What is systemic lupus erythematosus?
Systemic lupus erythematosus (SLE, Libman-Sachs disease) is a complex diffuse connective tissue disease characterized by systemic immune complex damage. With it, the body’s immune system begins to perceive its own cells as hostile and begins to suppress them.
Lupus erythematosus is a chronic disease that provokes a number of inflammatory processes in the joints and muscles, damaging the microvasculature.
The disease received its name because of its characteristic feature - rashes on the bridge of the nose and cheeks (the affected area is shaped like a butterfly), which, as was believed in the Middle Ages, resembles the sites of wolf bites.
During the course of the disease, a person forms antibodies with personal DNA, nDNA-antibody complexes and nDNA-compliments are formed, which are deposited on the kidneys, skin and internal organs.
The inflammatory process and destruction of connective tissue release newly created antigens. Antibodies and immune complexes are already formed in them. Systemic lupus erythematosus is a whole vicious circle, where each new process gives rise to another.
Experts say : a person has a genetic predisposition to this disease. Those who asked whether the disease is contagious, no? The disease is in no way contagious to others and is not transmitted through the air or saliva!
Women are most often affected by lupus. The disease also occurs among men, but less frequently. The first signs of the disease become noticeable between 20 and 45 years of life.
Aseptic thromboendocarditis (Liebman-Sachs endocarditis)
A characteristic feature of infective endocarditis is the formation of vegetations on the valves or parietal endocardium. Typically, endocarditis develops as a result of bacterial colonization of initially sterile vegetations consisting of platelets and fibrin.
Sterile vegetations (aseptic thromboendocarditis) are formed at sites of endothelial injury due to a foreign body in the heart cavity or turbulent blood flow (for example, with valve deformation), on scars and in severe non-cardiac diseases (marantic endocarditis).
Atypical verrucous Liebman-Sachs endocarditis
Endocarditis in systemic lupus erythematosus was first described by E. Libman and B. Sacks in 1924, long before it was established that this pathology belonged to systemic connective tissue diseases. Endocarditis is detected at autopsy in 20-60 %
such patients, on average 40%, and after widespread use in the treatment of systemic redness
In case of glucocorticosteroids for lupus, its frequency decreased slightly. Macroscopically, on both surfaces of the leaflets of any of the four valves, most often the mitral valve, small warty growths are detected, which can spread to the valve ring, chords, papillary muscles and parietal endocardium. Only rarely do they reach 10 mm in length, becoming overgrown with thrombotic masses and can interfere with the closure of the valves. Valve dysfunction usually does not develop. Only a small proportion of patients may experience valve insufficiency, mainly mitral, which very rarely reaches significant severity. Microscopic examination reveals endothelial proliferation with thrombotic overlays, inflammatory infiltration, foci of necrosis with hematoxylin bodies - analogues of lupus cells - and fibrosis. The immune pathogenesis of endocarditis is evidenced by the detection of immunoglobulins and complement on the endothelium of small vessels growing into warty growths. During healing, a fibrous plaque forms. Moreover, in some patients, local deformation of the valves can cause persistent mitral or aortic insufficiency.
Clinical manifestations of Libman-Sachs endocarditis are often absent. Its most common sign is a murmur (in approximately 50% of patients), in most cases systolic, usually low-intensity, short and unstable. In the presence of anemia, fever, tachycardia and signs of myocarditis, it is often impossible to confidently attribute it to endocarditis. A more specific sign of lupus endocarditis is the protodiastolic murmur of aortic regurgitation, which, however, is mild in most cases. There are isolated reports of the occurrence of stenosis of the mitral and aortic valves as a result of occlusion of the orifices by large vegetations with thrombotic overlays.
Diagnosis is based primarily on the identification of valve leaflet overlaps, thickening, and regurgitant flows on two-dimensional Doppler echocardiography. Due to the impossibility of visualizing small-sized vegetations, on the one hand, and the nonspecific thickening of the valve leaflets,
Panov as a sign of endocarditis - on the other hand, the accuracy of intravital diagnosis of Libman-Sachs endocarditis in the absence of significant valve dysfunction is low.
