A decrease in circulating blood volume is called hypovolemia. It occurs with bleeding, burns, severe vomiting or diarrhea, dehydration due to diuretics or hormonal disorders. Manifested by a drop in blood pressure, increased heart rate, thirst, dizziness, and fainting. Severe hypovolemia causes shock, which can result in the death of the patient.
Hypovolemia as a condition
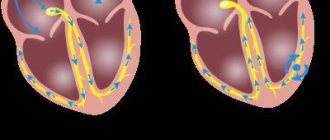
Normally, men have 70 ml of blood per 1 kg of body weight, and women have about 66. When its volume decreases, the filling of the ventricles of the heart decreases, the nutrition of internal organs deteriorates, and total oxygen starvation develops. In response to hypovolemia, blood enters the vascular bed from the reserve network (bones, liver, spleen). If this is not enough, then the vessels of the limbs and internal organs narrow to provide priority nutrition to the brain, heart and lungs.
Vascular spasm gives way to expansion, which leads to overflow of the veins and microvasculature
This is called centralization of blood circulation, it intensifies if fluid does not begin to enter the body. Vascular spasm gives way to expansion, which leads to congestion of the veins and microvasculature, severe oxygen deficiency for vital organs. Severe metabolic disorders and shock are a threat to life.
We recommend reading about the symptoms of hypomagnesemia. From the article you will learn about the role of magnesium in the body, the causes of hypomagnesemia, symptoms of deficiency, diagnostic methods and treatment of this pathology. Read more about drug treatment for stroke here.
Pathogenesis
Hypovolemia of any type leads to a compensatory hemodynamic reaction. The resulting deficiency of circulating blood volume causes a decrease in plasma volume and venous return, as the cardiac and pulmonary veins are fixed and sympathetically mediated vasoconstriction occurs. This protective mechanism allows you to maintain blood circulation for brain and cardiac activity.
Severe hypovolemia reduces cardiac output and thus reduces systemic blood pressure. This reduces blood supply to tissues and organs.
Blood pressure is normalized due to increased venous return, cardiac contractility and heart rate, as well as increased vascular resistance due to increased secretion of renin by the kidneys and the sympathetic effect.
With a mild degree of decrease in blood volume, activation of the sympathetic nervous system, accompanied by slight tachycardia, is sufficient to bring blood pressure back to normal.
In severe hypovolemia, vasoconstriction is more pronounced due to the influence of the hormone angiotensin II and the activity of the sympathetic nervous system. This hormone helps maintain blood pressure in a supine position, but when changing position, hypotension may appear (manifested by dizziness).
Sustained fluid loss during severe hypovolemia leads to severe hypotension even in a supine position. Shock may develop.
Causes of development in adults and children
The main factors that can lead to hypovolemia are:
- blood loss due to injury, surgery, fracture, gastrointestinal, pulmonary, renal, uterine (including during childbirth);
- loss of the liquid part (plasma) - extensive burn, intestinal obstruction, peritonitis, pancreatic necrosis, congestive heart failure with ascites or hydrothorax;
- excretion of fluid during vomiting and diarrhea is associated with poisoning, salmonellosis, gastroenteritis, cholera, staphylococcal infection;
- accumulation of blood in capillaries during traumatic shock, acute infections.
4.Treatment
Since different forms of hypervolemia have significantly different causes, there cannot be a single pattern of therapeutic response. In some cases, the first priority is to normalize the content and metabolism of sodium in the body, in other cases they begin with the examination and treatment of kidney diseases, etc. A separate important area is the prevention of severe complications from the cardiovascular system, pulmonary edema with rapidly progressing hypervolemia. Hypervolemia is especially dangerous for severe somatic patients who are in hospital and receiving transfusions, IVs, parenteral nutrition: data are published that hypervolemia in this case is one of the factors of intoxication and, ultimately, increased mortality.
The simplest, accessible to any person, widely known and effective way to avoid the development of hypervolemia (as well as many other problems) is to consciously limit the consumption of foods with a high sodium content: baked goods, fast food, salty dishes, etc.
