The resulting circulatory deficiency in the human brain can lead to circulatory hypoxia, as a result of which an insufficient amount of glucose will reach the brain cells. The condition resulting from this process is called cerebral ischemia.
Brain tissue is very sensitive to disruptions in blood supply; daily it requires consumption of 25% oxygen and 70% glucose. By newborn children, the volume of oxygen consumption by the brain increases to 50%.
If specialists diagnose a newborn child with a disease such as cerebral ischemia, then later he may develop health problems such as:
- Delayed development and intellectual activity.
- Dysarthria.
- Visual impairment.
- Hyperactivity syndrome.
- Epilepsy.
- Hydrocephalus.
Ischemia is essentially the initial start for neurosomatic abnormalities that manifest themselves in subsequent age-related life periods.
What are the degrees of development?
The disease is dangerous because of its imperceptible onset, which can develop over years, turning into a chronic specific form of cerebrovascular pathological picture.
Processes that cause destruction to the neurons of brain tissue progress. In turn, this leads to a reduction in the flow of blood in the arteries to the parts of the brain.
Prolonged vasoconstriction leads to focal lesions and contributes to the development of microinfarctions.
There are three degrees of the disease:
- 1st degree. Initial, accompanied by headaches, some memory loss, confusion of life events and dates, sleep disturbances, weakness, rapid fatigue, emotional instability;
- 2nd degree. It is characterized by increasing symptoms that noticeably change the personal qualities of the patient, including apathy, depression, and a decrease in former desires and interests; neurological syndromes gradually come to the fore;
- 3rd degree. Neurological disorders are clearly expressed, multiple cortical infarctions develop with the subsequent formation of vascular dementia.
The disease is dangerous because of its imperceptible onset, which can develop over years, turning into a chronic specific form of cerebrovascular pathological picture.
Symptoms and signs
Symptoms depend on how extensive the damage to the central neurons of the baby’s brain has become. The more severe the oxygen starvation, the longer it lasted, the more nerve cells die. The earliest symptoms are observed immediately after birth: the child does not cry within the time limits allotted for this in obstetrics, or his cry is too weak. Children with ischemia most often have an Apgar score below 7/7.
On the very first day, doctors may suspect cerebral ischemia due to increased hypertonicity of the baby’s large muscle groups, convulsions, tremors, or prolonged prolonged crying of the newborn, even if there are no objective reasons for crying. Too lethargic, apathetic newborns who suck poorly and sleep a lot will also cause reasonable suspicion.
Symptoms of ischemia depend on the degree. Grade 1 is characterized by minor deviations in the child’s behavior and condition. In the first days of life, it manifests itself either as excessive depression of the nervous system or its increased excitation. Typically, such mild ischemia resolves within a week.
If pathological abnormalities are noticeable even after the first seven days of the baby’s life, they speak of grade 2 ischemia. With it, convulsions and strabismus are added to minor neurological manifestations (crying, sleep disturbances, excessive regurgitation). With timely medical care, it can be dealt with.
The third degree of ischemia usually manifests itself as coma. The baby is unconscious, he has no swallowing and sucking reflexes, or muscle tone. Many children cannot breathe on their own without the use of a ventilator. If a baby can be saved under intensive care conditions, then the brain lesions are most often large-scale and can manifest themselves both in impairments of individual functions (hearing or vision) and in systemic lesions - paralysis, paresis, cerebral palsy, dementia.
Infantile stroke - cerebral hemorrhage due to acute cerebral ischemia - mainly develops in premature infants. In babies born at term, the probability of such a complication is only 10%, while in children weighing less than 2 kilograms, a stroke or microstroke (transient ischemic attack) develops in 35% of cases, and in very premature children weighing less than a kilogram, a stroke occurs in 95% of cases. cases.
Symptoms of ischemic stroke are also based on neurological manifestations and are in many ways similar to the symptoms described above.
General information
What CCI is is quite simple to determine, but coping with the disease and identifying its causes is not so easy. Ischemic disease develops when there is insufficient blood supply to the brain (BM), which is provoked by various pathological processes in the body. In the acute form of ischemia, tissue necrosis occurs instantly and causes a stroke.
Chronic cerebral ischemia is cerebrovascular insufficiency caused by a progressive deterioration of blood supply to brain tissue
The term “chronic cerebral ischemia” suggests the parallel development of diseases:
- encephalopathy (dyscirculatory, vascular or atherosclerotic);
- cerebrovascular insufficiency;
- vascular parkinsonism;
- vascular epilepsy;
- vascular dementia.
Brain disease requires immediate treatment, since dying organ cells cannot be restored, and if there is no effect on the pathological process, the patient faces disability and, in the most severe cases, death.
How does the treatment work?
It should be understood that it is impossible to completely restore damaged brain structures. Modern medicine can only stop the progression of pathology and help the brain partially compensate for impaired functions.
Treatment in the acute period is aimed at maintaining the vital functions of the body and depends on the stage of the disease:
- Ventilation In severe cases, independent breathing is impossible or significantly difficult.
- Treatment of seizures. They lead to an increase in the area of seizure activity in the brain, damaging previously untouched areas. Various anticonvulsants are used as therapy
- For severe spasms, muscle relaxants may be prescribed.
- Diuretics if there are signs of cerebral edema.
- Surgical treatment of hydrocephalus.
- Treatment of cardiovascular system disorders. Arrhythmias, pressure surges, low cardiac output aggravate the child's condition.
- Treatment of complications that develop in the acute period: pneumonia, bedsores.
Nootropics, neuroprotectors and drugs that improve cerebral circulation are used in combination and over long courses.
After stabilization of the condition, the next recovery period begins, which sometimes lasts a lifetime.
It includes:
- Massage. For mild ischemia, the mother performs a relaxing massage on her own. In stages 2 and 3, massage is performed only by a specialist or under his supervision.
- Exercise therapy. An essential component of effective rehabilitation. Physical education is aimed at stimulating blood supply to the brain, developing paralytic limbs, and also at adapting the child to social life.
