When is the diagnosis of “sinus tachycardia vertical position of the EOS” made?
The diagnosis of “sinus tachycardia with a vertical position of the EOS” is often found in children and adolescents.
It implies an acceleration of the rhythm in which the sinus node operates. An electrical impulse emanates from this area, initiating contraction of the heart and determining the speed of its work. Sinus tachycardia at this age is considered normal. Heart rate readings may exceed 90 beats per minute. In the absence of serious complaints and normal test results, this condition is not regarded as a manifestation of pathology.
https://www.youtube.com/watch?v=LBQbq78D3Wk
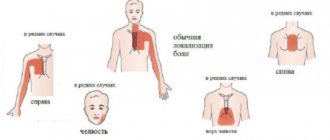
Tachycardia requires more serious consideration when it appears:
- various forms of shortness of breath;
- feeling of constriction in the chest area;
- chest pain;
- dizziness, fainting, low blood pressure (in cases where orthostatic tachycardia develops);
- panic attacks;
- increased fatigue and loss of performance.
Postural orthostatic tachycardia syndrome leads to an increase in heart rate when changing body position (suddenly standing up). This is often observed in people whose professional activities are associated with increased physical activity (general workers, loaders, storekeepers).
Possible long-term consequences of sinus tachycardia are heart failure and other diseases.
general information
Sinus arrhythmia implies a malfunction of the heart when the difference between heartbeats is more than 10% (if this figure is less, there is no pathology).
At the same time, the pulse remains within normal limits (60-80 beats per minute). Sinus arrhythmia must be present in a person, since in a calm state the heart beats moderately, and in response to excitement or during physical activity, the pulse quickens. It allows you to see the level of adaptation of the heart muscle to stress and is, within certain limits, a sign of good health.
A person’s heart cannot constantly beat in the same rhythm (like a clock), this indicates the depletion of its reserve abilities.
According to statistics, arrhythmias account for 10-15% of all heart diseases. In recent years, the number of cases has been growing. Sinus arrhythmia is most often observed in older people, as well as in those who abuse alcohol or drugs.
In children, sinus arrhythmia is present quite often, but in most cases it is not a pathology, since the nervous system simply cannot keep up with the growing body.
The disease does not require treatment if it develops against the background of severe nervous experiences. As soon as a person relaxes, it goes away on its own. To calm down in this case, you can use herbal remedies (valerian, motherwort).
Symptoms of the disease, especially in the early stages, do not appear clearly. A person may not realize that he has health problems for quite a long time.
What does the vertical position of the heart axis on an ECG mean?
When the EOS is in a vertical position, the S wave is most pronounced in leads I and aVL. ECG in children aged 7–15 years. Characterized by respiratory arrhythmia, heart rate 65-90 per minute. The position of the EOS is normal or vertical.
Regular sinus rhythm - this phrase means an absolutely normal heart rhythm, which is generated in the sinus node (the main source of cardiac electrical potentials).
Left ventricular hypertrophy (LVH) #8212; this is a thickening of the wall and/or an increase in the size of the left ventricle of the heart. All five position options (normal, horizontal, semi-horizontal, vertical and semi-vertical) occur in healthy people and are not pathological.
Specifics of the concept
There are several variations in the location of the cardiac electrical axis, and under some conditions its position changes. This does not in all cases indicate diseases and disorders. In a healthy human body, depending on the build and anatomy, the EOS deviates within 0...+90˚ (considered normal with a normal sinus rhythm of +30...+90).
Vertical EOS is noted when it is within the range of +70...+90˚. This is typical for tall people with a thin build (asthenics).
Intermediate types of addition are often found. Thus, the position of the cardiac electrical axis also changes; for example, it can become semi-vertical. Such displacements are not a pathology; they are typical for people with normal body functions.
Diagnosis of sinus tachycardia
Diagnosis of sinus tachycardia requires the use of various analytical techniques. It becomes mandatory to study the patient’s medical history and clarify information regarding the types of medications used by him in the past. Such moments make it possible to identify the presence of factors and circumstances that caused the onset of the disease.
- Physical examination of the patient, including examination of the condition of the skin, assessment of the degree of its oxygen saturation.
- Listening to breathing and heart rate (in some cases, with little physical activity).
- General and biochemical blood test to determine the level of leukocytes, cholesterol, potassium, glucose, urea.
- A urine test is necessary to exclude diseases of the genitourinary system from the list of suspected causes of pathology.
The state of the thyroid gland makes it possible to determine the degree of its influence on the heart rate. Vagal tests and daily monitoring are performed as additional diagnostic methods.
The most important method for diagnosing sinus tachycardia remains the cardiogram, which is based on recording electrical oscillations that occur during the work of the heart.
Consequences of displacement and their specificity
The displacement of the EOS is detected on the cardiogram. Consultation with a cardiologist and additional studies are required when the deviation goes beyond the normal range, which is set in the range from 0 to +90 degrees.
The processes and factors involved in the displacement of the heart axis, accompanied by severe clinical symptoms, require additional examinations without fail. Particular attention should be paid to circumstances when, with previously stable indicators of axis deviation, a change in the ECG suddenly occurs or sinus rhythm is disrupted. This is one of the symptoms of blockade.
In itself, EOS deviation does not require therapeutic measures; it is classified as a cardiac parameter that first requires determining the cause of its occurrence. Only a cardiologist decides whether treatment is necessary in each individual case.
ECG interpretation, vertical position of the EOS
Chronic diseases: not specified
Hello, I did an ECG at rest and with stress. What does this conclusion mean? ECG at rest: sinus rhythm with heart rate - 75v. Vertical position of the EOS. STIII, aVF below the isoline. ECG with stress: sinus tachyarrhythmia with heart rate 81-100v. Vertical position of the EOS. STIII, aVF below the isoline. I had an ECG done when I went to work, I don’t feel any pain, not at rest, not during physical activity, I can run 3 km with ease.
