influenced by the nervous system, various hormones and drugs.
The physiological characteristics of the heart muscle are regulated by the vagus and sympathetic nerves, which can influence the myocardium:
- chronotropic;
- inotropic;
- bathmotropic;
- dromotropic;
- tonotropically.
How is reduced contractility treated?
The most accurate assessment of myocardial contractility is possible by performing ventriculography with simultaneous recording of intraventricular pressure. Many formulas and coefficients proposed for clinical practice only indirectly reflect myocardial contractility.
Further improvement in myocardial pumping function can be achieved by using several drugs that improve contractile function (eg, dopamine).
The ideal inotropic agent would appear to increase myocardial contractility without affecting heart rate. Unfortunately, there is currently no such tool. However, the doctor already has several drugs, each of which increases the inotropic properties of the myocardium.
Myocardial hypokinesis is
CREATE NEW MESSAGE.
But you are an unauthorized user.
If you have registered previously, then “log in” (login form in the upper right part of the site). If this is your first time here, please register.
If you register, you will be able to further track responses to your messages and continue the dialogue on interesting topics with other users and consultants. In addition, registration will allow you to conduct private correspondence with consultants and other users of the site.
Hypokinesia – what is it? You can find out the answer to this question from this article. In addition, we will tell you in detail about the reasons for which this pathological condition occurs, describe its types and present treatment methods.
Causes
Hypokinesia is a limitation of a person’s mobility, which can occur due to various reasons. Let's look at some of them in more detail:
- Infections of the central nervous system quite often cause disorders that become the causes of the development of hypokinesia.
- Pharmacological agents sometimes also cause a similar deviation. As a rule, this occurs due to blocking of neuroreceptors.
- Various injuries often cause such a pathological condition as hypokinesia. This can happen after gunshot wounds, falls, severe blows to the head, etc.
- When intoxicated, specific neurons are also affected, which lead to partial immobility or lethargy of a person.
- Vascular disorders often become the causes of isolated infarction, which leads to the development of hypokinesia. By the way, such a deviation often manifests itself in a multi-infarction state.
- Degenerative disorders can quite easily lead to the loss of specific cells with neurotransmitters that are responsible for a person's physiological function.
Only true opinion
There are also three types of disturbances in regional contractility of the left ventricle. Loop T is oriented to zone III of the octant.
Bottom: formulas for calculating left ventricular myocardial mass used in computer programs. The orientation of the moment vectors of the QRS loop changes 0.02 - 0.04 s; they are located in the zone of VIII and V octants.
Post-infarction remodeling of the left ventricle. This is called early left ventricular dilatation.
Increase el. PP activity.
Changes in the myocardium with signs of decreased blood supply in the front and top... At the end of summer, when walking, first coldness, “pins and needles”, numbness appeared in the area of the left shoulder blade, then it turned into a strong burning sensation. Judging by the description, ECG data and, especially, EchoCG, you suffered a myocardial infarction on your legs in the summer. The boundary between akinetic and normal myocardium is sometimes clearly visualized.
VKG for myocardial infarction (anteroseptal - posterolateral)
Despite these limitations, resting echocardiography provides valuable information in coronary artery disease. The absence of disturbances in local contractility of the LV during chest pain practically excludes ischemia or myocardial infarction as a cause of pain (with good visualization of the heart).
The educational and methodological manual is intended for students studying propaedeutics of internal diseases in the system of Higher Professional Education in the specialty "Dentistry"
In addition, the local contractility of different segments of the LV should be compared and the echo structure of the myocardial tissue in the area under study should be examined.
To describe the identified violations of local contractility of the LV and their quantitative expression, they resort to dividing the myocardium into segments.
Disturbances of local contractility in the basins of the right and left coronary arteries are detected during echocardiographic examination with approximately the same frequency. Figure 5.6. Effect of heart rate on left ventricular diastolic filling studies.
What is normokinesis of myocardial contractility?
Dopamine increases myocardial contractility and reduces total pulmonary and total peripheral vascular resistance. Inotropic drugs increase myocardial oxygen consumption, which in turn requires an increase in coronary blood flow.
The purpose of the study was to study the contractile function of the myocardium of the left and right ventricles using radioventriculographic methods.
LVEF in patients on the waiting list for heart transplantation is significantly reduced (Ј 40% in 78% and € 20% in 18% of patients). 13. Kapelko V.I. The importance of assessing ventricular diastole in the diagnosis of heart diseases.
SIMON 111 system
The last mode is the most informative, as it allows you to give not only qualitative, but also quantitative characteristics of myocardial movement.
This is due to an insufficient supply of oxygen and nutrients to the heart muscle, and, accordingly, the inability to synthesize the required amount of energy. It is important to know! Violation of local myocardial contractility entails not only a deterioration in the patient’s well-being, but also the development of heart failure.
It consists of continuously recording heart performance using a portable electrocardiograph attached to clothing. It helps to more accurately assess a person’s condition, as well as the functional characteristics of the heart, and identify disorders if they exist.
It is imperative to prescribe drug therapy, which consists of vitamin preparations and agents that improve metabolic processes in the heart muscle and support the performance of the heart. When a doctor examines a patient’s heart, he necessarily compares the proper performance indicators (normokinesis) and the data obtained after diagnosis.
In the group of patients with mitral defects, end-diastolic pressure in the left ventricle correlated with the value of ventricular end-diastolic volume.
When myocardial contractility decreases, the ventricle does not empty completely. If the volume of blood circulation does not increase with increasing load, they speak of a decrease in myocardial contractility. Assessment of myocardial contractility takes into account its ability to respond to increased load.
mama.freezeet.ru
Features of treatment
Treatment of decreased contractility
When it is noted that the contractility of the heart muscle is reduced due to improper work and rest or nutrition, the person will be given general recommendations that involve restoring the normal balance of states of activity and rest, and may be prescribed vitamin preparations that replenish the energy reserves of the middle layer of the heart.
If global contractility of the left ventricular myocardium is diagnosed, longer treatment will be required. It usually involves the patient taking the following medications:
- phosphocreatine;
- panangin;
- riboxin;
- iron supplements;
- royal jelly.
Additionally, treatment will be carried out aimed at eliminating the root cause of the pathological condition. Its tactics depend on the disease that provoked the development of decreased contractility of the heart muscle. If cardiac diseases occur, drugs will be used aimed at normalizing blood circulation, stabilizing excitability processes in the myocardium, as well as antiarrhythmic drugs.
Interpretation of normal cardiac ultrasound indicators
Examination of internal organs using ultrasound is considered one of the main diagnostic methods in various fields of medicine. In cardiology, ultrasound of the heart, better known as echocardiography, which allows to identify morphological and functional changes in the functioning of the heart, anomalies and disorders in the valve apparatus.
Echocardiography (Echo CG) is a non-invasive diagnostic method that is highly informative, safe and is performed for people of different age groups, including newborns and pregnant women . This examination method does not require special preparation and can be carried out at any convenient time.