- Physiotherapy. The use of special devices, such as rollers, splints, to maintain spastic limbs in a physiological position.
- Classes with a speech therapist, various methods of psychological therapy and social adaptation.
For adults, treatment is aimed at eliminating the cause:
Neuroprotection This may include taking statins, antiplatelet agents, strict control of sugar and blood pressure. The use of surgical treatment methods (stenting, bypass surgery, thrombectomy, etc.), if it is possible to restore adequate blood supply to the brain. Special attention should be paid to psychological assistance for older people
Older people experience their own inadequacy and dependence on others very hard. Therefore, it is important for relatives to pay attention to changes in the behavior and character of a loved one in time for timely diagnosis.
Symptoms of the initial stage of chronic cerebral ischemia
The chronic form is formed from the acute one and has degrees of its development. The most progressive of them is degree 2, characterized by special symptoms:
- increased headaches, feeling of heaviness in the head;
- approaching nausea;
- general malaise;
- slow speech;
- unsteady gait, loss of balance when walking;
- irritation and aggression, isolation and unpredictability;
- decision to change your usual lifestyle;
- loss of interest in life situations, in society;
- decreased appetite, weight loss.
In the chronic form of cerebral ischemia, transformations begin in the white matter with the subsequent formation of microfoci, increasing compression of microcapillaries, and destructive processes in the cortical and stem connections of neurons.
Chronic cerebrovascular disorders of the brain cause changes in white matter with the development of foci of demyelination and damage to oligo- and astrodendroglia with progressive compression of microcapillaries with disruption of cortical-stem and corticostriatal connections of neurons. Chronic cerebral ischemia manifests itself in the form of subjective and subjective symptoms.
The main symptoms of chronic ischemic brain lesions characterize the clinical degrees of chronic cerebral ischemia, on which timely diagnosis and treatment of the pathological process depends.
Chronic cerebral ischemia is clinically manifested by headaches, heaviness in the head, dizziness, a progressive decrease in attention and memory, sleep disturbances, the development of emotional lability and coordination disorders (unsteady gait and unsteadiness when walking). As the blood supply to neurons deteriorates due to the progression of stenosis and spasm of the cerebral arteries, ischemia worsens and foci of infarction of various locations develop with the addition of focal symptoms depending on the degree of cerebrovascular disorders.
In the initial (I stage) cerebrovascular insufficiency, patients complain of constant headaches, heaviness and noise in the head, dizziness, various types of sleep disturbances, increased weakness and fatigue, decreased memory and attention, emotional lability, irritability and impaired coordination of movements.
The neurological status is determined by minimal organic symptoms, which are manifested by the revival of deep reflexes with their slight asymmetry, the presence of convergence disorders, subcortical reflexes and the presence of moderate cognitive disorders in the form of decreased cognitive activity, impaired attention, decreased memory for current events.
Signs of CCI have features of manifestation depending on the stage of the lesion. Unlike many other pathologies that occur in the body, ischemic cerebral disease in chronic form is characterized by a decrease in patient complaints as the disease progresses, and not vice versa. In this case, deviations in the patient’s condition are present, but he himself cannot adequately assess them.
Chronic cerebral ischemia stage 2: treatment, symptoms and disability
DEP is an abbreviation that stands for discirculatory encephalopathy, that is, disturbances in the functioning of the brain caused by impaired blood supply.
It is divided into three degrees depending on the severity of the lesion:
- In the first degree, most symptoms are subjective - fatigue, decreased mental performance.
- The second degree is obvious disorders of thinking and memory, as well as neurological symptoms.
- The most severe, third degree , is dementia with obvious neurological disorders.
The danger of DEP is that the disease slowly but inevitably impairs a person's ability to think clearly and can lead to disability.
We also bring to your attention an article about dyscirculatory, post-traumatic and residual encephalopathy.
What is alcoholic encephalopathy
As a result of the disease, disorders of the autonomic, somatic, nervous and other systems of the human body are observed.
Encephalopathy has the most unfavorable effect on metabolic processes, which leads to deterioration in physical health.
The disease worsens in spring and summer, accompanied by paranoia and obsessive delusions, since brain cells die due to alcohol abuse. This is a whole complex of diseases that occur simultaneously in chronic or acute form.
Symptoms of alcoholic encephalopathy
Symptoms of alcoholic encephalopathy appear one at a time or all at once. They look like this:
Chronic encephalopathy
Chronic encephalopathy in patients is expressed in different ways. With a neurological status, muscle hypotonia, decreased vision, moderate hyperreflexia, and signs of autonomic dysfunction are possible.
If the chronic form of the disease progresses, it is accompanied by a worsening of symptoms, in which neurological syndromes are formed: pseudobulbar, hyperkinetic, parkinsonian, vestibulo-atactic.
Acute toxic encephalopathy
Without medical assistance, such conditions can lead to disruption of cerebral centers and circulatory disorders. The degree of destruction depends on the duration of alcohol intoxication and associated health problems. Acute toxic encephalopathy of the brain, if left untreated, does not go away without leaving a trace and often leads to death.
Causes of alcoholic encephalopathy
The disease can develop without alcoholism. Sometimes, due to individual characteristics, against the background of rare alcoholic excesses or taking small doses of alcoholic beverages, a person can also receive a diagnosis of alcoholic encephalopolyneuropathy. In this case, the cause of the disease lies in metabolic disorders, a lack of vitamin B1 in the body, which is caused by a monotonous diet.
Diagnostics
- find out what kind of alcoholic drinks the patient drinks;
- determine the time of onset of symptoms;
- conduct a visual inspection;
- collect information on the amount of alcohol taken now and in the early stages.
Treatment of alcoholic encephalopathy
- reduction of intoxication in a hospital setting with the help of vitamins B, C, nicotinic acid, which are administered using intramuscular injections (injections into the muscle);
- to improve cerebral circulation and the supply of nutrients to the brain, vasodilator drugs Hydralazine, Apressin are prescribed;
- for seizures, anticonvulsant drugs Amizepine, Tegretol are prescribed;
- The doctor must get the patient to completely abstain from alcohol, otherwise drug treatment will be ineffective.