Tags: ECG interpretation sinus rhythm vertical position of EOS, ECG interpretation vertical position of EOS
Decoding ECG online Please help me decipher the ECG response. ECG at rest is standard.
Decoding ECG, sinus rhythm Good evening! My husband is 27 years old and received the result of an ecg.
Interpretation of ECG with stress I am undergoing VVC, contract renewal, military personnel. I did.
Interpretation of the ECG In the ECG dated September 19, 2014 it is written in the conclusion: ectopic atrial.
Decoding the ECG conclusion Please help me decipher the ECG, I am 26 years old. PR-133.
Deciphering the ECG of the heart online Please help me decipher the ECG of my husband, he is 45.
ECG of the heart, respiratory arrhythmia I’m going through the IVK at the VV of the Ministry of Internal Affairs, I’m worried about the ECG, the initial ECG.
Interpretation of ECG upon admission to SVU My son is preparing to enter the Suvorov military.
Decoding ECG in children online My child is 2.4 years old, the doctors said that he has a noise.
Decoding ecg. Please help. Help me decipher the ecg. Baby 3 months old. Is that all.
Please decipher the cardiogram. Please tell me what sinus rhythm means.
Tachycardio Please help me decipher the ECG conclusion. at rest: sinus rhythm.
1 answer
Don't forget to rate the doctors' answers, help us improve them by asking additional questions on the topic of this question. Also don't forget to thank the doctors.
Hello! At this age there should be no heart problems; such changes are more like science fiction. Perhaps they are related to your body type (not thin as far as I understand). And since the initial deviations from the norm do not change during physical activity, I am inclined to believe that you do not have an organic heart pathology.
ECG formulation
The conclusion of the ECG may include the following wording: “Vertical EOS, sinus rhythm, heart rate per minute. – 77” – this is normal. It should be noted that the concept of “rotation of the EOS around an axis”, the mark of which may be in the electrocardiogram, does not indicate any violations. Such a deviation in itself is not regarded as a diagnosis.
There is a group of ailments that differ precisely in the vertical sinus EOS: various types of cardiomyopathy, especially in the dilated form; ischemia; congenital abnormalities; chronic heart failure.
With these pathologies, a violation of the sinus rhythm of the heart occurs.
Treatment of sinus tachycardia in children
In uncomplicated cases of sinus tachycardia, changes in the patient's diet and lifestyle are sufficient. You will need to minimize the presence of spicy and excessively salty dishes on the menu, give up strong tea and coffee, alcohol, and chocolate. Walking in the fresh air without intense physical activity is beneficial.
If there is a need for therapeutic treatment, medications are selected based on the reasons for the development of the pathology. Various specialists are involved in drawing up a treatment plan - a cardiologist, an endocrinologist, a phlebologist, a vascular surgeon.
Traditionally, therapy is carried out with the appointment:
- beta-blockers (Bisoprolol, Metoprolol);
- non-dihydropyridine calcium antagonists (Verapamid, Diltiazem);
- drugs that suppress the synthesis of thyrotropin (Metizol, Carbimazole);
- sedatives (tinctures of motherwort, Persen, valerian extract).
In the case of diagnosing highly symptomatic sinus tachycardia, it becomes advisable to use surgical treatment methods - radiofrequency catheter ablation of the sinus node with the installation of a permanent pacemaker.
Sinus tachycardia in children is characterized by an increase in heart rate by 10–60%. This pathology occurs very often in children of preschool and school age. It is not a life-threatening condition and in most cases goes away on its own and does not require treatment.
A rapid heartbeat is normal in young children. The heart rate can increase as a result of physical activity (running, swimming, jumping, etc.), emotional experiences, and in the presence of infectious and viral diseases characterized by elevated body temperature.
However, when exposed to the above factors, the heart rhythm returns to normal after a few minutes of rest. In infectious and viral diseases, the heart rate returns to normal after the body temperature decreases. Such conditions do not indicate the presence of sinus tachycardia, although parents very often confuse them with this pathology.
The main symptoms of sinusoidal tachycardia in a child are:
- cardiopalmus;
- dizziness;
- darkening of the eyes;
- temporary loss of consciousness;
- dyspnea;
- pain in the chest area.
Only if these symptoms are present can it be said that the child has sinus tachycardia.
The reasons for the development of sinus tachycardia in children of different age categories are different. For example, in newborn children, the automatism of the sinus node is increased, so an increase in the heart rate in infants is considered normal, but only if it lasts a short period of time (it goes away on its own within 1 - 2 months).
If in a newborn child tachycardia does not go away on its own for a long time, then there is a possibility of disturbances in myocardial metabolism. The following reasons may also cause increased heart rate:
- physiological (overheating, hypothermia, prolonged crying, anxiety, etc.);
- dysfunction of the central nervous system;
- congenital heart pathologies.
At school age, the reasons for the development of sinus tachycardia are completely different. These include:
- emotional experiences;
- physical stress;
- physiological characteristics of a growing organism (puberty, rapid growth, first menstruation in girls, etc.);
- endocrine diseases;
- Iron-deficiency anemia;
- disorders of the cardiovascular system, etc.
All therapeutic measures aimed at eliminating the pathology are prescribed individually, depending on the root cause that triggered the development of the disease and the age of the patient.
https://www.youtube.com/watch?v=u0cH2ODgfXw
In cases where the cause of the development of pathology is anemia, iron-containing medications are prescribed. If an increase in heart rate provokes an increase in body temperature, it is important to take antipyretic drugs.