Unlike an X-ray examination, (Echo CG) can be performed several times. It is completely safe and allows the attending physician to monitor the patient’s health and the dynamics of cardiac pathologies. During the examination, a special gel is used, which allows ultrasound to better penetrate the heart muscles and other structures.
Content
What allows examination (EchoCG)
Ultrasound of the heart allows the doctor to determine many parameters, norms and abnormalities in the functioning of the cardiovascular system, assess the size of the heart, the volume of the heart cavities, the thickness of the walls, the frequency of strokes, the presence or absence of blood clots and scars.
This examination also shows the condition of the myocardium, pericardium, large vessels, the mitral valve, the size and thickness of the walls of the ventricles, determines the condition of the valve structures and other parameters of the heart muscle.
After the examination (Echo CG), the doctor records the results of the examination in a special protocol, the decoding of which allows one to detect cardiac diseases, deviations from the norm, anomalies, pathologies, also make a diagnosis and prescribe appropriate treatment.
When should it be performed (Echo CG)
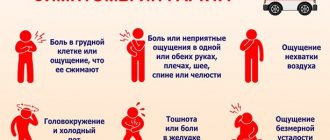
The earlier pathologies or diseases of the heart muscle are diagnosed, the greater the chance of a positive prognosis after treatment. An ultrasound should be performed for the following symptoms:
- periodic or frequent pain in the heart;
- rhythm disturbances: arrhythmia, tachycardia;
- dyspnea;
- increased blood pressure;
- signs of heart failure;
- previous myocardial infarction;
- if there is a history of heart disease;
You can undergo this examination not only with the direction of a cardiologist, but also with other doctors: endocrinologist, gynecologist, neurologist, pulmonologist.
What diseases can be diagnosed by cardiac ultrasound?
There are a large number of diseases and pathologies that are diagnosed by echocardiography:
- ischemic disease;
- myocardial infarction or pre-infarction condition;
- arterial hypertension and hypotension;
- congenital and acquired heart defects;
- heart failure;
- rhythm disturbances;
- rheumatism;
- myocarditis, pericarditis, cardiomyopathy;
- vegetative – vascular dystonia.
Ultrasound examination can detect other disorders or diseases of the heart muscle. In the protocol of diagnostic results, the doctor makes a conclusion, which displays the information received from the ultrasound machine.
These examination results are reviewed by the attending cardiologist and, if any deviations are present, he prescribes treatment measures.
Decoding a heart ultrasound consists of multiple points and abbreviations that are difficult for a person who does not have a special medical education to understand, so we will try to briefly describe the normal indicators obtained by a person who does not have abnormalities or diseases of the cardiovascular system.
Decoding echocardiography
Below is a list of abbreviations that are recorded in the protocol after the examination. These indicators are considered the norm.
- Left ventricular myocardial mass (LVMM):
- Left ventricular myocardial mass index (LVMI): 71-94 g/m2;
- Left ventricular end-diastolic volume (EDV): 112±27 (65-193) ml;
- End-diastolic size (EDD): 4.6 – 5.7 cm;
- End systolic size (ESR): 3.1 – 4.3 cm;
- Wall thickness in diastole: 1.1 cm
- Long axis (LO);
- Short axis (KO);
- Aorta (AO): 2.1 – 4.1;
- Aortic valve (AV): 1.5 – 2.6;
- Left anterior (LA): 1.9 – 4.0;
- Right atrium (RA); 2.7 – 4.5;
- Diastological thickness of the myocardium of the interventricular septum (TMVSD): 0.4 – 0.7;
- Thickness of the myocardium of the interventricular septum systological (TMVPS): 0.3 – 0.6;
- Ejection fraction (EF): 55-60%;
- Miltra valve (MK);
- Myocardial movement (MM);
- Pulmonary artery (PA): 0.75;
- Stroke volume (SV) is the amount of blood volume ejected by the left ventricle in one contraction: 60-100 ml.
- Diastolic size (DS): 0.95-2.05 cm;
- Wall thickness (diastolic): 0.75-1.1 cm;
After the results of the examination, at the end of the protocol, the doctor makes a conclusion in which he reports on the deviations or norms of the examination, and also notes the expected or exact diagnosis of the patient. Depending on the purpose of the examination, the person’s health status, age and gender of the patient, the examination may show slightly different results.
A complete interpretation of echocardiography is assessed by a cardiologist. Independent study of cardiac parameters will not give a person complete information on assessing the health of the cardiovascular system if he does not have special education. Only an experienced doctor in the field of cardiology will be able to interpret echocardiography and answer the patient’s questions.
Some indicators may deviate slightly from the norm or be recorded in the examination protocol under other points. It depends on the quality of the device. If the clinic uses modern equipment in 3D, 4D images, then more accurate results can be obtained, on which the patient will be diagnosed and treated.
Ultrasound of the heart is considered a necessary procedure that should be performed once or twice a year for prevention, or after the first ailments from the cardiovascular system. The results of this examination allow a medical specialist to detect cardiac diseases, disorders and pathologies in the early stages, as well as carry out treatment, give useful recommendations and return a person to a full life.
Sperm count
ok
zoospermia - normal spermogram indicators
and
zoospermia - absence of sperm in the ejaculate (after centrifugation)
necrozoospermia
- increase in the number of dead or immobile sperm
teratozoospermia
- increase in the number of pathological sperm
asthenozoospermia
- decrease in the number of motile sperm
asthenoteratozoospermia
- decrease in the number of motile sperm, increase number of pathological sperm
oligozoospermia
- decrease in the number of sperm in the ejaculate
oligoterato
zoospermia - decrease in the number of sperm in the ejaculate, increase in the number of pathological sperm
oligoastheno
zoospermia - decrease in the number of sperm in the ejaculate, decrease in the number of motile sperm
oligoasthenozoospermia
- decrease in the number of sperm in ejaculate, decreased number of motile sperm, increased number of pathological sperm
cryptozoospermia
- a critically small number of sperm in the ejaculate (after centrifugation)
cryptoterato
zoospermia - a critically small number of sperm in the ejaculate (after centrifugation), an increase in the number of pathological sperm
cryptoastheno
zoospermia - a critically small number of sperm in the ejaculate (after centrifugation), reduction in quantity motile sperm
cryptoasthenoterato
zoospermia – a critically low number of sperm in the ejaculate (after centrifugation), a decrease in the number of motile sperm, an increase in the number of pathological sperm
polyzoospermia
– an increased number of sperm in the ejaculate (>250,000,000/ml)
Hello, is it possible to conceive with such a spermogram? Abstinence 3 days. (02/18/2015) (WHO laboratory standard 2010) Color: milky gray Viscosity: 0 (0-3) pH: 7.3 (7.2 or more) Agglutination: 0 (0-4) Volume: 1 ml (1.5 ml or more) Liquefaction time: 30 minutes (up to 60 minutes) Number of sperm: in 1 ml: 59 million (15 million or more) Number of sperm in the ejaculate: 59 million (39 million or more) Number of other (round) cells: 2.36 million/ml (less than 5 million/ml) Sperm motility (%) Translational movement (PR): 43% (32 or more) Stationary movement (NP): 4% Immotile (IM):53% Overall mobility (PR+NP):47% (40 or more) Note aggregation+ MORPHOLOGY according to strict Kruger-Menkveid criteria Normal:3% (4 or more) Pathology: head and neck:97% Middle part :20% Tail:6% Leukocytes:less than 1 million/ml Spermatogenesis cells:less than 4 million/ml MAR test iG:0% (less than 50%) IgA (if positive IgG>10%:0 (
I made a spermogram, there: transparent, liquefaction time 1 minute, the number of sperm in 1 ml is 9 million, a total of 46 million, actively motile 18, slow 26%, live 68%, dead 32%, normal morphology 47% and pathological 53%. ,betcher crystals +, leukocytes 0-2. What is the percentage of pregnancy naturally?
