Lipodermatosclerosis: what it is, symptoms and treatment of leg disease
1. Clinic of lipodermatosclerosis
: - Consolidated plaques of a woody consistency on the legs, acute and chronic changes, often pain. — Chronic venous insufficiency, body mass index above normal, female gender, arterial hypertension, arterial ischemia, episodes of thrombophlebitis. — Pulmonary hypertension in patients with systemic sclerosis and sclerosing panniculitis.
2. Histopathology of lipodermatosclerosis
: - Predominantly lobular panniculitis without vasculitis against the background of stasis. — Ischemic necrosis in the center of the fat lobule. — Thickened and fibrous septa and atrophy of subcutaneous fat with pronounced fibrosis and sclerosis in the later stages in severe cases. — Frequent membranous cystic changes.
3. Therapy for lipodermatosclerosis
: - Compression stockings, ultrasound therapy, pentoxifylline. - In some cases, a good response to anabolic steroids.
Lipodermatosclerosis
(
LSD
) (synonyms: sclerosing panniculitis, hypodermitis sclerodermiformis, chronic panniculitis with lipomembrane changes, sclerotic atrophic cellulitis, venous stasis panniculitis) is a form of sclerosing panniculitis affecting the lower extremities.
a) Epidemiology
. Lipodermatosclerosis (LDS) is the most common form of panniculitis and is seen by doctors much more often than erythema nodosum, the second most common panniculitis. VDS develops in combination with venous insufficiency, often in overweight women over 40 years of age. In a review of 97 patients with LDS, 87% were women with a mean age at diagnosis of 62 years; 85% of patients were overweight (body mass index > 30); 66% were obese (body mass index >34). Concomitant diseases included hypertension (41% of patients), thyroid diseases (29%), diabetes mellitus (21%), a history of cellulitis of the lower extremities (23%), deep vein thrombosis (19%), psychiatric pathology (13%) , peripheral neuropathy (8%) and obliterating atherosclerosis (5%). Partly because this disease was placed in the ICD-9 classification in the section “Venous insufficiency with inflammation”, and also due to the designation of this pathology by various medical terms (see above for the list of synonyms for VDS), accurate data on the prevalence of VDS are not available. With the increasing obesity population and the aging of the baby boom generation, the incidence and prevalence of LDS is likely to increase in the United States.
b) Etiology and pathogenesis of lipodermatosclerosis
(LDS). The majority of patients with VDS are women, with common characteristics being venous hypertension and a higher than normal body mass index. Additional associated signs that are considered pathogenetic factors in LDS include increased vascular permeability due to increased hydrostatic pressure as a result of inactivation of locking intercellular contacts with extravascular diffusion of fibrin; microthrombi; abnormalities in protein S and protein C; hypoxia; damage to endothelial cells by inflammatory cells; activation of intercellular adhesion molecule 1 (ICAM-1), vascular cell adhesion molecule 1 (VCAM-1), leukocyte functional antigen 1 (LFA-1), platelet and endothelial factors; as well as inflammation with wound healing and local stimulation of collagen synthesis leading to fibrosis and further damage to blood and lymphatic vessels. Fibrosis is accompanied by increased expression of the transforming growth factor-31 (TGF-β1) gene and protein, as well as increased expression of the procollagen type 1 gene.
Hypoxia in adipose tissue (AT) causes chronic inflammation with macrophage infiltration and expression of inflammatory cytokines. The adipocyte plays an important role in the remodeling of extracellular tissue. To this end, the adipocyte synthesizes numerous matrix metalloproteinases (MMPs), as well as tissue inhibitors of matrix metalloproteinases (TIMPs) and other tissue proteases required during tissue remodeling, all of which may contribute significantly to the remodeling process observed in LDS. Recent studies have linked the expansion of AT (observed in obesity) with subsequent hypoxia, which causes an increase in the expression of hypoxia-inducible factor la (HIF 1α). This stimulates numerous extracellular factors, including collagen I and III, as well as other components involved in the remodeling of the extracellular matrix and ultimately leading to fibrosis.