In other cases, there may be no treatment for tachycardia at all, even with a disease such as hyperthyroidism. The heart rate will be completely normalized only when the thyroid gland begins to produce hormones at the required level, and not exceeding it.
If the appearance of sinus tachycardia is associated with an emotional state, it is recommended to take sedatives. It is also possible to use traditional medicine. Taking herbal tinctures that have a calming effect have a beneficial effect on the nervous system.
In 80% of cases, this pathology resolves without undergoing special courses of treatment. Parents should constantly monitor their child's weight, as excess fat increases the load on the heart.
If sinus tachycardia is observed in a child during adolescence, you should monitor his diet and exclude drinks containing caffeine (tea, coffee, cocoa), as well as spicy, fried and highly fatty foods.
If the doctor insists on taking certain medications, then it is better to listen to him. Since, despite the fact that sinus tachycardia is not a serious disease, it can cause the development of heart failure, which will affect the child’s quality of life in the future.
Seizures may occur differently in each child. Some people simply experience slight dizziness and increased heart rate, while others experience all the symptoms of sinus tachycardia (see above).
If a child has a seizure, he must be given first aid. To do this, you need to free the chest (unfasten buttons or even remove clothes from the upper torso) and bring the child to the open window. You need to ask the child to take a deep breath and hold it as long as possible. This should help reduce the frequency of contractions.
If the patient’s condition does not improve after a few minutes, you need to call an ambulance.
Early ventricular repolarization syndrome
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day.
For the first time, such an electrocardiographic phenomenon as early ventricular repolarization syndrome was discovered in the middle of the 20th century. For many years, it was considered by cardiologists only as an ECG phenomenon that does not have any effect on the functioning of the heart. But in recent years, this syndrome has begun to be increasingly detected in young people, adolescents and children.
According to world statistics, it is observed in 1-8.2% of the population, and the risk group includes patients with heart pathologies, which are accompanied by cardiac disorders, patients with dysplastic collagenosis and dark-skinned men under 35 years of age. It was also revealed that this ECG phenomenon is detected in most cases in people who are actively involved in sports.
Our readers successfully use ReCardio to treat hypertension. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
A number of studies have confirmed the fact that early ventricular repolarization syndrome, especially if it is accompanied by episodes of syncope of cardiac origin, increases the risk of sudden coronary death. Also, this phenomenon is often combined with the development of supraventricular arrhythmias, deterioration of hemodynamics and, with progression, leads to heart failure. That is why early ventricular repolarization syndrome has attracted the attention of cardiologists.
In our article we will introduce you to the causes, symptoms, methods of diagnosis and treatment of early ventricular repolarization syndrome. This knowledge will help you to adequately identify it and take the necessary measures to prevent complications.
What is early ventricular repolarization syndrome?
This ECG phenomenon is accompanied by the appearance of the following uncharacteristic changes in the ECG curve:
- pseudocoronary elevation (elevation) of the ST segment above the isoline in the chest leads;
- additional J waves at the end of the QRS complex;
- shift to the left of the electrical axis.
Based on the presence of concomitant pathologies, early repolarization syndrome can be:
- with damage to the heart, blood vessels and other systems;
- without damage to the heart, blood vessels and other systems.
According to its severity, the ECG phenomenon can be:
- minimal – 2-3 ECG leads with signs of the syndrome;
- moderate – 4-5 ECG leads with signs of the syndrome;
- maximum – 6 or more ECG leads with signs of the syndrome.
In terms of its persistence, early ventricular repolarization syndrome can be:
- permanent;
- transient.
While cardiologists do not know the exact cause of the development of early ventricular repolarization syndrome. It is detected both in absolutely healthy people and in persons with various pathologies. But many doctors identify some nonspecific factors that may contribute to the appearance of this ECG phenomenon:
- overdose or long-term use of adrenergic agonists;
- dysplastic collagenoses, accompanied by the appearance of additional chords in the ventricles;
- congenital (familial) hyperlipidemia, leading to atherosclerosis of the heart;
- hypertrophic obstructive cardiomyopathy;
- congenital or acquired heart defects;
- hypothermia.
Research is currently underway on the possible hereditary nature of this ECG phenomenon, but so far no data on a possible genetic cause have been identified.
The pathogenesis of early ventricular repolarization is the activation of additional abnormal pathways that transmit electrical impulses and disruption of the conduction of impulses along the pathways that are directed from the atria to the ventricles. The notch at the end of the QRS complex is a delayed delta wave, and the shortening of the PQ interval observed in most patients indicates activation of abnormal nerve impulse transmission pathways.
In addition, early ventricular repolarization develops due to an imbalance between depolarization and repolarization in the myocardial structures of the basal sections and apex of the heart. With this ECG phenomenon, repolarization becomes significantly accelerated.
Cardiologists have identified a clear relationship between early ventricular repolarization syndrome and nervous system dysfunction. When carrying out dosed physical activity and a drug test with Isoproterenol, the patient experiences normalization of the ECG curve, and during night sleep the ECG indicators worsen.
Also during the tests it was revealed that early repolarization syndrome progresses with hypercalcemia and hyperkalemia. This fact indicates that electrolyte imbalance in the body can provoke this ECG phenomenon.
This ECG phenomenon can exist for a long time and not cause any symptoms. However, this background often contributes to the occurrence of life-threatening arrhythmias.
Many large-scale studies have been conducted to identify the specific symptoms of early ventricular repolarization, but all of them have been inconclusive. ECG abnormalities characteristic of the phenomenon are detected both in absolutely healthy people who do not make any complaints, and among patients with cardiac and other pathologies who make complaints only about the underlying disease.