Types and manifestations of the disease
Hypovolemia is not a uniform condition. It is divided into several types depending on the mechanism of development, the predominance of plasma or cell loss.
Normocythemic
The total volume of blood circulating in the vessels decreases, and the hematocrit remains normal or changes slightly. It happens with acute loss of blood, shock conditions, collapse with dilation of blood vessels and retention of blood in them (redistribution of blood flow occurs).
Polycythemic
The decrease in blood volume is mainly due to loss of plasma. Hematocrit is increased. The causes of this pathology are:
- frequent vomiting – poisoning, toxic infection, toxicosis of pregnant women;
- severe diarrhea - malabsorption in the intestines, infectious processes, deficiency of digestive enzymes;
- intense sweating in hot climates or work in production (hot workshop);
- increased urination – diabetes mellitus, renal failure, massive excretion of fluid with diuretics;
- burns on a large surface;
- reduced intake of water into the body - long-term dry food, quenching thirst with tea or coffee, pharyngeal spasm during tetanus or rabies.
One of the causes of pathology is burns
Oligocythemic
With this option, mainly blood cells are lost and the hematocrit decreases. It happens in the following pathological processes:
- massive destruction of red blood cells;
- suppression of cell formation during tumor processes;
- a condition after acute blood loss, when reserve fluid reserves from the intercellular space enter the vessels.
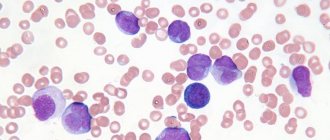
Massive destruction of red blood cells
Acute
Hypovolemia may develop suddenly. It is provoked by trauma, wounds, blood loss during surgical interventions, collapsed and shock conditions. In chronic processes, the decrease in blood volume increases gradually.
The danger of the acute form is that compensatory reactions do not have time to fully manifest themselves, which creates difficult conditions for the functioning of the brain, cardiac and pulmonary systems.
The prognosis is determined by the degree of fluid deficiency, but the condition worsens in elderly patients with concomitant diseases of vital organs.
Absolute and relative
True blood deficiency in the arterial and venous beds is absolute hypovolemia. This condition is always associated with loss of plasma, bleeding, or cessation of fluid intake into the body while the excretory function of the kidneys is preserved.
A relative insufficiency of circulating blood volume can occur against the background of normal or even increased fluid content in the body, but there is little of it in the vessels due to sweating into the tissue through the capillaries or with a sharp expansion of the vascular bed with the deposition of blood in it. Occurs in anaphylactic shock and poisoning .
Kinds
Depending on the ratio of BCC and the proportion of erythrocytes, leukocytes and platelets (Ht or hematocrit), normocythemic, oligocythemic and polycythemic hypovolemia are distinguished.
Normocythemic hypovolemia is a condition in which the hematocrit number in the total blood volume is within the normal range, but the total blood volume is reduced.
Oligocythemic hypovolemia is characterized by a decrease in blood volume and hematocrit.
In polycythemic hypovolemia, a decrease in BCC is associated primarily with a decrease in plasma volume and is accompanied by an increase in the hematocrit value.
Hypovolemia is also called a violation of the correspondence between the blood volume and the capacity of the bloodstream, which occurs when the capacity of this channel increases (relative hypovolemia).
Hypovolemia of the thyroid gland is a diagnosis that is made in cases when not only the fluid level in the body, but also the production of thyroid hormones is significantly reduced. Usually observed after prolonged blood loss.
Symptoms of hypovolemia
This pathological condition has various symptoms depending on the type and severity.
Oligocythemic
Due to a deficiency of red blood cells, oxygen transfer to tissues decreases, headaches, discomfort in the heart area, general weakness, severe dizziness, pale skin, and shortness of breath on exertion appear.
Polycythemic
Blood viscosity increases, which is accompanied by massive intravascular coagulation. Manifestations are caused by the underlying condition, as well as a rapidly progressing state of shock, a drop in blood pressure, impaired consciousness, respiratory decompensation up to pulmonary edema, and severe bleeding. The skin is pale with a marbled tint, the temperature is reduced.