Cantwell et al. proposed a theory of the infectious pathogenesis of LDS, they reported the presence of unusual acid-fast bacteria in biopsies of several patients with LDS that could not be grown in culture. A 1979 paper addressed the controversial proposal of pleomorphic, non-rod-shaped acid-fast bacteria as the cause of the disease. It is well known that other infections associated with multiple episodes of cellulitis cause damage to the lymphatic vessels and subsequent changes in AT. In light of recent evidence that adipocytes are cells of the innate immune system and possible reservoirs of infectious organisms of all types, the role of infection as a causative factor in LDS needs to be reconsidered and investigated, perhaps in the same way that led to the discovery of Mtb DNA and latent Mtb in the AT of the lower extremities with indurative erythema.
b) Symptoms and clinical picture of lipodermatosclerosis
(LDS). LDS has an acute inflammatory stage and a chronic fibrotic stage with a spectrum of intermediate and cross manifestations. Patients with the acute form present with a pattern of very painful, ill-defined lesions ranging from cellulite-like, erythematous to purple, swollen, somewhat indurated plaques or nodules on the lower extremities, most commonly in the lower anteromedial gastrocnemius region. In some cases, peeling is observed. The pain can be so severe that patients cannot tolerate the touch of sheets while in bed. At this stage, patients are often diagnosed with erythema nodosum, cellulitis or thrombophlebitis, and patients cannot tolerate compression. The acute form can last for several months or even a year. Although patients in this acute stage may not have obvious signs of venous pathology, vascular examination reveals venous insufficiency in most patients. In the group of remaining patients with LDS and a normal vascular examination, the majority have a high body mass index, and given that obesity is usually associated with inactivity, in such patients the contraction of the calf muscles may be insufficient to maintain normal venous pressure in the lower extremities; obesity is also often associated with hypertension.
The clinically obvious acute form does not always precede the chronic form of LDS. Chronic LDS is characterized by thickened or sclerotic, sunken, hyperpigmented skin. Such signs are noted on the lower part of the legs, mainly, but not exclusively on the medial surface or in the “stocking” localization. This distribution of lesions has been described as an "upside down champagne bottle" or "bowling pin" pattern. Although some patients do not report associated pain or tenderness, these are the most common symptoms reported by other patients. Most patients are obese or overweight, have hypertension and evidence of venous anomaly, but only rarely venous obstruction. Unilateral lesions are observed in 55% of cases, localized plaques in 51%, and ulceration in 13% of cases. Dermatosclerosis in patients with systemic sclerosis is associated with pulmonary infarction and hypertension due to lower extremity thrombi.
Treatment of venous dermatitis
In case of dermatitis associated with vein pathology, it is necessary to consult a doctor as soon as possible. If treatment is not started on time, dangerous complications can develop that can be very difficult to cope with.
All therapy is divided into drug treatment and a number of non-drug measures aimed at alleviating the condition and reducing symptoms.
- For venous dermatitis, soaps and bubble baths are contraindicated, as they dry out the skin and irritate areas of the body affected by eczema. Regular moisturizing lotion can be used as a substitute for soap by applying to damp skin and then rinsing off.
- When using a shower or bath for personal hygiene, the water should be lukewarm, or even cool. Hot water causes severe loss of moisture and worsens the itching.
- Contact with water should be short. Water washes away the fatty protective layer, and moisture freely evaporates from the skin. You should not take a bath longer than 10 - 15 minutes.
- Products containing alcohol, dyes and fragrances are dangerous for eczema skin. They can cause irritation and allergies, and worsen the symptoms of dermatitis.
Treatment with medications
- Emollients, or medicated moisturizers, help keep skin hydrated and elastic and prevent damage and cracking. This is one of the most important groups of drugs in the treatment of all types of eczema. Use the product on your legs and feet twice a day, or more often if your skin is very dry. Apply it with light movements, in enough quantity to make the skin look slightly shiny.
