Thrombosis of the arteries of the lower extremities is characterized by blockage of its lumen with a thrombus and insufficiency of local blood flow. Unlike vein damage, arterial thrombosis is a more dangerous pathology, which, in the absence of appropriate treatment, can lead to gangrene and other serious complications.
According to clinical manifestations, several stages of the disease are distinguished, which are characterized by a certain clinical picture. Let's talk in more detail about what arterial thrombosis of the lower extremities is - about the causes, main signs, diagnosis and treatment methods.
Etiology
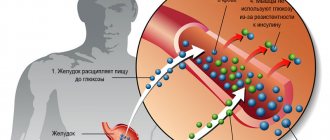
The main condition for the development of vascular thrombosis is the formation of clots on their walls, which gradually increase in size and clog the lumen of the artery. The culprits of these changes are white blood cells - platelets, whose function is to form blood clots at sites of injury, protecting the body from bleeding.
Under certain pathological conditions, platelets begin to stick together and form clots inside the arteries, which settle on their walls - this is how arterial thrombosis of the lower extremities begins to develop.
Basic conditions for the development of arterial thrombosis:
- Injury to the arterial wall is one of the main conditions for the development of pathology. The cause of damage may be surgery or displacement of a bone fragment during fractures. As a result, a special enzyme is released into the blood that promotes the formation of blood clots,
- Tumor processes - according to the observations of clinicians, in oncology, white blood cells are predisposed to increased aggregation and clot formation,
- Excess weight - with obesity, an increased amount of hormones are released into the bloodstream, which can cause platelets to stick together in the lumen of the artery,
- Hormonal imbalances - some sex hormones regulate the vital activity of blood cells; if they are in excess, blood clots can form, leading to the development of this disease,
- Infectious diseases - when organs and tissues are damaged, protective processes are activated, which increases the tendency of white blood cells to stick together. If their concentration in the arteries of the lower extremities is increased, thrombosis may develop.
In addition to the main causes, there are risk factors that can provoke pathology - these are various heart diseases that affect the valve apparatus.
Interesting!
Do not confuse embolism and thrombosis of the arteries of the lower extremities. An embolus is the separation of a blood clot and its movement along the bloodstream; during thrombosis, a clot forms on the vessel wall, which gradually increases and closes its lumen.
At-risk groups
Thromboembolic vascular disease of the legs can be encountered by a patient of any age and gender. For the process of thrombosis to occur, the body must be affected by negative phenomena. These may be pathological processes and external factors that provoke the development of thromboembolism.
The risk group includes people who suffer from the following diseases:
- increased blood clotting;
- atherosclerosis;
- myocardial infarction;
- heart disease;
- diabetes;
- aortic aneurysm;
- vasculitis;
- arrhythmia;
- rheumatism.
External factors contributing to thrombosis and subsequent blockage of the vessel include the following:
- Sedentary lifestyle.
- Poor nutrition.
- Smoking.
- Drinking alcoholic beverages.
- Excess body weight.
- Excessive stress on the legs.
Most patients with thromboembolism are people over 55 years of age, but the risk of developing the disease at a younger age is no less high.
Clinical picture
The disease usually begins acutely, in which a blood clot in the leg artery clogs its lumen. The heart continues to pump and pump blood, in the path of which there is an obstacle. As a result, the first signs of the disease appear, which require emergency care.
Acute thrombosis of the arteries of the lower extremities is almost always associated with arterial embolism and is characterized by:
- Acute pain of a bursting nature, which intensifies when touched,
- The sore limb swells,
- The skin over the affected area is cold and pale to the touch,
- The pulse below the suspected area of blockage is weak or absent,
- There are difficulties in movement in the lower limb, loss of sensation,
- The patient shows signs of shock - chills, cold sweat, and loss of consciousness.
According to statistical data, thrombosis of the iliac artery, located in the upper part of the thigh, is most often detected. When it is affected, the pain is localized in the groin and gluteal region. Thrombosis of the femoral artery, which is located just below, is characterized by pain in the hip area, which increases with flexion.