Consequences of toxic encephalopathy of the brain
- stroke;
- weakening of mental abilities;
- schizophrenia;
- severe stun;
- a brain tumor;
- coma;
- death.
Prevention
Prevention of alcoholic encephalopathy should include avoidance or minimal doses of alcohol-containing drinks, especially for young girls.
The female body is more susceptible to the influence of alcohol due to genetic inability.
The fight against alcoholism among adolescents, women and men should be carried out at the state level, through a set of social, legal, economic, medical and administrative measures.
What is a differential diagnosis?
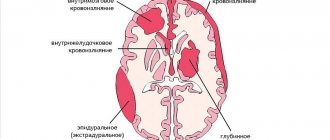
In case of acute onset, development of general brain symptoms, determination of high blood pressure values, differential diagnosis between cerebral hemorrhage and embolic stroke is necessary for an accurate diagnosis.
In the acute period, differential diagnosis between ischemic stroke and head injuries, as well as CT scanning and radiography of the skull, are important.
Direct and differential diagnosis involves consideration of similarities with encephalitis, usually indicating that the lesions are not vascular.
It is important to differentiate ischemia from encephalitis caused by herpes simplex.
A differential diagnosis is made between subdural hematoma and ordinary thrombotic stroke. A history of trauma, as well as the presence of anisocoria - mydriasis on the side of the hematoma, speaks in favor of a subdural hematoma.
Differentiation between ischemic stroke and tumor is particularly important. For this purpose, photographs are taken with the introduction of contrast. Examination of the cerebrospinal fluid can sometimes facilitate an accurate diagnosis.
Brain tumor
The differential diagnosis includes cerebral abscess, where CT is combined with contrast injection. The diagnosis of ischemic stroke is based on medical history, neurological status, and investigations. Modern clinical examination includes the establishment of classical neurological status.
At this stage, the first necessary examination is a CT scan. It is performed early to exclude other brain diseases (cerebral hemorrhages, tumors) and to identify early signs of ischemia (cerebral edema, thrombosis of certain vessels, etc.).
A late CT scan of the head, usually after 24 hours, covers an area around which an increased area of blood flow can be visualized.
Later scans may reveal areas of hemorrhagic hemorrhage - most often as a consequence of embolic stroke, poor blood pressure control and early introduction of coumarin anticoagulants.
Magnetic resonance imaging detects cerebral ischemia in the first 24 hours and is considered significantly more sensitive than CT in examining the posterior fossa.
If imaging is not possible, a lumbar puncture is performed to rule out other diseases, and most cases of ischemic stroke reveal a normal result. Lumbar puncture is preceded by an ophthalmological consultation.
Doppler sonography reveals abnormalities of large and small cerebral arteries, its results are important for the possibility of stent placement, endarterectomy, the inclusion of anticoagulant and antiplatelet therapy, and to determine the patient's prognosis.
Source: //neuro-orto.ru/bolezni/encefalopatiya/ostd-2-stepeni.html
Reasons for this condition
When this process is disrupted, a disease appears - cerebral ischemia. There are major factors contributing to the disease and secondary ones. The main factors include:
- diabetes;
- heart diseases;
- thrombosis leading to blockage of brain vessels;
- osteocondritis of the spine;
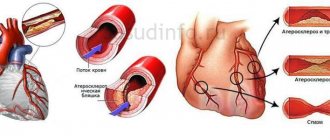
- vascular atherosclerosis;
- amyloidosis of the circulatory system and other organs;
- violation of the correct lifestyle;
- alcohol and smoking abuse;
- maintaining an unbalanced diet;
- age over 50 years.
Congestive heart failure
Having studied Elena Malysheva’s methods in the treatment of HEART DISEASE, as well as restoration and cleansing of VESSELS, we decided to offer it to your attention.
Today, the progression of chronic cerebral ischemia occurs:
- with anomalies in the development of vessels in the systemic circulation (carotid arteries, aorta) and cerebral arteries, which are asymptomatic and progress with pronounced spastic and atherosclerotic changes in the vascular bed;
- with pathological processes in the venous system (thrombophlebitis and thrombosis of various localizations);
- for inflammatory and destructive diseases of the spine that cause disruption of blood flow in the vertebral arteries (osteochondrosis, spondyloarthrosis, disc herniation);
- with amyloidosis of blood vessels and internal organs;
- for collagenosis, vasculitis and other blood diseases.
The stage of decompensation (stage III) of chronic cerebral ischemia is characterized by a combination of progressive syndromes in the form of pseudobulbar disorders, extrapyramidal and pyramidal insufficiency with the addition of amyostatic syndrome, which is characterized by hypomimia, muscle rigidity (the phenomenon of “counteraction” in the lower extremities) and difficulty initiating movements.
Cognitive disorders are manifested by a decrease in criticism, the development of subcortical-cortical or subcortical dementia with the presence of paroxysmal conditions in the form of fainting, falls and epileptic seizures. Emotional and personality disorders are expressed by disinhibition and apathetic-abulic syndrome. These patients are disabled with impaired everyday and social adaptation, losing the ability to self-care.
Among the main etiological factors, atherosclerosis and arterial hypertension are considered; a combination of these two conditions is often identified
Provoking factors include:
- traumatic brain injuries;
- congenital anomalies of the brain;
- aneurysms;
- heart failure and others.
All of the above reasons are usually associated with damage to the cerebral vessels. However, cerebrovascular accident can also be caused by damage to the arteries. Provoking processes include:
- change in the direction of the carotid or vertebral artery;
- abnormal structure of blood vessels;
- compressed vertebral artery due to spondyloarthrosis or osteochondrosis;
- insufficient collateral blood supply;
- coronary-cerebral syndrome in ischemic heart disease;
- blood pressure surges;
- abnormalities in the hemodynamics of the brain.
Anomalies of the vessels of the brain, neck, shoulder girdle, and aorta are also important.
