Blockage of blood vessels by a blood clot reduces the speed of blood flow, which is manifested by ischemia (arterial thrombosis), venous stagnation. The most common consequences of thrombosis include chronic occlusion of the vessels of the extremities, angina pectoris, transient attacks of cerebral ischemia, and ischemic colitis. With an acute stop in tissue nutrition, organ infarctions and gangrene of the extremities occur.
What is a blood clot
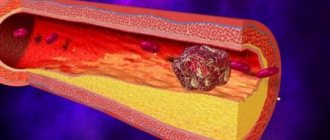
A thrombus is a blood clot that forms when the wall of a vein or artery is damaged. In some cases, it can form inside the heart, as well as in a healthy vessel. It consists of blood cells (mainly platelets) and fibrin strands.
If the thrombus is large, then it becomes an obstacle to the movement of blood - its inflow through the arteries or outflow through the venous system is disrupted. In the first case, the cells lack nutrition and oxygen, which leads to their death. This is how infarctions of internal organs (myocardium, lungs, kidneys, intestines) and brain (stroke) occur.
Venous thrombosis causes swelling and pain in the limbs, but the greatest danger is a detached blood clot. It travels with the bloodstream and enters the pulmonary artery system. A blockage of the branch occurs - pulmonary thromboembolism, which can result in the death of the patient.
We recommend reading the article about ileofemoral thrombosis. From it you will learn about the causes and symptoms, including the acute stage, methods of diagnosis and treatment of ileofemoral thrombosis. Read more about deep vein thrombosis here.
Symptoms of a blood clot
Dizziness or fainting
The combination of chest pain and difficulty breathing can make you feel dizzy and lead to fainting.
Cardiopalmus
If your heart rate increases, this could be a dangerous symptom of a pulmonary embolism. When the clot reaches the lungs, there is a lack of oxygen, and your heart tries to compensate by increasing the heart rate. This is a warning sign that should not be ignored.
Unexplained cough
If coughing attacks appear along with a feeling of shortness of breath and an accelerated heartbeat, this may indicate that a blood clot has formed in your body. A cough may be accompanied by blood, and this is a serious reason to consult a doctor.
The cause of such a cough may be a blood clot in the lungs, which leads to congestion in the airways and manifests itself in the form of a cough.
Strong headache
Many people suffer from chronic headaches, but the pain is often worse than usual. Such unbearable pain can completely incapacitate you, making it impossible for you to concentrate on anything.
However, conventional headache medications may not relieve symptoms. In this case, consult a doctor immediately as this may indicate a blood clot in the brain, which can lead to a stroke.
Pain or tenderness in a limb
It is very difficult to understand that you have a blood clot without medical knowledge, but one of the most common symptoms of this problem is pain in the arm or leg.
If not due to injury, pain may be a warning sign of deep vein thrombosis. In this case, there may be pain when pressing or touching the affected area. To distinguish it from muscle cramps, pay attention to whether the pain gets worse when you walk or bend your leg. If so, there is a possibility of a blood clot.
Even if the clot is present in one leg, you may experience soreness in both legs. This occurs because you try to relieve discomfort in one leg and put more strain on the other leg, which can lead to tension and pain.
What substance is involved in the formation of a blood clot?
The main substance that participates in the formation of a blood clot is fibrin threads. They are formed from a blood protein - fibrinogen. This transformation requires the enzyme thrombin to “cut off the extra” parts. Fibrinogen is synthesized in liver cells and enters the bloodstream from them.
With a deficiency, increased bleeding occurs, and with an excess amount, the risk of thrombosis increases. To study the fibrinogen content, a blood test is prescribed - a coagulogram. The norm is considered to be in the range from 1.8 to 3.5 g/l.
Where do blood clots form - in veins or arteries?
Blood clots form in veins or arteries, as well as in other parts of the circulatory system, where there is blood. It can be:
- capillaries;
- small branches of blood vessels: venules and arterioles (microcirculatory link);
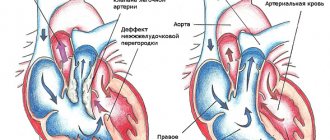
- heart cavity.
For the formation of arterial thrombosis, the main factor is tissue injury (the inner lining of the vessel or heart). With venous it is important to thicken the blood and slow its movement. In the case of small vessel occlusion, plasma composition, intravascular coagulation, and low blood flow are critical.
Diagram of blood clot formation
The formation of a blood clot can be simplified as follows:
- Vessel damage.
- Platelet adhesion and connection.
- Activation of coagulation factors and its result – the formation of fibrin threads.
Two groups of factors are important for vessel damage:
- destruction of the membrane - injury, infection, immune complex, increased content of glucose molecules;
- functional - a decrease in the protective properties of the natural anticoagulant system, which happens during stress, atherosclerosis, burns, and radiation.
For pathological thrombus formation, the presence of 2 groups of signs is required. Normally, when the protective mechanisms work well, with active blood movement there are no conditions for the formation of a large blood clot.
If the process has already started, then another condition is important to maintain it - high blood coagulation activity. It's called thrombophilia. Occurs when the number and rapid activation of platelets increases, blood thickening (dehydration, high cholesterol, glucose).
Stages of thrombosis
Several successive stages of thrombus formation have been identified:
- Injury to the inner lining of the vessel.
- Release of tissue coagulation factors.
- Fixation of platelets at the site of injury.
- The release of platelet substances, which trigger a chain of sequential reactions to form fibrin threads.
- A mesh of fibrin strands traps blood cells.
- A clot forms.
- The thrombus contracts with the release of plasma and becomes denser.
Causes of thrombosis
Thrombogenic risk factors include:
- genetic predisposition;
- blood stagnation during prolonged physical inactivity (sedentary, standing work, immobilization after a fracture, sedentary lifestyle, bed rest);
- increased blood clotting activity (hereditary origin, taking contraceptives, anti-inflammatory drugs, dehydration, surgery or injury, pregnancy);
- circulatory disorders (turbulent blood flows) with arrhythmia, heart attack, prosthetic heart valves, rheumatism, cardiomyopathy;
- changes in the walls of blood vessels with varicose veins, atherosclerosis, aneurysm, vasculitis, diabetic angiopathy;
Varicose veins increase the risk of blood clots - liver dysfunction;
- age-related (hormonal and vascular) changes in men after 45 years, during menopause in women;
- metabolic syndrome, obesity, hypertension;
- smoking and chronic alcoholism.