Having tested and checked a lot, I can say that the surest way to improve sperm quality is sports, diet and proper nutrition. And the doctor also recommended Profertil to my husband as an active dietary supplement that affects sperm quality. This helped us a lot in conceiving a child.
Hello! please decipher the spermogram, thank you in advance MAP test: negative Volume: 3.0 ml Color: yellowish-green Odor: Specific Viscosity: 0.2 cm Liquefaction: 60 min Quantity in million per ml: 29 million Total quantity: 87 million fluidity class A%: 20% mobility class B%: 32% mobility class C%: 42% mobility class D%: 6% A+B+C, %(viability): 94% Agglutination: (+) — Aggregation: (++ ) — Leukocytes: 10-12 in p/zr Epithelium. cells: 0-1 in the subsurface Macrophages: 0-1 — Lecithin grains: (++) — Böttcher crystals: absent — Amyloid bodies: absent — Normal form: 85% Tail pathology: 3% Juvenile: 5% Head pathology: 2% Turbidity: cloudy -
85% of normal sperm is highly questionable. Pregnancy can occur naturally even with 4% normal sperm. But draw conclusions about fertility only based on sperm morphology. wrong. Such indicators of ejaculate as concentration, volume, mobility (a + b) are also important. The fertility index is calculated and if it is equal to or higher than 0.5-0.6, then conception naturally within a year is possible. WHO data on the study of human ejaculate, fifth edition.
Please help. decipher the spermogram analysis: Volume – 2.6 ml., pH – 8, leukemia – 1, round cells – 2, motile sperm in 1 ml. – 7, immobile in 1 ml. – 16,
A spermogram is the main laboratory method for examining sperm for men. It is incorrect to evaluate the “quality” of sperm based on individual indicators - it is necessary to take into account all indicators comprehensively. It is important to understand that even with poor results, conception sometimes happens. If the data obtained differ greatly from the norm, the spermogram is retaken again after 1-2 weeks.
Before submitting sperm (ejaculate) for analysis, it is necessary to properly prepare. The material is collected by the man himself through masturbation into a sterile plastic bottle. In order for the spermogram to be good, it is necessary:
- Do not have sex for 3-4 days, but longer sexual abstinence is not recommended, as the quality of the ejaculate deteriorates.
- On the day of submitting the biomaterial, do not take a hot shower, do not visit the sauna, bathhouse.
- The day before the test, do not drink alcohol or smoke.
- If possible, do not take medications. Many drugs are harmful to sperm and can affect their motility when assessing spermogram parameters.
- Retake the test as recommended by your doctor.
Read more Psychosomatics: thrush in a woman
Inflammation affects normal sperm counts. For example, in case of a “cold”, flu or acute respiratory viral infection, that is, any process that is accompanied by an increase in temperature, a spermogram is not carried out earlier than 2 weeks after the end of the illness. The same rule applies if a man is diagnosed with a disease of the genitourinary system. After a course of prostate massage, a spermogram can be performed within 2-3 days.
In addition, it is important to remember that the most important spermogram indicators will be normal if you avoid heavy physical labor and avoid stressful situations before taking the test.
Ultrasound of the heart
The modern world of diagnostics in cardiology offers various methods that allow timely identification of pathologies and abnormalities. One such method is cardiac ultrasound. Such an examination has many advantages. These are high information content and accuracy, ease of implementation, a minimum of possible contraindications, and the absence of complex preparation. Ultrasound examinations can be performed not only in specialized departments and offices, but also even in the intensive care unit, in regular wards of the department, or in an ambulance during urgent hospitalization of a patient. Various portable devices, as well as the latest equipment, help with such ultrasound of the heart.
What is cardiac ultrasound
With the help of this examination, an ultrasound specialist can obtain an image from which he determines the pathology. For these purposes, special equipment is used, which has an ultrasonic sensor. This sensor is tightly attached to the patient's chest, and the resulting image is displayed on the monitor. There is a concept of “standard positions”. This can be called a standard “set” of images necessary for examination, so that the doctor can formulate his conclusion. Each position implies its own sensor position or access. Each position of the sensor gives the doctor the opportunity to see different structures of the heart and examine the vessels. Many patients notice that during a cardiac ultrasound, the sensor is not only placed on the chest, but also tilted or rotated, which allows you to see different planes. In addition to standard accesses, there are also additional ones. They are used only when necessary.
What diseases can be detected
The list of possible pathologies that can be seen on cardiac ultrasound is very large. We list the main diagnostic capabilities of this examination:
- cardiac ischemia ;
- examinations for arterial hypertension;
- aortic diseases;
- pericardial diseases;
- intracardiac formations;
- cardiomyopathy;
- myocarditis;
- endocardial damage;
- acquired valvular heart defects;
- study of mechanical valves and diagnosis of dysfunction of valve prostheses;
- diagnosis of heart failure.
If you have any complaints about feeling unwell, pain or discomfort in the heart area, as well as other signs that worry you, you should contact a cardiologist. It is he who makes the decision about the examination.
Heart ultrasound norms
It is difficult to list all the norms of cardiac ultrasound, but we will touch on some.
Mitral valve
Be sure to identify the anterior and posterior leaflets, two commissures, chords and papillary muscles, and the mitral annulus. Some normal indicators:
- thickness of mitral valves up to 2 mm;
- diameter of the fibrous ring - 2.0-2.6 cm;
- The diameter of the mitral orifice is 2–3 cm.
- the area of the mitral orifice is 4 - 6 cm2.
- the circumference of the left atrioventricular orifice at 25-40 years old is 6-9 cm;
- the circumference of the left atrioventricular orifice at 41-55 years old is 9.1-12 cm;
- active but smooth movement of the valves;
- smooth surface of the valves;
- the deflection of the leaflets into the cavity of the left atrium during systole is no more than 2 mm;
- the chordae are visible as thin, linear structures.