In rare cases, ischemia of mixed origin of the brain is observed. It is caused by several pathological processes: liver disease, alcohol addiction or trauma to the skull.
- blood diseases;
- cardiovascular failure;
Congestive heart failure
- atrial fibrillation;
- anemia;
- injury.
Disability for hypertension: is a group given for grade 3 hypertension?
It is possible to get disability with grade 3 hypertension, risk 4.
The fourth risk is characterized by a probability of complications above 30%; heart attacks and strokes often develop, leading to irreversible organ damage and death. To obtain a group, they undergo a medical and social examination (MSE). Its results are taken into account with other criteria - the stage of hypertension, the presence of complications and their severity, the frequency of hypertensive crises. Additionally, an assessment of a person’s work activity is given.
To conduct an examination, the patient needs a referral to the place of observation or from social protection authorities (in the absence of registration). The examination is carried out where the referral is submitted. If the patient cannot come on his own, then in a hospital or at home.
It is possible to receive disability in absentia. But this process will take a lot of time and a larger list of documents will be needed. A verdict on appropriation is made only if there is a special commission.
Where can I get a group for stage 3 hypertension?
Chronically high DM and DD lead to damage to internal organs.
The heart and blood vessels are mainly affected. Arterial hypertension “requires” special working conditions, which are necessarily created for the employee. Hypertension is said to be in cases where the systolic value is equal to or higher than 140 mm, and the diastolic value is 90 mm inclusive or higher.
After confirming the diagnosis, the patient is prescribed to take medications with an antihypertensive effect, and special working conditions are recommended to prevent the development of a hypertensive attack.
In case of hypertension of the 1st degree, the target organs are practically not susceptible to negative influence, therefore it is inappropriate to talk about recognition as a disabled person.
Is disability given for grade 3 hypertension at risk 4? The answer is a clear yes. Since the pathology is characterized by the following:
- The patient is incapacitated.
- Blood pressure is constantly above 180/110 mmHg.
- A decrease in arterial values leads to severe heart failure.
- The risk of target organ damage is over 30%.
Hypertension, even in its early stages, is a dangerous disease. Accordingly, hypertensive patients need favorable working conditions. The following activities are strictly prohibited:
- Work associated with excessive physical, mental and emotional stress; proceeding at a given technological pace or rhythm.
- Work in conditions with intense noise, vibration, and high indoor temperatures is contraindicated.
- It is strictly forbidden to work at night.
- Hypertensive patients should not work at heights or in extreme conditions.
- It is not recommended to choose an activity that could lead to an emergency in the event of a hypertensive attack - driving, etc.
Is it possible to give disability for 2nd degree hypertension? The commission's decision depends on the risk of chronic pathology. For example, with 1 or 2 risks, receiving is practically impossible. But against the background of 3 or even 4 risks, the verdict is positive in 99% of clinical pictures.
If stage 2 hypertension is accompanied by diabetes mellitus, severe damage to blood vessels and internal organs, then the group must be assigned.
Only specialists working in the ITU bureau decide which disability group the patient is assigned to. They receive it only after a thorough and comprehensive check.
What does a hypertensive patient need to register for disability?
To establish incapacity for work, it is necessary to conduct a medical and social examination. To do this, the patient writes a statement addressed to the head of the medical institution where he is being observed. You should also get a referral from your local clinic.
The document must contain information about your current health status. Data are indicated showing the degree of disorder of specific organs and internal systems. Treatment regimens and results achieved are prescribed.
The examination is carried out in the institution where the application was submitted. In a situation where the patient cannot move independently due to illness or age, doctors come to the home or the person is hospitalized.
To obtain disability, a number of diagnostic measures are prescribed. Let's look at the required research:
- A clinical blood test determines the hemoglobin concentration and the number of red blood cells.
- Biochemical research. Determine cholesterol content; the degree of predisposition to atherosclerotic changes in the body.
- A glucose test shows the presence of diabetes mellitus.
- A urinalysis provides information about kidney function.
- The Nechiporenko test and the Zemnitsky study study the function of the kidneys.
- An electrocardiogram can detect angina pectoris, signs of coronary heart disease (CHD), left ventricular hypertrophy and other pathologies.
- Echocardiography determines the condition of the valves in the heart.
According to indications, additional studies are prescribed that are not included in the standard diagnostic list.
For example, if hypertensive angiopathy is suspected, a full examination by an ophthalmologist is required. The referral must include the conclusion of all doctors - a surgeon, cardiologist, therapist, endocrinologist, neurologist, etc. The decision is made by a commission. Disability is granted for a period of 12 months. Then re-examination is carried out annually. In the first group, re-examination is carried out after two years.
There are certain conditions that qualify for permanent disability. That is, if a person is prohibited from any activity, repeated confirmations are no longer needed:
- Women over 55 years of age.
- Retired men over 60 years of age.
- Persons with disabilities who have a history of irreversible anatomical defects.
When a person is declared disabled for several years in a row, the examination may issue an order to recognize him as disabled for life, which excludes annual re-examination.
What groups are prescribed for hypertensive patients?
To assign a group to a patient, doctors study the medical history.
Many circumstances are taken into account - the frequency of visits to a medical institution, the stage and degree of chronic pathology, and examination results. Be sure to take into account the frequency and severity of hypertensive crises; concomitant diseases, their severity and rate of progression; features of the working conditions of each specific patient.
The third point is not particularly important. When a patient is declared completely incapacitated, he is removed from work. He should be entitled to a monthly allowance in accordance with the laws of his place of residence and registration.
Reviews show that disability group for hypertension degree 3, risk 4 is always given. However, to obtain it you have to “run around”, since you need to undergo many examinations and collect a large list of documents.
Criteria determining the disability group:
- The first is given in cases where hypertension is accompanied by severe symptoms, drug therapy does not help reduce blood pressure monitor readings. Heart failure has been detected and there is a high risk of death from a heart attack. The functionality of target organs is impaired. Any work is contraindicated for the patient.
