Etiology of the disease
Long-term studies have made it possible to study in detail the symptoms and mechanisms of development of various forms of telangiectasia. Based on the data obtained, three main causes of telangiectasia were identified. One of the main reasons is hormonal imbalance with increased production of estrogen. An excess of the hormone provokes the expansion of the lumen of the veins. The change in their appearance is clearly visible on the faces and in photographs of women during pregnancy.
The next cause of telangiectasia is considered to be dysfunction of the heart, which reduces the elasticity of the walls of blood vessels. As a result, their uneven narrowing and expansion is observed. With pathological changes, the blood is unable to circulate normally, creating excessive pressure in the surface capillaries and forming a reddish spot.
The third cause of telangiectasia is genetic predisposition. Red spots on the skin are explained by the special sensitivity of the circulatory system, transmitted at the genetic level. In this case, hereditary hemorrhagic telangiectasia manifests itself even in newborns and infancy.
This does not mean that with single manifestations of the listed factors, vascular networks will necessarily arise. Basically, pathology develops after prolonged exposure to certain established diseases:
- Radiation type dermatitis.
- Mastocytosis: cutaneous, systemic.
- Xeroderma pigmentosum.
- Phlebeurysm.
- Louis-Bar syndrome, also known as ataxia telangiectasia.
- Raynaud's disease.
- Catarrhal gingivitis.
- Rosacea and similar chronic diseases.
One of the causes of the disease is dysfunction of the heart.
The disease also occurs in completely healthy people under the influence of certain factors:
- Excessive exposure to the sun, in solariums.
- Drinking large amounts of alcohol.
- Exposure to chemicals and carcinogens.
- Smoking.
- Taking hormonal drugs.
- Increase physical activity.
Depending on the initial state of the veins, telangiectasia can manifest itself both under the influence of a single cause or a group of them.
Other classifications of telangiectasia
Depending on the type of affected vessels, telangiectasia is distinguished:
- arterial,
- venous,
- capillary.
Capillary and arterial ones are distinguished by their red color, small diameter (0.2 mm or less), and lack of elevation above the surface of the skin. They can turn into venous when pressure increases and blood flows from the venules.
Venous ones are characterized by a blue color, a larger diameter, and the formation of nodules protruding above the skin.
There is a division according to shape and color:
- spotted - more or less bright spots of pink and red shades;
- tree-like - the pattern corresponds to the name, often have a dark blue color, predominant localization on the legs;
- “stars” and “spiders” - rays radiate from one point to the periphery, usually red;
- linear - straight or curved short stripes of bluish or red color, more common on the face.
Therapy methods
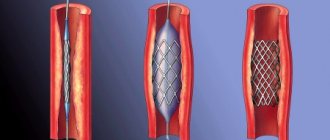
It is a method in which a specialist injects a sclerosant into the affected area using a thin needle. Under its influence, a strand is formed in the capillaries, which dissolves over time.
The main advantage of the procedure is that it leaves no visible marks.
Sclerotherapy for telangiectasia has several types:
- Microsclerotherapy. Combines the standard technique with cold wrap. Prescribed for the restoration of the reticular vein. To obtain a positive effect, 2-5 sessions are sufficient.
- Microfoam. Unlike the classical procedure, effective foam is used as a sclerosant, which is evenly distributed over the affected area of the vessels.
- Segmental. Indicated for varicose veins. Eliminates telangiectasia after 2-3 sessions, but has a temporary side effect - hyperpigmentation, which disappears a few weeks after treatment.
- Echosclerotherapy. Treatment of telangiectasia is carried out when localized on the legs, using a duplex scanner.
The advantage of therapy is that such an effect does not leave visible marks. It allows you to remove up to 50% of pathological vessels in one session. The final result appears a month after the start of the course. The only drawback of the technique is its superficial action, without eliminating the underlying cause of the pathology.
The laser is used to eliminate telangiectasia on the face as an independent option or in combination with other treatment methods when a large area is affected. The essence of the method is the targeted effect of a heat ray on pathological vessels, during which their walls are destroyed. The radiation technique is performed once or several times with an interval of 2 months.
