Stages of gangrene development
The source of the pathological process in the peripheral tissues of the extremities is the restriction or final cessation of blood flow and oxygen supply. Based on this, doctors distinguish two stages of gangrene of the leg:
- Gradual development. Tissue death occurs sequentially. Initially, cells on the foot or toe begin to die. If at this stage the necessary measures are not taken to eliminate the problem, necrosis develops further, spreading to the subcutaneous tissue and bones. If an infection occurs, gangrene becomes moist and gradually spreads to other tissues, causing serious intoxication of the body. As a rule, such a clinical picture is observed in diabetes mellitus.
- Lightning-fast development. A sudden cessation of blood circulation in the legs contributes to the formation of blood clots in the arteries of the affected area of the limb. As a result, tissues die. The absence of the so-called restrictive granulation shaft entails rapid absorption of decomposition products. In terms of saving the leg, the clock literally counts.
Causes and first signs of gangrene - how does the disease begin?
The rapid development and neglect of necrotic phenomena often makes the prognosis of the disease unfavorable. In the early stages, some cases of gangrene can be treated.
With this disease, tissues affected by necrosis gradually become dead. At the same time, they change color to a very dark, almost black, lifeless color.
The cessation of blood supply to an area of the human body leads to a decrease in its sensitivity, dry skin, brittleness and thinning of hair. The skin of the affected area first turns pale and cold, then acquires a marble-blue hue. The changes are accompanied by severe pain.
As the disease progresses, the dying tissues become increasingly darker. In places affected by pathology, the pulse can no longer be felt. At the next stages of the disease, despite the lack of tissue sensitivity, severe pain in the area of necrotic changes persists.
The disease can affect not only the skin and subcutaneous tissue, but also muscles, gall bladder, intestines, lungs, and limbs. It develops in parts of the body distant from the heart against the background of the fact that oxygen ceases to flow into the tissue.
Comment by Boris Sergeevich Kravchenko, surgeon, ultrasound diagnostics doctor:With wet gangrene, tissue necrosis is more severe, often with the addition of a putrefactive infection, which leads to the disintegration of dead tissue and the development of severe intoxication.
Thrombosis of large veins and insufficiency of venous collaterals with undisturbed arterial blood flow can sometimes also be one of the causes of the development of wet gangrene.
It is very important to provide timely qualified assistance, which will improve the further prognosis of this disease.
If you have diabetes, high blood sugar can eventually damage blood vessels, cutting off blood flow to parts of your body. The pressure of excess weight can also constrict arteries, leading to decreased blood flow and increasing the risk of infection and poor wound healing.
Gangrene infected with pathogenic bacteria can quickly spread to other organs and can be fatal without treatment.
The causes of gangrene can be divided into five main groups:
- Disturbance of local blood supply to tissues
This occurs with vascular spasms, blockage of large arteries, and in the presence of anatomical abnormalities. Similar phenomena are typical for diabetes mellitus, thrombosis, heart attacks and strokes.
- The effect of mechanical causes - such as bedsores in long-term bedridden patients, injuries in which blood vessels are damaged or tissue crushing occurs.
- Chemical damage in the form of acid or alkaline burns.
- Impact of physical factors.
These include third degree burns, frostbite of tissues and organs.
Etiology of gangrene
The main causes of the development of the disease can be divided into external and internal. The first ones include the following:
- Mechanical damage and injury.
- Bedsores.
- Ionizing radiation, burns/frostbite.
- Exposure to chemical agents (phosphorus, alkali, arsenic).
Internal causes include any pathological processes that occur with impaired tissue nutrition. They are usually accompanied by deformation of blood vessels and anatomical changes, which is often observed in atherosclerosis and diabetes.
Sometimes gangrene of the legs develops without the participation of microorganisms. In this case we are talking about the aseptic form of pathology. If anaerobic flora is involved in the pathogenesis, they speak of septic gangrene.