- Glucocorticosteroids are medications based on adrenal hormones. They have an anti-inflammatory effect. Entering the subcutaneous tissue, glucocorticoids inhibit immune cells and prevent them from releasing inflammatory mediators - chemicals responsible for the symptoms of eczema. In the treatment of venous dermatitis, these drugs should be used with caution, since tissue swelling and increased vascular permeability in the area of the pathological process lead to the fact that the drug is absorbed in large quantities and enters the bloodstream. Side effects can be quite serious: decreased immunity, obesity, increased blood pressure and blood sugar levels, suppression of the adrenal glands. Therefore, moderate or weak glucocorticoids are used according to their potency, and they are prescribed for a short course. Hydrocortisone and prednisolone ointments are suitable.
- Non-steroidal anti-inflammatory ointments regulate immunity and suppress inflammation, while they do not contain hormones and are free of their side effects. These drugs include Elidel cream; it is well suited for targeted therapy of varicose veins dermatitis.
- Zinc oxide is used in this disease due to its drying effect. Due to swelling, eczema against the background of varicose veins often becomes wet, and clear discharge oozes from the lesions on the skin. Zinc oxide reduces itching, softens and alleviates general discomfort.
- Antimicrobial agents become relevant if an infection occurs. In conditions of impaired microcirculation, edema and damage to the epithelium, bacteria inhabiting the surface of the body easily penetrate inside, into the subcutaneous tissue, and cause inflammation. In this situation, antibiotics must be taken in tablet form, and antiseptic solutions must be used topically. The doctor selects a suitable drug, usually a broad-spectrum antibiotic from the group of penicillins, cephalosporins or macrolides.
Manifestations and complications of varicose veins
Edema . In the initial stages of the disease, swelling occurs in the afternoon in the area of the foot and lower third of the leg, and goes away in the morning when the limb is in a horizontal position for a long time.
Pain . The pain is bursting, aching in nature and is associated with the development of edema. In the initial stages it occurs in a lying position, but as the disease progresses it can be permanent.
Night cramps . In the area of the calf muscles, convulsive twitching may occur mainly at night. The development of seizures is associated with impaired venous circulation in the muscles.
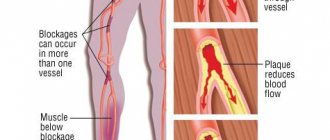
Lipodermatosclerosis is thickening of the skin and subcutaneous tissue due to chronic inflammation. In this case, the skin and fiber are fixed to the underlying muscle fascia and lose mobility. In this case, it is impossible to gather the skin into a fold on the shin.
Skin pigmentation . Pigmentation develops with prolonged venous stasis. Altered vessels with a thinned wall are much more susceptible to injury, and even minor impacts cause them to rupture and the release of red blood cells outside the vessel. Histologically, hyperpigmentation represents released red blood cells and macrophages with hemosiderin between dilated capillaries.
Venous dermatitis . Also called venous eczema, varicose eczema, hypostatic dermatitis. Of course, since true “stasis” cannot exist, but venous hypertension occurs, the optimal name is venous dermatitis.
More often, venous dermatitis appears in women, in obese patients, in patients who have suffered superficial and deep thrombophlebitis. A precursor to dermatitis, which disrupts normal blood circulation in the skin, is swelling. Dermatitis usually begins in the area of the medial ankle and is manifested by redness, peeling, and often weeping of the skin. Histological examination of the skin shows diffuse destruction of collagen, fragmentation or absence of elastic fibers, thickening or narrowing of arterioles. These changes are nonspecific, and the diagnosis of venous dermatitis can only be made taking into account the general clinical picture.
Clinical manifestations
The disease progresses for quite a long time. The first symptom of changes occurring in the skin may be itching. The inner and back surface of the lower limb itches and burns, especially after prolonged standing. Often these manifestations go unnoticed.
As the disease progresses, other symptoms appear. One of them is swelling of the lower third of the leg. Initially, it appears only in the evening in the form of a slight increase in the volume of the leg; in the morning there are no signs of swelling.
You should know that the accumulation of excess fluid in tissues can be compensated for a long time, in which case the person does not notice it. Hidden swelling can be identified by looking at the part of the lower leg to which the elastic of the sock is adjacent. If a trace of the gum remains, it means there is swelling. When the flow of venous blood is significantly impaired, the legs remain enlarged due to fluid throughout the day.