Laser treatment of the disease is painless and leaves no scars; even a child can easily tolerate it. During the postoperative period, slight swelling is allowed to occur, which goes away within a few days. Unlike sclerotherapy, laser coagulation does not require wearing compression garments during the rehabilitation period.
This treatment method does not leave scars on the patient's skin.
Indicated for the diagnosis of telangiectasia of the lower extremities. The principle is to stimulate blood vessels with high-frequency alternating current. It is brought down using special thin needles. The procedure provokes their narrowing and coagulation of the blood in them. As a result of this process, crusts appear at the site of the vein lesion, which fall off within 10 days after electrocoagulation. Removing the crusts yourself will lead to the formation of visible scars.
Ozone therapy
Another alternative method for removing mesh is ozone therapy. The technique is recommended for lesions of facial vessels, especially in the cheek area. The procedure involves administering a microdose of ozone by injection directly into pathological veins. To administer the product, microcatheters are used to prevent ozone from reaching surrounding tissues. Ozone narrows the lumen of the capillaries and gradually sticks them together, preventing blood flow from entering.
To completely eliminate the problem, it will take from 5 to 15 sessions.
Depending on the degree and volume of the problem, it may take from 5 to 15 sessions, conducted at intervals of 3-7 days, to completely eliminate it. Symptoms of the disease decrease in intensity after just a few procedures. The therapeutic process takes place without pain and discomfort due to the analgesic properties of ozone.
Simultaneously with the elimination of the consequences of telangiectasia, metabolic processes are restored, improving the condition of the skin. The advantage of ozone therapy is that it can be used to treat telangiectasia in children and women during pregnancy.
Despite the variability of treatment methods for various forms of telangiectasia, each of them is intended to relieve a specific type of this disease. Therefore, the attending physician must select a method, taking into account the characteristics of the pathology, cause and patient’s body.
It must be remembered that the effectiveness of treatment will only be in relation to a cosmetic defect, which may arise again in the absence of treatment for the root cause of the disease.
Irina, 32 years old: “How I got rid of spider veins in 2 weeks + PHOTO”
- Description of the disease
- Causes of telangiectasia
- Symptomatic manifestations of the disease
- Methods for detecting and treating telangiectasia
- Methods for diagnosing the disease
- Methods of treating the disease
- Preventive measures
Types of disease
Primary and secondary telangiectasia will manifest itself on the lower extremities and face. The doctor’s task is to analyze the factors that became the starting point in the development of the disease.
| Criterion | Primary (hereditary) | Secondary (acquired) |
| Period of occurrence | Early childhood | No age or time restrictions |
| Kinds | Most of the surface of the skin is covered with “stars”. Mucous surfaces are not affected | Likewise |
| Hemorrhagic - pathology is localized on mucous surfaces. “Stars” are visible on the fingertips, in the brain, on the feet. | ||
| Nevoid – traces of pathology are visible near the cervical nerves | ||
| Generalized essential - pathology first makes itself felt in the area of the feet. Gradually the “stars” “rise” to the neck | ||
| “Marble” - signs are noticeable in the baby immediately after birth. Symptoms will become more pronounced with mental or physical stress | ||
| Ataxia – symptoms are noticeable in children under 5 years of age. “Stars” are located in the auricle and near the nose |
On a note! Secondary or acquired telangiectasia has no subtypes. The exception is the nevoid variety.
Specific subtypes of the disease
They are diagnosed less frequently than the types listed above. The reason will be the presence of a concomitant disease:
- Dermatomyositis - the patient has multiple dilated capillaries. Location: fingertips. The patient complains of severe pain.
- Scleroderma - spots have the shape of a polygon or oval. Spots are found on mucous surfaces, face and hands.
- Lupus erythematosus - symptoms of telangiectasia are visible on the nail plates.
Rendu-Osler disease will complicate the course of hereditary telangiectasia. “Stars” are noticeable on the surface of the nose, the mucous membrane of the bronchi, and the gastrointestinal tract.