Etiology
Despite the fact that such a disease is considered quite rare by clinicians in our time, the causes of gangrene are varied and numerous. The most common triggers are:
- extensive injury to connective or cartilage tissue;
- deep burns;
- prolonged exposure to low temperatures on the feet;
- a powerful electric shock or a person being struck by lightning;
- the influence of chemical reagents, for example, acidic, alkaline or other aggressive substances;
- wounds resulting from a knife or gunshot wound;
- the formation of trophic ulcers, which are often a consequence of varicose veins of the legs;
- crushing of connective tissue or bones;
- bedsores;
- vibration disease;
- the development of an infectious process against the background of the influence of pathogenic or conditionally pathogenic microflora - this includes streptococci and enterococci, Staphylococcus aureus and Escherichia, as well as clostridia;
- the course of atherosclerosis or diabetes mellitus;
- Raynaud's disease;
- pathologies of the cardiovascular system, in particular heart failure, blood clots, ischemia or embolism;
- obliterating endarteritis;
- polyneuropathy;
- strangulation of a hernia formed in the groin area;
- applying a tight bandage, tourniquet or other medical manipulations that lead to severe compression of blood vessels;
- a wide range of vascular damage to the lower extremity.
Predisposing factors that increase the risk of necrosis of the skin tissue of the legs are:
- sharp fluctuations in body weight - its gain or loss;
- a history of anemia;
- diseases of the endocrine system;
- lack of vitamins in the human body;
- failure of the immune system;
- the course of chronic pathologies of an infectious nature;
- malignant arterial hypertension;
- prolonged fasting;
- metabolic disorder;
- intoxication or dehydration of the body.
Regardless of the influence of one or another cause of gangrene of the lower extremities, in any case, a disruption of the blood circulation process occurs.
What symptoms indicate illness?
The first sign of pathology is severe pain. The discomfort is so strong and painful that the patient tries to alleviate his condition by any means. Over time, the intensity of the pain only increases and persists until the final death of the nerve fibers.
Another symptom is a change in skin tone. The color of the affected area may vary from bluish to greenish. Patients also complain of numbness of the limbs, loss of sensitivity, and severe cramps. My feet get cold all the time, even in warm weather. Small ulcers gradually develop on the skin, which heal very slowly.
Signs of gangrene of the leg may vary depending on the form of the pathology. Currently, doctors distinguish three types of the disease: wet gangrene, dry and gas. Next, we will consider each option in more detail.
Classification
Based on which segment of the leg is affected, the disease is divided into:
- gangrene spreading along the entire length of the leg;
- gangrene of the foot;
- gangrene of the toes;
- gangrene of the nail.
Depending on the etiological factor, there are:
- ischemic gangrene;
- toxic gangrene;
- infectious gangrene;
- toxic gangrene;
- allergic gangrene;
- anaerobic gangrene;
- hospital gangrene caused by surgery.
Types of gangrene according to clinical course:
- dry - formed against the background of a long-term disorder of the circulatory process under aseptic conditions, i.e., without the occurrence of infections. Most often it affects both extremities. It is noteworthy that dry gangrene of the lower extremities very rarely threatens human life - the danger arises only with secondary infection;
- gas - there is only one cause - the presence of a deep wound into which pathological microorganisms have penetrated and negatively affected;
- wet gangrene is always an unfavorable prognosis. This is due to the fact that the pathological process is always accompanied by infections.
With lesions of the legs, types 1 and 3 of the disease are most common.
Dry gangrene has the following stages of progression:
- circulatory disorders;
- tissue necrosis;
- formation of an inflammatory cushion;
- mummification;
- development of putrefactive processes;
- amputation.
Wet gangrene of the lower extremities as it develops goes through the following stages:
- sudden cessation of blood supply;
- rapid tissue necrosis, sometimes fulminant;
- decomposition or rotting of dead tissue;
- penetration of toxins into the blood;
- disruption of the functioning of many organs and systems, up to multiple organ failure.
Stages of development of diabetic foot:
- severe itching;
- violation of skin integrity;
- the appearance of an ischemic zone without inflammation;
- attachment of the inflammatory process;
- the occurrence of foci of necrosis;
- gangrene.