In many patients with early ventricular repolarization, changes in the conduction system provoke various arrhythmias:
- ventricular fibrillation;
- ventricular extrasystole;
- supraventricular tachyarrhythmia;
- other forms of tachyarrhythmias.
Such arrhythmogenic complications of this ECG phenomenon pose a significant threat to the health and life of the patient and often provoke death. According to world statistics, a large number of deaths caused by asystole during ventricular fibrillation occurred precisely against the background of early ventricular repolarization.
Half of the patients with this syndrome have systolic and diastolic cardiac dysfunction, which leads to central hemodynamic disturbances. The patient may develop shortness of breath, pulmonary edema, hypertensive crisis, or cardiogenic shock.
The syndrome of early ventricular repolarization, especially in children and adolescents with neurocirculatory dystonia, is often combined with syndromes (tachycardial, vagotonic, dystrophic or hyperamphotonic) caused by the influence of humoral factors on the hypothalamic-pituitary system.
ECG phenomenon in children and adolescents
In recent years, the number of children and adolescents with early ventricular repolarization syndrome has been increasing. Despite the fact that the syndrome itself does not cause significant heart problems, such children must undergo a comprehensive examination, which will identify the cause of the ECG phenomenon and possible concomitant diseases. For diagnosis, the child is prescribed:
Read also: Medicine for cardiac arrhythmia concor
In the absence of heart pathologies, drug therapy is not prescribed. The child's parents are advised to:
- clinical observation by a cardiologist with ECG and ECHO-CG once every six months;
- eliminate stressful situations;
- limit excessive physical activity;
- Enrich your daily menu with foods rich in heart-healthy vitamins and minerals.
If arrhythmias are detected, the child, in addition to the above recommendations, is prescribed antiarrhythmic, energy-tropic and magnesium-containing drugs.
Diagnostics
Electrocardiography is the main method for diagnosing early ventricular repolarization syndrome.
The diagnosis of “early ventricular repolarization syndrome” can be made on the basis of an ECG study. The main signs of this phenomenon are the following deviations:
- displacement above the isoline by more than 3 mm of the ST segment;
- prolongation of the QRS complex;
- in the chest leads, simultaneous leveling of the S wave and increase in the R wave;
- asymmetrical high T waves;
- shift to the left of the electrical axis.
For a more detailed examination, patients are prescribed:
- ECG with physical and drug stress;
- 24-hour Holter monitoring;
- ECHO-KG;
- urine and blood tests.
Once early repolarization syndrome is identified, patients are advised to continually provide their physician with past ECG results, as ECG changes may be mistaken for an episode of coronary artery disease. This phenomenon can be distinguished from myocardial infarction by the consistency of characteristic changes in the electrocardiogram and the absence of typical radiating chest pain.
If early repolarization syndrome is detected, which is not accompanied by heart pathologies, the patient is not prescribed drug therapy. It is recommended for such people:
- Avoiding intense physical activity.
- Prevention of stressful situations.
- Introduction to the daily menu of foods rich in potassium, magnesium and B vitamins (nuts, raw vegetables and fruits, soy and sea fish).
If a patient with this ECG phenomenon has cardiac pathologies (coronary syndrome, arrhythmias), then the following medications are prescribed:
- energy-tropic agents: Carnitine, Kudesan, Neurovitan;
- antiarrhythmic drugs: Ethmozin, Quinidine sulfate, Novocainamide.
If drug therapy is ineffective, the patient may be recommended to undergo minimally invasive surgery using catheter radiofrequency ablation. This surgical technique eliminates the bundle of abnormal pathways that cause arrhythmia in early ventricular repolarization syndrome. Such an operation should be prescribed with caution and after eliminating all risks, since it may be accompanied by severe complications (PE, damage to the coronary vessels, cardiac tamponade).
In some cases, early ventricular repolarization is accompanied by repeated episodes of ventricular fibrillation. Such life-threatening complications become the reason for an operation to implant a cardioverter-defibrillator. Thanks to progress in cardiac surgery, the operation can be performed using a minimally invasive technique, and implantation of a third-generation cardioverter-defibrillator does not cause any adverse reactions and is well tolerated by all patients.
Detection of early ventricular repolarization syndrome always requires complex diagnostics and follow-up with a cardiologist. Compliance with a number of restrictions in physical activity, correction of the daily menu and exclusion of psycho-emotional stress is indicated for all patients with this ECG phenomenon. When concomitant pathologies and life-threatening arrhythmias are identified, patients are prescribed drug therapy to prevent the development of severe complications. In some cases, the patient may be indicated for surgical treatment.
Left ventricular hypertrophy on the ECG: recommendations from a cardiologist The left ventricle is the part of the heart, during the contraction of which blood is ejected into the aorta. This is the main chamber of the heart, providing blood flow throughout the organ...
Ventricular extrasystoles: causes, signs, treatment Ventricular extrasystoles (VES) are extraordinary contractions of the heart that occur under the influence of premature impulses that originate from the intraventricular...
Right atrial hypertrophy: causes, symptoms, diagnosis Right atrial hypertrophy (RAH) is a term that refers to the enlargement of this part of the heart. Let us remember that venous blood enters the right atrium...
How to decipher a cardiogram of the heart? The formation of a conclusion on an electrocardiogram (ECG) is carried out by a functional diagnostics doctor or cardiologist. This is a difficult diagnostic process,...
Help from traditional medicine
The following are the safest folk recipes for tachycardia.
The process of preparing a “medicine” from nuts (Brazil) and dried fruits will require combining 2 tbsp. l. main components, dried apricots, figs, raisins, hazelnuts. The ingredients are thoroughly ground in a blender and 300 ml of natural honey is poured in. The composition is taken 1 tsp. three times a day for a 3-week course. If you are obese and have problems with the thyroid gland, it is better to avoid the product.