Description of the disease
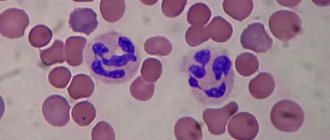
Telangiectasia is a cosmetic disease. What is it - telangiectasia of the lower extremities? This disease is characterized by the manifestation of blood vessels on the skin of the legs, either congenital or acquired. Protruding capillaries or veins exist in the form of individual lesions or in the form of large plexuses affecting large areas of the skin. Spider veins vary in color and size. Such differentiation depends on what type of vessels loses elasticity.
Telangiectasia is a cosmetic disease.
For example, when arteries and capillaries are damaged, the mesh looks like a spider web of thin threads of red shades. And if the venous vessels are affected, the mesh appears in the form of blue or purple spots.
In some cases, telangiectasia can affect several types of vessels at the same time.
Telangiectasia (examples in the photo) has been recorded in the following manifestations:
Irina, 32 years old: “How I got rid of spider veins in 2 weeks + PHOTO”
- In the shape of red stars with a pronounced center inside and thin cobwebs radiating from it.
- Tree-shaped, deep blue color.
- Like red or blue lines.
- In the form of spots, most often red.
Women suffer the most from this unpleasant skin formation. At the same time, cases of telangiectasia of the lower extremities also occur in newborns. With age, the risk of spider veins increases. The disease is characterized by relapses even after complete recovery.
Classification
According to their shape, spider veins can be:
- Stellate (or arachnid). They are a spot (usually red) from which a network of capillaries radiates.
- Tree-like. Typically appearing on the skin of the legs, they resemble tree branches and are dark blue, blue or purple in color.
- Spot-like. Often accompanied by collagenosis and other skin pathologies, they appear as bright red spots.
- Linear (or sinusoidal, simple). Appear on the face and appear in shades of blue or red.
Depending on the type of vessels affected, telangiectasias can be:
- capillary – capillaries are dilated;
- arterial – arterioles are dilated;
- venous – venules are dilated.
Spider veins can be a primary or secondary syndrome.
The first group includes the following telangiectasia:
- hereditary hemorrhagic - blood mesh appears on the mucous membranes of the mouth, nose, feet and fingertips; with progression, they can appear in the gastrointestinal tract, brain and bronchi;
- hereditary - blood mesh appears only on the skin and never affects the mucous membranes;
- invisible - small blood networks appear only in the areas of the cervical nerves;
- marbled skin - red blood networks appear on the skin from birth, and their pattern becomes brighter during psycho-emotional or physical stress;
- generalized essential - blood networks begin to spread from the feet, rise upward, covering all the legs;
- ataxia - blood networks appear in early childhood (about 5 years) on many parts of the body and mucous membranes.
The second group includes the following telangiectasias:
- disturbances in the synthesis of collagen and estrogen;
- basal cell skin cancer;
- solar keratosis;
- reaction to transplants.
Causes of telangiectasia
Telangiectasia, the causes of which are congenital or acquired, is determined by the disturbed state of the blood vessels.
One of the main causes of acquired disease on the legs is impaired blood circulation.
The following genetic factors are identified that influence the formation of congenital vascular pathology:
- neuroangiopathy (vascular damage as a consequence of a general disease);
- infantile hemangioma (benign vascular tumor);
- poikiloderma (brown pigment spots);
- vascular nevi (pathological processes of development and proliferation of blood vessels).
One of the main causes of acquired disease on the legs is impaired blood circulation. In the process of losing elasticity and strength, the vessel stretches, the blood passing through it increases the pressure in its cavity, as a result of which it expands, creating a striking pattern.
Other factors that influence the appearance of acquired vascular pathology:
Irina, 32 years old: “How I got rid of spider veins in 2 weeks + PHOTO”
- varicose veins;
- infectious diseases;
- hormonal changes;
- physical damage to the limbs;
- skin diseases.
The main manifestation of the pathology is protruding blood vessels.
People with healthy and strong blood vessels from birth may experience symptoms of this disease if they abuse sunbathing, visiting a solarium, or have an unhealthy lifestyle.