Wet gangrene of the leg (photo)
The initial stage of this pathology is characterized by rapid development, which is accompanied by rapid blockage of the vessels of the affected organ.
Wet gangrene of the leg (see photo below) usually occurs due to injuries, burns or frostbite. Dead tissue does not have time to dry and begins to rot. This serves as a favorable environment for the proliferation of many microorganisms, which only aggravates the course of the pathology. Rotting and subsequent breakdown of bacterial waste products leads to intoxication of the body.
As a result of the development of the disease, not only the limbs are affected, but also the internal organ systems (intestines, gall bladder, lungs). They gradually increase in size and acquire a bluish tint. The pathology is manifested by pallor of the skin, the appearance of dark spots, and the epidermis gradually begins to peel off. As it progresses, a wet and foul-smelling mass consisting of necrotic tissue appears in the lesion.
Patients complain of a sharp increase in temperature, dry mouth, and low blood pressure. The pathological process very quickly spreads to healthy tissues and organs, which can result in sepsis and death. Wet gangrene of the legs is especially dangerous in diabetes mellitus, when the body is not able to fully resist illnesses.
Symptoms of gangrene of the foot and toes at the initial stage
The disease begins dynamically, so it is almost impossible to confuse it with other pathologies of the lower extremities. Especially if the diagnosis and initial examination are carried out by an experienced surgeon. In the first stages of development of gangrenous necrosis of the foot or toe, the symptoms are as follows.
Excessive swelling
The skin at the site of the future lesion first becomes enlarged and swells. A person who has no idea about the possible onset of gangrene (if there was no actual injury) gets the impression that he hit himself somewhere or rubbed his finger with tight shoes. Gradually, the swelling increases and the affected part of the limb becomes completely swollen, like after a bee sting.
Pain syndrome
As the inflammatory process progresses, pain begins to be felt inside the toe or foot. It always has the acute nature of a prolonged attack or a few seconds of lumbago. This indicates that an abscess of soft tissues is occurring and purulent exudate is actively accumulating in the subcutaneous layer.
Temperature increase
Almost always, gangrene is caused by pathogens that enter the limb from the environment along with infected water, particles of dust, soil, or dirty hands. Much less often, necrosis occurs against the background of secondary pathologies such as diabetes mellitus or thrombosis of the main blood vessels. As the number of microbes increases and their activity increases, body temperature rises to 39 degrees Celsius and above. It all depends on which strain of microflora is parasitic and systematically destroys the soft tissue of the limb.
Pale skin
Along with swelling, the first signs of gangrene of the toes are an unnaturally pale appearance of the epithelial surface. The leg in the affected area becomes waxy and lifeless. During palpation, it is discovered that there is no pulse, there is no blood supply, or it is minimal and it is not possible to record it.
Rapid color change
The previous pallor begins to change to a uniform red tint, which completely covers the entire finger or foot. Then the redness darkens, becomes cyanotic, and then every day the color of the limb changes only towards darkening. A black tint indicates that the necrosis process has reached its peak and the situation is dire.
Tissue swelling
In the subcutaneous layer of the sore leg, purulent exudate begins to accumulate, along with which a certain volume of gases is formed. As a result of this, the finger spreads and it increases in size by 3-4 times. An ulcerative formation may appear, from which pus flows.
gangrene of the foot and toe in the photo
At this stage of the disease, the primary symptoms of gangrene end. All further processes relate to later periods of manifestation of necrosis and are accompanied by severe intoxication, cadaveric decomposition of tissues and other signs of mass death of cells of the lower limb. The description of foot gangrene in theory and what awaits a person in practice is still slightly different.
Therefore, the real clinical picture of the course of the disease looks more intense than indicated in textbooks.
Gas gangrene
This form of pathology develops at the site of crushed tissue due to infection of the wound. Gangrene is accompanied by the active activity of anaerobic microbes, which produce a specific gas when multiplying. Bacteria spread very quickly to wet wounds and dead tissue. The infection usually develops over several days and leads to severe intoxication of the body. The wound swells, gas gradually accumulates in its tissues, and muscle decomposition begins. This clinical picture is accompanied by gas gangrene of the leg.
Symptoms of intoxication may be as follows:
- Heat.
- Nausea.
- Reduced blood pressure.
- Rapid breathing.
- Tachycardia.
When pressing on the affected area, an unpleasant odor is felt. It is explained by the release of gas bubbles from under the skin.
Treatment of gangrene
Surgery is the only way to eliminate gangrene of the arms/legs. In dry and wet forms, as a rule, amputation of the affected segment (hand, foot, leg, etc.) is performed. The presence of severe symptoms of intoxication is an indication for intravenous infusions of crystalloids (Ringer's solution or 0.9% sodium chloride) and the prescription of antibiotics. Antimicrobial therapy must cover different types of bacteria, since it is almost impossible to accurately determine the causative agent in the early stages.
If possible, doctors try to save the infected arm or leg. Treatment without amputation for gas gangrene, which is most often located on the lower extremities, is carried out gradually. For this purpose, all dead tissue within the wound is removed. The operation is complemented by “lampas” incisions - long longitudinal dissections of the skin and fatty tissue to ensure a constant flow of air. This procedure reduces the growth and spread of anaerobic microbes. In addition, several antibiotics, anti-gangrenous serum and intravenous infusions of crystalloid solutions (up to 4-5 liters/day) are prescribed.
If the above measures are ineffective, treatment of gangrene of the lower limb (or upper) is carried out by amputation. This procedure can only be performed until the infection spreads to the torso.
Gangrene of internal organs is treated according to similar principles:
- Dead tissue is removed (part of the lung, gall bladder or appendix);
- Eliminate symptoms of intoxication (intravenous infusions of Ringer's solutions/sodium chloride);
- Several antibiotics are prescribed.
The prognosis for the patient depends on the timeliness of treatment, the condition of the body and the speed of spread of the infection.
Dry gangrene
The disease predominantly affects the lower extremities in patients who are extremely malnourished. The initial stage of gangrene of the legs is accompanied by disturbances in the circulatory system and blockage of blood vessels. This is a very slow process that can take months or even years. Initially, patients complain of severe pain discomfort in the feet and toes, the limb takes on a marbled tint and becomes cold. As the disease progresses, the tissues slowly die. First they dry and wrinkle, then thicken and become bluish in color. Externally, the border between healthy and already dead tissues is clearly visible.
Dry gangrene is not accompanied by intoxication of the body, since there is no process of suppuration. As long as it does not transform into a wet form, there is no threat to the patient’s life. Typically, dry gangrene of the leg does not spread to adjacent tissues, but stops in a limited area of the limb. During this period of time, the body has time to react and “turn on” protective mechanisms in order to isolate healthy areas from necrotic ones.
How does gangrene manifest?
Signs of gangrene vary depending on what type of pathology develops.
Dry
In this case, the “culprit” of the disease is impaired venous or arterial circulation or its complete stop. This explains the fact that the first manifestations at the onset of gangrene development are associated with insufficient blood flow. Symptoms include:
- "Crawling" sensation.
- Tingling in the legs.
- Pain syndrome. Sometimes it is acute, disturbing during physical activity, but subsiding when at rest.
- Weakness in the limbs that occurs during exercise.
- Paleness of the outer integument.
- Feeling cold.
- Lameness.
If blood circulation in the extremities is completely stopped, then the symptoms of gangrene of the leg will be as follows:
- Presence of black skin tone. This color is characteristic of the dry type of necrosis.
- Reducing the parameters of the injured leg. To determine, it is enough to measure the length of these parts of the body.
- Excessive dryness in the problem area, cessation of activity of the sweat glands.
- Increased tissue density due to moisture deficiency.
- Stopping hair and nail growth on the affected leg.
Patients also show signs of general intoxication. But they are weakly expressed, because the body manages to fight toxins released into the circulatory system.
Wet
The clinical picture for this type of pathology is more extensive. Local and general symptoms are observed, since the infectious process affects not only the leg itself, but also the internal systems of the body. Among the local signs the following are distinguished:
- Blueness of the skin or its acquisition of a dark purple color.
- Painful sensations in the affected area.
- An increase in local temperature in the area where pathogenic microflora is actively multiplying, and its decrease in areas that have already died.
- Swelling of the injured leg.
- The appearance of a putrid odor.
Wet gangrene is also accompanied by general signs of intoxication of the body, since the immune system cannot cope with the elimination of harmful substances released into the blood. Patients complain of the following symptoms:
- High body temperature.
- General weakness.
- Decreased appetite.
- Nausea that occurs regularly.
- Attacks of dizziness.
- Excessive sweating.
In childhood, seizures often occur. This is due to the fact that the body is not yet able to fight such a dangerous disease. In older people, the body does not respond adequately to pathology, so the manifestations may be mild.
Anaerobic necrosis
With this type of gangrene, symptoms are also divided into local and general. Pathogenic microorganisms spread through the legs at high speed, releasing many waste products into the circulatory system, which poisons the internal systems.
The area affected by the gas type of necrosis has the following features:
- Pale skin.
- Low local temperature.
- The appearance of blue or red spots.
- Tissue swelling that is constantly increasing.
- Putrid odor from the affected area of the body.
- Discharge from wounds of a cloudy liquid that smells unpleasant and has a greenish or brown tint.
- The appearance of a crunch when palpating the sore limb.
When the muscles in the wound area are exposed, the tissues resemble cooked meat, having a white tint and separation into individual fibers.
Symptoms of general intoxication with gas gangrene appear quite pronounced. Most often they cause the death of the patient. These signs include the following:
- Weakness throughout the body. It can be so severe that it becomes difficult for a person to move.
- High body temperature.
- Sleep disorders.
- Impaired consciousness. Sometimes a delusional state is observed.
- Regular vomiting that does not bring relief.
- Reduced blood pressure.
- Cardiopalmus.
Pathogenic microorganisms can infect internal organs, which will disrupt their functioning and cause the death of the patient in a short time. Therefore, it is important to promptly identify anaerobic necrosis during gangrene and eliminate it.
Bedsores
This type of disease occurs when pressure is placed on tissue for a long time. The necrotic process develops gradually. If blood flow is impaired, the outer skin becomes pale, then the local temperature decreases, and numbness appears.
Next, swelling of the skin forms. In later stages, the compressed areas of the legs turn black. If treatment is not timely, an infectious process develops, aggravating the course of the disease and causing symptoms of general intoxication.
How to diagnose gangrene?
For the most informative and accurate diagnosis of the pathological process, doctors today use several effective techniques. These include the following:
- Microbiological diagnostics. Allows you to determine the type of pathogen and its sensitivity to antibiotics.
- CT.
- Radiography. Helps determine the presence of even small volumes of gas in affected tissues.
- Bronchoscopy.
Based on the test results, the doctor can confirm the diagnosis of gangrene of the leg. Photos of the pathology and treatment options are presented in this article.
Diagnostic measures
It is enough to make an accurate diagnosis based on the patient’s complaints, the results of a visual examination and palpation of the limb. Laboratory research methods are carried out only to clarify the general condition of the patient and determine the sensitivity of microorganisms to antibiotics.
To assess health status, a number of the following studies are carried out:
- blood biochemistry for the degree of inflammation (leukocyte level, urea/creatinine, reactive protein and other indicators);
- urine analysis (protein and glucose content, density);
- smear from the site of gangrenous changes;
- Bethe test (placing a piece of tissue in 6% sodium chloride to determine anaerobic gangrene - if the tissue floats, then we can talk about gas gangrene).
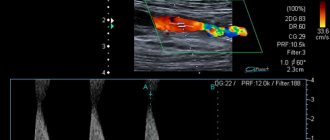
If there are doubts about determining the degree of gangrenous lesion of the limb, then an x-ray or ultrasound is performed. The anaerobic process is confirmed by the presence of gaseous bubbles on the image or computer monitor. All diagnostic measures are carried out quickly to immediately prescribe therapeutic or surgical treatment.
Drug therapy
Treatment methods for pathology are determined on an individual basis. It is usually not possible to restore the affected area. The doctor’s priority task is to determine the causes of the development of pathology and preserve all healthy tissue. If disorders arise as a result of changes in general health indicators, medical measures are usually complex.
If gangrene of the leg is detected in the initial stages of development, the lesion is not huge in scale, you can save the limb and manage with conservative treatment methods. Such therapy usually includes:
- Taking medications to reduce inflammation and block infection in healthy areas. These can be antibacterial agents, complex ointments (Iruksol) and other medications.
- Changing your diet, taking multivitamin complexes and medications to stimulate the immune system. The method of strengthening the body’s protective functions is selected simultaneously by several specialists.
- Physiotherapy. It is considered advisable to use a number of hardware (for example, infrared) to remove dead cells, stimulate the regenerative functions of tissues and prevent the further spread of necrosis.
- Exercise therapy course. Gymnastics is usually prescribed during the rehabilitation period, when drug therapy produces positive results.
If suppuration is present, gangrene of the leg spreads over large areas, it is not possible to do without surgical intervention. In this case, it is important to eliminate all dead tissue and restore the blood supply necessary for proper nutrition of the cells.
Causes of gangrene
- Impaired blood supply to tissues (incorrectly applied plaster, which restricts the movement of blood, heavy pressure on the body. For example, in car accidents or under rubble, when a medical tourniquet is applied for a long time to stop bleeding). Basically, in such cases, the limbs are damaged and a dry type of gangrene develops.
- Diseases of the heart or blood vessels (atherosclerosis, thrombosis and others).
- Bacterial infection (microbes that get into the wound - streptococci, proteus, enterobacteria, etc. can give rise to the disease).
- Frostbite, burns, including chemical burns (in damaged areas, blood supply is disrupted and inflammation begins, which, if infected, can provoke disease).
- Mechanical injuries aggravated by infections.
When is surgery indicated?
Some patients often experience rapid development of necrosis. Sometimes tissue death leads to the “drying out” of the limbs and subsequent infection of the affected area. In such situations, doctors decide to amputate in order to save the patient’s life.
Currently, the following surgical options are used in medical practice:
- Prosthetics. Restoring blood flow through the introduction of a prosthesis is a fairly popular technique. The surgeon installs it in an artery or vessel, due to which blood subsequently flows to all tissues and cells. This option allows you to prevent relapses of pathologies such as gangrene of the leg.
- Treatment with bypass surgery. This is a fairly serious operation. Its main purpose is to allow blood to flow to the tissues through a special shunt - a vessel formed artificially.
- Endovascular surgery. This is a modern technique for restoring vascular patency. The surgeon inserts a catheter with a built-in balloon. The device then moves down the artery to the affected area and dilates it. To avoid re-narrowing, doctors usually install a special stent.
If gangrene of the toe develops due to the presence of plaques that interfere with the normal supply of nutrients, thromboendarterectomy is performed.
Treatment of gangrene is a rather complex process that does not always allow saving a limb. If there are factors predisposing to the development of pathology (diabetes mellitus, blood disorders, mechanical injuries and damage), additional consultation with specialized specialists is required. A special category includes bedridden patients and elderly patients in whom gangrene of the legs is highly likely to develop. Such people require special care and periodic examination to assess vascular patency.
Treatment
This disease is treated surgically. At all stages of treatment of dry or wet gangrene, the doctor’s task is to save the diseased limb and prevent its cutting off. To achieve this goal, a number of therapeutic actions and manipulations are performed.
Drug therapy
The procedure for using medications for each patient with gangrene is determined individually. The affected tissue can no longer be restored. Therefore, the doctor’s task is to determine the cause of the disease in order to prevent infection of healthy areas of the limb.
With early diagnosis of gangrene, the affected area has not yet reached a large size. Then it is possible to save the limb with conservative treatment, including:
- Taking medications to reduce inflammation and prevent infection from spreading to healthy areas. This list includes antibacterial drugs, ointments with complex effects and other medications.
- Changing your usual diet. The patient is prescribed multivitamin complexes and medications to stimulate the immune system.
- Physiotherapy to remove tissue after necrosis and stimulate regeneration, as well as to prevent the spread of necrotic processes.
- Gymnastics during rehabilitation when other therapeutic measures have already had a positive effect.
Surgery
With the rapid development of the infectious process, it is impossible to do without surgery. In the case of dry gangrene, death sometimes occurs spontaneously. But more often the affected area becomes infected. Then, to save the patient’s life, the injured limb is amputated.
Surgery for gangrene is performed in several ways:
- Prosthetics to restore blood flow are performed by implanting a prosthesis into a major vessel. Thanks to this, normal blood supply to the leg is restored and it is possible to prevent relapses of the disease.
- Bypass surgery is also aimed at restoring proper blood circulation. Then a vessel is artificially formed to allow blood to flow to the tissues.
- Endovascular dilatation of blood vessels is intended to restore their patency. The balloon expands the damaged vessel using a catheter. Then a stent is installed in this area to prevent re-narrowing of the walls.
ethnoscience
Doctors advise using white lily oil to treat gangrene. They moisten a cloth with it and apply it to the damaged area in the form of a compress. Every 3 hours, the bandage is replaced with a fresh one and the affected limb is washed with a solution of potassium permanganate.
Rye bread is chewed into pulp and mixed with fine salt. This mass is applied to the gangrenous area in the form of a compress.
Help from traditional medicine
Experienced herbalists recommend using the power of nature to treat gangrene. The most effective and at the same time effective methods include the following:
- White lily oil. This product can be purchased at a pharmacy. Traditional healers recommend soaking a cloth in oil and making compresses. They should be changed every three hours. In between compresses, it is important to rinse the affected area with a manganese solution.
- Rye bread. Pieces of rye bread must be chewed and mixed with a small amount of salt. The resulting mixture can be used as compresses for pathologies such as gangrene of the leg.
- The symptoms of this disease can be relieved with the help of a special ointment. To prepare it, you will need to mix rosin, honey, and laundry soap in equal proportions (approximately 50 g each). After this, the resulting composition must be boiled, add garlic, onion and aloe in the same proportions. The result should be an ointment, which should be heated in a water bath before direct use.
The above recipes should not be used as the only treatment option for gangrene. Moreover, before using traditional medicine methods, you should consult your doctor.
Is home treatment possible?
Necrotic processes should be treated in a hospital. At home, the disease is dangerous and will quickly end in the death of the patient.
Doctors allow some methods of traditional medicine during therapy:
- juniper leaves - sprinkle the affected tissues with powder from the crushed leaves of the plant;
- applications with salt solution;
- using decoctions of medicinal herbs - chamomile, St. John's wort, oak bark to care for the affected limb;
- using aloe juice.
On the Internet there are recipes from healers using the liver of a ram or an ox, ink nuts that appear on oak leaves, chewed bread with salt, and clove oil.
It is impossible to cure a patient with gangrene using these methods. They contribute to delaying the time of contacting a specialist. The result is more extensive surgical intervention or death due to intoxication of the body.
Preventive actions
Many people are interested in what gangrene of the leg looks like (photo). The initial stage of this pathology usually develops slowly, which makes it possible to consult a doctor and undergo a course of treatment. Can this disease be prevented?
First of all, doctors advise observing basic hygiene rules, because gangrene often occurs after infection and dirt penetrate into an open wound. In addition, if alarming symptoms appear, you should immediately seek help from a doctor. Only a qualified specialist after a diagnostic examination will be able to confirm the diagnosis and recommend adequate therapy.
It is important to carefully and promptly treat wound surfaces. If you are at risk of developing gangrene, you must periodically undergo health assessment examinations and promptly treat concomitant pathologies (diabetes mellitus, pancreatitis).