The lemon-garlic mixture contains 10 peeled heads of garlic, 10 diced and peeled citrus fruits. The components are mixed in a blender, liquid honey is added. After thorough mixing, store in a dark place for at least 1 week. Next, take 1 dessert spoon 4 times during the day. The course lasts 1 month.
Hawthorn infusion
A tablespoon of dried hawthorn flowers is poured with an incomplete glass of boiling water and left for at least half an hour. The infusion is drunk three times a day, 100 ml, regardless of meals. The recommended duration of treatment is 1–3 months.
Sinus tachycardia often requires an integrated approach to treatment. To obtain positive results from therapy, the patient will need to follow all medical prescriptions and recommendations, give up bad habits, and control his physical activity. If you maintain a sedentary lifestyle, smoking, consuming high-calorie foods, alcohol, the effectiveness of even the most professional treatment, as well as the best folk methods, will significantly decrease.
Treatment tactics
Treatment should be strictly under the supervision of a specialist. Basic techniques:
- healthy balanced diet (refusal of coffee, strong tea, alcohol, fatty and sweet foods);
- to give up smoking;
- drug treatment (sedatives, tranquilizers, antiarrhythmic drugs);
- installation of a pacemaker (for severe disease);
- surgery;
- traditional medicine (only together with the main treatment and with the permission of a doctor): treatment with asparagus, lemons, walnuts and honey, hawthorn;
- treatment with leeches.
How to treat sinus arrhythmia in each individual case is determined by the attending physician.
Rehabilitation after an attack of sinus arrhythmia consists of receiving medical care, which will be aimed at restoring the heart rhythm (drug or electrical stimulation), ensuring the most calm conditions.
The patient himself must adhere to a healthy lifestyle (balanced diet and giving up bad habits), and reasonably limit physical activity.
Sinus arrhythmia does not require special treatment. An incorrect rhythm does not mean that you have any of the listed diseases. Heart rhythm disturbances are a common syndrome characteristic of any age.
By giving up smoking and alcohol, doping and energy drinks, excessive physical or psycho-emotional stress, a person can avoid adverse cardiac abnormalities and achieve normal levels.
A proper diet, daily routine, and lack of stress can greatly help to avoid heart problems. It would be useful to take vitamins to maintain heart function and improve the elasticity of blood vessels. In pharmacies you can find a large number of complex vitamins containing all the necessary components and specialized vitamins to maintain the functioning of the heart muscle.
In addition to them, you can enrich your diet with foods such as oranges, raisins, blueberries, beets, onions, cabbage, and spinach. They contain many antioxidants that regulate the number of free radicals, an excessive amount of which can cause myocardial infarction.
For the smooth functioning of the heart, the body needs vitamin D, which is found in parsley, chicken eggs, salmon, and milk.
If you plan your diet correctly and adhere to a daily routine, you can achieve long and uninterrupted functioning of the heart muscle and not worry about it until you are very old.
Cardiography
The concept of “cardiography” combines different methods of studying cardiac activity. Electrocardiography has become widespread, with the help of which electrical signals are recorded.
cardiac activity. Such cardiography of blood vessels and the heart makes it possible to evaluate the blood supply to the myocardium, conductivity and heart rhythm, changes in the size of the heart cavities, thickening of the heart muscle, identify electrolyte imbalances, the duration of the infarction, and toxic damage to the myocardium.
The activity of the heart is recorded from the surface of the patient’s body (electrodes are attached to the chest, legs and arms). The results of cardiography of the vessels and heart are recorded for 5-10 minutes. The result of such a diagnosis is a cardiogram of the heart, according to which the attending physician - therapist, cardiologist or other specialist can analyze the patient’s condition.
Indications for cardiography are pain, discomfort in the heart, neck, back, abdomen, chest (this is how ischemia manifests itself in some cases), shortness of breath, frequent fainting, swelling of the legs, high blood pressure, heart murmurs, rheumatism, diabetes, stroke.
A cardiogram is prescribed to patients in preparation for surgery, during preventive annual examinations, pregnancy, when completing documentation before being assigned to health institutions and sports sections, etc.
In addition, people over 40 years of age are recommended to have a heart cardiogram performed annually, despite the absence of complaints. This is the only way to detect hidden heart rhythm disturbances, ischemia, and heart attack in a timely manner.
Only a specialist can take a cardiogram, decipher the data obtained and, if necessary, prescribe appropriate treatment. But patients themselves can understand some terms that are important for decoding the cardiogram:
- heart rate (HR). The indicator displays the number of contractions of the heart muscle per minute. If the contractions are more than 91 per minute, this is tachycardia, if 59 beats or less is bradycardia. The normal heart rate for an adult is 60-90 beats.
- Electrical axis of the heart (EOS). This indicator, obtained using cardiography, helps to understand the location of the heart and determine the functions of its different parts. The cardiac cardiogram can indicate normal, horizontal, vertical, and deviated to the left or right position of the EOS.
- Regular sinus rhythm. This is the name given to the normal heart rhythm, which is set by the sinus node.
- Non-sinus rhythm. This formulation in the heart cardiogram indicates that the heart rhythm is not set by the sinus node, but by some secondary source of electrical cardiac potentials, which in turn indicates heart pathology.
- Sinus arrhythmia (irregular sinus rhythm). This term means that the cardiograph shows an abnormal sinus rhythm with a gradual decrease and increase in heart rate. Such arrhythmia can be non-respiratory and respiratory.
- Atrial fibrillation or atrial fibrillation. A similar conclusion from cardiography of blood vessels and the heart suggests that there is some disturbance of heart rhythm, most often found in patients after 60 years of age, occurring without obvious symptoms and often provoking heart failure and cerebral stroke.