Normocythemic
Symptoms depend on the degree of lack of circulating blood volume (CBV):
- From 10 to 20 percent. Mild form of hypovolemia. Hypotension, rapid pulse, shortness of breath, pale skin, cold extremities. When changing body position, dizziness and fainting occur.
- Moderate severity (BCC deficit 21-39%) – pressure drops to 90, tachycardia, breathing is frequent, shallow, irregular. The skin is covered with cold sweat, has a bluish tint in the area of the lips and nasolabial triangle, facial features become sharper, and pallor increases. Patients are lethargic, apathetic, yawning and drowsiness are noted due to oxygen deficiency.
- Over 40%, but up to 70 – severe hypovolemia. Pressure 60 mm Hg. Art. pulse is more than 120 beats per minute, extremely weak or undetectable, consciousness is confused or completely absent, urine stops being released, eyes become dull and sunken, breathing is rare, there are convulsions, coma.
Tachycardia
With greater loss of blood or fluid, compensatory mechanisms are ineffective, and death occurs.
Treatment
The main goal of treating hypovolemia is to restore normal circulating blood volume, increase cardiac output and improve oxygen transport to tissues and organs. Infusion-transfusion therapy will help achieve this effect. To carry it out, plasma replacement drugs (Dextran solution), fresh frozen plasma, protein (serum albumin) and crystalloid solutions (sodium chloride or Ringer's solution) are used.
In difficult cases, medications that normalize vascular regulation are used.
Transfusion of fresh frozen plasma is performed in exceptional cases: severe bleeding, hemophilia or thrombocytopenic purpura. This caution is due to the high risk of immunological incompatibility or infection with AIDS, hepatitis and other diseases.
Effective treatment of hypovolemia includes the use of plasma replacement drugs. They do not require defrosting and serological testing. Such medications are indispensable in providing first aid. However, the use of this therapy alone increases the risk of ischemia or hypoxia.
To correct the condition, drugs based on hydroxyethyl starch are used. They improve hemodynamics and blood circulation, normalize the transport of oxygen to organs, and reduce hematocrit and plasma viscosity.
In case of severe bleeding and the development of anemia, intravenous infusion of red blood cells and the use of Albumin are performed. For hypovolemia of the thyroid gland, hormonal drugs (TSH, T3 and T4) and medications with a high concentration of iodine are used.
To achieve stable remission, it is important to eliminate the causes of the pathology.
Possible complications without treatment
If the deficiency of blood or fluid in it is not restored in time, then signs of prolonged oxygen starvation of organs and tissues increase.
The initial compensatory vascular spasm turns into sustained paralysis of the vascular wall, and fluid is directed from the arterial and venous beds into the intercellular space, which further reduces the volume of blood volume. This condition means the onset of hypovolemic shock. When it occurs, the return of blood to the heart decreases, cardiac output decreases, and hypotension occurs.
Due to nutritional deficiency, insufficiency of the functions of all internal organs develops in the following sequence - skin, body muscles, kidneys, intestines, lungs, brain cells and myocardium . At this stage, emergency resuscitation measures are required; their effectiveness may be low.
Insufficiency of functions of all internal organs
Symptoms of the pathological process
The trigger for the appearance of external manifestations of hypovolemia is a sharp drop in the liquid part in the cells, which entails a decrease in the amount of plasma in the vessels and a drop in blood pressure. The force of the cardiac impulse increases, the load on the venous walls increases and their turgor decreases.
The main symptoms of dehydration are severe weakness, dry skin and mucous membranes, muscle cramps in the arms and legs, and the possible development of orthostatic collapse. All these manifestations are caused by an imbalance of electrolytes and changes in interstitial fluid exchange. Also common signs of this pathology include a decrease in body temperature, a weak pulse impulse, cyanosis of the skin and mucous membranes, and decreased urination.
Disturbances in water metabolism in the tissues of the abdominal and chest organs lead to severe pain in the abdomen and lungs, neurological disorders in the form of stupor and loss of consciousness. Problems of the cardiovascular system are also pronounced.
With massive fluid losses, a severe complication – hypovolemic shock – may develop. Its relief and further therapy requires the participation of resuscitators in the treatment.