Symptomatic manifestations of the disease
Symptoms depend on the cause of the formation of the spider veins, since telangiectasia is the body’s response to the effects of a disease or external factors. The main manifestation of the pathology is protruding vessels, which are characterized by the following signs:
- the size can vary from 0.2 to 5 centimeters;
- color - from light shades of red to dark tones of blue;
- In some cases, itching sensations may occur.
Telangiectasia is caused by various diseases, but its appearance can be recognized by some common signs:
- swelling of the affected area of the legs;
- feeling of heaviness in the limbs;
- skin rash;
- high sensitivity of the integument;
- state of malaise.
If you notice a venous network on your legs, do not hesitate to visit a doctor.
Telangiectasia of the lower extremities is often expressed symmetrically, that is, both legs are affected. Typically, spider veins are located in areas under the knees, thighs, lower legs, ankles or feet. This disease does not cause pain, but it affects the appearance of the legs and is a clear indicator of vascular problems. It is very important, having noticed a venous network on the legs, not to hesitate to visit a doctor, who, with proper examination, will be able to diagnose the cause of this pathology and begin appropriate treatment.
What is telangiectasia
Those skin lesions that are hidden under the popular names “spider veins” or “vessels” are telangiectasias. These are very overstretched capillaries, the diameter of which is 5 times greater than the diameter of their normal “brothers”.
Just as a runny nose or cough is not a disease, but the body’s reaction to a disease, so vascular telangiectasias are signs of various disorders occurring in the body.
Expert comment:
“Many people believe that telangiectasia on the face or body is an unpleasant but harmless phenomenon. In fact, it is important to distinguish them by origin. There are hereditary telangiectasia, and there are acquired ones.
If you inherited blood vessels on your face, they are relatively harmless.
Acquired telangiectasia is formed under the influence of various factors: hormonal imbalance, certain infections, vascular problems, solar radiation; may be a symptom of lupus erythematosus, rosacea, etc.
But regardless of the reason, any vascular pattern has a tendency to grow and increase. Therefore, you cannot let them out of your attention zone!
Anna Smirnova, dermatocosmetologist at the Platinental Medical Center.
It is also important to remember that if telangiectasias are located on the body, especially on the legs, this is a symptom that should be dealt with by a phlebologist, since any vascular pattern in this case is a sign of a problem with the vessels or veins.
Facial vessels most often represent manifestations of rosacea.
A cosmetic defect can be removed quite easily. But in order to avoid the formation of a new vascular network, you will need to first eliminate the causes of rosacea.
Laser treatment of rosacea - intravascular coagulation using a Fotona Nd:YAG neodymium laser.
Methods for detecting and treating telangiectasia
If barely noticeable blood vessels appear on the skin, you should immediately consult a therapist. First, the doctor must determine the factor that influenced the change in the strength of the veins or capillaries. Having previously established the degree of influence of the factor, the therapist will refer the patient to a specialist who will help eliminate the consequences of the pathological process.
Irina, 32 years old: “How I got rid of spider veins in 2 weeks + PHOTO”
The main symptom of telangiectasia refers to those that are detected without any auxiliary instruments. An accurate diagnosis is determined using urine and blood tests. If necessary, internal organs are examined. In order to determine the nature of damage to the walls of blood vessels, the following diagnostic methods are used:
An accurate diagnosis is determined using urine and blood tests.
- Ultrasound using the Doppler effect: measure the density of the walls, as well as the characteristics of blood movement in the cavity of the vessel;
- rheovasography: check the quality of blood flow and determine the cause of telangiectasia;
- other tests that are used to identify damage to the internal organs of various body systems.
Treatment of this disease is aimed at eliminating vascular weaves on the legs in combination with measures aimed at getting rid of the cause of the appearance of such a defect on the skin. Telangiectasia, the treatment of which depends on several factors, is largely a problem with the appearance of the legs. The choice of method for getting rid of it is influenced by the severity of the vascular network. They use conservative therapy, traditional medicine recipes, and sometimes resort to surgical intervention.
