Leukemia is a disease related to hemablastosis, as a result of which bone marrow cells are everywhere replaced by malignant ones.
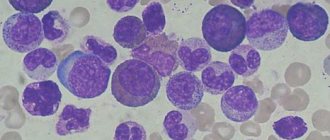
In the blood of leukemia, not only tumor leukocytes appear, but also erythrokaryocytes and megakaryocytes. In addition, the formation of an excess number of leukocytes in the blood with such a pathology is not necessary. The malignant tumor is actively growing and is practically not controlled by the body.
In general, leukemia is potentially curable, but in the chronic form in old age the prognosis is not very favorable. However, the pathological course of the disease can be controlled over a long period.
What it is?
Leukemia (leukemia, blood cancer, leukemia) is a tumor disease of the hematopoietic system (hemoblastosis), associated with the replacement of healthy specialized cells of the leukocyte series with abnormally changed leukemic cells. Leukemia is characterized by rapid expansion and systemic damage to the body - the hematopoietic and circulatory systems, lymph nodes and lymphoid formations, spleen, liver, central nervous system, etc. Leukemia affects both adults and children, and is the most common childhood cancer.
With normal functioning of the bone marrow and good human health, it produces:
- Erythrocytes (red blood cells) - perform a transport function, delivering oxygen and nutrients to the internal organs.
- Leukocytes (white cells) - protect the body from infectious diseases, viruses and other foreign bodies.
- Platelets - ensure blood clotting, which makes it possible to avoid large blood loss during injuries.
As a result of mutation, cells degenerate into cancer cells and are no longer able to perform their functions, which provokes the development of the disease and causes a number of complications. The main danger is that once they enter the circulatory system, they begin to quickly and uncontrollably divide, displacing and replacing healthy ones.
Changed blood cells can enter internal organs and cause pathological changes in them. This often leads to diseases such as anemia, migraine, arthritis, etc. For the development of leukemia, a pathological change in the structure and structure of one cell and its entry into the circulatory system is sufficient. Curing the disease and stopping the spread of cancerous blood cells is extremely difficult and often the outcome is very sad.
What is ALL
Acute lymphoblastic leukemia is an oncological disease that manifests itself in preschool children. It can also occur in an adult in the form of a late relapse, when a case of leukemia has already been established in the medical history. Having similar clinical manifestations at the initial stage of development, it can easily be confused with viral and cold infections.
Lymphoblastic leukemia is characterized by the uncontrolled formation of young forms of lymphocytes - lymphoblasts and prolymphocytes. In cancer, lymphocytes are not produced, so the bone marrow, trying to restore balance, releases immature forms of cells into the peripheral blood (shift to the left).
The appearance of blast cells in any type of disease indicates not only serious disorders in the hematopoietic organs, but also an unfavorable prognosis in the treatment of the patient. Due to a violation of the structure of deoxyribonucleic acid, chromosomal abnormalities develop, and prolymphocytes do not mature.
Forms
Lymphocyte cells are presented in two forms in the body: small and large. The larger forms are –NK cells. The uniqueness of these lymphocytes lies in their ability to destroy cancerous formations. Small forms, in turn, are represented by T- and B-lymphocytes.
- T-lymphocytes are classified as: T-helpers, T-killers and T-suppressors. Their main task is to carry out phagocytosis - devouring bacteria and viruses. T-lymphocytes are produced in the bone marrow and mature in the thymus and thymus. 20% of cases of lymphocytic leukemia are of the T-cell type. It is detected at the age of 15 years, when the formation of the thymus gland ends.
- B lymphocytes play an important role in the formation of immune antibodies. B-lymphocytes mature in lymphoid tissue. Children are susceptible to the B-cell form of lymphocytic leukemia. At the age of 3-4 years, activation of the bone marrow in the production of B-lymphocytes is observed (humoral immunity is formed).
Even more information in the article Lymphocytic leukemia disease: what is it?
B-cell lymphocytic leukemia differs in type:
- pre-pre-B-cell;
- B-II-cellular;
- pre-B cell;
- B-mature cell.
When diagnosing acute lymphocytic leukemia in children, it is important to determine the type of B-cell phenotype, since a specific treatment algorithm has been developed for each subtype. In both cases, the red bone marrow suffers. The work in the formation of cells is disrupted - they do not perform their main functions, moreover, infected with cancer and carrying cancer cells on the surface of the membrane, T- and B-lymphocytes lead to inhibition of cells of another series - erythropoiesis.
Stages of the disease
- Initial stage. It is characterized by the development of anemia, but in the early period of the disease, hemoglobin does not drop to critically low levels (30 -50 g/l). The number of platelets and red blood cells decreases. White blood cells begin to grow rapidly.
- Expanded stage. The main feature of the advanced stage is leukocytosis. The number of leukocytes reaches 250-300*10/9/l. A leukemic failure is recorded (the predominance of cancer cells and immature forms of cells of the leukocyte series) and a leukemic window (there is no division of cells from young to mature forms).
- Remission. In the peripheral blood, blast cells disappear, the level of leukocytes decreases, and all forms of the leukocyte series appear. In bone marrow analysis, blast levels are stable, but not more than 5%.
- Relapse. Return of the disease to a more or less pronounced degree of clinical manifestations. At this stage, the issue of additional treatment measures or treatment in other ways is decided.
- Terminal stage. Therapeutic measures did not lead to the expected results. Hematopoiesis is completely inhibited, cell formation stops. The terminal stage is fatal and patients do not survive.
Causes
What actually causes leukemia is currently unknown. Meanwhile, there are certain ideas on this matter, which may well contribute to the development of this disease.
In particular these are:
- Down syndrome, as well as a number of other diseases with concomitant chromosomal abnormalities, all of this can also provoke acute leukemia.
- Chemotherapy for certain types of cancer can also cause the development of leukemia in the future.
- Heredity, this time, does not play a significant role in the predisposition to the development of leukemia. It is extremely rare in practice to encounter cases in which several family members develop cancer in a manner characteristic of identifying heredity as the factor that provoked it. And if it happens that such an option actually becomes possible, then it mainly implies chronic lymphocytic leukemia.
- Radiation exposure: It is noted that those people who have been exposed to significant amounts of radiation are at greater risk of acquiring acute myeloid leukemia, acute lymphoblastic leukemia or chronic myelocytic leukemia.
- .Prolonged contact with benzenes, widely used in the chemical industry, as a result of exposure to which, accordingly, the risk of developing certain types of leukemia increases. By the way, benzenes are also found in gasoline and cigarette smoke.
It is also important to note that if you have determined, based on the listed factors, your risk of developing leukemia, this is not at all a reliable fact for you to necessarily develop it. Many people, even if they simultaneously note several relevant factors listed above, do not encounter the disease.
Reasons for the development of pathology in children
The causes of leukemia in children and adults have not yet been identified. However, there is an assumption that acute lymphocytic leukemia in children may be caused by a lymphoid virus.
Supposed causes of the development of ALL in children:
- viral infections of the mother during pregnancy;
- antisocial lifestyle of a pregnant woman;
- mother's age at the time of conception;
- immunodeficiency;
- radiography of a pregnant woman;
- exposure to radiation on the fetus;
- chromosomal diseases (Down syndrome, cyalkia).
Common causes of ALL:
- weight over 4 kg;
- illnesses suffered in infancy;
- hereditary predisposition.
Among the most common causes of the development of not only lymphocytic leukemia, but also other types of leukemia, there are radiation and carcinogenic effects on the human body (both mother and father).
We also recommend reading the article Chronic myeloid leukemia - life expectancy at different stages of the disease
Classification
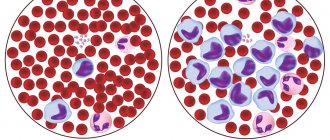
Depending on the number of leukocytes in the peripheral blood, several types of the disease are distinguished. These are leukemic, subleukemic, leukopenic and aleukemic leukemia. According to developmental characteristics, acute and chronic pathologies are distinguished. The first accounts for up to 60% of cases, with it there is a rapid increase in the population of blast cells that do not mature.
The acute type of the disease is divided into types:
- lymphoblastic – diagnosed in 85% of cases in sick children 2–5 years old. The tumor is formed along the lymphoid line and consists of lymphoblasts;
- myeloblastic – damage to the myeloid line of hematopoiesis, noted in 15% of cases in children with leukemia. With it, myeloblasts grow. Leukemia of this type is divided into myelomonoblastic, promyelocytic, monoblastic, megakaryocytic, erythroid;
- undifferentiated - characterized by cell growth without signs of differences, represented by homogeneous small stem blasts.
The disease develops slowly and is characterized by excessive growth of mature inactive leukocytes. In the lymphocytic form of the disease, B and T cells develop (lymphocytes responsible for the absorption of foreign agents), while in the myelocytic form, granulocytes develop.
When classifying chronic leukemia, juvenile, childhood, adult types, myeloma, and erythremia are distinguished. The latter is characterized by leukocytosis and thrombocytosis. In the myeloma type, plasma cells grow and immunoglobulin metabolism is disrupted.
Stages of leukemia
In differentiated acute leukemias, the process occurs in stages and goes through three stages.
- Initial – the symptoms are expressed to a minor extent, often the initial stage goes unnoticed by the patient. Sometimes leukemia is detected by a random blood test.
- The stage of advanced manifestations, with clear clinical and hematological signs of the disease.
- Terminal – lack of effect from cytostatic therapy, pronounced inhibition of normal hematopoiesis, ulcerative-necrotic processes.
Remission in acute leukemia may be complete or incomplete. Relapses are possible; each subsequent relapse is prognostically more dangerous than the previous one.
Chronic leukemia is characterized by a more benign and prolonged course, periods of remissions and exacerbations. There are three stages of chronic leukemia.
- Chronic stage - characterized by gradually increasing leukocytosis, increased overproduction of granulocytes, and a tendency to thrombocytosis. The disease at this stage, as a rule, is asymptomatic or manifests itself with mild signs of hypermetabolism, anemic syndrome.
- The acceleration stage is a change in the blood picture, reflecting a decrease in sensitivity to ongoing and previously effective therapy. Most patients do not have new characteristic clinical symptoms or they are not clearly expressed.
- The blast crisis stage (acute stage) is a sharp decrease in the level of red blood cells, platelets and granulocytes, which leads to internal bleeding, ulcerative necrotic complications, and the development of sepsis.
The proliferation of leukemic cells in organs and tissues leads to serious anemia, severe degenerative changes in parenchymal organs, infectious complications, and hemorrhagic syndrome.
In undifferentiated and poorly differentiated forms of leukemia, there is no staging of the pathological process.
Types of Leukemia
The different forms of leukemia are classified according to the speed at which the disease manifests and the type of cell of origin.
Based on the speed of occurrence of the disease, we distinguish:
ACUTE LEUKEMIA
In acute leukemia, immature cells called leukemic “blasts” accumulate in the blood, bone marrow, and sometimes also in the spleen and lymph nodes. These cells do not work properly, have a very long average life and excellent ability to reproduce, so the disease occurs and progresses quickly. Acute leukemia requires rapid and aggressive therapy.
CHRONIC LEUKEMIA
Chronic leukemias are characterized by the accumulation in the blood, bone marrow, spleen, and often lymph nodes of white blood cells that mature almost normally, grow indefinitely, and tend to accumulate over a long period of time. They may work normally for a certain period of time. Chronic leukemias are often asymptomatic initially and remain silent for a long period before diagnosis.
However, based on the cell type of origin they differ:
LYMPHATIC LEUKEMIA
This type of leukemia involves lymphocytes, which are part of our immune system. Lymphocytes are found in circulating blood and lymphatic tissue.
Myeloid leukemia - This type of leukemia involves cells of myeloid origin, which gives rise to red blood cells, white blood cells and platelets.
Signs of Leukemia
With leukemia, one can distinguish the characteristic signs of this oncological disease of general and local manifestations.
These symptoms of leukemia in adults include: fatigue and weakness; insomnia or constant desire to sleep; deterioration of concentration and memory; pale skin and dark circles under the eyes; non-healing wounds; the formation of various hematomas on the body for no apparent reason; nosebleeds; frequently occurring acute respiratory viral infections and infections; splenomegaly and enlargement of lymph nodes, as well as liver, rise in temperature.
Laboratory blood tests reveal a decrease or increase in ESR, various types of leukocytosis, thrombocytopenia and anemia.
One or more of the above signs does not indicate leukemia. And in order to exclude or confirm the diagnosis, it is advisable to be examined in a specialized clinic and consult with professionals.
Symptoms and signs
Symptoms directly depend on the stage of the disease, and at an early stage it has a common clinical picture with a viral infection: dizziness, malaise, fever, lethargy and fatigue.
The main symptoms of acute lymphocytic leukemia in a child include:
- Anemia syndrome. Due to the inadequate production of hemoglobin by red blood cells, the body does not receive enough oxygen. This is expressed in lack of appetite, dizziness, low-grade fever. The skin is pale and dry. Pre-fainting conditions are characteristic when hemoglobin is less than 80 g/l.
- Hemorrhage syndrome. Due to a decrease in the quantitative and qualitative properties of platelets, small dots (bruises) appear on the skin and mucous membranes. Sometimes vomiting with blood appears.
- Overgrowth syndrome (hyperplastic symptom). Cancer cells, complicating the functioning of internal organs, lead to an enlargement of the spleen, liver, and lymph nodes. Due to the proliferation of bone marrow, swelling of the joints appears.
Signs of lymphoblastic type leukemia are associated with a decreased immune response:
- pain in the limbs, the body aches from pain;
- persistent colds (sore throat, bronchitis);
- difficulties with breathing rhythm due to enlarged lymph nodes;
- formation of abscesses and boils;
- the appearance of leukemia - brown formations on the skin - appear as confirmation of the advanced process of ALL.
Acute form
The most common form of acute leukemia in adults is acute myeloid leukemia (AML). The prevalence of this disease is 1 in 100,000 people over 30 years of age and 1 in 10,000 people over 65 years of age. The causes of acute myeloid leukemia in adults are not fully understood.
Symptoms of acute leukemia in adults:
- Symptoms of influenza are fever, weakness, bone pain, symptoms of inflammation of the respiratory tract.
- Symptoms of the so-called purpura - bleeding from mucous membranes, mainly from the gums, nose, gastrointestinal tract or genital tract and hemorrhagic purpura on the skin and membranes.
- Symptoms associated with weakened immunity - frequent colds, activation of herpes, poor health, lack of appetite, bacterial and fungal infections, erosion on the membranes, etc.
- In addition, leukemia causes a number of other symptoms, not all of which occur in all patients and are not typical for leukemia. But they are very “valuable” in diagnosing the disease.
- With acute lymphoblastic leukemia, an enlargement of the spleen and/or lymph nodes occurs in 75% of patients, which allows for preliminary differentiation in relation to acute myeloid leukemia.
- Some patients with lymphoblastic leukemia also experience problems with blood flow in small vessels as a result of blockages of blood cells, most often when the number of white blood cells in the blood is significantly higher than normal. This may manifest itself in the form of visual or mental disturbances.
During acute leukemia, rapid diagnosis and immediate treatment are very important. Acute leukemia, if left untreated, usually leads to death within a few weeks.
Acute lymphoblastic leukemia in children: what is it?
The essence of the disease is as follows. Before following one of the developmental paths and becoming a full-fledged lymphocyte, the cell is in the red bone marrow in an embryonic state. It is called a progenitor cell or an immature cell.
If at this stage the cell has undergone a mutation, it stops developing according to the intended scenario and acquires atypical features. Such modified cells are called blasts or lymphoblasts.
The blast cell begins to actively divide and multiply, inhibiting the division of other, healthy cells. Multiple lymphoblasts fill the bone marrow, then go beyond it, into the patient’s bloodstream, and are carried throughout the body through the bloodstream. As a result, the composition of the blood changes, and organs and tissues do not receive the necessary nutrition. The first to suffer in such a situation are the lymph nodes, liver, spleen and brain - this is where lymphoblasts are primarily sent.
A concomitant pathology that accelerates the development of a malignant process in the red bone marrow and blood is mutations in genes responsible for apoptosis - the death of cells with DNA abnormalities.
On average, the time from the onset of blast division to the appearance of the first pronounced symptoms in ALL is 2-3 years.
Stages of ALL in children
Now, having told in general that this is lymphoblastic leukemia in children, we can detail the information. The medical classification distinguishes several stages of this oncological pathology.
- Initial period with mild symptoms. At this stage, ALL in children is diagnosed in isolated cases.
- Advanced stage of pathology. It is also called primary active. Symptoms become noticeable, moreover, they appear simultaneously or one after another. It is at this stage that acute lymphoblastic leukemia is most often diagnosed in children.
- Remission stage. It is characterized by satisfactory well-being of the patient and a decrease in the number of blast cells in the blood. If this figure fluctuates between 5-20%, it is customary to talk about incomplete remission. If there are less than 5% of atopic cells in the patient’s blood, we can talk about complete remission.
- Relapse stage. Doctors talk about it during exacerbation of the disease in the remission stage, as well as when secondary disorders associated with the underlying disease occur.
- Terminal stage. The most complex and severe stage of childhood blood cancer of the lymphoblastic type with a large number of blast cells, critical inhibition of the hematopoietic system and life-threatening conditions.
- Recovery stage. It occurs infrequently; most often, the patient experiences a long-term stable remission. Nevertheless, in some cases, doctors have reason to talk about complete recovery. It is confirmed by a zero level of blasts in the blood, a complete absence of clinical manifestations of ALL and the consequences of the disease.
Children's acute leukemia of lymphoblastic type: prerequisites for its occurrence
The exact causes of acute lymphoblastic leukemia in children are still not known. Given the same initial data and life circumstances, the process may start for one child, but not for the second.
Presumably the prerequisites for the manifestation of ALL are:
- hereditary factors. This includes genetic mutations, chromosomal pathologies, congenital gene defects, as well as the presence of other genetic diseases, for example, Down syndrome, Fanconi anemia, and some others;
- congenital immunodeficiency;
- exposure to ionizing radiation (radiation) both on the child and on the mother during pregnancy;
- accumulation in the body of salts of heavy metals, as well as pesticides, herbicides and industrial carcinogens;
- certain viruses - Epstein-Barr, human papillomavirus of some types, herpes and others;
- a child or woman taking a large number of non-steroidal anti-inflammatory drugs and antibiotics during pregnancy, as well as immunosuppressants and cytostatics, for example, as part of the treatment of another cancer.
The high-risk group for acute lymphoblastic leukemia includes Caucasian male children aged 2 to 5 years, whose close relatives have already been diagnosed with this disease.
Chronic form
This type of disease is characterized by a slow or moderate course (from 4 to 12 years). Manifestations of the disease are observed in the terminal stage after metastasis of blast cells beyond the bone marrow. A person loses weight sharply, his spleen enlarges, pustular skin lesions and pneumonia develop.
Symptoms depending on the type of chronic leukemia:
- Myeloblastic - rapid or slow heartbeat, stomatitis, sore throat, kidney failure.
- Lymphoblastic – impaired immunity, cystitis, urethritis, tendency to ulcers, pulmonary lesions, herpes zoster.
Common symptoms of chronic leukemia in adults are specific signs:
- bleeding – nasal, skin, heavy menstruation in women;
- bruises that appear suddenly, without mechanical trauma;
- joint pain in the area of the sternum, pelvic bone;
- chronic fever - appears due to the fact that internal inflammatory processes activate the work of the hypothalamus, which is responsible for the increase in temperature;
- cough, nasal congestion, frequent infections caused by decreased immunity;
- constant fatigue, weakness, depression, which arise due to a drop in the level of red blood cells.
Symptoms
| Occurrence (how often a symptom occurs in a given disease) | |
| General weakness (fatigue, tiredness, weakness of the body) | 70% |
| Nosebleeds (nosebleeds, epistaxis) | 60% |
| General increase in body temperature (fever, fever) | 60% |
| Weight loss (emaciation, weight loss, thinness, weight loss, weight loss) | 60% |
| Heaviness, pain in the left hypochondrium | 50% |
| Bleeding gums | 40% |
| Star-shaped rashes, burgundy, bluish | 0% |
Complications
Many of the complications of leukemia depend on a decrease in the number of normal blood cells, as well as side effects from treatment.
These include frequent infectious diseases, bleeding, weight loss and anemia. Other complications of leukemia are related to the specific type of leukemia. For example, in 3–5% of cases of chronic lymphocytic leukemia, the cells transform into an aggressive form of lymphoma. Another potential complication of this type of leukemia is autoimmune hemolytic anemia, in which the body destroys its own red blood cells.
Tumor lysis syndrome is a condition caused by the rapid death of cancer cells during treatment. It can develop in any cancer, including leukemia with a large number of abnormal cells (for example, acute leukemia). The rapid destruction of these cells releases large amounts of phosphate, which can cause metabolic disorders and kidney failure. Children treated for acute lymphoblastic leukemia may develop long-term adverse effects, including central nervous system problems, slowed growth, infertility, cataracts, and an increased risk of developing other cancers.
The incidence of these long-term complications varies depending on age at the time of treatment and the type and strength of therapy administered.
Symptoms
The development of lymphocytic leukemia is accompanied by the appearance of a whole symptomatic complex. At the very beginning of the development of the disease, the patient may complain of fatigue and lethargy. The child has no desire to participate in outdoor games.
The disease causes oxygen starvation. It arises for the reason that with intensive reproduction of pathologically altered cells, the division of normal cells is slowed down, as well as their growth. As a result, anemia and oxygen starvation develops.
Due to the insufficient number of leukocytes, the immune system decreases. A lack of platelets causes frequent bleeding and bruising.
Let's consider the main symptoms of the development of acute lymphoblastic leukemia in children:
- Intoxication of the body. Since the baby’s immunity is reduced, his body is defenseless against all kinds of bacteria and viruses. Their activity is evidenced by such symptoms of intoxication as lethargy, weakness, fever, and pale skin. Often these symptoms are accompanied by fever.
- Respiratory dysfunction. The result of enlarged mediastinal lymph nodes is respiratory rhythm disturbances. As a result, there may be hemorrhages in the lung tissue with symptoms such as coughing with sputum in which blood is visible.
- Hemorrhages. We are talking about subcutaneous hemorrhages. Due to the fact that the patient’s body has a reduced number of platelets, petechiae – small hemorrhages – appear on the child’s mucous membranes and skin. Blood may also appear in the stool, as well as bloody vomiting.
- Syndrome of proliferation or hyperplasia of lymphoid tissue. The liver, lymph nodes and spleen enlarge. Due to the proliferation of bone marrow, swelling and painful joints may occur. The bones become more brittle, making the patient susceptible to fractures.
- Frequent skin infections. With reduced immunity, even minor skin lesions lead to subsequent infection. Children with leukemia often suffer from furunculosis, abscesses at injection sites and purulent inflammation of the nail bed.
- Anemia. Characterized by a decrease in the amount of hemoglobin and red blood cells. Accompanied by dry and pale skin and mucous membranes, decreased appetite, and weakness.
Diagnostics
If there is a suspicion of leukemia, the person must be sent to an oncohematology hospital. Staying at home with such a disease or suspicion is strictly contraindicated! Within a few days, specialists will take all the necessary tests and perform all instrumental studies.
- First of all, a general and biochemical blood test is taken. In the general analysis for leukemia, anemia (reduced number of red blood cells and hemoglobin), thrombocytopenia (decreased number of platelets) is often noted; the number of leukocytes can be either reduced or increased. Sometimes blast cells can be found in the blood.
- Be sure to take bone marrow and cerebrospinal fluid. Bone marrow analysis is the most important; it is on its basis that the diagnosis of leukemia is established or removed. Cerebrospinal fluid is a mirror of the state of the central nervous system. If blast cells are detected in it, more intensive treatment regimens are used.
All other studies, such as ultrasound, computed tomography, radiography, are additional and necessary to assess the extent of the process.
Diagnostic measures
Diagnosis of acute lymphoblastic leukemia consists of studying blood parameters, bone marrow and clinical manifestations of leukemia.
- Taking blood for a detailed analysis with counting of formed elements. Biochemical and cytochemical studies to clarify the phenotype of ALL.
- X-ray and ultrasound examination of the abdominal cavity and chest.
- Myelogram. Study of red bone marrow puncture to determine the composition of the CSF and count the formed elements. In exceptional cases, a spinal cord biopsy is performed to determine neuroleukemia.
- Genetic examination. The detection of chromosome 22 in a CSF specimen makes it possible to determine the correct treatment tactics.
- Other studies: urine analysis, ECG, fluorography, MRI of extremities.
Treatment
Leukemia therapy is differentiated; the choice of treatment methods depends on the morphological and cytochemical type of the disease. The main goal of complex therapy is to rid the body of leukemic cells.
The main methods of treating leukemia:
- chemotherapy - treatment with various combinations of cytostatics in high dosages (polychemotherapy);
- radiation therapy;
- bone marrow transplantation – transplantation of donor stem cells (allogeneic transplantation).
There are 5 stages of chemotherapy:
- The cytoreductive preliminary stage of treatment is carried out during the first attack of acute leukemia.
- Induction therapy.
- Consolidation of remission (2–3 courses).
- Reinduction therapy (repetition of the induction stage).
- Maintenance therapy.
All forms of leukemia are characterized by the replacement of normal tissue with pathological tumor tissue; the form of leukemia depends on which cell makes up the morphological substrate of the tumor.
For chronic leukemia in the preclinical stage, restorative treatment and constant medical supervision are sufficient. If there are clear signs of the disease transitioning to the acceleration phase and blast crisis, cytostatic therapy is carried out. For special indications, irradiation of lymph nodes, skin, and spleen is used, and splenectomy is performed. Allogeneic bone marrow transplantation can provide good results.
Rehabilitation after treatment
The recovery process from acute lymphoblastic leukemia is long and difficult, and the earlier the disease is diagnosed, the faster and better it will be overcome.
For children, the prognosis is favorable - about 90% are completely cured. Relapses occur in only 5% of the young population, but can be treated with a bone marrow transplant. As statistics show, timely treatment of leukemia in a child leads to a one hundred percent guarantee of recovery, which cannot be said about the adult population.
Forecast
The prognosis for life with leukemia depends on the form of the disease, the extent of the lesion, the patient’s risk group, timing of diagnosis, response to treatment, etc.
Leukemia has a worse prognosis in male patients, in children over 10 years of age and adults over 60 years of age; with a high level of leukocytes, the presence of the Philadelphia chromosome, neuroleukemia; in cases of delayed diagnosis. Acute leukemias have a much worse prognosis due to their rapid progression and, if left untreated, quickly lead to death. In children, with timely and rational treatment, the prognosis of acute leukemia is more favorable than in adults. A good prognosis for leukemia is considered to be a 5-year survival rate of 70% or more; the risk of relapse is less than 25%.
Chronic leukemia, upon reaching blast crisis, acquires an aggressive course with the risk of death due to the development of complications. With proper treatment of the chronic form, it is possible to achieve remission of leukemia for many years.
Hepatitis C: first signs and treatment regimen Psoriasis Diabetes mellitus Demodicosis in humans: photos, symptoms and treatment Pancreatitis Glaucoma