When changing body position, a rapid heartbeat is often observed, and slight dizziness may even occur. Is this normal or is it possible that some kind of pathology is manifesting itself? In some cases, they talk about orthostatic tachycardia; whether this condition is dangerous can be understood after studying the thematic material.
Orthostatic tachycardia (OST) is one of the types of rhythm disturbances in which a characteristic symptom of tachycardia is determined - rapid heartbeat. Orthostatic pathology is called because signs of the disease appear during a person’s transition from a lying position to a sitting position.
Orthostatic tachycardia is not a universally accepted definition, therefore such a term is not present in the International Classification of Diseases, 10th revision. It is most often used in clinical practice by cardiologists.
The highest incidence of pathology is observed among convalescents, that is, patients recovering. OCT is especially common in those people who have not gotten out of bed for a long time. To find out why orthostatic tachycardia is dangerous, you should read the information provided in more detail.
Video Three tests for abnormal pulse. Live healthy!
Description of orthostatic tachycardia
The pathology develops as a result of a sharp transition from a horizontal to a vertical position. Rhythm disturbances can occur both in clinically healthy people and in patients bedridden for a long time. The occurrence of symptoms characteristic of an orthostatic test is associated with a sharp decrease in blood pressure due to a rapid change in body position, which contributes to a reflex increase in heart rate, that is, tachycardia.
With a one-time occurrence, orthostatic tachycardia is not capable of causing serious disorders, but with its frequent development, changes in the circulatory system can be observed. In particular, tachycardia leads to a shortening of the diastolic phase, which in turn contributes to less filling of the ventricles. This causes a decrease in cardiac and systolic volume, as a result of which the organs receive insufficient oxygen and nutrients.
Significant tachycardia causes disruption of coronary blood flow, which in turn harms the heart muscle.
Due to the shortened diastole during tachycardia, a disorder of biochemical processes is observed in the heart muscle, slowing down the process of myocardial recovery. The heart overworks faster, which makes it more susceptible to various destructive processes. If, in addition, the myocardium is affected by excess production of thyroxine in thyrotoxicosis or lack of oxygen in anemia, then heart failure can develop very quickly.
Severe tachycardia often causes:
- disorders of the functional activity of the heart;
- stagnation of blood in the venous system;
- decompensation of existing heart failure.
Therefore, any tachycardia, including orthostatic, poses a danger to human health, especially when it is extremely severe.
Orthostatic (postural) hypotension: causes, symptoms, diagnosis, treatment
Orthostatic (postural) hypotension is a sharp drop in blood pressure (most often more than 20/10 mmHg) when the patient assumes an upright position. Fainting, loss and confusion, dizziness, and blurred vision may occur within a few seconds or over a longer period. Some patients experience serial syncope. Physical activity or large meals can trigger such conditions. Most other manifestations are related to the underlying cause. Orthostatic hypotension is a manifestation of abnormal regulation of blood pressure due to various reasons, and not a separate disease.
Orthostatic hypotension occurs in 20% of older people. More often, it may be present in people with concomitant diseases, mainly arterial hypertension, and in patients who have been on bed rest for a long time. Many falls occur due to unrecognized orthostatic hypotension. Manifestations of hypotension are aggravated immediately after eating and stimulation of the vagus nerve (for example, after urination, defecation).
Postural orthostatic tachycardia syndrome (POTS), or so-called spontaneous postural tachycardia, or chronic or idiopathic orthostatic reaction, is a syndrome of pronounced tendency to orthostatic reactions at a young age. Standing up is accompanied by the appearance of tachycardia and various other symptoms (such as weakness, dizziness, inability to perform physical activity, clouding of consciousness), while blood pressure decreases by a very small amount or does not change. The cause of the syndrome is unknown.
Pathophysiology of orthostatic hypotension
Normally, gravitational stress due to rapid standing up leads to the movement of a certain volume of blood (from 0.5 to 1 l) into the veins of the lower extremities and torso. The subsequent transient decrease in venous return reduces cardiac output and hence blood pressure. The first manifestations may be signs of decreased blood supply to the brain. At the same time, a decrease in blood pressure does not always lead to brain hypoperfusion.