Causes
All components of a blood clot move freely in the circulatory system of a healthy person. The connection of the constituent elements does not occur spontaneously; there must be certain reasons for the formation of blood clots in the vessels:
- The disease can begin with injury to blood vessels. The damage does not have to be mechanical, it can be the result of radiation, chemotherapy or trauma, inflammation due to infections and even excessive amounts of cholesterol in the walls. When the vessel wall is damaged, fibrin threads appear. They literally “cling” to the first components of the future clot, tying them to the walls of the vessel.
- It is worth remembering that surgery is the most common cause of blood clots, so after surgery it is very common for blood clots to begin to form. Natural childbirth can bring similar results.
- Thrombosis can be a consequence of improper functioning of the coagulation system, because it is responsible for blood clotting and the formation of blood clots. This is usually good for the body; during an injury, the clot prevents the free flow of blood at the site of the rupture. This is enough to wait until the tissue scars, as it saves you from losing precious blood.
- Failure of the coagulation system is often, but not necessarily, associated with congenital pathologies or heredity. Failure also occurs when there is a virus or bacteria in the blood, if the immune system is inhibited by certain medications. The body simply cannot understand what happened and starts a cascade of blood clotting, creating the basis for the formation of blood clots.
The reason why blood clots form is not always the result of a short process. In sedentary people, circulatory problems occur due to squeezing of blood vessels. Typically, this disorder occurs due to varicose veins, excess weight, pregnancy, or taking hormonal medications in women. Some scientists even argue that the risk of thrombosis for this reason is associated with height, so it occurs more often in people who are too short or too tall.
The first signs of a blood clot
The early stages of vascular thrombosis are manifested by symptoms of poor blood supply and impaired outflow from the affected area. They occur during exercise, disappear or decrease after rest, periods of deterioration of the condition alternate with a fairly long normalization of well-being. It should be noted that it is the initial signs that are reversible and respond well to treatment, since at this time irreversible changes in the organs have not yet had time to develop.
Thrombosis can be suspected based on the following symptoms:
| Localization location | Symptoms |
| Arteries of the extremities | cold hands or feet, fatigue, low exercise tolerance, intermittent claudication after a long walk |
| Veins on the arms or legs | swelling at the end of the day, heaviness, feeling of fullness, tingling, appearance of a network of dilated vessels on the skin |
| Coronary arteries | after physical or emotional stress of high intensity, discomfort or pressing pain in the heart, weakness, difficulty breathing appears |
| Brain vessels | tinnitus, occasional dizziness, blurred vision, forgetfulness, absent-mindedness, decreased ability to coordinate movements, slight or occasional unsteadiness of gait |
| Intestinal arteries | abdominal pain without clear localization and connection with food intake, worsens after physical exertion, bloating, alternating diarrhea and constipation |
All these signs are not specific to thrombosis; they also occur in other diseases, so it is important to be examined as early as possible. To detect blockage of a vessel and determine the cause, you need to contact a surgeon (pain and swelling of the extremities), a cardiologist, a neurologist for symptoms of the heart, brain, or a gastroenterologist for digestive disorders.
Diagnosis is carried out using angiographic studies, ECG and ultrasound of blood vessels, often with stress tests.
Prevention of thrombosis
Measures necessary to avoid blood flow problems:
- stable physical activity, combating physical inactivity - proper formation of working conditions, therapeutic exercises, walking in the fresh air;
- following simple rules during long trips - warming up your knees and ankles, drinking enough fluids, wearing comfortable clothes;
- hardening the body, strengthening the immune system, reasonable nutrition rich in vitamins;
- giving up negative habits - alcohol and tobacco;
- wearing compression clothing - stockings, tights, knee socks;
- stopping the use of restrictive clothing - belts, tight elastic bands on underwear, corsets, narrow shoes, tight-fitting clothing;
- exclusion of various types of thermal procedures - baths, baths, saunas, prolonged exposure to the scorching sun;
- therapeutic diet;
- taking medications at critical stages and under increased stress - various vitamins, acids and anticoagulants.
Both treatment and prevention should be prescribed by an experienced specialist; do not self-medicate!
How to recognize a blood clot
A blood clot can be recognized if it interferes with blood circulation and symptoms of thrombosis appear:
| Type of thrombosis | Symptoms |
| Deep veins of the leg | Distension, pain, it becomes stronger when palpated in the area of the affected vessel, swelling, redness or bluish color of the skin, an increase in its temperature, a pronounced venous network, congested veins. |
| Pulmonary artery | Sudden onset of shortness of breath, bluish skin with a gray tint, drop in pressure, chest pain, heart rhythm disturbances, bulging neck veins, fainting, cough, wheezing, pinkish sputum, increased body temperature, pain in the right hypochondrium. |
| Coronary arteries of the heart | Pain behind the sternum, radiating to the back and neck, occurs during stress, physical activity, and is accompanied by shortness of breath and rapid heartbeat. |
| Arterial network of the legs | Chilliness, numbness of the feet, burning, pain when walking, which stops when you stop, the skin becomes pale, and then the fingers turn blue. |
| Cerebral arteries | Dizziness, unsteadiness, various visual disturbances, unclear speech, decreased muscle strength and sensitivity in the arm and leg, memory loss. |
Symptoms
Thrombosis is a dangerous disease, as it is not always possible to detect it in the early stages. External symptoms of the presence of blood clots do not appear immediately, and with a mild course of the disease they may be completely absent. Other signs of a blood clot are very varied and largely depend on where the compaction is located and how severe the disease is.
It is characteristic of superficial vein thrombosis that it can be detected by palpation, since it is close to the surface of the skin. Such a clot is a dense formation; in the primary stage it is soft, but upon palpation you can feel a hard formation. Additional symptoms include redness of the skin, swelling of the limb, and increased temperature at the site of the blood clot. Swelling develops over several hours and hurts when pressed. Symptoms of superficial thrombosis can sometimes be confused with infection.
Symptoms of a venous thrombus in the deep veins are redness and swelling, as in the previous case. The affected area will be warmer, the temperature of the whole body will most likely rise, and fever is possible. The patient feels pain when pressing on an area close to the source of inflammation. Traces also appear on the skin - blue spots.
The most dangerous are arterial blood clots. Symptoms of blood clots largely depend on the organ affected. Thrombosis of the arteries in the heart refers to coronary heart disease, therefore, among the signs:
- dyspnea;
- pain behind the sternum, which radiates to the arm or back;
- increased sweating;
- nausea.
Arterial thrombosis in the extremities leads to severe pain and pallor of the skin, a decrease in the temperature of tissues deprived of blood supply. In such situations, the patient needs urgent medical care, only this gives a chance to save the affected arm or leg from amputation.
Arterial thrombosis in the head causes more obvious disorders that are noticeable to others. Problems with speech, coordination, swallowing, vision, muscle strength and movement. Symptoms of a blood clot have a lot of overlap with stroke, as it is the most common outcome if left untreated.
Blood clots located in the arteries of the brain often cause strokes; such lesions can be identified by the loss of speech, vision, and sensitivity. Symptoms are usually temporary, but recovery may take quite a long time. In addition, there is no guarantee that there will be a complete recovery.
The main complication of venous thrombosis is the detachment of a blood clot, its migration with the bloodstream to the lungs and the development of pulmonary embolism (PE). PE is a life-threatening disease that manifests itself with the sudden onset of chest pain, shortness of breath, and coughing with blood. In severe cases, a drop in blood pressure and loss of consciousness develops, and cardiac arrest is possible.
Portal expert, first category doctor Taras Nevelichuk.
The main signs of formation and symptoms
The formation of a blood clot in the veins or arteries becomes an obstruction to blood circulation. At the stage of pronounced clinical manifestations, patients develop ischemic syndrome of varying degrees of intensity or venous stagnation.
Vein thrombosis of the extremities
The presence of a blood clot in the venous network of the upper or lower extremities (more common) may be accompanied by the following symptoms:
- swelling;
- heaviness in the legs or arms;
- increased fatigue;
- decreased load tolerance;
- pain along the vein;
- redness of the skin;
- expansion of subcutaneous vessels (mesh pattern);
- an increase in local temperature.
At first, these signs appear only during exercise, and disappear after a night's rest. As they progress, they also appear at rest.
Arterial thrombosis in the arm or leg
Symptoms are associated not only with blockage of blood vessels, but also with spasm of the arterial walls. The main manifestations of ischemia of tissues of the extremities:
- pale and cold skin;
- chilliness of the feet or hands;
- pain of varying intensity, changing with movement;
- weakening of the pulsation of the arteries below the site of blockage;
- numbness of the limbs, tingling.
In heart
The occurrence of chest pain during physical or emotional stress is the main sign of coronary thrombosis. In the vast majority of cases, it is associated with atherosclerosis of the arteries. The attacks can be short-term, and the pain is tolerable or long-lasting, unbearable with fear of death.
In addition to the heart area, painful sensations also extend to the left half of the body, shoulder blade, or may be atypical (abdomen, right limbs). Relief occurs at rest, after taking Nitroglycerin.
Thrombosis of coronary vessels
In my head
With incomplete blockage of cerebral vessels, transient disturbances of cerebral circulation occur. The source of the thrombus is most often an atherosclerotic plaque in the carotid, vertebral or intracerebral artery. Clinical signs may include:
- unsteadiness when walking;
- speech disorder;
- decreased vision - blurred outlines of objects, double vision, brief episodes of blindness or loss of visual fields;
- dizziness;
- muscle weakness in the limbs;
- facial asymmetry;
- loss of skin sensitivity;
- convulsive muscle twitching;
- changes in memory - disorientation in space, inability to remember and reproduce current information, repetition of words.
CT angiography of cerebral vessels
Such attacks of cerebral ischemia can disappear within 24 hours or transform into an ischemic stroke.
Headache due to thrombosis
Headache due to thrombosis occurs when the arteries, veins and sinuses of the brain are blocked. Typical signs:
| Type of thrombosis | Symptoms |
| Arterial (ischemic stroke) | Elderly patients, the condition gradually worsens, speech, movement and sensitivity of the limbs are impaired (paralysis), visual fields are lost. Headache occurs more often in the occipital or temporal region. |
| Venous | It begins with a severe headache with nausea and vomiting, impaired consciousness, movement of arms and legs on half the body, convulsions are possible, and symptoms change as they progress. |
| Venous sinuses | It occurs as a complication of otitis media, sinusitis, there is a constant increasing headache, it is not affected by painkillers, it intensifies with physical stress, in a lying position, fever, and vomiting are noted. |
Pain from a blood clot
Pain from a blood clot can appear in different parts of the body; symptoms depend on the location of the blockage, the type and size of the vessel, and the presence of bypass circulatory pathways. The following signs are possible:
- deep veins of the leg - distension in the leg, pain along the affected vein, increases when palpated, there is swelling, redness of the skin, a distinct venous pattern;
- coronary arteries - attacks of angina pectoris (retrosternal pain), intensifying with movement, subsiding with rest, relieved with Nitroglycerin, possibly spreading to the left half of the body, neck, a prolonged attack means the development of a heart attack;
- cerebral vessels - focal signs of destruction of brain tissue (muscle weakness, sensitivity disorders), speech impairment, swallowing, unsteadiness when walking, blurred vision;
- pulmonary arteries - sudden chest pain, shortness of breath, cough, fever, bluish skin;
- renal - lower back pain, similar to renal colic, blood in the urine.
Intestinal ischemia
Pain in the abdomen becomes almost constant, stool becomes more frequent, mucus and blood streaks appear in it, and then blood is almost always found in the stool. Eating and physical activity contribute to increased pain. The duration of the attack can be from 0.5 to 5 hours. There is loss of appetite, emaciation, nausea and periodic vomiting.
Blood clots: what causes them? Mechanisms of formation and types of blood clots
It is important for every modern person to know the causes of blood clots.
Without understanding the mechanism of disease development, it is impossible to prevent it. Thrombosis is a dangerous condition that in some cases leads to death.
If previously it was believed that only older people were at risk, today the disease also affects young people, so it is important for everyone, without exception, to follow the principles of prevention.
Causes of blood clots
The formation of a clot in the lumen of a vessel is a consequence of damage to the inner wall. This occurs under the influence of various pathogenetic factors.
As a result, the state of the endothelial layer changes, which provokes the release of large amounts of interleukin into the blood. This substance promotes the aggregation of blood cells.
The platelets arriving at the site are destroyed, thromboplastin and thrombin are released from them, this significantly increases the viscosity of the blood.