Diagnosis of the condition
Signs of hypovolemia are easy to anticipate in case of visible blood loss, acute conditions, and restoration of blood volume is necessary for health reasons. Therefore, examination is often limited to a blood test, determination of hematocrit, pressure in the arteries and veins, and pulse rate.
There are situations when hypovolemia occurs with normal blood pressure and heart rate. This is possible with increased arterial tone and high peripheral vascular resistance. The danger of this form is ischemia of internal organs due to centralization of blood circulation.
To clarify the degree of violations, the transpulmonary hemodilution technique is used - installation of a catheter in the femoral artery with simultaneous catheterization of the subclavian vein, a cold solution is injected into it, and a temperature sensor in the artery records the time during which it will overcome the pulmonary circulation and appear in a diluted form in the vessel.
3.Symptoms
Classic signs of hypervolemia include excess body weight, a tendency to edema, persistently elevated blood pressure, dysuria (impaired urination), sweating or, conversely, dry skin. Patients complain of headaches, shortness of breath and difficulty breathing, general weakness, and fatigue.
The diagnosis is established clinically, confirmed and clarified laboratory: careful and reliable studies of the composition of blood and urine are necessary.
About our clinic Chistye Prudy metro station Medintercom page!
Treatment of hypovolemia
The most important condition for effective therapy is the rapid restoration of blood volume. To do this, one or two or even three veins are catheterized. For infusions, glucose and saline solutions (Ringer's, Hartmann's, Jonosteril, Sterofundin) are used until the pressure rises to at least 75 mm Hg. Art.
If such a result is not achieved, then switch to Refortan, Reopoliglyukin, Volutens. In addition to them, sympathomimetics are prescribed - Dopamine, Dobutamine, Norepinephrine, Mezaton.
Patients are prescribed oxygen therapy in the form of inhalation or mechanical ventilation in the absence of spontaneous breathing. Only after the blood volume has been restored, further examination and surgical intervention are carried out, and blood loss is corrected by transfusion of red blood cells, albumin, and fresh frozen plasma.
If the composition of electrolytes is disturbed, solutions of potassium and magnesium are used; calcium is used to a limited extent, only in cases of severe hypocalcemia.
The criteria for the effectiveness of therapy are:
- normalization of blood pressure (at least 90 units) and pulse below 95 beats per minute;
- warm skin of normal color, dry to the touch;
- restoration of oxygen concentration in the blood according to pulse oximetry;
- urine is excreted at a rate of more than 40 ml/hour.
Hypovolemia
- Kinds
- Causes
- Pathogenesis
- Symptoms
- Diagnostics
- Treatment
- Prevention
This condition is characterized by a change in the ratio of blood plasma and its formed elements. Hypovolemia is often a symptom of serious pathological processes and requires urgent medical intervention.
Depending on the ratio of BCC and the proportion of erythrocytes, leukocytes and platelets (Ht or hematocrit), normocythemic, oligocythemic and polycythemic hypovolemia are distinguished.
Normocythemic hypovolemia is a condition in which the hematocrit number in the total blood volume is within the normal range, but the total blood volume is reduced.
Oligocythemic hypovolemia is characterized by a decrease in blood volume and hematocrit.
In polycythemic hypovolemia, a decrease in BCC is associated primarily with a decrease in plasma volume and is accompanied by an increase in the hematocrit value.
Hypovolemia is also called a violation of the correspondence between the blood volume and the capacity of the bloodstream, which occurs when the capacity of this channel increases (relative hypovolemia).
Hypovolemia of the thyroid gland is a diagnosis that is made in cases when not only the fluid level in the body, but also the production of thyroid hormones is significantly reduced. Usually observed after prolonged blood loss.
The main causes of normocythemic type hypovolemia include:
- Blood loss. It can be controlled (during surgery) or uncontrolled. Accompanied by a compensatory reaction of the body.
- State of shock.
- Vasodilation collapse. It can occur with severe infection, intoxication, hyperthermia, improper use of certain medications (sympatholytics, calcium antagonists, etc.), histamine overdose, etc.