Aortic valve
Some normal indicators:
- systolic opening of the leaflets is more than 15-16 mm;
- the area of the aortic opening is 2 - 4 cm2.
- the doors are proportionally identical;
- full opening in systole, close well in diastole;
- aortic ring of medium uniform echogenicity;
Tricuspid (tricuspid) valve
- the area of the valve opening is 6-7 cm2;
- the doors can be split, reaching a thickness of up to 2 mm.
Left ventricle
- the thickness of the posterior wall in diastole is 8-11 mm, and the thickness of the interventricular septum is 7-10 cm.
- myocardial mass in men is 135 g, myocardial mass in women is 95 g.
Nina Rumyantseva, 02/01/2015
Reproduction without an active link is prohibited!
Hypokinesia
Hypokinesia, that is, inactivity, is one of the most unfavorable social phenomena, which is a major risk factor for disability and premature death.
The consequences of hypokinesia include a number of systems - the consequences of a lack of movement are visible in the functioning of the circulatory, motor, respiratory and nervous systems.
Hypokinesia is especially dangerous for the elderly and children.
What is hypokinesia?
generalized decrease in physical activity is the most simplified definition of hypokinesia, which perfectly highlights the essence of the problem.
Hypokinesis as a clinical symptom can occur on the basis of neurological diseases, for example, Parkinson's disease, mental illness and severe general diseases that limit motor activity.
Such hypokinesia is often accompanied by progressive akinesia, i.e. complete immobility, paralysis or bradykinesia (slowing of body movements).
Nowadays, the term "hypokinesia" is much more often used in the context of physical inactivity . Therefore, hypokinesis is considered not as an immediate symptom, but as a risk factor for various diseases.
It is not for nothing that the human body is built in such a way that it constantly needs physical activity.
Various forms of activity have accompanied human life for thousands of years, and the right dose of movement is an absolutely necessary element to maintain the psychosomatic balance of the body.
Hypokinesis is the most indirect and direct cause of reduced life expectancy in health after poor nutrition, smoking and alcohol abuse.
The effects of physical inactivity are already evident among school-aged children, mainly on their motor development, but also on mental and emotional ones.
Epidemiological data indicate that the longer the period of hypokinesia, the longer the consequences of lack of exercise become more severe and even lead to permanent disability.
Lack of physical activity, as a medical and social problem, intensified with the development of technology and economics at the beginning of the second half of the 20th century. especially in highly developed countries. The effects of hypokinesia are noticeable in all areas of human life.
Physical activity and human health
Hypokinesia, or the deliberate restriction of movement, is observed in all areas of everyday life of a modern person, despite the fact that the effect of movement on health is public knowledge disseminated by doctors, nutritionists and physiotherapists.
Regular physical activity causes a number of physiological changes that are the most effective way to prevent diseases of civilization, such as coronary heart disease, hypertension or metabolic syndrome.
Sport is health because it contributes to the physical, mental and social well-being of every person.
The consequences of lack of movement are not only poor appearance, decreased self-esteem and chronic lack of energy.
Hypokinesis increasingly leads to various diseases, the treatment of which is lengthy and expensive, and which can be prevented in the least demanding way - by activating one’s physical capabilities.
The influence of physical activity on the human body is assessed taking into account the performance of individual organs or systems, but the main indicators of the positive measurement of physical health are:
- prolongation of healthy life and slowing down the aging process,
- improving quality of life and resistance to fatigue,
- improvement of intellectual functions,
- reduction of cancer risk,
- strengthening physical fitness by influencing the muscular and skeletal systems,
- strengthening mental health,
- assistance in maintaining proper weight and body composition,
- reducing the risk of heart disease, atherosclerosis, tumor diseases, diabetes, hypertension.
Complications of hypokinesia
The impact of sports on health is most often discussed in terms of the movement system, that is, bones, joints and muscles. Any regular physical activity - not only tiring workouts, but also regular walks, cycling, playing with children - increases the density and strength of bone tissue .
It has been proven that in adults, the consequence of hypokinesia is more often osteopenia, osteoporosis, pathological fractures and osteoarthritis.
Hypokinesia in people over 70 also usually results in permanent immobility due to muscle atrophy and lack of coordination. Hypokinesis in children leads to postural defects, which are a consequence of progressive atrophy of the postural muscles that stabilize the growing spine.
Sports, in addition to improving appearance, provide sufficient mobility in the joints, also influencing the shape of the articular surfaces and maintaining the flexibility of tendons and ligaments. Physical effort improves the strength and endurance of muscle tissue, and in combination with the right diet allows for any reconstruction of the body.
Hypokinesis and the cardiovascular system
Physical activity is critical for cardiovascular health, especially for optimizing cardiac function and blood pressure. 150 minutes of moderate-intensity aerobic exercise per week has been shown to reduce the risk of cardiovascular disease (heart attack, stroke).
Hypokinesis in combination with an improper diet has an adverse effect on the lipid profile, that is, on the level of cholesterol and triglycerides, which act directly cardiotoxic and are responsible for the development of atherosclerosis.
Systematic physical activity lowers blood pressure (in some situations it can replace antihypertensive drugs), reduces heart rate and increases its output volume, that is, the volume of blood pumped out of the ventricle during one contraction.
The effect of hypokinesia on the respiratory system
To be able to perform any physical effort, the respiratory system must undergo a period of necessary adaptation.
The first step is to increase ventilation through physical activity, which is the process of inhaling oxygen and exhaling carbon dioxide from the lungs.
A stimulated respiratory center, in addition to increasing respiratory movements, also determines an increase in oxygen levels in the body, which is a consequence of the fact that working muscles require a constant supply of oxygen for intracellular energy transformation.
The oxygen ceiling is a parameter that determines the ability to absorb oxygen.
The effect of hypokinesia is to reduce the maximum amount of oxygen that can be consumed during 1 minute of physical activity. Overall lung capacity also decreases. Lack of movement also predisposes to episodes of shortness of breath even during the least demanding household tasks.
How hypokinesia affects the nervous system
Prolonged hypokinesia leads to decreased muscle strength and impaired coordination of movements. The level of training determines the activation of muscle fibers, and lack of exercise reduces the ergonomics of movements controlled by the central nervous system.
Regular physical activity protects the brain and, by stimulating the production of insulin-like growth factor (IGF-1), triggers neurogenesis, the process of creating new connections between nerve cells.
Physical activity as therapy
The impact of physical activity on human health is multifaceted. It helps maintain a slim figure, strengthens the immune system, and also helps reduce muscle tone. People who exercise have a much better mood, a greater sense of happiness and increased self-esteem.
Sport is physical health, which at the same time helps maintain mental balance. “Movement can replace almost all drugs, but all drugs taken together cannot replace movement,” any doctor will tell you.
Due to the numerous threats arising from hypokinesia, international organizations involved in health promotion involve people in promoting physical activity in all age groups.