In both cases, the entire lower limb swells, and the patient is unable to step on his foot. Less common than previous pathologies is thrombosis of the popliteal artery - characterized by swelling below the knee, and the pain intensifies when lifting the foot up or applying light pressure to the calf muscle.
In fact, all three arteries - the iliac, femoral and popliteal - are one long vessel that descends and decreases in diameter. Depending on the size of the embolus, a blockage occurs at a certain level - the largest ones get stuck in the iliac artery, the small ones - in the popliteal vessel.
Prevention
Preventive measures are a guarantee of health. This is especially true for the vascular system, which directly depends on external influences on the body. First of all, it is important to maintain good blood circulation, as well as the elasticity and integrity of the arteries. To do this you should:
- eat right: eat as much fiber, fruits (especially citrus fruits) and vegetables as possible;
- exclude harmful products and cooking methods;
- take vitamins B, AD and C, rutin;
- move a lot, walk more often in the fresh air;
- do morning exercises;
- be as nervous as possible and avoid stressful situations;
- treat viral diseases to the end, observe hospital regime;
- rest more often, get enough sleep;
- toughen up, maintain immunity.
A healthy lifestyle will help maintain your cardiovascular system for a full-fledged working regime. Anticoagulants can also be taken as a preventative measure.
Attention! At an early stage, and also for prevention, you should rest several times a day, raising your legs up at a level of at least 90 degrees. This relieves swelling and has a beneficial effect on blood circulation.
Much attention should be paid to drinking clean water. It is recommended to drink at least 2.5 liters per day. The last dose should be no later than two hours before bedtime. Water cleanses blood vessels, removes “bad” cholesterol, and thins the blood.
Forms of the disease
Symptoms of thrombosis of the arteries of the lower extremities vary depending on the density of blockage of the artery lumen and circulatory disorders in the lower extremity. Therefore, doctors distinguish several degrees of development of the disease.
Interesting!
According to ICD 10, this pathology is assigned the code “I 74.3 – embolism and thrombosis of the lower extremities.
First stage
It is characterized by the appearance of slight pain, which may intensify during physical activity. In some clinical cases, slight pain is noted at rest.
Second stage
This degree is divided into several subcategories:
- II A – there is pain, limited movement in the legs, but the ability to move is preserved. A decrease in muscle strength and general activity is recorded,
- II B – paralysis is registered, but movements at rest are preserved,
- II B – swelling of the legs is added to the listed symptoms, the feet remain unchanged.
Third stage
This is the last stage of arterial thrombosis and requires urgent assistance from medical staff:
- III A - severe damage in which the legs are swollen, the skin is pale and cold, the patient cannot move his fingers and feet,
- III B – the described symptoms are accompanied by a lack of mobility in the entire lower limb.
Symptoms and signs
Pathogenesis is closely related to the cyclical development of the disease. At the zero or first stage there are actually no special signs. Sometimes there are sensations of internal “pulling”, bursting. The next stage will be associated with pain and a decrease in the sensitivity of the skin. This is followed by complete numbness, dramatic changes in skin color, and gangrene of the lower extremities.
In parallel with the above symptoms, the following may occur:
- increased temperature and blood pressure;
- paroxysmal pain;
- swelling, puffiness of the legs;
- problem with joint extension;
- amyotrophy.
All of the above symptoms do not arise spontaneously, but come as the diagnosis develops.
Diagnostics
To identify pathology, an examination by the attending physician is required, as well as some laboratory and instrumental examination methods.
- Upon external examination or identification of signs in the photo - the limb is pale, swollen - the main swelling is noted in the lower leg area,
- MRI or ultrasound are informative methods that allow you to diagnose pathology and identify the affected area,
- Ultrasound Dopplerography or duplex angioscanning - show the condition of blood vessels,
- X-ray with a contrast agent - prescribed additionally, allows you to see the location of the blockage,
- Blood testing is necessary to detect special enzymes and proteins that indicate thrombosis.