Hypovolemia of the oligocythaemic type is usually caused by:
- Loss of blood, which was observed before. It occurs at the stage when hypovolemia has not yet been eliminated due to the release of deposited blood into the bloodstream, and new blood cells have not yet arrived from the hematopoietic organs.
- Erythropenia with massive hemolysis of erythrocytes (observed in burn injury when the destruction of erythrocytes (hemolysis) is combined with the release of plasma from the bloodstream (plasmorrhagia)).
- Erythropoiesis observed in aplastic anemia and in aregenerative conditions.
The main cause of polycythaemic hypovolemia is dehydration.
Dehydration can be caused by:
- repeated vomiting (toxicosis during pregnancy, etc.);
- prolonged diarrhea of various etiologies;
- polyuria (for example, with uncompensated diabetes or primary hyperparathyroidism);
- increased sweat separation at elevated ambient temperatures;
- cholera;
- excessive use of diuretics;
- release of fluid into the third space with intestinal obstruction;
- peritonitis.
Hypovolemia of this type can also develop with muscle spasm (tetanus, rabies).
Excessive fluid loss can cause hypovolemic shock.
The reasons for the relative decrease in BCC are intense allergic reactions and intoxications of various origins.
Hypovolemia of any type leads to a compensatory hemodynamic reaction. The resulting deficiency of circulating blood volume causes a decrease in plasma volume and venous return, as the cardiac and pulmonary veins are fixed and sympathetically mediated vasoconstriction occurs. This protective mechanism allows you to maintain blood circulation for brain and cardiac activity.
Severe hypovolemia reduces cardiac output and thus reduces systemic blood pressure. This reduces blood supply to tissues and organs.
Blood pressure is normalized due to increased venous return, cardiac contractility and heart rate, as well as increased vascular resistance due to increased secretion of renin by the kidneys and the sympathetic effect.
With a mild degree of decrease in blood volume, activation of the sympathetic nervous system, accompanied by slight tachycardia, is sufficient to bring blood pressure back to normal.
In severe hypovolemia, vasoconstriction is more pronounced due to the influence of the hormone angiotensin II and the activity of the sympathetic nervous system. This hormone helps maintain blood pressure in a supine position, but when changing position, hypotension may appear (manifested by dizziness).
Sustained fluid loss during severe hypovolemia leads to severe hypotension even in a supine position. Shock may develop.
Hypovolemia is characterized by a decrease in blood pressure and an increase in cardiac output.
The symptoms of each type of hypovolemia depend on the nature of the cause that caused this condition.
With normocythemic hypovolemia, symptoms appear depending on the volume of blood lost:
- Mild hypovolemia is observed with an average degree of blood loss (from 11 to 20% of blood volume). In this case, there is a decrease in blood pressure by 10%, moderate tachycardia, slightly increased pulse and breathing. The skin becomes pale, the extremities become cold, there is dizziness, a feeling of weakness, dry mouth and nausea. Possible delayed reaction, fainting and sudden loss of strength.
- Hypovolemia of moderate severity is observed with a large degree of blood loss (from 21 to 40% of blood volume). Blood pressure drops to 90 mmHg. Art., pulse quickens, breathing is arrhythmic, shallow and rapid. The presence of cold sticky sweat, cyanotic nasolabial triangle and lips, pointed nose, progressive pallor, drowsiness and yawning are noted as a sign of lack of oxygen. There may be darkness of consciousness, apathy, increased thirst, possible vomiting, bluish discoloration of the skin and a decrease in the amount of urine.
- Severe hypovolemia is observed with massive blood loss (up to 70% of the blood volume). Blood pressure in this case does not exceed 60 mm Hg, the threadlike pulse reaches 150 beats/min, there is a sharp tachycardia, complete apathy, confusion or lack of consciousness, delirium and deathly pallor, anuria. The features become sharper, the eyes become dull and sunken, and convulsions are possible. Breathing becomes periodic (Cheyne-Stokes type).
With a loss of more than 70% of the blood volume, the compensation mechanisms do not have time to turn on - such blood loss is fraught with death.
In case of shock, breathing disturbances, a decrease in blood pressure and the volume of urine excreted, marbled skin coloring and cold sweat are observed, in the torpid phase - tachycardia and darkened consciousness, in the erectile phase - anxiety, but the presence of these symptoms depends on the stage of shock.