Complications of atypical warty endocarditis are rare. These include systemic emboli from fragments of vegetation, mainly thrombotic masses, the addition of infective endocarditis and heart failure. Infectious endocarditis was identified by N. Doherty et al (1985) in 4.9% of deceased patients with warty endocarditis at autopsy and in 1.3% of patients in the clinic. The development of heart failure is associated mainly with myocarditis concomitant with lupus endocarditis and, in some cases, with pericarditis.
In most patients, atypical warty endocarditis does not require special treatment. This also applies to pathogenetic therapy with glucocorticosteroids, the dose of which is determined, as a rule, based on the nature and severity of other manifestations of systemic lupus erythematosus. There is no data on the possibility of accelerated healing of affected valves and a decrease in their residual dysfunction under the influence of glucocorticosteroids in such patients. In rare cases of the development of hemodynamically significant valve insufficiency, valve replacement is resorted to, guided by generally accepted indications. These operations are, however, associated with a significant increase in risk.
Most experts consider it advisable to carry out primary antibiotic prophylaxis of infective endocarditis in patients with systemic lupus erythematosus with the presence, according to echocardiography, of overlaps on the valves and their thickening. These recommendations are, however, empirical in nature, since special studies of the effectiveness of such prophylaxis for Liebman-Sachs endocarditis have not been conducted,
Abacterial thrombotic endocarditis
Abacterial thrombotic endocarditis develops mainly in patients with severe chronic diseases, most often malignant tumors, especially of the stomach, pancreas and lungs. Second place
The most common type is severe congestive heart failure. Less commonly, abacterial thrombotic endocarditis occurs in patients with stroke and infectious diseases - osteomyelitis, tuberculosis, pneumonia, etc. Since a significant part of such patients are elderly, as well as with significant loss of body weight associated with the underlying disease, this form of endocarditis was previously called marantic or cachectic. Both of these terms cannot be considered successful, since neither old age nor cachexia are obligatory signs of this disease. The mitral valve is most often affected, less often the aortic valve or both valves.
The etiology and pathogenesis of abacterial thrombotic endocarditis have not been established. It is assumed that disseminated intravascular coagulation plays an important role, the activation of which is often observed in all diseases associated with abacterial thrombotic endocarditis. In a significant proportion of such patients, nonspecific degenerative changes in the valvular endocardium can also be detected. Focal exposure of collagen fibers and connective tissue ground substance causes platelet adhesion and thrombus formation. Since microscopic examination of the affected leaflets always shows no signs of inflammation, the question arises about the legality of using the term endocarditis. The resulting vegetations do not cause valve dysfunction, but can serve as sources of thromboembolism, primarily in the brain, kidneys, spleen, sometimes with serious consequences, including death. They can also become infected and cause the development of infective endocarditis.
In the clinic, abacterial thrombotic endocarditis often remains unrecognized or this diagnosis is made only tentatively. Heart murmurs are heard in no more than 1/3 of such patients and have no characteristic signs. In this regard, in most cases they are attributed to background degenerative changes in the valves that develop with age, or anemia and fever, which are often observed in patients with nonbacterial thrombotic
endocarditis due to the underlying disease. This diagnosis can be assumed by the occurrence of systemic thromboembolism, especially recurrent, in patients with malignant tumors or other serious diseases in the absence of other possible causes, such as atrial fibrillation or post-infarction left ventricular aneurysm with thrombosis. Aseptic thrombotic endocarditis can also be accompanied by an unreasonable increase in body temperature, sometimes to febrile levels, not inferior to antibacterial therapy. After a few days, body temperature usually returns to normal spontaneously. Therefore, this disease must be remembered as a possible cause of temperature reaction in patients with severe chronic diseases of internal organs.
There are no methods for verifying the diagnosis of abacterial thrombotic endocarditis. Suspicion of its occurrence in the case of causeless thromboembolism allows in some cases to identify a previously undiagnosed curable tumor.
There are no specific treatment methods.
Liebman-Sachs endocarditis is characterized by endocardial damage by systemic lupus erythematosus and antiphospholipid syndrome. This is a kind of pathology that is most often discovered in a person after his death. It has several names: lupus, warty, myrantic, thrombotic endocarditis.