- The second for hypertension is given to persons with a malignant course. The functioning of the kidneys, brain and other internal organs is moderately impaired in patients; A mild form of heart failure was detected. A person may be declared completely or partially disabled. Most often the first option.
- The third is assigned against the background of second degree hypertension. Considering the fact that the disease occurs with a slight disorder of the internal organs, the patient is considered partially able to work. Special working conditions are required, work in hazardous and noisy industries is excluded, etc.
To qualify for total or partial disability, you should contact your doctor. He will give the necessary recommendations and issue a referral for examination. Statistics say that more than 90% of hypertensive patients who have passed a medical and social examination receive group 2 or 3.
The best modern remedy for hypertension and high blood pressure. 100% guarantee of pressure control and excellent prevention!
TO THE DOCTOR
how can I call you?:
Email (not published)
Subject of the question:
Question:
Last questions for specialists:
- Do IVs help with hypertension?
- If you take Eleutherococcus, does it lower or increase your blood pressure?
- Is it possible to treat hypertension with fasting?
- How much pressure should be reduced in a person?
Pathological picture
The subcompensatory degree is characterized by a rapid increase in pathological symptoms and the appearance of cognitive impairment. Occurs 3-5 days from the onset of the acute form or after a month. Active mental processes slow down. You lose control over your appearance, your attitude towards hygiene processes, and sloppiness appears.
Planning of affairs at work and in solving family problems becomes disrupted and becomes unimportant. Interest in the affairs and mood of loved ones disappears. The sick person is often capricious and does not accurately perform small actions with his hands.
A symptom of parkinsonism appears, in the form of trembling hands, small uncertain steps, trembling of the head, and slow speech. Self-service continues. The quality of professional activity is deteriorating.
Planning of affairs at work and in solving family problems becomes disrupted and becomes unimportant. Interest in the affairs and mood of loved ones disappears. The sick person is often capricious and does not accurately perform small actions with his hands.
For the treatment of cardiovascular diseases, Elena Malysheva recommends a new method based on Monastic tea.
It contains 8 useful medicinal plants that are extremely effective in the treatment and prevention of arrhythmia, heart failure, atherosclerosis, ischemic heart disease, myocardial infarction, and many other diseases. Only natural ingredients are used, no chemicals or hormones!
Stages of cerebral ischemia
The stages of cerebrovascular insufficiency are determined by clinical manifestations and the presence of objective neurological symptoms.
There are three degrees of chronic cerebral ischemia:
- the initial stage with the presence of the main symptoms in the form of headaches, memory loss, dizziness with moderate sleep disturbances, emotional lability and general weakness without the presence of objective neurological symptoms;
- the stage of subcompensation, which is characterized by a gradual progression of symptoms with personality changes - the development of apathy, depression with a decrease in the range of interests and the addition of major neurological syndromes (mild pyramidal insufficiency, reflexes of oral automatism and coordination disorders;
- stage of decompensation with severe neurological disorders caused by the development of multiple lacunar and cortical infarctions with clear manifestations of pyramidal, pseudobulbar, discoordination, amyostatic and psychoorganic syndromes with the gradual formation of vascular dementia.
Stage II of chronic cerebral ischemia (subcompensation) is characterized by the progression of clinical symptoms and the presence of focal neurological symptoms with the formation of pathological clinical syndromes with worsening cognitive disorders. They manifest themselves in a progressive decline in memory due to a violation of the active search and reproduction of necessary data with sufficient preservation of anamnestic material.
Attention disorders, bradyphrenia (slowing the activity of mental processes) and limited ability to control and plan are also observed. Patients experience emotional and personal disorders, which are manifested by severe emotional lability, depression and decreased criticism. At this stage of the disease, social and professional adaptation is disrupted, but the ability to self-care is preserved.
Disability due to hypertension of various stages and degrees
Many people suffer from high blood pressure levels from time to time. However, the vast majority of them are not even aware of their disease – arterial hypertension.
The initial stages of hypertension are hidden, its symptoms are blurred and do not particularly bother the patient. But if treatment is not undertaken, the pathology worsens and irreversible damage to target organs occurs.
In addition, the disease often acts as a factor causing disability, and this is high rice, due to the fact that it entails a serious decrease in the patient’s performance and the disease only progresses further.
A person with hypertension is prohibited from performing any work involving significant mental or physical stress. They are also contraindicated from working in hot workshops, working under the influence of pronounced noise, vibration, with certain types of poisons, as well as on night shifts.
You should know that a patient with hypertension must:
- be registered with a dispensary;
- undergo medical examination at established intervals;
- You can undergo a course of rehabilitation treatment.
If a person experiences a rapid deterioration in health, severe complications of the disease have begun, treatment in sanatoriums is contraindicated until his condition normalizes.
Stages of hypertension
The appropriate disability group for hypertension will be established, first of all, depending on its current stage.
Doctors distinguish three degrees of hypertension. The initial stage is characterized by:
- heart lesions have not yet developed;
- blood pressure rises periodically;
- ability to work is maintained.
However, even in the presence of the first degree of illness, it is necessary to create more comfortable working conditions.
As noted above, a hypertensive patient should be protected from severe stressful situations, contact with vascular poisons, excessive noise and vibration. When a person is diagnosed with an illness at this stage, he needs to contact a medical and labor expert commission to resolve the issue of employment.
The second degree of hypertension is characterized by cardiomuscular changes and persistently elevated blood pressure. If this form of pathology is present, the following restrictions will be added to the restrictions listed above:
- prevention of work activities that involve constant overexertion;
- prohibition of working at heights, near moving mechanisms, in hot shops.
The patient needs to reduce the amount of work that requires increased concentration and reduce the length of the working day.
At the third stage of hypertension, a person is almost always unable to work, resulting in the need to establish a specific disability group.
Sometimes, based on the results of a full medical examination, a patient may be recognized as partially able to work. He will be allowed to do his work at home or in comfortable, favorable conditions.