Analysis of the long-term consequences of lack of exercise has recognized physical activity as a priority element for maintaining and improving the health of the entire population.
Source: https://tvojajbolit.ru/ortopediya/gipokineziya/
Ultrasound examination of the heart
Ultrasound examination in cardiology is the most significant and widespread research method, which occupies a leading position among non-invasive procedures.
Ultrasound diagnostics has great advantages: the doctor receives objective, reliable information about the state of the organ, its functional activity, anatomical structure in real time; the method makes it possible to measure almost any anatomical structure, while remaining absolutely harmless.
However, the results of the study and their interpretation directly depend on the resolution of the ultrasound device, on the skills, experience and acquired knowledge of the specialist.
Ultrasound of the heart, or echocardiography, makes it possible to visualize organs and great vessels on the screen, and evaluate the blood flow in them using ultrasound waves.
Cardiologists use different modes of the device for research: one-dimensional or M-mode, D-mode, or two-dimensional, Doppler Echocardiography.
Currently, modern and promising methods for examining patients using ultrasound waves have been developed:
- Echo-CG with three-dimensional image. Computer summation of a large number of two-dimensional images obtained in several planes results in a three-dimensional image of the organ.
- Echo-CG using a transesophageal sensor. A one- or two-dimensional sensor is placed in the subject’s esophagus, with the help of which basic information about the organ is obtained.
- Echo-CG using an intracoronary sensor. A high-frequency ultrasonic sensor is placed in the cavity of the vessel to be examined. Provides information about the lumen of the vessel and the condition of its walls.
- Use of contrast in ultrasound examination. The image of the structures to be described is improved.
- High resolution cardiac ultrasound. The increased resolution of the device makes it possible to obtain high-quality images.
- M-mode anatomical. One-dimensional image with spatial rotation of the plane.
Methods of conducting research
Diagnosis of cardiac structures and large vessels is carried out in two ways:
- transthoracic,
- transesophageal.
The most common is transthoracic, through the anterior surface of the chest. The transesophageal method is considered more informative, since it can be used to assess the condition of the heart and large vessels from all possible angles.
Heart ultrasound can be supplemented with functional tests. The patient performs the proposed physical exercises, after or during which the result is deciphered: the doctor evaluates changes in the structures of the heart and its functional activity.
The study of the heart and large vessels is supplemented with Dopplerography. With its help, you can determine the speed of blood flow in the vessels (coronary, portal veins, pulmonary trunk, aorta).
In addition, Doppler shows the blood flow inside the cavities, which is important in the presence of defects and to confirm the diagnosis.
There are certain symptoms that indicate the need to visit a cardiologist and conduct an ultrasound examination:
- Lethargy, the appearance or intensification of shortness of breath, fatigue.
- A feeling of palpitations, which may be a sign of an irregular heart rhythm.
- Extremities become cold.
- The skin often turns pale.
- Presence of congenital heart defect.
- The child is gaining weight poorly or slowly.
- The skin is bluish (lips, fingertips, ears and nasolabial triangle).
- Presence of a heart murmur during a previous examination.
- Acquired or congenital defects, the presence of a valve prosthesis.
- Trembling is clearly felt above the apex of the heart.
- Any signs of heart failure (shortness of breath, edema, distal cyanosis).
- Heart failure.
- Palpation detectable “heart hump”.
- Ultrasound of the heart is widely used to study the structure of organ tissue, its valve apparatus, detect fluid in the pericardial cavity (pericardial effusion), blood clots, and also to study the functional activity of the myocardium.
Diagnosis of the following diseases is impossible without ultrasound:
- Different degrees of manifestation of ischemic disease (myocardial infarction and angina).
- Inflammation of the cardiac membranes (endocarditis, myocarditis, pericarditis, cardiomyopathies).
- All patients are indicated for diagnosis after a myocardial infarction.
- For diseases of other organs and systems that have a direct or indirect damaging effect on the heart (pathology of the peripheral bloodstream of the kidneys, organs located in the abdominal cavity, brain, vascular diseases of the lower extremities).
Modern ultrasound diagnostic devices make it possible to obtain many quantitative indicators with which one can characterize the basic cardiac function - contraction. Even the early stages of decreased myocardial contractility can be identified by a good specialist and therapy can be started on time. And to assess the dynamics of the disease, ultrasound examination is performed repeatedly, which is also important for checking the correctness of treatment.
What does pre-study preparation include?
More often, the patient is prescribed a standard method - transthoracic, which does not require special preparation. The patient is only advised to maintain emotional calm, since anxiety or previous stress may affect the diagnostic results. For example, your heart rate increases. It is also not recommended to eat a large meal before a cardiac ultrasound.
The preparation before performing a transesophageal ultrasound of the heart is a little stricter. The patient should not eat 3 hours before the procedure, and for infants the study is carried out in between feedings.
Carrying out echocardiography
During the study, the patient lies on his left side on the couch. This position will bring the cardiac apex and the anterior wall of the chest closer together, thus, the four-dimensional image of the organ will be more detailed.
Such an examination requires technically sophisticated and high-quality equipment. Before attaching the sensors, the doctor applies the gel to the skin. Special sensors are located in different positions, which will allow visualizing all parts of the heart, assessing its work, changes in structures and valve apparatus, and measuring parameters.
The sensors emit ultrasonic vibrations that are transmitted to the human body. The procedure does not cause even the slightest discomfort. Modified acoustic waves return to the device through the same sensors. At this level, they are converted into electrical signals processed by an echocardiograph.
A change in the type of wave from an ultrasonic sensor is associated with changes in tissues and changes in their structure. The specialist receives a clear picture of the organ on the monitor screen, and at the end of the study, the patient is provided with a transcript.
Otherwise, transesophageal manipulation is performed. The need for it arises when some “obstacles” interfere with the passage of acoustic waves. This could be subcutaneous fat, chest bones, muscles or lung tissue.
Transesophageal echocardiography exists in a three-dimensional version, with the probe inserted through the esophagus. The anatomy of this area (the junction of the esophagus with the left atrium) makes it possible to obtain a clear image of small anatomical structures.
The method is contraindicated for diseases of the esophagus (strictures, varicose veins, inflammation, bleeding or the risk of their development during manipulation).
Fasting for 6 hours is mandatory before transesophageal echocardiography. The specialist does not delay the sensor for more than 12 minutes in the study area.
Indicators and their parameters
After the end of the study, the patient and the attending physician are provided with a transcript of the results.
The values may have age-related characteristics, and the indicators for men and women are also different.
Mandatory indicators are: parameters of the interventricular septum, the left and right parts of the heart, the state of the pericardium and the valve apparatus.
Normal for the left ventricle:
- The mass of its myocardium ranges from 135 to 182 grams in men, and from 95 to 141 grams in women.
- Left ventricular myocardial mass index: for men from 71 to 94 grams per m², for women from 71 to 80.