The release of prothrombinase is aimed at activating prothrombin, from which fibrin is formed.
Its fibers are located in the cavity of the vessel in such a way that a mesh is formed; it is this structure that serves as the basis for the future blood clot and retains the formed elements, which allows limiting the flow of blood.
This is a physiological process that allows you to stop bleeding, but its intensification leads to the development of thrombosis.
When determining why blood clots form, the main reasons should be highlighted:
- damage to the vessel wall;
- blood thickening is caused by autoimmune processes, cancer pathology, dehydration of the body;
- slowing of blood flow - people at risk are those leading a sedentary lifestyle, suffering from varicose veins, high blood pressure;
- increased blood clotting.
A common cause of blood clots in the arteries is atherosclerosis. Cholesterol, deposited on the wall, forms an atherosclerotic plaque. The body evaluates such a formation as a defect, and thrombus formation mechanisms are triggered.
Unlike arterial thrombosis, venous thrombosis is not characterized by cholesterol deposition. When a vein is blocked, the main thing is damage to the wall, which occurs as a result of 2 processes:
- phlebothrombosis – the main significance is inflammation of the vascular wall, which occurs as a result of exposure to an infectious agent, with valve disease, varicose veins;
- thrombophlebitis - the formation of blood clots not associated with inflammation.
Types of blood clots and mechanisms of their formation
Depending on the structure and properties, there are several types of thrombus:
- white - occur more often in the vessels of the arterial network, consist of fibrin, leukocytes and platelets;
- red - contain fibrin, platelets and erythrocytes;
- mixed - they are more common than others, they have in their structure a head with the structure of a white blood clot, a body - a mixed substance and a tail - a red blood clot;
- hyaline blood clots cause capillary blockage and are composed of red blood cells, proteins and platelets.
White blood clots form in vessels with good blood flow , they increase slowly, are located perpendicular to the blood flow, gradually the structure becomes voluminous and resembles coral in shape.
The substance has a gray or white color and a textured surface. Red blood clots form in vessels with slow blood flow . These clots are usually loosely bound to the surface and affect the veins.
Hyaline clots form after burns, shocks, electric shocks, and extensive damage to the skin.
The greatest danger is the tail of a mixed thrombus. It is located against the blood flow and can easily come off, causing an embolism. In addition, if it reaches a large size, it can lead to the separation of the entire blood clot, which causes blockage of large vessels.
Depending on the location of the blockage, the following types of thrombosis can be distinguished:
Based on the degree of blockage of the vessel, the following types of blood clots are distinguished:
- parietal (cover part of the vessel, form in large veins and arteries);
- obstructive (covers the entire lumen, located in small vessels);
- axial (attached by the head).
How to recognize blood clots
Vein blockage can be recognized by the following manifestations: symptoms of outflow disturbance (heaviness, swelling, distension), pain. The severity of symptoms depends on the degree of damage to the vessel. Blockage of deep vessels causes the blood flow to be redirected to the superficial veins, they bulge and become visible. Arterial thrombosis manifests itself as slowly increasing signs of ischemia.
You can find out whether pathological thrombus formation is occurring and identify its location thanks to specific symptoms:
- when the pulmonary artery is damaged, chest pain occurs, the skin turns pale or blue, the veins in the neck are swollen, and wheezing occurs;
- portal vein thrombosis is associated with chest pain, bloating, indigestion, vomiting, change in stool color;
- blood clots in the veins of the legs are manifested by swelling, pain while walking, unpleasant sensations on the inner surface of the thigh and foot, and cramps;
- blockage of blood vessels in the upper extremities has symptoms in the form of swelling, pain, blue discoloration;
- damage to the blood vessels of the brain is manifested by headache and dizziness, loss of consciousness, convulsions, nausea, vomiting, hearing and vision impairment;
- blockage of the mesenteric vessels is indicated by dull pain in the body, bloating, increased body temperature, nausea, vomiting, and deterioration of the patient’s condition.
Every patient should understand how to know if thrombosis has occurred. Especially people at risk. If you detect the first signs of pathology, you should consult a doctor who will confirm or refute the diagnosis and prescribe treatment.
Diagnostics
How to determine whether a blockage of blood vessels has occurred or whether the symptoms have another explanation? The diagnosis is established based on the patient's complaints and objective symptoms. It is often possible to detect a blood clot in the body without special equipment.
An experienced doctor can determine the presence of a blockage through examination and functional tests.
Laboratory and instrumental research methods are informative, but auxiliary diagnostic methods; they allow you to check the body for blood clots when the available objective data is insufficient.
- Laboratory tests make it possible to determine signs characteristic of thrombosis: an increase in ESR to 30-40 millimeters per hour, with stagnation of blood in the veins, anemia is diagnosed. Changes in urine occur when the inferior vena cava is blocked. Determining the state of the blood coagulation system is important during hypercoagulation. Acute thrombosis is manifested by a positive C-reactive protein reaction and elevated fibrinogen levels.
- Magnetic resonance angiography is an x-ray method that involves the introduction of a contrast agent. As a result, the patency of the vessels is assessed.
- Phlebography is a type of angiography, a contrast study of veins. A substance is injected into the vessels of the foot or femoral vein, after which several photographs are taken. An accumulation of contrast is detected at the site of the lesion.
- Rheography is a method for determining the state of blood flow through vessels. A special device delivers a series of weak electrical impulses to the tissue. The results are recorded and then decrypted.
- Doppler ultrasound is a method of examining veins using Doppler. This method is painless, allows you to check the vessels for the presence of blood clots, assess the condition of the vascular wall and the speed of blood flow, and also localizes the lesion. Ultrasound scanning is used everywhere, but the accuracy depends on the technical parameters of the device and the qualifications of the specialist.
- Duplex scanning allows you to assess the condition of the vessel and the blood flow in it. During the study, it is determined whether there is any obstruction in blood flow; if there is a blockage, the risk of clot rupture is assessed, and the focus and density of the clot is determined.
- Magnetic resonance imaging is a highly accurate research method that allows you to examine the vessels of the brain, neck, coronary and vertebral arteries. It determines the narrowing of the lumen of the vessel, the presence of a clot, atherosclerotic deposits and other types of violation of the integrity of the vascular wall.
- Computed tomography determines the presence of inflammation of the vascular wall, blood clots, and evaluates the condition of the valves.