With oligocythemic hypovolemia, signs of hypoxia, a decrease in the oxygen capacity of the blood and impaired organ-tissue circulation are observed.
Symptoms of polycythaemic hypovolemia include:
- increased blood viscosity;
- disseminated microthrombosis;
- microcirculation disorders;
- symptoms of the pathology that caused this condition.
Diagnosis of hypovolemia is based on:
- studying anamnesis;
- physical research methods.
To confirm the diagnosis, laboratory methods are used (not informative in the presence of renal failure).
Treatment of hypovolemia consists of restoring blood volume, increasing cardiac output and ensuring the delivery of oxygen to the tissues of all organs. The dominant role is given to infusion-transfusion therapy, which allows you to quickly achieve the desired effect and prevent the development of hypovolemic shock.
In infusion-transfusion therapy the following are used:
- dextran solutions (plasma replacement drugs);
- fresh frozen plasma;
- serum albumin (a protein found in plasma);
- crystalloid solutions (saline sodium chloride solution, Ringer's solution).
The combination of these drugs does not always achieve the desired clinical effect.
In severe cases, medications are used to restore cardiac output and eliminate disturbances in vascular regulation.
Transfusion of fresh frozen plasma is carried out according to strict indications (for severe bleeding, hemophilia, thrombocytopenic purpura), since there is a risk of immunological incompatibility and the possibility of infection with viral hepatitis, AIDS, etc.
Plasma transfusion requires:
- pre-defrosting;
- carrying out isoserological tests;
- determining the patient's blood group.
Intravenous administration of plasma replacement solutions allows immediate therapy to begin, since the solutions do not require serological testing. Crystalloid solutions are useful in first aid.
The maximum effect is achieved by administering an amount exceeding the volume of lost blood three times, but the use of exclusively these solutions during therapy increases hypoxia and ischemia.
Correction of hypovolemia is also carried out with drugs based on hydroxyethyl starch. These drugs:
- normalize regional hemodynamics and microcirculation;
- improve the delivery and consumption of oxygen to tissues and organs, as well as the rheological properties of blood;
- reduce plasma viscosity and hematocrit;
- do not affect the hemostatic system.
Hypovolemia due to fluid loss is treated with electrolyte solutions and eliminating the cause of dehydration.
To eliminate hypovolemia of the thyroid gland, iodine and hormonal drugs are used.
Prevention of hypovolemia is important during surgery. Consists of:
- preoperative prophylaxis (additional infusion of colloid or crystalloid solution, preventing fluid loss at the initial stage of surgery);
- measuring any blood loss during surgical procedures;
- infusion therapy corresponding in volume to the amount of blood lost.
Source: https://liqmed.ru/disease/gipovolemiya/
Prevention measures
To prevent hypovolemia, timely diagnosis of the causes of its occurrence and rapid replenishment of the circulating blood deficiency are required. For diarrhea and vomiting, frequent and fractional drinking of plain water is necessary; if a decrease in pressure is noted, the patient requires infusion therapy.
When performing surgical interventions, preparation is required - the introduction of saline or plasma-substituting solutions. Immediately after surgery, it is necessary to determine the degree of blood loss and restore its deficiency using infusion therapy.
We recommend reading about cerebral hypoxia. From the article you will learn about the causes of cerebral hypoxia, acute and chronic forms, as well as methods for diagnosing and treating this pathology. And here is more information about the treatment of dyslipidemia.
A decrease in circulating blood volume is called hypovolemia. It occurs with a normal, increased, or decreased ratio of red blood cells to plasma. These conditions are characterized by progressive disruption of blood circulation and nutrition of internal organs, myocardium, lungs and brain. If solutions are not administered in a timely manner, hypovolemic shock develops with an unfavorable prognosis. Emergency intravenous infusion therapy is indicated for treatment.