In addition, with lipodermatosclerosis, heaviness in the legs may be bothersome, increasing in the evening and decreasing after sleep. The color of the shins changes gradually. At first they turn pale, then acquire a bluish tint, and then brown. Even minor trauma to the skin leads to long-term non-healing wounds.
The skin is very dense and thin - a symptom of parchment paper. Sometimes you can see the leakage of cerebrospinal fluid from the enlarged, pasty lower extremities in the form of a clean, transparent liquid without color or odor. In this case, there is often no pain, but numbness or tingling may be felt.
If the disease is not treated, trophic ulcers may appear.
Depending on the cause of lipodermatosclerosis, all manifestations can occur on one leg or on both.
Changes in the skin of the legs with varicose veins
Saratov State Medical University named after. IN AND. Razumovsky (SSMU, media)
Level of education - Specialist
1990 - Ryazan Medical Institute named after Academician I.P. Pavlova
Pathological changes in the veins of the lower extremities are considered common, especially among athletes and the elderly. If the blood supply to a certain area of the skin is disrupted, venous pressure increases and varicose veins occur. The dilation of the veins becomes very noticeable, blood vessels appear, and changes in the process of cellular nutrition (trophism) occur. When the disease is not treated for a long time, trophic changes in the skin occur with varicose veins, which are accompanied by damage to the skin. In the affected area, significant increases in skin pigmentation, dermatitis, eczema and trophic ulcers are observed.
What does varicose veins look like and what to do?
Symptoms of lipodermatosclerosis with varicose veins appear in chronic venous insufficiency. External symptoms reflect complex processes that cannot be changed. This:
- The shape of a leg affected by varicose veins becomes similar to an inverted pin with the narrowest point in the shin area.
- The lower part of the leg is compacted and may have a dark color due to pigmentation or bluish discoloration.
- Symptoms of focal structural disturbances appear in the form of ulcerative processes with a long course.
- Varicose dermatitis with other symptoms (itching, peeling, erosion, purulent complications) may be present.
Such a complex condition can only be treated comprehensively. After the examination, the doctor suggests ways to eliminate the insufficiency of the venous vessels, as a radical method of treating varicose veins. Usually they combine surgical manipulations with local treatment and the prescription of general drugs. Before the surgical stage of treatment of varicose veins, the doctor suggests that the patient (usually women) reconsider her lifestyle.
The disease develops as a consequence of lupus erythematosus or dermatomyositis.
The volume of possible physical activity and the optimal weight that the patient should have are clarified. Compression stockings must be used in the preoperative period and after surgery. Local treatment includes hardware or manual lymphatic drainage, physiotherapy using galvanization, the use of gels, ointments, compresses, lotions, baths, and wraps.
Phlebopathies and lymphostasis can be causes of lipodermatosclerosis in advanced cases. It also appears after several years of the process's existence. The best prevention of its occurrence is timely treatment of the diseases that cause it.
Causes
Predisposing factors for inflammation of the skin on the legs are quite similar to the causes of varicose veins:
- carrying heavy objects;
- overweight;
- diabetes;
- pregnancy and childbirth;
- genetic predisposition;
- lower limb injuries;
- chronic infections;
- decrease in the body's defenses;
- metabolic disorder (metabolic process) and microcirculation;
- disruptions in the functioning of the cardiovascular system;
- venous insufficiency;
- swelling of tissues.
With trophic disorders, the skin becomes thin, dry and easily injured. Other problems with the skin and condition of the legs also arise:
- puffiness and swelling;
- burning and pain in the affected area, the skin becomes very hot;
- heaviness in the limbs;
- necrosis of the epidermis;
- the appearance of red itchy spots, which eventually acquire a blue tint;
- the skin becomes smooth and shiny;
- small bubbles appear, which burst and erosions form in their place;
- Liquid begins to seep through the skin.
Trophic ulcers develop both on the top layer of skin and can go deep into the wound. In this case, the person experiences severe pain in the calves or tendons of the legs, and there is a high risk of osteomyelitis (an infectious inflammation of all parts of the bone tissue). The person becomes irritable and restless, and sleep disturbances occur.