Causes
Systemic lupus erythematosus (SLE) is a complex hereditary disease that is provoked by various factors. Doctors' opinions about the occurrence of the disease differ to this day, but most argue that the culprits are the measles viruses, influenza A, and B.
These viruses are classified as paramyxoviruses, which alter human antiviral immunity. Although the assumption has not yet been fully proven.
There are also other factors that cause lupus:
- environment;
- hormonal disorders.
There are no specific causes of SLE (other than a hereditary predisposition). The disease can be triggered by stress, acute respiratory viral infections or hormonal disorders due to pregnancy, puberty, menopause, abortion, etc.
Keep in mind! Systemic lupus erythematosus is not transmitted in any way; it is not an infectious or contagious disease. Lupus is not classified as oncology or as acquired immunodeficiency syndrome.
Causes and mechanism of development
Lupus erythematosus is a disease whose main causes are still unclear. More often, the disease develops due to a combination of several causes and in people at risk.
The main suspected causes of the development of lupus erythematosus:
| Provoking factor | Description of the factor |
| Hereditary | This reason has not been confirmed, but if the mother or the first child is diagnosed with lupus, then the probability of having a second child with this pathology increases to 80%. |
| Genetic | The presence of a genetic predisposition to the development of immune pathologies. |
| Infectious | The presence of Epstein-Barr infection (related to herpes diseases). The involvement of the virus in the development of pathology has not been proven, but it is always diagnosed together with lupus erythematosus. |
| Hormone | The disease occurs with an increase in the hormone estrogen in women. It has not been proven whether hormones influence the development of the disease or whether this symptom is a consequence of lupus. |
| External | Prolonged exposure to ultraviolet light (sun rays) causes cell mutation, which can lead to a malfunction of the immune system and the development of lupus. Or frequent hypothermia, frostbite. |
| Drug | Taking certain medications can cause a malfunction of the immune system and further development of lupus. |
| Toxic | Exposure to toxins and chemicals. |
Pathology most often occurs in people at risk and in the presence of 2 or 3 of the listed reasons.
Risk factors causing the development of lupus erythematosus:
- pathologies of the skin (eczema, dermatitis) and the endocrine system (diabetes, thyroid diseases);
- infectious diseases in chronic form;
- depletion or severe weakening of the immune system;
- AIDS;
- nicotine and alcohol;
- liver diseases;
- frequent hormonal imbalances and allergies;
- female gender (childbirth, menopause and puberty) and Negroid race;
- frequent stress and depression, as well as diseases of the nervous system.
These factors can cause a malfunction of the immune system. It begins to destroy healthy cells, the process is accompanied by an inflammatory reaction. Antibodies and inflammation first destroy cells; without therapy, tissues and organs begin to deteriorate. If the disease is ignored further, death occurs.
Signs of systemic lupus erythematosus
There are certain signs of the disease, but each case of SLE is varied. Clinical manifestations can be mild or severe. It all depends on the level of organ damage.
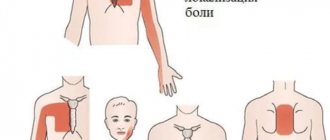
Some symptoms of the disease:
- joints swell;
- muscle pain;
- apathy, fatigue;
- fever;
- pink, red rashes on the skin of the face (see photo, the rash can also be on the shoulders, hands, chest);
- pain in the chest area when taking deep breaths;
- hair loss (rare);
- swelling of the legs and swelling around the eyes;
- inflammation of the lymph nodes in the neck, groin and armpits.
Classification of the disease
In the generalized form of the disease, three types of course are distinguished. Next, let's look at each in more detail.
The acute version is characterized by a sudden start. Often patients can pinpoint the exact time when lupus erythematosus began to develop. They usually find out what kind of disease it is after visiting a doctor. Among the main symptoms are the appearance of rashes on the skin, the development of polyarthritis, and an increase in temperature. Multiple organ damage entails a sharp deterioration of the condition, which in some cases lasts up to two years. Timely treatment with medications allows you to achieve stable remission.
Subacute wave-like course is characterized by gradual development of the pathological process. Initially, it involves the joints and skin. The remaining organs join each time there is a relapse. Systemic lupus develops very slowly and therefore has a multisyndromic clinical picture.