Baroreceptors of the aortic arch and carotid zone respond to arterial hypotension by activating autonomic reflexes aimed at restoring blood pressure. The sympathetic nervous system increases heart rate and myocardial contractility. Then the tone of the storage veins increases. At the same time, an increase in heart rate is caused by inhibition of parasympathetic reactions. If the patient continues to stand, activation of the renin-angiotensin-aldosterone system and secretion of antidiuretic hormone (ADH) occur, resulting in the retention of sodium and water ions and an increase in circulating blood volume.
Causes of orthostatic hypotension
The mechanisms for maintaining homeostasis may not be able to cope with the restoration of blood pressure in the event of disruption of the afferent, central or efferent link of autonomic reflexes. This can occur when taking certain medications, if myocardial contractility or vascular resistance are suppressed, with hypovolemia and dyshormonal conditions.
Symptoms of orthostatic tachycardia
In addition to palpitations, the main sign of tachycardia, patients may feel a number of other pathological changes:
- the head often feels “empty”;
- dizziness of varying severity;
- vision becomes blurred;
- when standing, weakness is very pronounced;
- nausea, headache;
- there may be fainting conditions.
During ORT, the same symptoms are often identified as with panic attacks, anxiety and somatization disorders. Therefore, orthostatic tachycardia is often associated with neurological diseases.
A characteristic sign of orthostatic tachycardia is that after moving to a vertical position, a person sways to the sides, as a result of which he can quickly sit down, even without fully straightening up, or faint. Immediately after this, the patient feels a strong heartbeat, which can quickly pass or, in more complex cases, continue for some time.
The severity of these symptoms depends on many factors. First of all, from the presence of organic heart pathology, which, against the background of frequently occurring tachycardia, can significantly worsen. The patient's condition is influenced by the presence of concomitant noncardiac pathology, thyrotoxicosis and pheochromocytoma have a particularly negative impact on health.
Video A girl with postural tachycardia syndrome was mistaken for an alcoholic
Causes of orthostatic tachycardia
The occurrence of orthostatic tachycardia has not yet been fully studied. Some scientists correlate the disease with postural tachycardia syndrome. Together with idiopathic hypovolemia and mitral valve prolapse, it is included in the orthostatic intolerance syndrome.
The main reasons contributing to the development of orthostatic tachycardia:
- Disturbance of sympathetic innervation of the lower extremities with preserved cardiac sympathetic innervation.
- Autonomic neuropathy, which can occur after infectious diseases or against the background of immune-dependent conditions.
- Changes in venous functions with simultaneous disruption of baroreflex activity.
Increased sympathetic activity is the main reason that most researchers are leaning towards today. Its role in the occurrence of OCT is explained by the fact that in a calm state an increased amount of arterial norepinephrine and an increased heart rate are detected.
Treatment methods
For such rhythm disturbances, in extreme cases, antiarrhythmic drugs are prescribed. Moreover, they are often ineffective. Therefore, the main thing in the treatment of orthostatic tachycardia is to identify the cause that caused it.
When palpitations occur due to thyrotoxicosis, methylthiouracil is used. Mercazolil, radioactive iodine-containing drugs. If the cause of the arrhythmia is heart failure, then digitalis is prescribed. Various heart defects and rheumatic carditis also provoke the development of orthostatic tachycardia and then reserpine and pyramidon are used.
According to various studies, the following drugs may be effective in the drug treatment of orthostatic tachycardia:
- Midodrine (belongs to adrenergic receptor antagonists).
- Propranolol (is a beta-blocker, start with small doses and gradually increase to 30 mg at a time).
Some researchers point to positive effects of rotary table testing, such as improved heart rate. But this method of treatment has not been fully studied.
Often used for neurogenic etiology of rhythm disturbances. First of all, this includes experienced stress, frequent anxiety, uncertainty and depression. It is prescribed only if, from a cardiological point of view, the patient is “all right.” That is, there are no significant disturbances in the functioning of the cardiovascular system and nothing else bothers the patient except the heartbeat.
In the process of psychotherapy, an individual approach is used, where all the issues that concern the patient are first clarified. Then, depending on the complexity of the situation, auto-training, positive psychotherapy, cognitive psychotherapy and other methods of influencing the patient’s psychological state are carried out.
If you follow medical recommendations, you can quickly recover from the discomfort. In the absence of organic heart damage, no consequences from the disease are observed.
Many people believe that only hypertension—high blood pressure—can threaten a person’s health. In fact, any deviation of systolic (upper) and diastolic (lower) pressure, including downward from the norm, is considered unfavorable. Hypotension occurs not only among people of retirement age, but also among young people.