Hypovolemic hypotension. Treatment of hypovolemic hypotension
Source: https://meduniver.com/Medical/cardiologia/311.html
| Hypovolemic hypotension often occurs at the prehospital stage of MI in elderly patients who have previously received long-term diuretics, large doses of nitrates, as well as against the background of increased sweating, vomiting, diarrhea and insufficient fluid intake. Hypovolemia contributes to inadequate LV filling, and subsequently to a decrease in stroke volume. Excessive hypovolemia (as one of the reasons) can lead to hypotension. Hypotension associated with bradycardia and often reflects excessive vagotonia. Hypotension is often determined against the background of a normal or accelerated heart rate, especially in patients who previously (even before the development of MI) received diuretics. Concomitant hypovolemia (relative or absolute) is also often noted. Relative hypovolemia may develop (even with normal vascular tone) due to a decrease in ventricular elasticity during MI. Therefore, increasing LV filling pressure (more than 20 mmHg) may be necessary to ensure optimal preload. If the patient is suspected of hypovolemia , then a small amount of liquid (50 ml of isotonic NaCl solution) is administered intravenously. If the cause is hypovolemia, then SVR quickly increases. Clinical symptoms of hypovolemia : absence of venous stagnation in the lungs, orthopnea and collapse of the saphenous veins. |
Causes
Partially the issue has already been addressed. What factors directly provoke the disorder:
Heavy bleeding
In the context of the situation, it does not matter whether it is external or internal. The point is that the amount of blood falls physically
This is fraught with the rapid development of hypoxia and ischemia of the whole organism. The condition is extremely dangerous. Therapy is carried out in a hospital. Treatment is selected according to the situation. As a rule, a combination of blood transfusion and symptomatic correction is used. Vomit. Strong, indomitable. When a person loses a lot of fluid along with waste masses. This situation is quite rare in clinical practice. Severe infectious processes can be considered typical provocateurs. For example, cholera. Also acute critical poisoning.
This occurs a little less frequently with toxicosis. But this is a clear indicator of an abnormal pregnancy. Usually vomiting is much milder and not as dangerous.
In the blade, you need to restore the volume of fluid in the body (drip solutions are used), and also eliminate the urge. For this, classic antiemetics are used, for example, Cerucal.
Polyuria. Excessive urination. This is not an independent disease, but a syndrome. That is, a complex of manifestations typical of any deviation. Particularly common in diabetes insipidus. The amount of urine can reach tens of liters. Without constant fluid replenishment, death cannot be avoided.
The situation with kidney diseases is a little simpler. But not always. Depending on the severity of the disorder, critical complications are possible.
With diabetes, the amount of urine can reach 5-6 liters and this is not the limit. All of these conditions are dangerous. It is necessary to treat them, and not the polyuria itself. There is little point in symptomatic correction.
Shock. Generalized name of the syndrome. Characterized by a drop in blood pressure, collapse, and possibly a coma. The body is not able to cope with the intense factor. Usually internal. Be it a severe injury, a pronounced response of the immune system (severe allergies) and others.
The blood concentration remains normal, but the number of formed cells is seriously affected. This is an additional risk factor.
Treatment takes place in the intensive care unit. After eliminating the abnormal condition, it is possible to return the patient to normal. Although they look after him for some time and only then discharge him.
- Severe diarrhea. Against the background of intestinal infections or, less commonly, intoxication. This condition is especially dangerous if a person cannot quickly receive competent help. The cause of the diarrhea must be eliminated. Internal antiseptics and antibiotics are used as needed. A special diet is also indicated. Then they act according to the circumstances. As a rule, with timely correction it is possible to avoid lethal and simply severe consequences.
- Dying of red blood cells. Hemolysis. It occurs for a variety of reasons. From some forms of streptococcal infection to congenital anomalies in the hematopoietic system. They influence the main factor provoking the problem.
- Use of certain medications. Especially often - diuretics. You can familiarize yourself with the possible complications and side effects in the annotation.
To eliminate the condition, simply stop taking the drug. Although in some cases this is not so easy to do. It makes sense to reconsider the treatment regimen. Under the supervision of a medical specialist. You cannot voluntarily abandon the course. Especially if there is a reason to take the medicine.
This is not a complete list. It reflects only a certain part of the possible diagnoses. Although just these conditions are found in the majority of cases.