Third-degree hypertension provokes pathological changes in the brain and increases the risk of ischemic and hemorrhagic stroke. The doctor will pay attention to damage to the blood vessels, the structure of the central nervous system, and the condition of the kidneys. These symptoms further aggravate hypertension.
From the side of the heart can begin:
- myocardial infarction;
- hemodynamic instability;
- impaired vision clarity.
In some patients, retinal vessels are damaged, arteries dilate, and aneurysms form. The disease increases the risk of developing encephalopathy and the formation of an aneurysm inside the skull or brain.
How can I get a group?
on
To obtain a disability group, you must undergo a medical examination. Its results will be taken into account along with:
- with the stage of hypertension;
- with the presence of complications, their severity;
- with a history of hypertensive crises.
Additionally, it is necessary to assess the professional characteristics inherent in a particular work activity. Disability due to hypertension is established in relation to patients suffering from the disease of the second degree. In such cases, you can get a third group.
Stage 2 hypertension itself occurs without severe disorders, and target organ damage is not sufficiently expressed.
For these reasons, hypertensive patients are classified as a low risk group (in exceptional cases – medium). That is why, in the presence of second-degree hypertension, disability will be established only for proper employment.
The second disability group is given to those patients whose hypertension occurs with complications. In this case, the pathology is of the third degree, damage to internal organs is pronounced, heart failure gives severe symptoms.
The risk for this form of the disease is increased, treatment gives insufficient results. The second group of disabilities in the vast majority of cases is non-working.
The first disability group will be established for patients who have arterial hypertension of the third degree, and the disease:
- progresses rapidly;
- the risk of severe end-organ damage increases;
- severe heart failure is observed;
- there is a significant limitation in the ability to self-care, communication, and normal movement.
Treatment in this case does not bring the desired result.
Diagnostics
Chronic cerebral ischemia syndrome can only be determined by conducting several laboratory and instrumental studies. Due to the similarity of symptoms with other diseases (for example, Alzheimer's or Parkinson's disease), differential diagnosis is also required. Laboratory blood tests include:
- general analysis;
- biochemistry;
- PTI.
Diagnosis of chronic cerebral ischemia is based on an analysis of the disease history, the presence of neuropsychological and neurological symptoms with cardiac examination (electrocardiography, Holter monitoring and echocardiography) to establish the main cause of progression of cerebral ischemia, as well as laboratory research methods to exclude somatic pathology.
The direct examination of the condition of brain tissue is carried out using paraclinical methods - CT or MRI of the brain, duplex ultrasound scanning, Doppler ultrasound, transcranial Doppler ultrasound with the mandatory determination of rheological and coagulation characteristics of blood, the content of lipid fractions, cholesterol and blood glucose.
Therapeutic measures
First of all, it is necessary to normalize blood pressure to prevent stroke and ischemic attacks. The doctor prescribes vasodilators, such as pentoxifylline and anticoagulants.
One of the conditions for successful treatment is the reproduction of standard blood flow to the brain, which will improve the metabolic processes occurring in its tissues. The treatment method will help improve memory, bring consciousness to normality and clarity of thinking. Along the way, motor functions begin to normalize. Nootropic drugs are used in treatment, among which piracetam occupies a central place.
To thin the blood, cardiomagnyl or aspicard is prescribed. We must not forget about vitamin preparations to maintain brain nerve cells. It is important to prevent blood clots and improve brain function. Physiological reactions are subject to restoration.
Surgical intervention is used quite rarely, especially during stage 2 ischemia. The operation is prescribed in special cases to eliminate atherosclerotic plaques.
Physiotherapeutic treatment in the form of massage and acupuncture helps in regulatory processes.
Quite often, treatment begins with prescribing a diet, eliminating fatty, spicy and salty foods. Fried foods disappear completely in order to keep the walls of blood vessels intact from the appearance of atherosclerotic plaques on them.
The circulatory system of the human body transports blood flow and distributes it to organs.
With improper nutrition, plaques begin to form in the vessels, salts and cholesterol are deposited on the walls.
A clogged and clogged blood vessel is not able to independently deal with the obstacles that have arisen in it. At the same time, all organs begin to experience a stressful situation due to lack of oxygen. The tissues literally “suffocate”; freeing the walls of blood vessels becomes the task of any person before the disease overtakes him.
Anyone can lower the disease threshold by leading an active lifestyle, especially after 50 years. Physical activity should replace intellectual tension. Fresh air before bed will have a beneficial effect on a good night's rest. Light exercise, walking, climbing stairs, healthy eating and good mood will be the key to your health.
First of all, it is necessary to normalize blood pressure to prevent stroke and ischemic attacks. The doctor prescribes vasodilators, such as pentoxifylline and anticoagulants.
To thin the blood, cardiomagnyl or aspicard is prescribed. We must not forget about vitamin preparations to maintain brain nerve cells. It is important to prevent blood clots and improve brain function. Physiological reactions are subject to restoration.
I recently read an article that talks about Monastic tea for treating heart disease. With this tea you can FOREVER cure arrhythmia, heart failure, atherosclerosis, coronary heart disease, myocardial infarction and many other diseases of the heart and blood vessels at home.
I’m not used to trusting any information, but I decided to check and ordered a bag. I noticed changes within a week: the constant pain and tingling in my heart that had tormented me before receded, and after 2 weeks disappeared completely. Try it too, and if anyone is interested, below is the link to the article.
Quite often, treatment begins with prescribing a diet, eliminating fatty, spicy and salty foods. Fried foods disappear completely in order to keep the walls of blood vessels intact from the appearance of atherosclerotic plaques on them.
Treatment
- Diet. Refusal to eat fatty, fried, salty, spicy foods, i.e. hypocholesterol and antihypertensive diet. Fight bad habits.
- Normalization of blood pressure (lisinopril, hartil), cholesterol (trovan, atorvastatin).
- Blood thinning (cardiomagnyl, aspicardium).
- Drugs to maintain the normal functioning of brain cells, nootropics and neuroprotectors (piracetam, actovegin, encephabol).