People who care about their health are wondering what blood pressure is considered low. Normal values fluctuate within 110/70 mmHg. Art. up to 130/85 mm Hg. Art. Thus, for men and women from 16 to 20 years old, a blood pressure of 100-120/70-80 mmHg is considered normal. Art. From 20 to 40 years – 120-130/70-80 mm Hg. Art. In people aged 40 years and older, normal levels should not exceed 150/90 mmHg. Art.
Low blood pressure is considered to be 110-100/70-60 mmHg. Art. and below. Such indicators on a tonometer do not always indicate the development of hypotension. Thus, blood pressure decreases if a person does not eat enough or exercises intensively. You can notice this phenomenon after visiting a sauna or steam bath.
Why is low blood pressure dangerous? In fact, a temporary decrease in the numbers on the tonometer is not considered dangerous. In a healthy person, the indicators quickly return to normal, but it happens that they permanently remain low. If systolic pressure is below 100 mm Hg. Art., and diastolic - below 60 mm Hg. Art., we are talking about hypotension.
Can this condition threaten your health? For young people, hypotension is not considered dangerous, although the person experiences discomfort as a result of this pathology. However, for people over 60 years of age, the prognosis of the disease becomes more complicated. Low blood pressure can cause:
- cerebral ischemia;
- loss of consciousness.
These life-threatening conditions are caused by obstruction of blood circulation due to excessive vasodilation and slowing of blood flow. Due to a lack of oxygen and nutrients, necrosis of some parts of the brain develops, which is why an ischemic stroke occurs. Brain hypoxia can also cause fainting.
Causes
Hypotension has 2 types of progression - acute and chronic.
An acute decrease in pressure occurs due to cardiac dysfunction, intoxication, drug overdose, injuries accompanied by blood loss, as well as allergic reactions. In such cases, the injured person needs emergency medical care, because reduced vascular tone leads to the development of hypoxia of organs and tissues, which can lead to irreversible consequences.
Chronic hypotension can be a manifestation of normality or pathology.
- The physiological form of hypotension occurs in people who play sports professionally, as well as in residents of high mountains. Low blood pressure is considered normal, since it does not harm human health. With physiological hypotension, a person feels normal.
- Young women and adolescents of asthenic physique are susceptible to hypotension. Women's blood pressure drops during menstruation and pregnancy. This phenomenon is associated with changes in hormone production and blood loss and is considered normal.
In other cases, low blood pressure is an indicator of pathological processes in the body.
If hypotension is considered as an independent phenomenon, then it will be called primary. However, often permanently low numbers on the tonometer are a consequence of some disease - in this case, the disease will be secondary. Among the reasons that provoke too low blood pressure are:
- Diseases of the endocrine system: diabetes mellitus and dysfunction of the adrenal glands.
- Osteocondritis of the spine.
- Heart defects.
- Cirrhosis of the liver.
- Ulcers of the stomach or duodenum.
- Vegetative-vascular dystonia of the hypotonic type.
- Heredity.
- Stress, overwork, lack of sleep.
- Poor nutrition.
Types / photos of orthostatic tachycardia
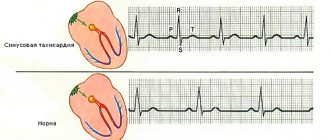
There are no specific forms and types of orthostatic tachycardia. The disease often manifests itself as a typical sinus tachycardia, which develops after the transition from a horizontal to a vertical body position.
Due to the development of orthostatic tachycardia, they are divided into primary and secondary. The former occur without visible influence factors, the latter are often associated with concomitant diseases.
Postural tachycardia: causes of health problems
With minor disturbances in the functioning of the autonomic nervous system, a person develops orthostatic tachycardia and an acceleration of the heart rate is observed. Pathology occurs when the body position changes.
The condition is common among patients during the recovery phase and in patients who have been lying down for a long time. the reason lies in neurological processes.
Treatment is required if the pathology becomes regular.
This type of tachycardia is not identified as a separate disease, so the term is not included in the International Classification of Diseases. But it is actively used by cardiologists in practice and refers to a wide range of characteristic symptoms.
Orthostatic tachycardia causes
People with an unstable autonomic nervous system often experience a strong acceleration of heart rate - orthostatic tachycardia.
This pathological condition often occurs when moving from a lying position to a standing position, and the heart rate greatly accelerates.