Causes of lipodermatosclerosis development
To understand the causes of the development of pathology and select the appropriate treatment method, it is necessary to know the principles of operation of all elements of the cardiovascular system of the human body.
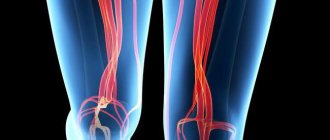
The outflow of blood from that part of the body that is located below the level of the heart is carried out due to the functioning of skeletal muscles and a special valve apparatus located in the venous vessels.
Venous vessels located in the lower extremities are at risk of the occurrence and progression of venous insufficiency, which may be due to the imperfection of the mechanisms ensuring the outflow of blood. As a result of such disorders, stagnation of venous blood occurs in the vascular system, which provokes the appearance of pathological phenomena.
There is a whole range of reasons for the appearance of chronic venous insufficiency. Among the variety of factors contributing to the occurrence of pathology, the following can be identified as the main ones:
- being overweight and leading a sedentary lifestyle;
- bearing a fetus and engaging in sedentary work;
- getting injured;
- changes in hormonal balance in women in the age group 40+;
- the body receiving excessive and regular static load in an uncomfortable position;
- presence of chronic heart disease;
- the occurrence and progression of varicose veins of the superficial venous vessels of the lower limb;
- development of thrombosis of deep venous vessels of the leg.
What happens in the skin of the lower extremities in the event of the appearance and progression of chronic venous insufficiency. Stagnation of venous blood, which is poor in oxygen content and leads to negative consequences. The deepest layer of the skin is essentially the hypodermis. It is represented by adipose tissue, the function of which is to provide thermal insulation, produce certain types of hormones and store energy. In addition, this layer of the skin is necessary for storing nutritional compounds and performing a shock-absorbing function.
Latest information: Postthrombophlebitic disease of the veins of the lower extremities: treatment
When venous circulation is disrupted, hypodermal cells experience oxygen starvation.
This state of cellular structures leads to a change in their functional activity. Which leads to the replacement of adipose tissue with connective tissue. Connective tissue fibers do not have the ability to perform the functions of the hypodermis.
All of these changes provoke the appearance and progression of symptoms characteristic of lipodermatosclerosis.
Types of trophic changes in the skin of the legs
Against the background of impaired venous outflow in the lower extremities, trophic skin changes occur, which are characterized by a chronic course. And even after successful surgical treatment of the disease, external signs of ulcers and eczema do not disappear. Trophic disorders of soft tissues include:
- lipodermatosclerosis;
- hyperpigmentation;
- microbial eczema;
- skin atrophy (exhaustion, loss of vitality);
- trophic ulcers.
Microbial eczema
When venous stagnation occurs, it becomes difficult for local immunity to fight the pathogenic microflora that is present on the skin. Therefore, at the site of inflammation, various infectious agents (streptococci) or fungi begin to actively multiply. The body’s immune system responds to the irritant with an allergic reaction, and venous microbial eczema occurs. In the acute stage of eczema, the patient complains of itchy skin in areas affected by varicose veins and throughout the body. The skin begins to separate in small films, small wounds such as abrasions appear, and therefore the quality of life and moral well-being of the patient decreases.
Trophic ulcers
They have a chronic course, do not heal for a long time, but only increase in size. The wound periodically heals, but after a while it opens again. Scratching the wound causes infection. Local medications only in rare cases help healing, and special dressings do not justify themselves at all. In this case, an urgent consultation with a phlebologist and a diagnostic examination is required.
Patients with varicose eczema need a comprehensive treatment approach: drug and local therapy, balanced nutrition, a healthy lifestyle, distribution of work and rest. For trophic ulcers, surgery is indicated. After which the ulcers quickly heal. But darkening and thickening of the skin remain forever. Compression garments are recommended for everyone, without exception.