Conservative procedures include:
Methods of treating the disease
- Sclerotherapy. The principle of operation of the method is to inject a substance of a chemical composition that eliminates stretched areas by gluing adjacent areas inside the cavity of the vessel. The procedure comes in several types: microsclerotherapy (about 5 procedures are performed that restore the reticular veins) and segmental sclerotherapy (up to 3 procedures are performed with a targeted effect on the segmental veins).
- Echosclerotherapy. Using a scanner, stretching of the walls of the communicating veins is eliminated.
- Sclerotherapy of the postoperative period. In special cases, this type of sclerotherapy is used as an additional therapy after surgical treatment.
- Coagulation. This is a physical-chemical process aimed at combining small particles into larger ones.
- Electrocoagulation. By touching the affected area with a needle through which a high-frequency electric current passes, the too thin walls of the vessel are connected and a kind of patch is formed.
- Laser coagulation. Using high temperatures, a laser beam connects the weak walls of blood vessels, while the effect is directed only to the affected tissue.
- Cryocoagulation. The principle of operation of this procedure is the effect of low temperatures on the affected areas of the skin.
In addition to the procedures described above, drug treatment is additionally used.
Stages of varicose veins of the lower extremities with photos
In especially severe cases, operations are performed to remove the affected areas of the vessels, followed by prosthetics.
Some patients resort to using traditional medicine recipes. These methods include:
- ointments prepared at home from natural ingredients;
- foot baths with the addition of decoctions and infusions of medicinal herbs;
- compresses, from which a lotion is extracted using apple cider vinegar.
Spider veins - symptoms and treatment
The choice of treatment method depends on the form of the disease, the experience of the surgeon and the patient's preferences.
If the patient is concerned about the appearance of the affected skin, then methods for removing telangiectasia are used.
Sclerotherapy is the most popular and one of the most effective methods for removing spider veins. A special drug is injected into telangiectasia - sclerosant, which acts on the vascular wall from the inside. This leads to gradual gluing of the vessel. After some time, no traces of the disease remain on the skin.
Sclerotherapy can be used on very thin and small telangiectasias, as well as on large veins and even on the trunk of the great saphenous vein. The most common area of application for sclerotherapy is the lower extremities. As a rule, lauromacrogol acts as a sclerosant. When used correctly, sclerosant causes only a local effect and does not have a toxic effect on the body. Immediately after exposure to the sclerosant, a specific clot (sclerothrombus) forms in the lumen of the vein, the vessel becomes dense, after which the process of resorption of the vein begins, which can take up to six months.
Sometimes an oxygen-ozone mixture acts as a sclerosant. In this case, the procedure will be called ozonosclerotherapy. Another popular option for sclerotherapy is cryosclerotherapy , which involves cooling the skin at the site of sclerosant injection using ice or cold air.
Laser cryotherapy (CLaCS) is gaining popularity - a method that combines cryotherapy, sclerotherapy and laser coagulation (narrowing) of veins. The affected vessel is exposed to a transcutaneous (percutaneous) laser, causing spasm of the vein. Next, a sclerosing compound is injected into the lumen of the vein. All manipulations are carried out under the influence of cryotherapy, which reduces pain in the patient. The results of this method are approximately comparable to the effectiveness of conventional sclerotherapy, therefore, given the higher cost of treatment, the need for it remains doubtful.
There are methods for treating telangiectasias using transcutaneous laser photocoagulation . This method is most often used on the facial skin and is safer than sclerotherapy, but less effective since spider veins often return.
It is important to note the possible complications of sclerotherapy . One of them is a cough after the injection of sclerosant into a vein (usually a large one). Part of the drug enters the deep veins, penetrates through the bloodstream into the pulmonary trunk and capillaries of the lungs, causing microembolism (clogging with small particles), which reflexively provokes a cough and a burning sensation in the respiratory tract. This complication is not life-threatening and usually resolves on its own within a few minutes.
Often after sclerotherapy, hyperpigmentation and bruising at the injection site appear, which disappear on their own within a few days [11][12][13].