- Thermography is a diagnostic method based on the assessment of infrared radiation of tissues and organs. Deviation of indicators indicates the presence of pathology. This method is informative and allows you to check the vessels of the legs for the presence of blood clots, as well as early signs of varicose veins.
Treatment methods
In each case, the decision on how to remove blood clots from blood vessels is made individually, depending on the patient’s condition, the form and location of the disease. When the lower extremities are affected, an obligatory component of complex therapy is the use of elastic bandages; this reduces symptoms and prevents complications. All thermal procedures are prohibited.
Conservative treatment begins with diet. The diet includes vegetables and fruits, lean meat, fish, and dairy products. Spicy, salty, fatty dishes, on the contrary. Completely prohibited.
The following groups of drugs are used for drug therapy:
- anticoagulant (Heparin);
- antispasmodics (No-shpa);
- thrombolytic therapy (Streptokinase, Urokinase);
- antiplatelet agents (Aspirin);
- means for improving trophism (Reopoliglyukin);
- sedatives;
- antiarrhythmic drugs for blockage of coronary arteries;
- analgesics.
It is possible to administer drugs that dissolve the blood clot directly into the lesion. This procedure is called thrombolysis. However, it is effective when the clot is not compacted, within 72 hours from the moment of formation.
Surgical therapy is carried out when medication is ineffective or there is a threat to the patient’s life. A thrombectomy operation is performed.
The blood clot is removed, and the affected vascular wall is replaced with a prosthesis. In addition, stitching, bypassing and vascular ligation can be used.
In patients at high risk of pulmonary embolism, vena cava filters are installed in the inferior vena cava.
Prevention
Thrombosis can develop in anyone. Prevention must be carried out comprehensively. In the presence of a hereditary predisposition, this is especially true. Basic measures:
- normalization of physical activity and elimination of physical inactivity;
- if you are forced to stay in one position for a long time, for example, when flying or traveling by bus, you should periodically perform exercises on the ankle and knee joints and wear loose clothing;
- prevent infectious diseases and strengthen the immune system;
- stop smoking and drinking alcohol;
- use of compression hosiery;
- refusal of tight clothes and underwear;
- cold and hot shower;
- weight normalization;
- proper nutrition;
- taking multivitamin complexes;
- antiplatelet therapy if there is a risk of thrombosis;
- early onset of activity in the postoperative period.
A disease such as thrombosis has a significant relationship with risk factors. Compliance with preventive measures will significantly reduce the risk of developing blockage of any location.
If the blockage has already developed, you should immediately seek medical help, this will prevent the development of complications.
Also, people who have had thrombosis should remember that there is a risk of relapse, so they should periodically visit a doctor to monitor the condition.
: What is a blood clot?
Source: https://bloodvessel.ru/tromby/trombi
How to find out if there are blood clots in the body
To find out whether there are blood clots in the body, you must first contact a phlebologist, who examines the limbs and conducts a march test - applies an elastic bandage to the entire leg from the toes to the groin. After this, the patient needs to walk until pain appears. If it occurs after a few minutes, and the superficial veins have not disappeared, then there is a high probability of a blockage. To confirm the diagnosis, the following is prescribed:
- Ultrasound of the vessels of the lower extremities with Doppler sonography;
- phlebography;
- rheovasography;
- radionuclide scanning (if indicated).
To identify arterial thrombosis, clinical manifestations are taken into account:
- pain in the heart during physical and emotional stress, angina attacks;
- intermittent claudication – you need to stop when walking due to severe pain;
- dizziness, headaches, memory impairment, fatigue during mental work.
In the first case, further examination is carried out by a cardiologist using:
- medical examination - identifying edema, changes in skin color, measuring blood pressure, listening to heart sounds;
- ECG, EchoCG, if necessary, with stress tests;
- blood tests for coagulability and cholesterol content (coagulogram and lipid profile), glucose level;
- general blood test with platelet count.
Example of a blood test with platelet count
If there are signs of thrombus formation, then coronary angiography is required to decide on surgical treatment. When there is blockage of the vessels of the lower extremities with attacks of pain in the legs when walking, the patency of the arteries is assessed by a vascular surgeon during:
- inspection;
- measuring pressure on the legs and arms;
- feeling the pulse;
- Ultrasound with duplex scanning;
- angiography (injection of a contrast agent) and assessment of its distribution using X-rays or tomography.
The condition of the cerebral arteries is examined by a neurologist. It determines reflexes and changes in sensitivity and movements. For visualization of blood vessels the following is used:
- rheoencephalography;
- electroencephalography;
- Ultrasound with Doppler sonography;
- Vascular MRI.
MRI of cerebral vessels
Treatment
Medication:
- when the leg veins are blocked, heparin-based medications, venotonics, and wearing elastic bandages and compression stockings are prescribed;
- To remove stagnation, anticoagulants and thrombolytics are prescribed;
- narrowed coronary arteries require the use of Nitroglycerin and antiplatelet agents;
- for encephalopathy, antihypoxic drugs are prescribed;
- during atherosclerosis, a treatment complex with statins, membrane stabilizers, and vasodilating drugs is used.
If medications do not bring any effect, then surgery is performed.
Surgically:
- coronary bypass surgery – blood flow in the heart is restored by installing a vascular prosthesis;
- stenting – expansion of stented vessels using a frame. Removal of fragments of affected areas surgically.
It is possible to install a filter that stops the movement of a severed blood clot.
How to check blood vessels for plaques and blood clots
In order to check the vessels for the presence of plaques and blood clots, an ultrasound with Doppler ultrasound is performed. Using this method you can evaluate:
- the presence of an obstacle to the movement of blood;
- the total diameter of the vessel and its patency;
- blood flow speed;
- thrombus density;
- its danger (mobility).
Dopplerography of vessels
If the data obtained is not enough to select a treatment method, then angiography is used. It involves the introduction of a contrast agent. Most often it is prescribed before surgery. One method of searching for a blood clot is the injection of fibrinogen labeled with radioisotopes. He will indicate hidden blood clots, but will not be able to determine their structure, size and risk of rupture.
How does a blood clot come off?
A thrombus (floating clots, or floating clots) comes off if its attachment to the wall of the vessel is fragile. A sharp jump in pressure or physical stress is enough for it to begin to move through the venous or arterial network. A blockage occurs in the branches of the pulmonary artery carrying venous blood, if it was in the veins or arteries of internal organs when forming in the arterial network, the left atrium.
Diagnostics
The diagnosis of thromboembolism must be made as soon as possible, since prolongation of diagnosis leads to irreversible changes in the absence of treatment, which determines an unfavorable prognosis.
The main criteria on the basis of which a doctor may suspect thromboembolism:
- Clinical picture of the disease, its sudden onset;
- Premorbid background (the presence of concomitant pathology of the endocrine glands, a disorder in the blood coagulation system, prolonged physical inactivity of the patient as a result of illness or surgical intervention, thrombophlebitis of the veins of the lower extremities, excess body weight, etc.).
At the clinic of various thromboembolisms the following is carried out:
- X-ray of the mediastinal organs with angiopulmonography - triangular atelectasis, increased airiness of the lung due to compensatory mechanisms are observed, with contrast, a break in the branch of the pulmonary artery is observed.
- ECG is the “gold standard” for diagnosing myocardial infarction. With other thromboembolism, nonspecific compensatory changes are also observed: increased heart rate, signs of hypoxia during pulmonary embolism.
- X-ray of the abdominal organs if thromboembolism of the mesenteric vessels is suspected - signs of dynamic intestinal obstruction.
- Diagnostic laparoscopy - detection of areas of visible intestinal necrosis.
- MRI of the brain - identifying areas of ischemic stroke in cerebral thromboembolism.
- Blood coagulation tests are mandatory.
Diagnostic measures also help to clarify the mechanism of blood clot formation and answer the question of why a blood clot breaks off in a person (diagnosis of concomitant pathology that led to thrombus formation).
Signs of a broken blood clot
The detached blood clot moves through the vessels until it causes blockage; signs appear depending on the size and location:
- sudden death (with damage to a large pulmonary artery) within a few minutes;
- increased pressure in the vessels of the lungs (medium-caliber branches are blocked) - shortness of breath, cough, attacks of suffocation, bluish skin;
- focal destruction of lung tissue (infarction-pneumonia) - chest pain, aggravated by coughing and breathing, hemoptysis, high fever.
The rupture of an intracardiac thrombus, which was previously located in the left atrium, leads to the circulation of clots in the blood through the arterial network. They can get into the brain and internal organs. This leads to the following symptoms:
| Consequence of a detached blood clot | Symptoms |
| Stroke | Facial asymmetry, noticeable when trying to smile, speech impairment, immobility of half the body, partial loss of visual fields. |
| Myocardial infarction | An attack of chest pain that lasts more than 15-20 minutes with cold sweat, redness of the upper half of the body, severe weakness, and fear of death. |
| Kidney infarction | Sharp pain in the lower back, increased blood pressure, blood in the urine, fever, nausea. |
| Intestinal infarction | Cramping pain, diarrhea, vomiting, and soreness may disappear, which is a bad sign, since it may mean a perforation of the intestinal wall. |
| Gangrene of the limbs | Pallor and then blackening of the skin, absence of pulse, skin sensitivity, wrinkling of tissues or their disintegration with a fetid odor. |
What is a blood clot? Symptoms, diagnosis, treatment and prevention of thrombosis
A thrombus is a blood clot in the lumen of a vessel or cavity of the heart, which, as a rule, forms at the site of its damage.
Once attached to the vessel wall, it not only impedes blood flow, leading to ischemia (reduced blood supply) in the area of occurrence.
Having broken off and moved with the bloodstream, a thrombus can cause a sudden blockage of a vessel located at a considerable distance from the site of formation.
Stopcock
Types and causes of blood clots
Blood clot formation, like a normal hematoma, is a natural physical response to injury. The blood thickens and forms a plug, which prevents bleeding. However, a blood clot inside an important vessel can cause serious problems - disruption of the blood supply to organs and tissues.
A thrombus, or a particle of it, called an embolus, can begin to move through the bloodstream and “settle” elsewhere in the circulatory system, interfering with normal blood supply. This condition is called thrombosis, and it is especially dangerous if a thrombus or embolus finds its “own” place in the heart, lungs or brain vessels.
Medicine classifies thrombosis depending on the type of vessels in which they develop:
- arterial thrombosis - the clot is localized in the arteries, including the heart
- venous thrombosis – a blood clot forms in the veins
In turn, each of these types of thrombosis is divided into several subtypes.
Causes
Blood clotting occurs through a chemical reaction between platelets and special proteins, which are called blood clotting factors.
A healthy body independently and effectively regulates the coagulation process in accordance with its needs.
However, under certain conditions, the blood becomes thicker and blood clots form faster. Here are some of them:
- smoking
- high cholesterol
- overweight, diabetes and sedentary lifestyle
- oncological diseases
- stress
- injuries
- dehydration
Some of these factors increase the risk of developing atherosclerosis, a condition in which cholesterol plaques deposit on the walls of blood vessels, blocking them, and increasing the likelihood of blood clots.
Symptoms
Angina pectoris
Physical reactions to a blood clot depend on its location. Initially, as long as the clot does not block or severely restrict blood flow, the person does not experience any significant discomfort or symptoms. However, over time, both arterial and venous thrombosis can lead to serious and life-threatening complications.
Symptoms of arterial thrombosis:
- unstable angina
- ischemia of peripheral arteries of the extremities
- heart attack
- ischemic stroke
These conditions require immediate medical attention and hospital treatment. In addition, emergency care is necessary for the following symptoms:
- chest pain and breathing problems
- paresis of the muscles of the lower part of the face
- sudden loss of strength and numbness in an upper or lower limb
- sudden coldness, paleness and pain in an arm or leg
Symptoms of venous thrombosis:
A particularly dangerous type of venous blockage is deep vein thrombosis, which is most often localized in the lower extremities. This condition causes the following symptoms:
- pain and swelling in the calf area
- heat and redness of the skin at the back of the leg below the knee
If any of these symptoms are present, a person should immediately consult a doctor. Deep vein thrombosis (DVT) is a potentially life-threatening condition. Moving through the bloodstream, emboli can block the pulmonary artery and lead to death.
Diagnostic methods
MRI
- Vascular duplex ultrasound
is the most common and accessible method for diagnosing DVT, in which, using ultrasound, the doctor determines the speed of blood flow in the veins and arteries, their lumen, geometry, the presence of blood clots and atherosclerotic plaques. - Blood test for D-dimer.
Allows you to evaluate and measure the level of fibrin, a substance that is formed as a result of the breakdown of blood clots. High levels may indicate the presence of DVT or another type of thrombosis. However, based on this indicator alone, an accurate diagnosis cannot be made.
- Angio and venography.
During this test, the doctor injects a special dye into the vein of the affected leg, which allows it to be seen under fluoroscopy and the speed of blood flow to be assessed. - MRI and CT
. Detailed scanning of tissues, organs and blood vessels. - VQ scan (Scintigraphy)
.Ventilation-perfusion scanning is a method for diagnosing pulmonary embolism in which the patient is injected intravenously with a protein labeled with a radioactive isotope. With its help, the doctor determines the location, shape and size of unventilated areas of the lungs.
In addition, the attending physician may refer the patient for additional tests to identify genetic bleeding disorders. This is necessary for difficult to explain recurrent thrombosis, especially in the liver or kidneys.
Treatment
Treatment of thrombosis is aimed at quickly and effectively achieving the following goals:
- relief of its symptoms and prevention of complications
- restoration of blood flow
- reduction and removal of blood clot
To achieve them, doctors use both surgical and conservative methods:
Elastic compression.
To improve blood flow in the lower extremities, patients with deep vein thrombosis are recommended to wear compression stockings, which help reduce pain and swelling, and also reduce the risk of complications. However, in severe forms of the disease and a significant decrease in pressure in the arteries of the legs, compression garments are contraindicated.
Exercises.
Along with special stockings, the doctor may advise people with DVT to take frequent walks during the day and, at night, to keep the lower leg of the affected leg above hip level.
Anticoagulants.
Anticoagulant therapy, if tolerated, is indicated in almost all patients with DVT. By influencing various blood clotting factors, drugs such as Warfarin reduce the risk of clot formation and its enlargement. If anticoagulants are intolerant or ineffective, the doctor begins to consider other treatment options.
Inferior vena cava filters (cava filters).
Vava filters are small mesh devices that the surgeon places in the inferior vena cava (large vein) under local anesthesia.
It traps emboli, preventing them from reaching the heart and lungs. The filter can be permanently in the vein and, along with anticoagulants, prevent serious complications.
However, it can be removed if the risk of thromboembolism and thrombosis is reduced.
Surgery.
Surgical interventions for the consequences of thrombosis are most often emergency and urgent care. They are aimed at unblocking the affected artery and restoring normal blood circulation.
Why a blood clot breaks off in a person, the main reasons
When a blood clot breaks away from the wall of a vessel, the cause is:
- its free location in the vessel (washed by blood on three sides);
- small attachment area;
- weak fixation in a place of increased blood flow (for example, a large vein of the lower extremities);
- addition of infection (purulent melting);
- increased body temperature (hot bath, sauna, fever);
- heavy lifting, sudden physical effort;
- straining with constipation;
- changes in blood pressure - hypertensive crisis, strong fluctuations;
- change of body position after a long period of bed rest.
Such factors are characteristic of the most common form of thrombosis – the veins of the lower extremities. In 10% of cases, a blood clot that has formed in the heart cavity breaks off. The provoking condition is an attack of severe coughing, as well as restoration of the heart rhythm after atrial fibrillation.
Types of formations
The simplest definition of what a thrombus is is a blood clot, which can be located both in the lumen of a blood vessel and in the cavity of the heart, and is formed as a result of blood coagulation in response to damage to the vessel. Blockage of blood vessels and blocking of blood flow is what makes such a clot dangerous.
There are two conditional classifications in which the division is based on different criteria. Depending on the location, the following types of clots can be distinguished:
- Venous/arterial/microcirculatory. These types of blood clots indicate where exactly it is located. In this case, we are usually talking not about a detached blood clot, but about thrombosis. Thrombosis is the primary site of clot formation, it constantly grows, and particles called emboli break off under the weight. A rather significant difference can be found between these types; for example, a venous clot cannot be formed from a plaque, since there are no plaques in the veins.
- Parietal. One of the segments is attached to the wall of the vessel, so the thrombus will not cause blockage of blood flow at the first stage, but it can become a “donor” of wandering clots. This layering can be of different sizes; sometimes there are quite long layers.
- Lining. Thrombosis occurs throughout the diameter of the vessel, leaving space in the middle for blood movement. This increases the pressure in the vessel, especially as the clot size increases.
- Central. It has fastenings to the walls on opposite sides. However, the main part is in the center, so the blood flows “around”. This position also greatly restricts blood flow.
Any of these forms of thrombosis can become a donor of a wandering embolus, which will move freely through the circulatory system. During this “journey,” it may increase in size or reach too narrow vessels. The final form of the wandering version, like all other types, is an occluding embolus. It completely blocks the movement of blood.
The second classification of blood clots is based on the composition:
- White. The medical name is agglutination. Its base is platelets and leukocytes, and there are many stages of thrombus formation, and they proceed slowly.
- Red blood clot. The medical name is coagulation; clotting factors and red blood cells are needed to form blood clots. Most often they are venous.
- Hyaline. The component is formed from plasma proteins to which red blood cells are attached, usually in the stage of hemolysis.
- Mixed. The pattern of thrombus formation requires the presence of different particles, some of them stick, others precipitate and themselves attach to the walls.
Several more classifications can be distinguished, but by location and composition they are the most comprehensive and important in diagnosis and treatment.
What will indicate a detached blood clot?
A blood clot can be tightly attached to the wall of the vessel, in which case it causes a gradual progression of circulatory disorders. The most dangerous variant of the development of the disease is the rupture of a blood clot and acute blockage of veins or arteries. Provoking factors are:
- intense physical stress;
- acute stress;
- acceleration of blood movement under the influence of high body temperature or the environment (overheating on the beach, in a sauna);
- infectious processes in the body;
- increased blood pressure;
- drinking alcohol.
Sudden vascular thrombosis is considered an acute condition requiring emergency medical care, since it can lead to death.
Blockage of the arteries of the extremities
The consequences of acute occlusion of blood vessels in the arms or legs are:
- numbness and stabbing sensations;
- loss of sensitivity to touch (paresthesia);
- decreased ability for active movements (paresis) or their complete impossibility (paralysis);
- absence of arterial pulsation;
- cold, pale, then bluish skin.