Therapy methods
Treatment of the disease is best started in the early stages, without leading the process to the development of serious problems . A comprehensive professional approach in this case includes:
- prevention of further stagnation of blood in the venous bed;
- improvement of microcirculation;
- strengthening the walls of blood vessels;
- restoring nutrition and moisturizing the skin;
- elimination of swelling in both legs;
- using compression stockings or tights;
- proper nutrition;
- weight loss;
- motor activity;
- physiotherapeutic techniques;
- local treatment.
Medicinal ointments and creams
The main method of getting rid of dermatosis against the background of varicose veins of the lower extremities is local therapy. For this purpose, ointments are used on an ongoing basis, along with medications for internal use.
Typically, treatment with various ointments provides hydration, relief from inflammation and itching.
- Menthol and camphor help relieve discomfort. They are available in the form of ointments and are used as needed.
- If the skin is severely dry, it is not recommended to perform hygiene procedures with soap, since the alkaline environment aggravates the condition of the dermis. Your doctor may recommend a special lotion for washing your feet.
- The presence of trophic ulcers leads to the need to use glucocorticoid creams and ointments. A short course of complex remedies is usually recommended. This avoids unwanted side effects.
- Before applying the drug, it is necessary to clean the skin; sometimes antiseptic solutions and anti-inflammatory drugs are used for this purpose.
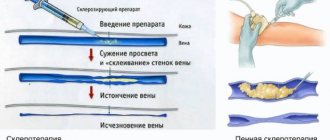
Phlebotonics (venotonics)
The most popular are Detralex and Phlebodia. Venoruton, Venitan, Escin are also effective. The mechanism of action of the funds is to influence the microcirculatory bed. Medicines in this group increase the tone of the venous wall, which improves the outflow of blood and lymph. At the same time, the activity of the inflammatory process decreases.
They are produced in tablets, ointments, gels and capsules. To obtain a quick effect, you should combine local application of the product with its oral administration .
Treatment is contraindicated for renal impairment or during acute illnesses. These medications should be used with caution and under the supervision of a specialist during pregnancy.
Antiplatelet agents and anticoagulants
To reduce the likelihood of developing thrombosis and improve microcirculation, anticoagulants and antiplatelet agents are prescribed. The first group acts on the blood, making it more liquid and preventing thickening. The second one inhibits the process of platelet aggregation, preventing them from sticking together. Lyoton, Curantil, Aspecard (aspirin), Trental have these features.
Antioxidants
Antioxidants help strengthen the vascular wall, therefore, thanks to them, the accumulation of the liquid part of the blood in the tissues is reduced and the symptom of swelling is eliminated. For complex treatment, Ascorutin or Venarus is used.
Anti-inflammatory drugs
NSAIDs help relieve inflammation, reduce the likelihood of blood clots, and relieve swelling. In addition, they reduce local discomfort - itching and soreness. Typically used are Indomethacin (solution for intramuscular administration, tablets or gel), or Diclofenac (tablets, ointment, gel, injections).
Antibacterial drugs
At the first stage, antibiotics are not used for varicose dermatitis. The need for them arises when complications develop in the form of suppuration or the appearance of concomitant ailments.
In case of infectious inflammation, it is no longer possible to do without antibiotics. Only they will help stop the further spread of the pathogen and the development of gangrene, phlegmon and sepsis.
For this purpose, wide-spectrum drugs are chosen to influence not only aerobic, but also anaerobic flora.
Penicillin drugs, tetracyclines and macrolides usually help in this case. Along with oral or parenteral administration, antiseptics are used in solutions to treat affected areas and antibacterial ointments.
Physiotherapy
In an integrated approach to the treatment of a disease such as venous dermatitis, physiotherapy plays a significant role . It acts on the body by enhancing physiological processes. This makes it possible to restore the vascular bed, increase the tone of the venous wall and capillaries, and eliminate edema. At the same time, there is no load on the liver and kidneys, which allows the body to recover faster.
There are many methods for influence. They are recommended by the doctor, taking into account the course of the disease and the individual characteristics of the patient’s body:
- Laser treatment. Exposure to radiation leads to cauterization of dilated veins.
- Pneumocompression. Helps to put pressure on the vessels in the direction of blood flow, stimulating the release of blood from stagnant places. Helps reduce swelling and improve local blood circulation.