Preventive measures
There are practically no specific measures to prevent telangiectasia. But to prevent the appearance of spider veins, the following is recommended:
- wear compression stockings;
- avoid too tight shoes and tight trousers, jeans and other things;
- use appropriate creams or ointments to strengthen the walls of blood vessels;
- Do not expose your legs to excessive physical activity.
You should pay attention to external factors that can trigger the formation of spider veins. The main thing is to immediately consult a doctor if there are pronounced blood vessels on the legs.
Modified, dilated small vessels (telangiectasia) due to circulatory disorders can appear on any part of the body. Spider veins on the legs occur when the capillary walls, thinned for one reason or another, can no longer cope with the pressure of venous blood, expand and burst. Small wreaths become visible on the surface of the skin. As a rule, dilated capillaries form a venous network, but there are also individual varicose veins of different shapes and sizes.
Diagnostics is carried out in several stages
The doctor examines the spider veins. Its goal is to determine the type of pathology. The list of techniques used and the duration of the course depend on the patient’s health condition. The second factor is the presence of concomitant diseases. Additionally, consultations with doctors of related specialties are prescribed:
- gastroenterologist;
- gynecologist;
- urologist;
- cardiologist;
- dermatologist;
- endocrinologist;
- rheumatologist.
Based on the information collected, a diagnosis is made:
- Capillary type - signs of telangiectasia occur in the patient’s legs. Visually they resemble tree branches. The predominant color is blue, violet, blue.
- Venous - visually resemble a spot. Pathology accompanies dermatological inflammatory processes. Bright red spots cover the upper or lower limbs.
- Arterial - a spot forms on the skin. The grid diverges from it in different directions. The predominant color is red-blue or bright red.
- Sinusoidal (linear) - occurs on the face. Red or blue spots cover up to 1/3 of the skin surface.
Having completed the examination, the doctor proceeds to study the symptoms. The more accurately the diagnosis is made, the higher the effectiveness of therapy.
Causes of telangiectasia
To a greater extent, spider veins on the legs bother women aged 30-40 years. Men pay less attention to such defects, although they do not occur much less frequently than women. With age, the walls of the capillaries located in the epidermis become thin, the vessels lose their elasticity, and become more vulnerable. Sometimes symptoms appear in women at an earlier age.
The main reason for the appearance of spider veins is hormonal imbalance.
This is why stars and capillary networks occur more often in women than in men. Why is this happening? Pregnancy, childbirth, abortion, menopause - all these conditions change hormonal levels, as a result of which the risk of star formation increases. The balance of hormones changes if you take pills for a long time - oral contraception or hormonal medications.
Causes not related to hormone imbalance:
deep vessel diseases;
In addition to the internal causes of the formation of reticular phenomena on the legs, there are a number of unfavorable factors that provoke pathological changes in the functions of the capillary system and deformation of blood vessels. These include:
- Increased stress on the legs (wearing high-heeled shoes, a profession that requires walking and standing all day).
- Bad habits (smoking, drinking alcohol).
- Poor nutrition.
- Overweight.
- Excessive passion for solarium, sunbathing.
- Sedentary lifestyle.
- Intense physical activity.
It is strictly not recommended to use medications on your own.
Telangiectasias on the legs come in different types, sizes and shapes. Taking into account the etiology, they are classified into capillary, venous and arterial. Accordingly, in order to cure blood vessels, you need to use different means, use conservative and surgical techniques.
This form of telangiectasia is called mixed.
Regardless of the type of spider veins, they do not cause pain in the localized areas. The painful form of such formations is extremely rare. Most often observed in women. It is characterized by minor pain during critical days, a change in the color of the vessels to a brighter one. Painkillers for their treatment are selected individually and are included in the complex of conservative therapy.
Before prescribing treatment for spider veins, the phlebologist uses special diagnostic measures to assess the condition of the peripheral vessels and the intensity of venous blood flow. In addition to visual examination, diagnosis of vascular diseases is carried out using Doppler ultrasound.