The chronic version of the disease manifests itself with one or more symptoms. Against the background of excellent health, patients develop skin rashes and arthritis. The pathological process develops very slowly, gradually capturing more and more organ systems.
Diagnosis of the disease
An accurate diagnosis of SLE can only be made by a specialist after conducting a series of laboratory tests. If, during a laboratory test, a significant number of LE cells are found in the patient’s blood, then he is definitely a person with lupus.
These cells are characteristic in most cases. In addition, diagnosing the disease is difficult. Experts often spend years confirming a diagnosis. The previously mentioned signs of the disease appear at different periods of the course of SLE, and it takes time to collect all the signs and make a diagnosis.
The diagnosis itself is individual for each patient. The doctor cannot confirm the final diagnosis based on any specific sign. To begin with, it is necessary for the patient to tell the attending physician a complete and detailed medication history. This is important in the diagnostic process.
Then the specialist will differentiate the information received, along with examination and laboratory tests, from other diseases that are similar to lupus.
Differential diagnosis
Diagnostic signs of lupus:
- the cheekbone is covered with red rashes in the form of a “butterfly”;
- discoid rash;
- severe sensitivity to sunlight for short periods of time;
- mouth ulcers;
- inflammation, swelling of joints;
- sharp, groundless psychoses and convulsions;
- decrease in blood cells;
- inflammation of the kidneys, serous membrane of the lungs;
- immune system disorders.
Based on these signs, a rheumatologist will be able to distinguish SLE from other diseases with similar symptoms. To make a diagnosis, the patient must have at least 5 of these signs.
The doctor should pay attention to the patient’s condition, namely, notice his weakness, loss of appetite, pain in the abdomen, and diarrhea. Therefore, the patient should tell the doctor about all pain and changes in the body.
When is hospitalization needed?
If you suspect that a person is developing signs of lupus erythematosus, immediately contact a medical facility to confirm or exclude the diagnosis. The examination is carried out in a hospital setting.
Hospitalization several times a year is necessary if there is an acute form of the disease
The acute course of the disease requires hospitalization 1–2 times a year. In chronic and subacute forms of lupus, much attention is paid to prevention - compliance with the medication schedule, a special diet, and limiting the time spent under bright sunlight.
For timely detection of new pathological changes in the body, patients undergo inpatient treatment once a year.
Treatment
There is no cure for lupus, but treatment can relieve symptoms.
Lupus is a chronic inflammatory disease that can cause different symptoms in different areas of the body.
Lupus symptoms can be controlled with various treatment options. The treatment plan will depend on the severity of the condition and whether the person has had recent flare-ups. They can range from mild to severe. The goal of treatment is to prevent and limit organ damage and other potential complications.
Medicines against lupus
Drugs commonly used to treat the disease:
- Nonsteroidal anti-inflammatory drugs: These medications will help relieve pain, swelling, and fever.
- antimalarial drugs. Medicines commonly used to treat malaria will help control lupus symptoms, such as fatigue, rashes, and mouth sores.
- corticosteroids. These medications can help control inflammation, but they can cause long-term side effects such as weight gain, thinning bones, diabetes, easy bruising, and infection.
- immunosuppressants. These drugs suppress the immune system, which is the source of inflammation associated with lupus. Immunosuppressants have serious side effects, including an increased risk of cancer, liver damage, and bone marrow suppression.
- biological drugs. These new drugs are already approved for the treatment of other rheumatic diseases such as rheumatoid arthritis.
Can lupus really be curable?
The description given in the previous section is frightening and forces you to look for alternative solutions. As revealed in the article above, it is unknown what causes this disease. It is a lifelong, incurable disease that is not contagious. Also, this is an autoimmune disease and heredity plays a role. One of these statements is not true according to A. William's book Meditsiinimeedium.
The author of the book writes that it is not known in the medical field that lupus is a reaction of the body to a virus or to EBV neurotoxins. This means that the body has an allergic reaction to these toxins, which increases levels of inflammatory markers. Doctors look for it to identify and diagnose lupus. Lupus is actually an Epstein-Barr virus infection.
The medical community recognizes only one form of EBV, but in reality there are more than 60 variants. You can read more about VEB in our article here.