- Vascular (sermion).
- Vitamin preparations for nervous tissue (milgamma, neuromultivit).
- Physiotherapy, massage, acupuncture.
- In severe cases, surgery is performed on the brain or neck vessels: removal of a blood clot or atherosclerotic plaque.
Treatment methods
In medicine, chronic cerebral ischemia syndrome is considered as a disorder that arises against the background of pathology of the circulatory system. For this reason, treatment consists of eliminating symptoms and the underlying disease. If CCI is diagnosed at the initial stage, then treatment is carried out only therapeutically at home. Grade 2 ischemia may require hospitalization if severe physical symptoms are observed.
The main direction of drug therapy is to normalize the functioning of the brain and eliminate the causes of vasoconstriction. For this purpose, four groups of drugs are used.
Drug treatment of chronic cerebral ischemia is carried out in two directions
- Antihypertensive group of drugs (inhibitors and antagonists). Affects blood pressure, helping to stabilize it. It is recommended to take Hydrochlorothiazide or Indapamide.
- Lipid-lowering drugs. When cholesterol plaques form, drugs are prescribed: Atorvastatin or Simvastatin. Medicines have an additional effect on reducing blood clotting, improving endothelial functionality and accelerating cell regeneration.
- Antiplatelet agents. To prevent the formation of blood clots, it is recommended to take blood thinning medications. Acetylsalicylic acid is considered one of the effective remedies. Dipyridamole or Clopidogrel can be taken together.
- Combined group of drugs. Chronic cerebral ischemia of the 2nd degree and decompensation stage requires enhanced drug therapy, so drugs of combined action are often prescribed. Complex drugs: Vinpocytine, Piracitam (together with Cinnarizine or Vinpocytine), Pentoxifylline, Nitroglycerin.
All medications are used in courses. The treatment regimen can only be determined by the attending physician. You should not determine the dosage or duration of the course yourself. Violations in the drug therapy system can provoke an acceleration of the process of damage to brain cells.
In case of chronic cerebral ischemia, surgical intervention is required in case of damage to the main cerebral artery or if the arteries are blocked by blood clots (plaques). The operation can also be performed to eliminate provoking causes associated with the development of vascular diseases (for example, deformation and change in direction).
In chronic cerebral ischemia, the indication for surgical intervention is considered to be the development of occlusive-stenotic lesions of the main arteries of the head
Surgical intervention to restore blood flow is performed by stenting or endarterectomy. In the first stage, surgery is not required. If chronic cerebral ischemia of the 2nd degree cannot be treated, but continues to progress, it is permissible to prescribe surgical intervention in order to eliminate the cause of vascular pathology associated with impaired blood supply to the brain.
Treatment of arterial hypertension includes non-drug and drug correction methods.
Non-drug means of preventing the occurrence of acute disorders of cerebrovascular circulation of the ischemic type and reducing the progression of chronic cerebral ischemia are increasing the physical activity of patients, quitting smoking, limiting the consumption of alcohol and table salt, increasing the content of fruits and vegetables, and fermented milk products in the diet.
Causes and consequences of cerebral ischemia in newborns
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
Cerebral ischemia is a condition in which the organ suffers from oxygen deficiency. Cerebral ischemia in newborns is a serious problem in perinatal neurology, because in modern medicine there are no effective treatments for this disease. The brain is the most sensitive organ to oxygen deficiency. If it is left without adequate supply for some time, some neurons die. But in young children, unlike adults, nerve cells are numerous and are able to restore their functions, which reduces the likelihood of negative consequences of ischemia. Effective and timely treatment can help restore brain tissue.
Degrees and reasons
There are 2 degrees of this pathology:
- Cerebral ischemia grade 1: the infant experiences periods of excessive lethargy or, conversely, activity. This condition lasts up to 7 days. With mild cerebral hypoxia, a child rarely develops significant neurological disorders.
- Cerebral ischemia of the 2nd degree is characterized by a longer period of behavioral disturbances, the appearance of seizures, twitching of the limbs, and frequent and profuse regurgitation. The child has an increased risk of developing neurological disorders in the future (delayed mental and speech development, visual and hearing impairment, etc.).
Mild cerebral ischemia in newborns develops if:
- the woman led an unhealthy lifestyle while carrying a child (smoked, drank alcohol, did not follow a daily routine, moved little, was in a state of severe stress);
- The expectant mother's chronic diseases worsened during pregnancy.
These negative factors contribute to the development of feto-placental insufficiency, which negatively affects the oxygen supply to the fetus, as well as the development of the unborn child.
The risk of such an anomaly in a baby increases if it was given birth to by a woman under 17 years of age. The likelihood of developing an unfavorable condition in an infant born as a result of late pregnancy (after 40 years) also increases.
Grade 2 cerebral ischemia develops for the following reasons:
- late gestosis;
- oligohydramnios;
- abnormal structure of the placenta and (or) umbilical cord;
- premature birth or, conversely, post-term pregnancy;
- high blood pressure in a pregnant woman;
- birth injuries;
- intrauterine infections.
Symptoms
With mild cerebral ischemia in a newborn, the following signs are observed:
- poor sleep, crying even while staying in comfortable conditions;
- weakening of the sucking (swallowing) reflex;
- facial asymmetry, strabismus (less commonly).
Stage 2 of this pathology has the following symptoms:
- increase in head size;
- increased nervous excitability (anxious sleep, tremor of the chin and lips, involuntary shudders, monotonous crying for no reason);
- “marbled” skin (spotted red or bluish stains on the child’s skin);
- gastrointestinal disorders (bloating, diarrhea, frequent and profuse regurgitation);
- increased muscle tone;
- convulsions;
- cessation of breathing;
- frequent episodes of loss of consciousness.
Diagnostics
If the parents of a newborn notice some of the listed symptoms in their child, they should immediately contact a pediatric neurologist. The sooner treatment is started, the faster the child will recover. The following studies are indicated for infants suspected of having this pathology:
- pulse oximetry (determination of oxygen saturation in the blood);
- magnetic resonance imaging (MRI) of the brain;
- Doppler examination of cerebral vessels;
- ultrasound examination (ultrasound) of the brain;
- echoencephalography.