The study allows you to make an accurate assessment of the condition of the walls of blood vessels, determine the speed of movement of venous blood and identify areas of localization of stagnation. Next, differential diagnosis is carried out to determine the root cause of the disease, and a functional study of the functioning of the liver, heart, ovaries and uterus is also carried out.
Methods and means for treating telangiectasias are selected based on the results obtained. But first it is necessary to cure the concomitant disease that caused their appearance. The patient is prescribed appropriate medications, tablets for oral administration, and ointments for external treatment are prescribed. Further treatment of spider veins on the legs depends on the location, type and severity of telangiectasia.
Modern medicine offers to treat pronounced, multiple spider veins using:
- sclerotherapy;
- laser photocoagulation.
Sclerotherapy or compression phlebosclerosis. During the procedure, a scleroizing agent is injected into the modified vessels. Under the influence of sclerosant, the vessel sticks together and the blood flow through it stops. Redness and slight swelling of the skin occurs in the injection area. The doctor presses the injection point with a tampon and secures it with a bandage. A compression bandage or compression stockings are placed on the leg. After 1–1.5 months, the stars disappear.
Laser photocoagulation. A luminous flux of a certain intensity heats the walls of the dilated vessel, as a result of which they become soldered and close the lumen of the capillary. The blood flow stops, the vessel regresses and the stars disappear.
The procedure is painless and is performed without the use of local anesthesia. Dilated vessels with a lumen diameter of up to 2 mm can be treated using laser photocoagulation. Minor vascular deformations can be eliminated with 1-2 laser therapy procedures. Strong changes require more sessions.
Why do spider veins appear on the legs?
Telangiectasia on the legs appears with varicose veins and chronic venous insufficiency. However, it is also possible without the participation of varicose veins.
The reasons are considered:
- “standing” work;
- hormonal disorders;
- overload of the veins when lifting heavy objects or under one’s own weight;
- unfavorable heredity.
In all cases, the tone of the superficial venous vessels suffers, insufficient blood outflow is transmitted to the level of the venous section of the capillaries, and they expand.
Telangiectasias are considered the initial stage of varicose veins. Most often accompany pregnancy and remain after childbirth. In women, in addition to cosmetic problems, there is increased fatigue in the legs, moderate swelling in the evening.
Causes of spider veins
If you approach this issue from a medical point of view, it turns out that there are enough reasons for the occurrence of spider veins:
- Vein diseases and phenomena of chronic venous insufficiency;
- Hormonal imbalance and diseases of the endocrine system;
- Previous pregnancies and a large number of abortions in history;
- Taking hormonal contraceptives high in estrogen;
- Connective tissue failure (congenital or acquired);
- Impaired removal of metabolites from the body in liver diseases;
- Pathology of the heart and blood vessels;
- Hypovitaminosis of vitamin C, causing increased permeability of vascular walls;
- A lifestyle with low physical activity or prolonged standing.
The presence of TAE on the body is a signal for a full examination and treatment by a specialist, and not just removal as a cosmetic defect. Spider veins on the legs usually do not cause any complaints other than an aesthetic defect, but the affected area can be significant, so every person is looking forward to getting rid of the problem.
Since the lesion can affect both arterial and venous vessels, the mesh on the legs can be of different colors - from bright red to bluish. Telangiectasias can be flat or raised above the surface of the skin, have many variations in size and shape (tree-shaped - often observed on the lower extremities, spotted, linear, stellate).
Causes
Some people believe that spider veins appear due to diseases of the heart and blood vessels, but this is not true. This stereotype has been refuted by independent studies, which have found that capillary dilation is most often caused by varicose veins or hormonal imbalances.
The appearance of telangiectasias can be caused by the following disorders and diseases:
- varicose veins;
- pigment xenoderma;
- Raynaud's disease;
- rosacea;
- radiation dermatitis;
- chronic skin diseases;
- basal cell skin cancer;
- diseases accompanied by ataxia;
- cardiovascular pathologies;
- prolonged exposure to ultraviolet rays;
- carcinogens;
- taking corticosteroids;
- taking oral contraceptives;
- hormonal imbalance;
- hereditary predisposition, etc.