- The volume of the left ventricular cavity at rest: in men from 65 to 193 ml, for women from 59 to 136 ml, the size of the left ventricle at rest is from 4.6 to 5.7 cm, during contraction the norm is from 3.1 to 4, 3 cm.
- The thickness of the walls of the left ventricle does not normally exceed 1.1 cm; increasing load leads to hypertrophy of muscle fibers, when the thickness can reach 1.4 cm or more.
- Ejection fraction. Its norm is not lower than 55–60%. This is the volume of blood that the heart pumps out with each contraction. A decrease in this indicator indicates heart failure and blood stagnation.
- Stroke volume. The norm from 60 to 100 ml also shows how much blood is ejected in one contraction.
Other options:
- The thickness of the interventricular septum is from 10 to 15 mm in systole and 6 – 11 mm in diastole.
- The normal diameter of the aortic lumen is from 18 to 35 mm.
- The thickness of the wall of the right ventricle is from 3 to 5 mm.
The procedure lasts no more than 20 minutes, all data about the patient and his heart parameters are stored electronically, and a transcript is provided that is understandable to the cardiologist. The reliability of the technique reaches 90%, that is, the disease can be identified in the early stages and adequate treatment can begin.
heal-cardio.ru
How to improve your sperm count
To improve your sperm count and get a chance to conceive, you need to follow certain rules.
- Eliminate stress. Since anxiety and constant tension affect hormonal levels, which affects the quality of sperm.
- Do not drink alcohol/smoking. For example, nicotine reduces the number of male germ cells in the ejaculate, while alcohol causes metabolic disorders.
- To live an active lifestyle. Do fitness 3-4 times a week, but not strength sports (weightlifting, powerlifting). The ideal option is swimming, race walking.
- Limit contact with gadgets. Do not carry smartphones in trouser pockets, as electromagnetic radiation negatively affects the process of sperm maturation.
- Change your diet. It is necessary to include foods rich in vitamins and minerals in the diet, exclude fast food (burgers, fries, processed foods), carbonated drinks, including energy drinks, which worsen sperm counts.
- Conduct a complete examination of the body. To exclude hereditary and chronic diseases (diabetes mellitus, arterial hypertension), infections that may cause lack of conception.
- It is important to understand that you should not expect quick results: spermatogenesis takes an average of 74 days, that is, positive dynamics are possible no earlier than after 2.5 months.
Sperm research (11)
| Code | Name | Term | Price | Order |
| 52-83-210 | Total antisperm antibodies in sperm | 2 w.d. | 630.00 rub. | |
| 71-83-001 | Sowing sperm for microflora with determination of sensitivity to antibiotics* | 4 w.d. | 790.00 rub. | |
| 72-83-001 | Sperm culture for anaerobes with determination of sensitivity to antibiotics* | 6 w.d. | 480.00 rub. | |
| 73-83-001 | Culture of MPO (sperm) for Ureaplasma spp. with determination of titer and sensitivity to antibiotics | 3 w.d. | 1260.00 rub. | |
| 73-83-002 | Culture for Mycoplasma hominis with determination of titer and sensitivity to antibiotics* | 3 w.d. | 1260.00 rub. | |
| 73-83-003 | Culture of MPO (sperm) for Ureaplasma spp. / Mycoplasma hominis with determination of titer and sensitivity to antibiotics | 3 w.d. | 1260.00 rub. | |
| 75-83-001 | Sowing sperm for fungi of the genus Candida with determination of sensitivity to antifungal drugs (sperm) | 5 w.d. | 850.00 rub. | |
| 83-83-001 | Spermogram with Kruger morphology | 1 w.d. | 530.00 rub. | |
| 97-83-300 | Sperm DNA fragmentation test using the TUNEL method (Order only with a spermogram) | 11 w.d. | 6830.00 rub. | |
| 97-83-301 | Electron microscopy of sperm (EMIS) (Order only with spermogram) | 17 w.d. | 9980.00 rub. | |
| 97-83-302 | Sperm biochemistry (zinc, citric acid, fructose) | 3 w.d. | 1300.00 rub. |
IMPORTANT INFORMATION: The information provided is for reference only and is not a public offer. For up-to-date information, contact the Contractor's medical center or call center. The service catalog indicates the maximum possible period for completing the study. It reflects the time it takes to complete the research in the laboratory and does not include the time for delivery of the biomaterial to the laboratory . Please check the deadlines for tests taken at regional medical centers by calling the contact numbers of the centers. To view the list of proposed tests, click on the section of the catalog that interests you.
Read more During pregnancy, menstruation occurs for 2 months
The main purpose of studying the ejaculate is to determine the ability of sperm to fertilize and identify diseases and/or pathological processes that caused the corresponding lesions. Sperm examination is an integral part of the diagnosis of infertility. In approximately 47% of cases, the cause of childlessness in married couples is the man. The cause of male infertility can be diseases of the testicles, prostate, conduction disorders of the deferent ducts, diseases and malformations of the urethra. Examination of seminal fluid is also one of the tests in the diagnosis of hormonal disorders, diseases of the genital organs or malformations.
Normally, ejaculate is a suspension of sperm in the secretion of the testicles and their appendages, which by the time of ejaculation is mixed with the secretion of the prostate gland, seminal vesicles and bulbous-urethral glands.
Sperm make up about 5% of semen volume and are produced in the testes. Approximately 60% of sperm volume is produced in the seminal vesicles. It is a viscous, neutral or slightly alkaline liquid, often yellow or even highly pigmented due to its high riboflavin content.
The prostate produces approximately 20% of seminal fluid volume. This milk-like liquid is slightly acidic (pH about 6.5), mainly due to its high citric acid content. Prostatic secretions are also rich in acid phosphatase and proteolytic enzymes; proteolytic enzymes are believed to be responsible for coagulation and liquefaction of seminal fluid.
Less than 10–15% of sperm volume is produced in the epididymis, vas deferens, bulbourethral and urethral glands.
A standard spermogram evaluates the physical (macroscopic) and microscopic parameters of the ejaculate (Table, Fig. 1-3).
| Index | Characteristic | Interpretation |
| Color | Grayish-whitish, slightly opalescent | Norm |
| Almost transparent | Sperm concentration is very low | |
| Reddish-brownish | Presence of red blood cells | |
| Greenish | Pyospermia | |
| Yellowish | Jaundice, taking certain vitamins, with prolonged abstinence | |
| pH reaction | 7.2–7.8, slightly alkaline | Norm |
| Below 7.0 | In a sample with azoospermia, the presence of obstruction or congenital bilateral absence of the vas deferens | |
| 9.0–10.0, alkaline | Prostate pathology | |
| Volume | 2–6 ml | Norm |
| Less than 1 ml | Androgen deficiency, endocrine diseases, narrowing and deformation of the vesicles, vas deferens |
Conditions for sample collection and storage
The ejaculate must be obtained after at least 48 hours, but not more than 7 days, of sexual abstinence.