- A.William raamat “Meditsiinimeedium”
- https://www.ncbi.nlm.nih.gov/pubmed/17121489
- Ajakiri “Mida arstid sulle ei räägi” August 2020 Nr 8 (44)
- Eesti Reumaliit
Was this post helpful?
Let us know if you liked the post. That's the only way we can improve.
Complications
In rare cases, patients are faced with the fact that the disease affects only one specific part of the body or organ, for example, the skin, joints or vascular system. However, in most cases, patients diagnosed with SLE suffer from multiple organ failure syndrome, that is, complications of the disease appear in many parts of the body and affect several organs at once.
The disease affects the following organs:
- Kidneys. They suffer from acute inflammation, which makes their work difficult. The efficiency of removing toxic substances from the body decreases. Lupus reduces kidney function. It is treated with medication to reduce the risk of serious organ damage. The extent of damage can be determined using a urine test.
- Central nervous system. Most patients experience damage to the central nervous system. The disease causes migraines, dizziness, problems with memory, vision, paralysis, psychosis and convulsions.
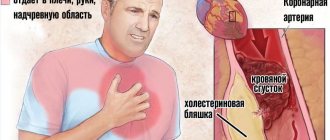
- The cardiovascular system. They often become inflamed. Vasculitis occurs, slowing down the passage of blood, and as a result, thrombosis. Inflammation of the arteries, myocarditis, and endocarditis occur .
- Pulmonary system. Patients often suffer from inflammation of the serous membrane of the lungs. Lupus causes atypical inflammatory processes in the lungs, shortness of breath and cough.
SLE disability and complications
Suppressed immunity during illness makes the body defenseless against bacterial and viral infections. Therefore, to reduce the risk of complications, it is necessary to minimize contact with other people. Upon diagnosis, study or work is interrupted for a year, issuing a 2nd disability group.
The inflammatory process that accompanies systemic lupus affects various organs, causing severe complications, such as:
- renal failure;
- hallucinations;
- headache;
- behavior change;
- dizziness;
- stroke;
- problems with expression, memory and speech;
- seizures;
- tendency to bleeding (with thrombocytopenia);
- disorders in the blood composition (anemia);
- vasculitis or inflammation of the blood vessels of various organs (the disease worsens in a smoker);
- pleurisy;
- disorders of the cardiac system;
- pathogens in the genitourinary system and respiratory infections;
- non-infectious or aseptic necrosis (destruction and fragility of bone tissue);
- oncology.
Consequences of lupus during pregnancy
Lupus in pregnant women increases the risk of premature birth and preeclampsia (complications of normal pregnancy that occur in the 2nd-3rd trimester). With the disease, the likelihood of miscarriage increases.
If a woman plans to become pregnant, the doctor recommends refraining from conceiving. The period is determined as follows: six months must have passed since the last exacerbation of the disease.
How to live with lupus?
If you have been diagnosed with this disease, it does not mean that you can give up on yourself. Many people live with a diagnosis of lupus. Photos of such patients clearly prove that it is simply necessary to fight the disease. You will probably have to make some changes to your usual lifestyle. Doctors recommend resting as needed. It is better to lie down several times a day than to work too hard.
Study the main symptoms indicating the transition of the disease to the acute stage. It is usually preceded by severe stress, prolonged exposure to the sun, and a cold. If you avoid these triggers, life can become much easier.
Don't forget about regular physical activity, but you shouldn't overwork your body either. You can choose Pilates or yoga as your main sport. On the other hand, it is necessary to give up all bad habits. Smoking and drinking alcoholic beverages do not improve your health. Such people get sick more often and overload their heart and kidneys. You shouldn't risk your own life for a moment's pleasure.
Accept your diagnosis and consult your doctor if necessary. The specialist should tell you how lupus develops and what kind of disease it is. Photos of patients living with this disease can motivate you to continue to actively fight it.
Particular attention must be paid to the diet. It is recommended to abandon all harmful products, because they negatively affect the functioning of the main systems of internal organs. Caffeine and products containing it are also prohibited. This substance makes the heart beat faster, does not allow it to rest, thereby overloading the central nervous system. The diet should consist of lean meat, fish in large quantities, as well as vegetables and fresh fruits. Don't forget about dairy products. They contain healthy amounts of calcium and vitamin D, which helps prevent osteoporosis.