In some diseases, spider veins manifest themselves in a special way:
- with scleroderma, telangiectasias have a speckled appearance, are represented by multiple oval or polygonal spots, and are localized on the hands, face and mucous membranes;
- with dermatomyositis, telangiectasias are accompanied by significant dilation of capillaries, are located on the fingertips and are painful;
- with systemic lupus erythematosus, telangiectasias are hyperpigmented and observed on the nail folds;
- in Randu-Osler disease, hemorrhagic telangiectasias often have hereditary causes and are localized on the mucous membranes of the digestive organs, bronchi, tongue and nasal skin.
Spider veins in themselves are not dangerous to health. Its appearance is one of the pathology syndromes that needs treatment.
Telangiectasias rarely appear in people with elastic vessels, but even in such cases, certain factors can cause capillaries to dilate. Such aggressive influences include:
- sudden changes in temperature;
- sun rays and visiting a solarium;
- excessive physical activity;
- smoking;
- alcohol;
- vitamin deficiencies.
How to remove spider veins on the legs?
What to do if spider veins appear on your legs? Do not panic and consult a phlebologist. An experienced doctor will examine the affected area, ask clarifying questions and prescribe additional research methods to assess the condition of blood vessels (USD) and determine the cause of the disease. Taking into account the characteristics of the patient’s health condition, the doctor will prescribe invasive or conservative treatment to remove spider veins on the legs. Conservative treatment methods include:
- wearing compression stockings;
- drug therapy;
- lymphatic drainage massage;
- physiotherapy.
Diagnostics
Using ultrasound, the doctor can assess the condition of the vascular system.
At the first signs of telangiectasias, you should contact a phlebologist. During the first visit, the doctor must:
- will study the patient’s complaints, medical history and family history;
- examine telangiectasia and blood vessels of the legs;
- will conduct Doppler ultrasound of the blood vessels of the legs.
Based on the results, the doctor will be able to prescribe treatment or consultation with additional specialists (endocrinologist, gynecologist, rheumatologist, cardiologist, dermatologist, gastroenterologist, etc.). Finding out the cause of telangiectasias is an extremely important part of the examination, since eliminating spider veins alone does not solve the health problems that caused them.
Invasive methods will help more effectively and quickly remove spider veins on the legs:
- sclerotherapy;
- microsclerotherapy;
- microfoam Foam Form sclerotherapy;
- ECHO sclerotherapy;
- percutaneous laser coagulation.
If there are contraindications to the use of a laser, the clinic’s phlebologists will select another suitable method for treating telangiectasia for the patient. All treatment methods are carried out on an outpatient basis and are painless. The clinic’s vascular surgeons have been helping patients with vascular disorders for many years and know how to remove spider veins on the legs forever. Doctors also pay great attention to the prevention of relapses and explain in detail to their patients how to behave after removal of the defect.
The clinic's doctors work only with certified modern equipment and use proven medications.
Rehabilitation period
All methods for removing spider veins are distinguished by the fact that after the manipulation you can quickly return to your normal lifestyle. It is not recommended to visit the bathhouse and sauna for 2-3 weeks, massage the affected area, or stay in the sun for a long time. Those patients who have undergone sclerotherapy are advised to wear compression garments for several weeks.
If electrocoagulation has been performed, then a special cream must be applied to the skin for 7-10 days. A thin crust forms at the site of cauterization of the vessels, which disappears after 2 weeks. It is also not recommended to rip it off ahead of time.
Recovery period
Its duration depends on the method used by the doctor. Minimally invasive microsclerotherapy will require compliance with restrictions for 3 weeks. The patient does not go to the bathhouse or sauna. The off-limits list includes the beach. The recommendations listed below continue:
- refusal of decorative cosmetics;
- avoidance of alcohol-based cosmetics;
- use sunscreen on the treated area of skin;
- the skin is not overcooled;
- after removal of blood vessels on the lower extremities, the patient wears compression garments;
- temporary refusal from active sports.