Treatment
Therapy is aimed at restoring impaired blood circulation in the brain and eliminating the consequences of hypoxia. The child’s body weight, type of delivery, and the presence of other pathologies are taken into account. First of all, a child with cerebral ischemia is provided with comfortable living conditions:
- maintain a daily routine;
- often walk in the fresh air (the baby is dressed according to the weather);
- do not overfeed;
- in the house where the baby lives, they take care of a calm environment.
Young patients with mild cerebral ischemia do not need drug therapy; treatment is limited to massage and recreational exercises. In the first years of life, it is important to observe a protective regime, which consists in eliminating factors that negatively affect the child’s psyche (aggression, noise, overabundance of impressions).
Why do you feed pharmacies if hypertension is afraid of the usual like fire...
Tabakov has revealed a unique remedy against hypertension! To reduce blood pressure while preserving blood vessels, add to…
Grade 2 cerebral ischemia in newborns requires intensive treatment. The baby is prescribed:
- anticonvulsants (Phenytonin, Phenobarbital);
- drugs that support normal heart function (Dopamine, Dobutamine);
- diuretics (Furosemide, Lasix);
- nootropics (Actovegin, Phenibut, Glycine, Encephabol, Pantogam).
The drugs are given to the child in strict accordance with the regimen prescribed by the doctor. If taking medications causes adverse reactions, you should immediately consult a doctor.
For grade 2 cerebral ischemia, relaxing massage and therapeutic exercises are also prescribed. However, for seizures, physical methods are not used. It is prohibited to treat pathology using traditional methods, because the fragile body of a newborn does not tolerate such experiments.
Parents of a child diagnosed with cerebral ischemia should carefully monitor the characteristics of his physical and mental development and report them to the attending physician. Often children with a similar diagnosis begin to hold their heads up, roll over, sit up, walk, and talk later than their peers. But adequate therapy helps normalize the child’s development.
Consequences
The risk of negative consequences depends on the severity of the disease, the effectiveness and timeliness of treatment, as well as the presence of other pathologies in the patient. Consequences of the disease:
- weather dependence;
- headache;
- insomnia at night or drowsiness during the day;
- retardation in speech and mental development;
- epilepsy;
- difficulties with communication;
- impaired concentration;
- excessive nervous excitability or aggression;
- psychical deviations;
- learning disabilities.
In the most severe case, the baby develops cerebral palsy (CP).
A child who has the negative consequences of cerebral hypoxia should grow up under the supervision of a child psychologist, speech therapist and psychiatrist.
Folk remedies in the treatment process
After consultation with a neurologist, you can turn to some traditional healing recipes. Among them, garlic is popular.
- The crushed garlic mass is poured with alcohol in a 1:1 ratio and infused for 15 days. Take 5 drops of tincture dissolved in a tablespoon of milk.
- From the leaves of the walnut tree 1 tbsp. l of the mixture, pour 300 ml of boiling water, infuse and take half a glass before meals.
After consultation with a neurologist, you can turn to some traditional healing recipes. Among them, garlic is popular.
Recommendations
CCI is characterized by gradual progression, therefore, the earlier the pathology is identified, the greater the chances of avoiding further brain damage, which threatens the complete elimination of the personality and the development of physiological disorders, which result in disability. In order to prevent ischemia, it is recommended to follow several expert tips:
- If possible, it is necessary to exclude the influence of external negative factors (stress, poor diet, bad habits, etc.).
- When diseases related to the vascular system and blood circulation appear, timely treatment and constant monitoring are required.
- For good blood circulation, daily walks (preferably in the fresh air) and exercise are recommended.
Signs of illness should not be ignored. You must always remember that brain cells do not regenerate and the more the pathological process starts, the more severe the consequences will be.
Reasons for the development of HIE
Ischemia in a newborn is not an independent disease, but a consequence of oxygen starvation of the brain (hypoxia). During its development, metabolic processes in brain cells are disrupted, and the brain is subject to various disorders. Such disorders cause the death of neurons, the development of necrosis and other conditions that negatively affect the functionality of the brain. And the higher the degree of oxygen deficiency, the more severe the child’s condition.
And the reasons for the development of hypoxia can be various factors. The most important and frequently encountered of them are:
- Intrauterine fetal hypoxia. One of the most common reasons. It occurs against the background of a disturbance in the flow of blood from the mother to the placenta, or vice versa.
- Asphyxia of a child. There are intranatal and postnatal. In the first case, asphyxia occurs during the passage of the child through the birth canal, in the second - in the first minutes after birth.
- Respiratory distress syndrome. A serious condition in which non-cardiogenic (not related to the functionality of the heart) pulmonary edema and disruption of external respiration occurs.
- Apnea attacks. The peak occurs during sleep and is accompanied by cessation of breathing.
- Congenital heart defect. If it is present, the blood flow to the brain is disrupted, which provokes the appearance of hypoxia. The most common occurrence in young children is PDA (patent ductus arteriosus).
- Disturbance of the hemodynamic system. In newborns, this condition causes a sharp drop in blood pressure, resulting in a decrease in the speed of cerebral blood flow.
It should also be noted that the development of hypoxia in a child can occur for other reasons related to the condition of the mother during pregnancy. For example:
- respiratory viral diseases;
- decreased level of hemoglobin in the blood (iron deficiency anemia);
- elevated blood glucose levels (diabetes mellitus);
- malnutrition (lack of the required amount of micro- and macroelements in the diet);
- bad habits (smoking, alcohol abuse, drug use, etc.);
- age (after 35 years, women are more likely to give birth to children with HIE, and the older the age, the higher the risk of developing this disease).
There is also so-called periventricular ischemia in newborns. What it is? This condition is also characterized by oxygen starvation of the brain, but the reason for this is most often premature birth. The peculiarities of this lesion are that it involves areas of the brain located around its ventricles.