The ejaculate obtained by masturbation must be collected completely and kept warm (20–40 ° C). The sample is stable for one hour, however, if sperm motility is pathologically low (less than 25% of sperm with rapid linear forward movement), the period between obtaining and analyzing the sample should be minimized.
Macroscopic examination - determination of the consistency, volume, odor, color, viscosity and pH of the ejaculate.
The sperm obtained during ejaculation is thick and viscous, which is due to the coagulation of the secretion of the seminal vesicles. Normally, at room temperature, the ejaculate sample should liquefy within 60 minutes. If the ejaculate remains viscous, semi-viscous or does not liquefy for a long time, then inflammation of the prostate gland can be assumed. Normally, the volume of ejaculate is 2–6 ml. An amount of less than 1.0 ml is typical for androgen deficiency, endocrine diseases, narrowing and deformation of the vesicles, and the vas deferens. The maximum volume can reach 15 ml. The volume of ejaculate does not affect fertility. The smell of normal ejaculate is specific and is caused by spermine (reminiscent of the smell of “fresh chestnuts”). The specific odor becomes weak or absent when the excretory ducts of the prostate gland are blocked. In purulent-inflammatory processes, the smell of semen is caused by waste products of bacteria that caused the inflammatory process.
Microscopic examination
– study of sperm motility and the presence of agglutination in a native preparation, counting the number of sperm in the Goryaev chamber, studying the morphology of sperm, spermatogenesis cells and differential diagnosis of live and dead sperm in stained preparations.
Microscopic examination of the ejaculate is carried out after its complete liquefaction
A simple categorization system is recommended to assess sperm motility. For classification, 200 spermatozoa are sequentially viewed in 5 microscope fields (Fig. 1).
The motility of each sperm is classified into categories using the following criteria:
A)
fast forward movement;
b)
slow and sluggish movement;
c)
non-forward movement;
d)
immotile sperm.
First, all sperm of categories a and b are counted in a limited area of the visual field or, if the sperm concentration is low, in the entire visual field (%). Next, spermatozoa with non-progressive movement (category c) (%) and immobile spermatozoa (category d) (%) are counted in the same area.
Mobility can be determined by counting in Goryaev’s chamber. The sperm is diluted 20 times with saline; only immobile and inactive sperm are observed in the chamber.
The calculation is carried out according to the formula:
A – total number of sperm;
B – number of sedentary spermatozoa;
C – number of immobile spermatozoa.
Hence the percentage of actively motile sperm is (Y):
Sperm motility depends on the time of year and day. There is evidence that in the spring there is a decrease in sperm motility (seasonal fluctuations). When monitoring the number of actively motile sperm during the day, an increase in their number was noted in the afternoon (circadian rhythms).
A decrease in sperm motility below normal is asthenozoospermia. Minor degree of asthenozoospermia - the number of actively and sedentary sperm with forward movement in total is less than 50%, but more than 30%.
Assessment of sperm agglutination.
Sperm agglutination means the gluing of motile spermatozoa together with heads, tails, or heads with tails. The adhesion of immobile spermatozoa to each other or motile spermatozoa to threads of mucus, other cells or cell debris should be considered and recorded not as agglutination, but as a nonspecific aggregation. During the study, the type of agglutination is recorded (heads, tails, mixed version). A semi-quantitative method can be used to assess the degree of agglutination from “–” (no agglutination) to “+++” (severe degree, in which all motile sperm are susceptible to agglutination). Normally, no more than 3–5% stick together. If the number of agglutinated sperm is 10–15%, we can talk about a decrease in their fertilizing ability.
The total number of sperm is counted in the Goryaev chamber. The total number of sperm in the ejaculate is calculated by multiplying the number of sperm in 1 ml of semen by the volume of semen released.
Normospermia
– in a healthy man, 1 ml of ejaculate contains more than 20 million sperm.
Read more Itches inside the pussy
Polyzoospermia
– the number of sperm in 1 ml of ejaculate exceeds 150 million.
Oligozoospermia
– 1 ml of ejaculate contains less than 20 million sperm.
Azoospermia
– absence of sperm in the ejaculate.
Aspermia
– there are no spermatozoa or spermatogenesis cells in the delivered liquid.
Assessment of sperm viability.
To assess sperm viability, mix one drop of fresh ejaculate with a drop of standard eosin dye on a glass slide. Live spermatozoa in such preparations are not colored (white); dead sperm turn red because... their plasma membranes are damaged. Viability refers to the percentage (as a percentage) of “live” sperm. Viability should be assessed if the percentage of immotile sperm exceeds 50%.
Viability assessment can serve as a control for the accuracy of sperm motility assessment, since the percentage of dead cells should not exceed (taking into account counting error) the percentage of immotile sperm. The presence of a large number of living but immobile sperm may indicate structural defects of the flagella. The sum of dead and live sperm should not exceed 100%.
Characteristics of the cellular elements of the ejaculate.
Typically, the ejaculate contains not only sperm, but also other cells, which are collectively referred to as “round cells”. These include epithelial cells of the urethra, prostate cells, immature germ cells and leukocytes. Normally, the ejaculate should not contain more than 5*106 round cells/ml.
In most cases, human ejaculate contains white blood cells, mainly neutrophils. An increased content of these cells (leukospermia) may indicate the presence of infection and poor sperm quality. The number of leukocytes should not exceed 1106/ml. The counting is carried out in Goryaev's chamber in the same way as sperm counting.
In addition to leukocytes, the ejaculate may contain immature germ cells (spermatogenesis cells) at different stages of maturation: spermatogonia, first-order spermatocyte, second-order spermatocyte, spermatid. (Fig. 2)
The presence of various types of immature spermatogenesis cells in the ejaculate usually indicates a violation of spermatogenesis. The excess of these cells is a consequence of dysfunction of the seminiferous tubules, in particular, with reduced spermatogenesis, varicocele and Sertoli cell pathology.
Assessment of sperm morphology.
For analysis, a smear is used, stained with histological dyes (hematoxylin, Romanovsky-Giemsa, etc.), in which a sequential count of 200 sperm is performed (a single count of 200 sperm is preferable to a double count of 100 sperm) and the number of normal and pathological forms is expressed as a percentage (Fig. 3 ).
The head of the sperm should be oval in shape. The ratio of the length of the head to its width should be from 1.5 to 1.75. A well-defined acrosomal region should be visible, representing 40–70% of the head area. The sperm neck should be thin, 1.5 times the length of the sperm head, and attached to the head along its axis. The size of the cytoplasmic droplets should not exceed 1/2 the size of the head of a normal sperm. The tail should be straight, of the same thickness throughout and somewhat narrower in the middle part, not curled and have a length of about 45 microns. The ratio of head length to tail length in normal sperm is 1:9 or 1:10.
Head defects: large, small, conical, pear-shaped, round, amorphous, with vacuoles in the chromatin area; heads with a small acrosomal region, a vacuolated acrosome, with an asymmetrically located acrosome; double and multiple heads, heads with compact chromatin structure, etc.
Neck and midsection defects: tilted neck (neck and tail forming a 90° angle to the long axis of the head), asymmetrical attachment of the midsection to the head, thickened or uneven midsection, abnormally thin midsection (absent mitochondrial sheath), and any combination of these .
Tail defects: short tails, multiple tails, hairpin-shaped tails, broken tails, slanted tails (angle greater than 90°), uneven tail thickness, thin middle part, curled end, completely curled tail, and any combination thereof. In differentiated morphological counting, only sperm with tails are taken into account.
Teratozoospermia
– an increase in the number of pathological forms of sperm above the reference values. Severe teratozoospermia sharply reduces the chances of fertilization and increases the likelihood of malformations in the fetus if fertilization occurs. Teratozoospermia is usually combined with oligozoospermia and asthenozoospermia.
Spermatozoa in which the head is enclosed in a cytoplasmic drop, and those in which the cytoplasmic drop is located on the neck in the form of a scarf and in relation to the size of the head is more than 1/3, are distinguished as immature or young. In a normal spermogram they make up about 1%.
Why is echocardiography performed?
EchoCG is used to identify changes in the structure of cardiac muscle tissue, dystrophic processes, malformations and diseases of this organ.
A similar study is carried out on pregnant women if there is a suspicion of pathology of fetal development, signs of developmental delay, the presence of epilepsy, diabetes mellitus, or endocrine disorders in the woman.
Indications for echocardiography may include symptoms of heart defects, suspected myocardial infarction, aortic aneurysm, inflammatory diseases, neoplasms of any etiology.
An ultrasound of the heart must be performed if the following symptoms are observed:
- chest pain;
- weakness during physical activity and regardless of it;
- cardiopalmus:
- interruptions in heart rhythm;
- swelling of the arms and legs;
- complications after influenza, ARVI, sore throat, rheumatism;
- arterial hypertension.
The examination can be done at the direction of a cardiologist or at your own request. There are no contraindications to its implementation . There is no special preparation for a cardiac ultrasound; it is enough to calm down and try to maintain a balanced state.
During the study, the specialist
- the state of the myocardium in the phase of systole and diastole (contraction and relaxation);
- the size of the heart chambers, their structure and wall thickness;
- the condition of the pericardium and the presence of exudate in the cardiac sac;
- functioning and structure of arterial and venous valves;
- the presence of blood clots, neoplasms;
- the presence of consequences of infectious diseases, inflammation, heart murmurs.
The results are most often processed using a computer program.
More details about this research methodology are described in this video:
Normal values in adults and newborns
It is impossible to determine uniform standards for the normal state of the heart muscle for men and women, for adults and children of different ages, for young and elderly patients. The figures below are average values, there may be slight differences in each case .
| Indicators | In adults | In newborns |
| Left ventricular wall thickness in systole | 10 – 16 mm | 4 – 5 mm |
| The same - in diastole | 8 - 11 mm | 3 – 4 mm |
| Right ventricular wall thickness | 3 – 5 mm | |
| Thickness of the interventricular septum in systole | 10 – 15 mm | 4 – 8 mm |
| The same - in diastole | 6 – 11 mm | 3 – 5 mm |
| Aortic diameter | 18 – 35 mm | |
| Left ventricular ejection fraction | More than 50% | 66 – 76% |
| Heart rate | 70 — 75 | 120 — 140 |
| Myocardial mass | 90 – 140 g – for women 130 – 180 g – for men |
The aortic valve in adults should open 1.5 centimeters or more, the opening area of the mitral valve in adults is 4 sq.cm. The volume of exudate (liquid) in the heart sac should not exceed 30 sq. ml.
Deviations from the norm and principles for interpreting results
As a result of echocardiography, the following pathologies of the development and functioning of the heart muscle and accompanying diseases can be detected:
- heart failure;
- slowing, accelerating or interrupting heart rhythm (tachycardia, bradycardia);
- pre-infarction condition, post-infarction;
- arterial hypertension;
- vegetative-vascular dystonia;
- inflammatory diseases: cardiac myocarditis, endocarditis, exudative or constrictive pericarditis;
- cardiomyopathy;
- signs of angina pectoris;
- heart defects.
The examination protocol is filled out by a specialist performing cardiac ultrasound. The parameters of the functioning of the heart muscle in this document are indicated in two values - the norm and the indicators of the subject. The protocol may contain abbreviations that are incomprehensible to the patient:
- LVMM – left ventricular mass;
- LVMI – mass index;
- EDD – end diastolic size;
- DO – long axis;
- KO – short axis;
- LA – left atrium;
- RA – right atrium;
- EF – ejection fraction;
- MK – mitral valve;
- AK – aortic valve;
- DM – myocardial movement;
- DR – diastolic size;
- SV – stroke volume (the amount of blood that is ejected by the left ventricle in one contraction;
- ТМВПд – thickness of the myocardium of the interventricular septum in the diastole phase;
- TMMVPs – the same, in the systole phase.
oserdce.com
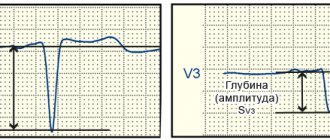
The normal value (normokinesis) of the amplitude of the interventricular septum is within 0.5-0.8 cm, the posterior wall of the LV is 0.9-1.4 cm. Hypokinesis is a decrease in the amplitude of movement, akinesis is the absence of amplitude, dyskinesis is movement of the walls with negative sign, hyperkinesis - amplitude exceeds normokinesis.
Asynchronous movement of the walls of the left ventricle is the systolic movement of one of the walls, not synchronous with the movement of the other wall to the center of the left ventricle (impaired intraventricular conduction, the presence of additional conduction pathways, atrial fibrillation, artificial pacemaker).
Doppler echocardiography also allows assessing the condition of the LV. (Doppler measurement of LV stroke volume.) This method is based on measuring the integral of the linear velocity of blood flow and the cross-sectional area of the vessel at the site of blood flow determination.
The internal diameter of the aortic root is measured in the first half of the systole phase and its cross-sectional area (CSA) is determined:
PPP = 4.
Then the integral flow velocity is determined planimetrically. Multiplying this value by the cross-sectional area of the aorta gives the stroke volume. The product of LV stroke volume and heart rate is the minute volume of blood flow. The use of this formula is incorrect in the presence of aortic disease.
Diastolic function of the left ventricle. It is determined by two properties of the myocardium - relaxation and rigidity. From a clinical point of view, diastole is the period lasting from the moment the sides of the aortic valve close until the first heart sound occurs.
Hemodynamically, diastole can be divided into four phases:
- isovolumic relaxation (from the moment of closure of the aortic valve leaflets to the onset of transmitral blood flow);
- rapid filling phase;
- slow filling phase (diastasis);
- atrial systole.
Diastolic dysfunction can occur with isolated disorders of any of the phases and with their combination.
www.medkurs.ru