- Paroxysm of atrial fibrillation. This is the name given to a sudden attack of atrial fibrillation detected on cardiography. This condition requires immediate treatment and the sooner it is started, the greater the likelihood of restoring normal heart rhythm.
- Atrial flutter. A type of arrhythmia that is more difficult to treat than classic arrhythmia.
- Extrasystole or extrasystole. This is what is called in a cardiac cardiogram an extraordinary contraction of the heart muscle, causing an abnormal impulse. Extrasystole can be ventricular, atrioventricular and atrial - depending on the part of the heart from which such an impulse originates.
- Wolff-Parkinson-White syndrome (WPW). A congenital pathology characterized by abnormal electrical impulses and dangerous attacks of arrhythmia.
- Sinoatrial block. Such wording in the transcript of the cardiogram indicates disturbances in the conduction of impulses to the atrial myocardium from the sinus node. This pathology often occurs with cardiosclerosis, cardiopathy, myocarditis, heart attack, overdose of potassium drugs, beta-blockers, cardiac glycosides, after heart surgery.
- Atrioventricular block. This is a pathology of the passage of impulses from the atria to the cardiac ventricles, detected on cardiography. This disorder is provoked by asynchronous contraction of the ventricles and atria of the heart.
- Complete, incomplete blockade of the bundle branches. Impairment of impulse conduction in the thickness of the myocardium of the ventricles of the heart. This deviation manifests itself in heart defects, cardiosclerosis, myocarditis, heart attack, myocardial hypertrophy, and high blood pressure.
- Left/right ventricular hypertrophy. This is the name for an increase in the size of the ventricle or thickening of its wall.
- Scarring. Cardiography with such a conclusion suggests that the patient suffered a heart attack in the past. In this case, preventive treatment is prescribed to prevent relapse and eliminate the cause of the blood supply disorder.
- Prolonged QT interval. In the interpretation of the cardiogram, this is an acquired or congenital disorder of cardiac conduction, which is accompanied by fainting, rhythm disturbances, and cardiac arrest.
During the examination, a cardiogram is often prescribed for children, but it should be taken into account that their cardiography indicators differ from those of adults. For children under one year old, fluctuations in heart contractions depending on their behavior are typical. Their average contraction frequency is 138 beats, the EOS is vertical.
Cardiography of children 1-6 years old displays a vertical, normal and sometimes horizontal location of the EOS, a contraction frequency of 128 beats, and sinus respiratory arrhythmia is often detected. A cardiogram of the heart of children 7-15 liters indicates that the normal heart rate is 65-90 beats, the position of the EOS is vertical or normal, and respiratory arrhythmia is characteristic.
15.07. | Admin | View 66 | Comm. x | Category: Hits
Copying without a link to the site is prohibited!
Normal location of the EOS and reasons for its displacement
The electrical axis of the heart is a concept that reflects the electrical processes in this organ. The direction of the EOS shows all the bioelectric changes in total that occur during the work of the heart muscle. During the recording of an electrocardiogram, each electrode records the bioelectric reaction in a strictly designated part of the myocardium. Then, to calculate the position and angle of the EOS, doctors represent the chest in the form of a coordinate system in order to subsequently project the indicators of the electrodes onto it. Horizontal position of the EOS, vertical and a number of other options are possible.
The importance of the cardiac conduction system for EOS
The conduction system of the heart muscle is atypical muscle fibers that connect different parts of the organ and help it contract synchronously. Its beginning is considered to be the sinus node, located between the mouths of the vena cava, so in healthy people the heart rate is sinus. When an impulse occurs in the sinus node, the myocardium contracts. If the conduction system malfunctions, the electrical axis changes its position, since this is where all the changes occur before the contraction of the heart muscle.
Axis directions and offset
Since the weight of the left ventricle of the heart muscle in completely healthy adults is greater than the right, all electrical processes occur there more strongly. Therefore, the axis of the heart is directed towards it.
- Normal position. If we project the location of the heart onto the expected coordinate system, then the direction of the left ventricle from +30 to +70 degrees will be considered normal. But it depends on the characteristics of each person, so the norm for this indicator for different people is considered to be a range from 0 to +90 degrees.
- Horizontal position (from 0 to +30 degrees). Displayed on the cardiogram in short people with a wide sternum.
- Vertical position. EOS ranges from +70 to +90 degrees. It is observed in tall people with a narrow chest.
There are diseases in which the axis shifts:
- Deviation to the left. If the axis deviates to the left, this may indicate enlargement (hypertrophy) of the left ventricle, which indicates its overload. This condition is often caused by arterial hypertension that lasts for a long time, when blood has difficulty passing through the vessels. As a result, the left ventricle works harder. Deviation to the left occurs with various blockades and lesions of the valve apparatus. With progressive heart failure, when the organ cannot fully perform its functions, the electrocardiogram also records a shift of the axis to the left. All these diseases force the left ventricle to work harder, so its walls become thicker, the impulse through the myocardium passes much worse, the axis deviates to the left.
- Offset to the right. Deviation of the electrical axis of the heart to the right most often occurs when the right ventricle is enlarged, for example, if a person has heart disease. This may be cardiomyopathy, coronary disease, structural abnormalities of the heart muscle. Right deviation is also caused by problems with the respiratory system such as pulmonary obstruction and bronchial asthma.