If blood flow is not restored in time, gangrene of the limb begins. The tissues die with the appearance of a typical black color due to the breakdown of hemoglobin. At first, there is a strong pain syndrome, as the nerve fibers are destroyed, the pain stops, and signs of intoxication increase. Treatment requires amputation of a limb or part thereof.
Watch the video about the first symptoms of varicose veins:
Venous thrombosis
Local symptoms are a feeling of fullness in the leg or arm, intense pain along the vein, increasing swelling, hot and red skin, overcrowded and tense vessels that appear above the skin level. The most dangerous condition with blood clots in the venous network is the migration of a blood clot into the pulmonary artery with the development of thromboembolism. Its occurrence is indicated by:
- acute and intense chest pain;
- shortness of breath, turning into an attack of suffocation;
- blue discoloration of the skin of the neck and face;
- a drop in blood pressure to the point of collapse or shock;
- palpitations, tachycardia.
Pulmonary artery thrombosis
Stroke
Acute blockage of a cerebral vessel leads to the cessation of nutrition of part of the brain tissue. This shows up:
- sudden weakness in the limbs followed by loss of movement and sensitivity;
- decreased clarity of speech, up to complete aphasia;
- severe headache, nausea, vomiting;
- disturbance of consciousness;
- distortion of the face, looking away to the side;
- hearing, vision, and swallowing disorders.
Acute blockage of a cerebral vessel leads to the cessation of nutrition of part of the brain tissue
Myocardial infarction
Thrombosis of the coronary vessels leads to a complete blockage of blood flow to part of the heart muscle. In a typical course, intense pain occurs in the heart or behind the sternum, spreading to the left shoulder, arm, back, lower half of the neck, and teeth. The nature of the pain is burning, sharp, pressing or squeezing.
The larger the area of myocardial destruction, the stronger the pain. The attack lasts from half an hour to a day, the use of nitrates is not removed, and is accompanied by agitation, severe weakness, rhythm disturbances, changes in blood pressure, shortness of breath and fear of death.
Intestinal infarction
The cessation of blood flow to part of the intestinal wall may be indicated by a significant deterioration in the patient’s condition:
- dry and pale skin;
- reduction of pain and its disappearance (the ghost of complete destruction of the intestines);
- bloating, but it remains soft for a long time (until the inflammation of the peritoneum increases);
- nausea, frequent vomiting.
As intestinal necrosis progresses, patients become apathetic, fall into a coma, and at this stage death occurs in most cases.
Watch the video about intestinal infarction:
Causes, symptoms, thrombophlebitis, prognosis
This serious disease can be caused by vein injuries, varicose veins, infectious, autoimmune processes in the body and developing atherosclerosis.
- The main signs of developing thrombophlebitis are heaviness in the muscles, swelling, and a bluish tint to the skin.
- In later stages, painful, bluish-purple, hardened venous nodes are visible, which can open and bleed, forming non-healing ulcers.
- It is important to know: the disease can lead to the death of the patient due to the detachment of a blood clot (thomboembolism), if the detached blood clot completely blocks the pulmonary artery or other important vessels.
- If left untreated, thrombophlebitis can cause limb loss, disability, and even death due to tissue necrosis.
- The development of blood clots in other parts of the body is also very dangerous.
A blood clot breaks off in the heart - instant death?
If a blood clot breaks loose in the heart, instant death does not occur in all cases. This will depend on the size of the clot and where it is moving. If a large clot was located in the right side of the heart, then the risk of an unfavorable outcome is high, since it enters the pulmonary artery system. When its major branch is blocked, death can be sudden.
If a blood clot is localized in the left half of the heart, its movements can lead to blockage of the arteries of the brain (stroke), heart (heart attack), kidneys, intestines, and lower extremities. In these cases, the severity of the condition and prognosis will be determined by the caliber of the blocked vessel and the timeliness of initiation of treatment.
Another difficult option is blocking the valve hole. It is caused by mobile blood clots, which, at the moment of ventricular contraction, fall between the valve leaflets. In this case, cardiac arrest is possible and immediate resuscitation measures are required.
Diagnosis of blood clots in leg veins
Before making a diagnosis and starting treatment for thrombosis, the doctor must conduct the necessary examinations.
Main actions and activities:
- Explaining to the patient what a blood clot is and why it can break off.
- Collecting anamnesis, including hereditary.
- Ultrasound with Dopplerography.
- Duplex angioscanning (one of the most informative methods).
- Rheovasography.
- CBC, biochemical analysis, OAM to identify additional pathological conditions.
Tests that allow you to diagnose the disease and find out whether there is an already formed blood clot:
- Lowenberg's sign - measurement using a blood pressure cuff. Blockage of a vessel causes pain when squeezed.
- They bandage the entire leg with an elastic bandage and ask the patient to walk around the room. After the procedure, pain in the legs and dilated saphenous veins appear.
- Pratt's test - the doctor places the patient on the couch and kneads the patient's lower limbs with massage movements. Then he applies a bandage and suggests moving around a little. A positive test result is pain in the calf muscles and swelling.
- A sign of thrombosis when flexing the foot is pale skin in the calves, pain.
- Test with a tourniquet - a compressive element is applied to the upper third of the thigh, with which the person walks for up to half an hour. If the test is positive, distension is felt in the lower extremities.
If necessary, consultation with narrow specialists is carried out.
What to do if a blood clot breaks loose
If a blood clot breaks loose, immediate hospitalization is required. This must be done when it is detected, especially a mobile, floating species. Prescribe complete rest and urgent treatment:
- installation of a trap - vena cava filter;
- suturing a vessel (vein);
- administration of drugs for resorption - enzymes (Streptokinase), low molecular weight heparins (Fraxiparin).
We recommend reading the article about thrombosis and thrombophlebitis. From it you will learn about the similarities and differences of pathologies, causes of development and risk factors, diagnostics and treatment methods. And here is more information about the prevention of thrombosis of the veins and vessels of the lower extremities.
The formation of a blood clot in blood vessels occurs with circulatory disorders, congestive processes, atherosclerosis, changes in the rheological properties of blood, and its clotting ability. In a chronic course, blood clots disrupt blood flow with the development of ischemic syndrome. Acute blockage when a blood clot breaks off leads to heart attacks and gangrene.
Venous thrombosis is accompanied by edema and congestion of the veins with expansion of the visible network of vessels and impaired outflow. A complication of blood clot movement from the extremities can be pulmonary embolism.