If there is a suspicion of thrombosis of the arteries of the lower extremities, the patient is subject to urgent hospitalization.
Treatment
Drug therapy for thrombosis is indicated only in the first stage of the disease, under the strict supervision of the attending physician. In severe cases, surgery is indicated to improve blood circulation in the limb.
Types of operations
Treatment of thrombosis of the arteries of the lower extremities in acute form, as well as at stages II-III, is possible only through surgery. The choice of type of surgical intervention depends on the patient’s condition and the extent of the lesion.
Type of operations:
- Classic thrombectomy is the removal of a blood clot from an artery using a scalpel and auxiliary surgical instruments. Indicated in emergency cases when blood circulation in the lower limb is severely impaired. The main danger is the possibility of bleeding,
- Radio wave thrombectomy is a more modern method, based on the dissolution of a blood clot using radio waves. Eliminates serious complications, but this operation is carried out as planned,
- Bypass surgery is the creation of a “backup” path along the blood flow, bypassing the affected area. It is carried out in cases where there is a high probability of a blood clot breaking off and entering the bloodstream.
Rehabilitation after surgery
After surgery, there is usually swelling and pain in the operated limb. For the purpose of recovery, bed rest is indicated for several days, then the patient is allowed to get out of bed using special medical devices.
During the first 2 weeks, all loads are strictly contraindicated, as they can provoke the formation of new blood clots. For successful recovery after surgery, the patient must follow all the recommendations of the attending physician.
On a note!
To prevent relapses of the disease, it is necessary to prevent thrombosis - lead an active lifestyle, monitor your diet, and give up bad habits.
Emergency help
When emergency care is provided, hospitalization is performed and surgery is performed to eliminate the blood clot that is in the vessel. Until the ambulance arrives, the patient must be in a horizontal position. Movement or physical activity is prohibited. When a clot blocks the popliteal and femoral arteries, direct access is used. If thromectomy is performed, an endovascular approach is necessary. After the operation, the patient needs special treatment. During it, tissues are restored and blood flow in the lower extremities is normalized. To prevent illness, you must follow the advice of the doctor who is treating you. When there is a possibility of high risk due to a clot blocking an artery, compliance with preventive measures is important. You must regularly take medications prescribed by your doctor.
These measures are especially necessary in case of damage to the pelvic artery, when the pathological process can affect the entire limb. The only emergency help is hospitalization and surgery to remove the blood clot from the blood vessel. Before the ambulance arrives, the patient must take a horizontal position. It is strictly forbidden to move or perform physical activity. When the popliteal and femoral arteries are blocked by a clot, direct access is used. Endovascular access is used when performing thrombectomy from small leg veins. After surgery, the patient needs special therapy. Its goal is to restore tissue and normalize blood flow to the legs at the local level.
In a medical institution, doctors perform basic therapeutic measures:
- Provide artificial ventilation.
- A catheter is inserted into the blood vessel.
- Bed rest is prescribed.
- Blood pressure is measured regularly.
- Heparin is administered (10,000 units).
- Dopamine, anesthetics, antibiotics are administered (if necessary)
- Saline solutions are administered.
- For hypotension, Eufillin is administered.
After examination, the doctor prescribes conservative therapy, and in advanced cases, the disease is treated with surgical methods.
Help with acute arterial thrombosis
The purpose of assistance is to reduce blood viscosity and dissolve the blood clot. For this purpose:
- Intramuscular injections of Halidor,
- Intravenous infusions of Heparin,
- Placement of a dropper with saline solution - to dilute the blood and reduce its viscosity.
Thrombosis of the arteries of the lower extremities is a dangerous pathology in which serious circulatory disorders occur. In the event of an acute condition, it is necessary to immediately seek medical help - even in the case of serious injuries, timely surgery will avoid gangrene.