EOS norm indicators
Age ECG indicators Axis direction Heart rate per minute
| A child from birth to one year. | Vertical. | 60–150 beats. |
| Children from one to 6 years old. | Vertical is normal, sometimes horizontal. | 95–128 beats. |
| Children and adolescents aged 7 to 15 years. | Normal or vertical. | 65–90 beats. |
| Adults. | Normal. | 60–90 beats, regular sinus rhythm. |
So, in healthy people, the direction of the heart axis can be normal, horizontal, vertical, and the heart rhythm can be regular sinus. If the rhythm is not sinus, then this indicates some kind of disease. Irregular sinus rhythm is an indicator of the disease if it persists during breath holding. A shift of the cardiac axis to the left or right may indicate problems with the heart and respiratory system. In no case should the diagnosis be made solely on the basis of EOS displacement. A cardiologist can determine the disease and prescribe treatment after a series of additional studies.
Finding the nearest clinic Find the clinic closest to your home in your city
Top
asosudy.ru
Sinus tachycardia vertical position of the EOS. Incomplete bdocade of the right…
Sinus tachycardia vertical position of the EOS. Incomplete bdocade of the right bundle branch.
The pulse is generally 80 or higher beats per minute. The feeling of heart beating is slipping, and sometimes it is compressing; there is not enough air for 1.2 seconds. Then it releases and again the feeling of a pulsating heart.
Hello. I am 16 years old. I have been suffering from VSD for a long time, and a couple of days ago I had a panic attack, after it passed, I felt strange sensations in my head: heaviness, noise in my head, something pressing in my ears, nausea, lethargy. This lasted 1.5 days. Now again I feel lethargic, depressed, and pain in my head when I move it.
Good afternoon Please tell me, is it possible to give a 4.5 month old child tanakan solution (0.3 ml 2 times a day) and magnesium b6 (1 ml 1 time a day) for a month? It is confusing that tanakan is an alcohol-based medicine for adults, and magnesium b6, as described, is not suitable for infants.
When the electrical axis is shifted to the left side, the left ventricle and its myocardium are hypertrophied (LVH). This is the most common specificity of the deviation. This pathology acts as an additional symptom, rather than independently, and indicates an overload of the ventricle and a change in the process of its work.
These problems appear with prolonged arterial hypertension.
The disorder is accompanied by a significant load on the vessels delivering blood to the organ, so contractions of the ventricle occur with excessive force, its muscles increase and hypertrophy. The same is observed with ischemia, cardiomyopathy, etc.
The left location of the electrical axis and LVH is also observed with disorders of the valve system, while the sinus rhythm of contractions is also disrupted. The pathology is based on the following processes:
- aortic stenosis, when the exit of blood from the ventricle is difficult;
- weakness of the aortic valve, when some of the blood flows back into the ventricle and overloads it.
The designated disorders are acquired or congenital. Often the cause of the former is rheumatism. Changes in ventricular volume are also observed in people who are professionally involved in sports. It is highly recommended that they consult a doctor to determine whether physical activity will cause irreparable harm to their health.
Deviation to the left is also detected when conduction inside the ventricle is impaired, during blockade disorders in the heart.
Hypertrophic processes of the right ventricle (RVH) accompany the right deviation of the EOS. The right side of the heart is responsible for sending blood to the lungs, where it is supplied with oxygen. RPG is characteristic of pathologies of the respiratory system: asthma, chronic obstructive processes in the lungs. If the disease lasts for a long time, this causes hypertrophic changes in the ventricle.
Other causes of the pathology are the same as for the left deviation: ischemia, abnormal rhythm, chronic heart failure, cardiomyopathy and blockade.
Left position
If the electrical axis is shifted to the left, the left ventricle and myocardium are hypertrophied (LVH). This type of violation is the most common. This pathology has the meaning of additional symptoms, not independent, it indicates an overload of the ventricle, a change in its working process.
The listed disorders occur with prolonged arterial hypertension. The pathology is accompanied by a strong load on the vessels that deliver blood to the organ, so ventricular contractions occur very strongly, its muscles increase in size and hypertrophy. The same process is observed in cardiomyopathy, ischemia, etc.
Left localization of the electrical axis, LVH are also diagnosed with defects in the valve system, and the sinus rhythm of contractions is disturbed. Pathology is based on the following processes:
- a weak aortic valve, with some of the blood returning back to the ventricle, overloading it;
- aortic stenosis, which makes it difficult for blood to exit the ventricle.
The listed disorders are congenital or acquired. Often the cause of the latter is rheumatism suffered by the patient. Changes in ventricular volume are observed in people who play sports professionally. Such patients are strongly recommended to consult a specialist in order to determine whether physical activity is harmful to health.
Deviation of the vertical position of the EOS and sinus rhythm are also detected with conduction defects in the ventricle and with heart blockades.
Subacute stage of pericarditis. Example of an ECG for pericarditis
Electrocardiography: what the ECG result will tell you
Extrasystoles are usually felt as interruptions in the heart. About tachycardia when moving to a vertical position many times.
In 1 minute (tachycardia). Vertical position of the sinus axis of the heart. Diagnostic changes in the myocardium of the left ventricle (most likely).
The vertical position of the electrical axis of the heart is 72 degrees. Tachycardia can occur both with illness and with excitement and physical activity.
In practically healthy individuals, even pronounced tachycardia is not always the case. Palpitation when the patient moves from a vertical position to.
When the heart rate increases above 91 beats/min, they speak of tachycardia; if heart rate. Allows you to roughly determine the location of the heart in the chest. Thin people usually have a vertical position of the EOS, while thick people.
They can also be caused by damage to the heart muscle. It is difficult to detect with tachycardia (heart rate more than 90 V. In an upright position of the patient, as well as after physical activity).
Leningrad blockade
Description and characteristics
Determination of EOS is a diagnostic method that displays the electrical parameters of the heart. The value that determines the position of the electrical axis of the heart is a summarized indicator of the bioelectric processes that occur during heart contractions. In cardiac diagnostics, the direction of the EOS is important.