Almost all patients who have been in a lying position for a long time due to illness face this problem.
Diagnosis of orthostatic tachycardia
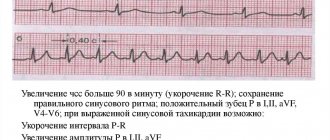
Patients suspected of having orthostatic tachycardia are first referred for rotary table testing. The standing method can also be used. A positive result is considered if the heart rate increases to 120 per minute in the first 10 minutes or the heart rate increases by 30 beats per minute. In this case, orthostatic hypotension should not occur.
Determination of norepinephrine in venous plasma is another diagnostic test for orthostatic tachycardia. The result is considered positive if up to 600 ng/ml norepinephrine is determined in a calm state.
Additional methods for examining patients for orthostatic tachycardia:
- echocardiography;
- stress echocardiography;
- Holter monitoring;
- laboratory tests (glucose, thyroid hormones, catecholamines).
It is important that all provoking tests are performed in a calm state in various body positions (lying, sitting, standing).
What is myocardial hypoxia and how does it manifest itself?
POTS is an increasingly recognized condition, particularly common in older women. POTS is characterized by orthostatic symptoms reflecting impaired orthostatic tolerance and occurring against the background of an excessive increase in heart rate (30 beats per minute or more) within five minutes of standing or in a rotating table test.
Heart rate after five minutes of standing usually exceeds 120 beats per minute. Although blood pressure does not decrease or decreases slightly when standing upright, patients experience various orthostatic symptoms: dizziness, fatigue, trembling, palpitations, nausea, vasomotor skin changes, hyperhidrosis, pain in the thoracic region.
Patients with POTS are often misdiagnosed as chronic fatigue syndrome, anxiety or panic disorder. Correct diagnosis of POTS is facilitated by a thorough history: symptoms regularly appear in an upright position and decrease after the patient lies down. In patients with orthostatic headache in the absence of signs of CSF leakage, POTS should also be excluded.
The causes of POTS remain unclear. Perhaps the syndrome occurs due to partial autonomic dysfunction, characterized by sympathetic denervation of the vessels of the lower extremities. Treatment includes increasing fluid and salt intake (to increase circulating blood volume), fludrocortisone, midodrine, α1-adrenergic agonists (which cause vasoconstriction), and measures to limit blood deposition in the vessels of the lower extremities.
The sudomotor axon reflex is based on the same mechanism as the cutaneous axon reflex, which mediates the spread of inflammation. The difference is that the excitation in this case spreads along the postganglionic sympathetic axons, which innervate the sweat glands and also belong to the C-fibers. The endings of these fibers are activated by local injection of acetylcholine, then the impulses go to the branch point, move to another branch of the axon and, spreading along it in the orthodromic direction, activate another sweat gland, releasing acetylcholine, which binds to the muscarinic M3-cholinergic receptor.
In other words, as a result of the sudomotor axon reflex, activation of some sweat glands leads to reflex activation of nearby glands. The resulting sweating can be measured quantitatively. The quantitative sudomotor test reliably reflects the state of postganglionic sympathetic sudomotor fibers.
Treatment and prevention of orthostatic tachycardia
Today there is no optimal way to treat orthostatic tachycardia. The exclusion of provoking factors has a positive effect on the dynamics of the disease:
- dehydration;
- prolonged immobilization;
- unbalanced diet.
Some patients on ORT benefit from saline infusions and mineralocorticoids. Rotary table testing also has a positive effect in some cases, but this method has not yet been used as a permanent therapy. During the course of research, the success of using adrenoreceptor agonists in the form of midodrine was determined.
Some studies used propranolol, which is a beta blocker. At first, small doses of the drug were prescribed and gradually increased to the optimal amount, for example, from 10 mg was increased to 30 mg 3-4 times a day.
3.78 avg. rating ( 76 % score) – 9 votes – ratings
How to treat?
There is no single treatment regimen for orthostatic tachycardia in medicine. Therefore, cardiologists focus on the individual condition of each patient. Firstly, exposure to harmful factors is excluded. It is very important to get a person out of the condition. During therapy, training is used on a rotary table, the loads are increased depending on the person’s condition. Secondly, the emphasis is on treating the primary disease, if any. In the most difficult cases, the cardiologist prescribes medications from the following groups:
Read also: Valerian for tachycardia