- Ural Federal District. Under the influence of ultraviolet radiation, substances that stimulate vascular contraction are activated. After the procedure, pain disappears and inflammation decreases.
- Balneotherapy. The effects of therapeutic baths, combined with control of hydrostatic and temperature conditions, help to tone the vascular wall.
- Cryotherapy. In response to short-term cold effects in the body at the local level, vasoconstriction and dilation occur.
- UHF therapy uses high-frequency current, causing an increase in defenses, relieving pain and inflammation.
- Galvanization is based on the use of a weak current with a low frequency; the procedure is considered contact.
Contraindications to physiotherapeutic methods are the presence of neoplasms, high blood pressure, pregnancy and breastfeeding. Such treatment cannot be carried out in case of an active form of tuberculosis, acute inflammatory processes in the body, or impaired blood circulation in the brain.
Traditional methods
Traditional methods of treatment help only as a complement to general therapy . To improve venous outflow and normalize skin trophism, it is recommended to prepare a Kalanchoe tincture and use it to rub the affected areas. Take a 0.5 liter bottle, fill it with crushed raw materials and fill it with alcohol or vodka to the top. Leave for one week, shaking occasionally. Use within 4 months.
Garlic infusion helps improve the condition of the vascular bed. Pour 350 g of liquid honey into garlic gruel (250 g) and leave for one week. Take one tablespoon daily, before breakfast, lunch and dinner. Duration: two months.
Local therapy
This type of treatment involves the use of special creams, ointments, lotions and baths. They are especially effective in the initial stages of inflammation of the skin with varicose veins. Local preparations moisturize, soften and disinfect the affected area of the skin. It is also necessary to monitor the hygiene of problem areas of the skin. Wash the skin with neutral soap, dry with sterile wipes or cotton wool, treat with solutions of antiseptic and antimicrobial agents. The use of hormonal drugs helps relieve inflammation and reduce itching.
Complications
How dangerous is lipodermatosclerosis? Due to a lack of oxygen and nutrients, the skin undergoes necrosis, and ulcerative defects appear on the surface of the legs. They are not able to heal like normal, unaltered tissue. Without proper treatment, the ulcer may persist indefinitely.
The main function of the skin, the barrier, is disrupted. Pathogenic microorganisms penetrate unprotected tissues and infection occurs. Bacteria are capable of causing purulent inflammation, which leads to necrosis of deeper underlying tissues. This condition is called gangrene. Symptoms of necrosis: the skin is covered with dark green, dark brown and black spots, the tissue in these lesions is thin, does not bleed or hurt. This process cannot be stopped; the limb must be amputated.
If you start treating lipodermatosclerosis at the initial stages of development, eliminating its cause, you can avoid complications and keep your legs healthy.
ethnoscience
To begin treating inflammatory processes of the skin with traditional medicine, you must first consult a doctor. If the patient has injuries and deep ulcers, folk remedies can only worsen the situation. Traditional therapy suggests the use of natural ingredients, vegetable oils, tinctures of medicinal herbs, and plant juices. As a rule, decoctions are prepared from chestnut extract, grape leaves, chamomile and calendula flowers, oak bark, which have disinfectant, anti-inflammatory properties, and also heal wounds. Vegetable oils from almond, coconut or wheat germ moisturize problematic skin after hygiene procedures.
Preventive actions
Preventive measures for a very life-threatening complication of venous pathology are of great importance. Moderate physical activity helps to increase the tone of the muscles and veins of the legs: walking, running, swimming. Massages, contrast showers, and dousing with cool water will also be helpful. You should not constantly sit or lie down, as movement increases microcirculation and promotes wound healing. Wear comfortable shoes that fit your feet, choose clothes exclusively from natural fabrics, especially for eczema and ulcers.
Inflammation of the skin of the legs with varicose veins is chronic, lasts for years and leads to irreparable changes in the skin. If changes in the skin are noticed in time, the doctor will conduct competent and correct therapy, which will stop the inflammatory process and even eliminate small trophic ulcers.