The heart is an organ with a three-dimensional structure and volume. Its position in medicine is represented and determined in a virtual coordinate grid. Atypical myocardial fibers intensively generate electrical impulses during their work. This is a complete system that conducts electrical signals. It is from there that electrical impulses originate, causing the movement of parts of the heart and determining the rhythm of its work. In a split second before contractions, electrical changes appear, forming the EOS value.
The heart is an organ with a three-dimensional structure and volume. This is a complete system that conducts electrical signals.
EOS parameters, sinus rhythm is shown by a cardiogram; indicators are taken by a diagnostic device with electrodes that are attached to the patient’s body. Each of them picks up bioelectrical signals emitted by myocardial segments. By projecting the electrodes onto a coordinate grid in three dimensions, the angle of the electrical axis is calculated and determined. It passes through the localization areas of the most active electrical processes.
What is sinus arrhythmia?
The human heart normally contracts in the correct sinus rhythm, which is set by the sinus node of the conduction system of the heart. The frequency of this rhythm in an adult is from 60 to 90 beats. in a minute. An indicator that the rhythm is correct is the presence of P waves and equal intervals between RR waves on the electrocardiogram (ECG).
If the RR intervals on the ECG are not the same and the difference between them exceeds 0.1 s, this means that the person has sinus arrhythmia of the heart (on the Internet you can see other names for this type of arrhythmia, for example, sinusoidal, sinusoidal, but they are not entirely correct) . In this condition, the heart beats sometimes faster, sometimes slower, but the contraction of all parts of the heart occurs consistently and correctly.
Causes
As mentioned above, sinus arrhythmia is most often a normal variant, but it can also be a manifestation of a number of pathological conditions. These include:
- vegetative-vascular dystonia;
- lack of certain chemical elements in the body (primarily magnesium and potassium);
- hormonal disorders;
- anemia;
- hypoxia;
- disorders in the functioning of the thyroid gland;
- physical and psycho-emotional exhaustion of the body;
- diseases of the spine and other ailments.
After treatment of these pathologies, the arrhythmia usually disappears and the heart begins to beat correctly again. That is, this condition does not require special treatment and does not harm the body as a whole, which cannot be said about its causes.
It is also worth noting that in old age, pronounced sinus arrhythmia can be a sign of cardiosclerosis and other heart diseases (which will be noticeable on the ECG), and when alternating with significant bradycardia (decreased heart rate) - neurosis requiring special treatment.
Sinus arrhythmia as a normal variant
Physiological sinus arrhythmia (that is, a normal variant) is quite common in childhood and adolescence, which is associated with the development of hormonal levels in children and a temporary imbalance in the functioning of the vegetative-vascular nervous system. According to some authors, such a heart rhythm disorder, to a greater or lesser extent, is observed in more than 90% of absolutely healthy children of any age.
In addition, there is respiratory sinus arrhythmia, a physiological phenomenon that is especially noticeable during slow, deep breathing and can be found in any person. Therefore, to determine whether there is a connection between the rhythm disturbance and the act of breathing, the health care worker asks the patient to hold his breath while recording the ECG.
Sinus arrhythmia during pregnancy
Often in pregnant women, when examining the heart, sinus arrhythmia is also detected. The main reasons for its appearance are electrolyte imbalance and hormonal changes that occur in the body of every expectant mother.
To eliminate rhythm disturbances without medications, doctors recommend pregnant women to eat properly, get proper rest, walk more in the fresh air and, if necessary, take special vitamin and mineral complexes. This condition does not require any other treatment and does not pose a danger to the child.
To completely rule out any suspicions, you can do a dynamic ECG and be sure to regularly take blood tests so as not to miss anemia.
Sinus arrhythmia and vertical position of the EOS
Such a conclusion after an ECG examination of children and adolescents can be found quite often. If there are no complaints, the child feels well and the results of other studies and tests are within normal limits, this condition should not be regarded as a manifestation of pathological changes in the body.
As mentioned above, sinus arrhythmia in childhood is very common, and the vertical position of the EOS (electrical axis of the heart) is typical for people of thin build, which are mainly children. That is, such an ECG conclusion can be considered as a variant of the norm.
What might the manifestations be?
This type of arrhythmia is usually discovered accidentally during an ECG examination. However, some people go to doctors because they have certain complaints and symptoms:
- feeling of lack of air;
- dizziness;
- periodic fainting;
- darkening of the eyes;
- interruptions in the work of the heart (patients say that the heart either stops or beats faster);
- discomfort in the chest (this may be pain, heaviness).
If there are any pathological symptoms and evidence of rhythm disturbances on the ECG, it is worth examining the heart in more detail. It is advisable to do an echocardiogram, Holter monitoring and repeated ECGs. In the absence of any symptoms, in order to make sure that sinus arrhythmia is normal, doctors recommend consulting a cardiologist and undergoing a full diagnosis.
Source: //KardioPortal.ru/content/chto-takoe-sinusnaya-aritmiya
The cardiogram shows a displacement of the EOS - what to do
When receiving such ECG results, you must first find out the opinion of your attending physician on this matter. It’s one thing if the electrical axis is initially vertical, then this is most likely a variant of the norm.
But any changes must be checked, as they may be a sign of the development of one or another pathology. In the case of the vertical electrical axis of the heart, this is quite likely to be a narrowing of such a large vessel as the pulmonary artery or another similar disease.
In this case, taking into account the clinical picture, more examinations will be prescribed to accurately determine the cause.
In the conclusion of a functional diagnostics specialist when performing an ECG, the phrase “vertical electrical axis of the heart” is often heard. In most cases, this is a variant of the norm, but it can also be a sign of pathology, and quite serious one at that.
You can learn how to decipher an ECG and determine the electrical axis of the heart by watching the video: