Disturbances in the circulatory system do not manifest themselves for a long time. They can occur in any organ, but the most dangerous is damage to the arteries of the heart and brain, as it often ends in a heart attack or stroke. Therefore, it is important to understand what cardiac vascular stenosis is and how it manifests itself in order to begin treatment on time and prevent serious consequences.
CVS pathologies can lead to serious consequences
General information
Stenosis is a narrowing of the lumen of arteries or veins. Cardiac vascular stenosis refers to the obstruction of the patency of the coronary (coronary) arteries, which provide blood supply to the heart muscle.
Thanks to them, the heart receives oxygen and essential nutrients. Accordingly, when these arteries narrow, the entire body suffers, since under conditions of insufficient nutrition, the heart ceases to fully cope with its functions.
This pathology leads to disruption of the myocardium.
Neck vasoconstriction: symptoms, diagnosis
In this case, the vessels supplying blood to the brain narrow. Often the carotid arteries are affected, while the veins of the neck are practically unaffected.
Often, cervical vascular stenosis remains invisible to a person until a stroke occurs. Symptoms of the disease will be:
- dizziness,
- noise in ears,
- weakness in the limbs,
- veil, “sights” and darkness in the eyes.
Possible reasons
Narrowing of the heart vessels can develop for various reasons.
These include:
- atherosclerosis;
- obesity;
- metabolic diseases;
- endocrine diseases;
- elderly age;
- smoking;
- sedentary lifestyle;
- congenital malformations;
- vasculitis and other diseases of the blood and blood vessels.
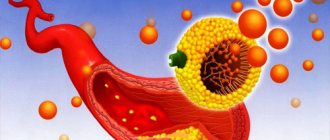
Depending on the mechanism of development, narrowing of the coronary arteries may occur due to vasospasm, blockage by a blood clot or cholesterol plaque.
The coronary arteries must ensure uninterrupted flow of blood into the myocardium
Classification
Depending on which vessels are affected, stenosis is distinguished:
- right coronary artery;
- left coronary artery;
- tandem (simultaneously right and left).
In addition, critical stenosis is identified - when the lumen of the vessel narrows by more than 70%. This condition is especially dangerous, since at any time it can provoke myocardial infarction and severe heart failure (HF).
Restenosis is the development of repeated stenosis after a vessel bypass operation. This complication is quite rare, provided the patient follows all the doctor’s recommendations in the postoperative period.
Arteries supplying the heart
Arterial stenosis: description of the disease, treatment and prevention
Additional education:
"Cardiology"
State educational institution "Institute for Advanced Medical Studies" of the Ministry of Health and Social Development of Chuvashia
Contacts
Normal blood circulation ensures optimal functioning of all internal organs of the body. It is through the blood that they receive oxygen in the required volume and nutrients. In other words, damage to blood vessels inevitably leads to damage to all organs.
A rather serious vascular disease is coronary artery stenosis. Bifurcation stenoses of the coronary arteries are quite common in medical practice. Arterial stenosis is a significant narrowing of the lumen of the arteries. This leads to the development of their complete or partial obstruction.
Classification of arterial stenosis
SLCA affects many arteries. The lesions differ from each other in symptoms and possible consequences. It is worth considering them in more detail.
Stenosis of the right main coronary artery
The vessels that are located in the heart are called coronary. Another name for them is coronoids. They are responsible for normal blood supply and myocardial function.
The RCA, in turn, is responsible for providing oxygen to the sinus node. Damage to the right coronary artery can lead to disturbances in the rhythm and speed of ventricular contractions.
The consequences of delaying medical care can be very serious. Due to stenosis of the RCA trunk, the following ailments can rapidly develop:
- Ischemia.
- Angina pectoris.
- Myocardial infarction.
- Arrhythmia.
- Rapid increase or decrease in blood pressure, etc.
But in medical practice this disease is quite rare.
Stenosis of the left main coronary artery
Unlike the previous disease, stenosis of the left main coronary artery is much more common. But it is also a more dangerous disease.
The greatest health risk is that the left ventricle is responsible for almost the entire circulatory system. If there are disturbances in its functioning, the remaining internal organs suffer.
Symptoms of left coronary artery stenosis
With STLC, a person feels a loss of strength. First, his general condition worsens, inability to work and drowsiness are observed.
As the disease progresses, the following symptoms may appear:
- Shortness of breath.
- Frequent headaches and migraines.
- Discomfort in the chest area.
- Angina attacks during physical exertion and emotional stress.
- Nausea, etc.
Consequences of STLC
Significant narrowing of the left coronary artery is largely caused by the formation of plaques in its thickness. Their formation is caused by a high percentage of low-density lipoproteins in the patient’s body.
Similar vascular conditions, as with stenosis of the right coronary artery, can lead to the following consequences:
- Development of ischemic diseases and their consequences.
- Pre-infarction conditions.
- Myocardial infarction, etc.
Tandem coronary artery stenosis
This type of stenosis is quite rare. It is characterized by damage to both the left and right coronary arteries. The diagnosis is very negative.
If only one ventricle in the heart is damaged, the second one can take on the main job of pumping blood. In this case, the disease develops much more rapidly.
In the absence of timely medical intervention, there is only one consequence for tandem stenosis - death. To get rid of this disease, surgical intervention is necessary to replace or restore damaged coronary arteries.
Vertebral artery stenosis
The vertebral arteries are no less important than the coronary arteries. Violations of PA can lead to serious changes in the human body.
VA stenosis can be caused by intervertebral hernias, inflammatory processes, tumors, congenital vertebral disorders, etc. Narrowing of the VA lumen leads to a complete or partial cessation of blood flow to the brain and, accordingly, oxygen.
Symptoms of vertebral artery stenosis
The main symptoms of VA stenosis are:
- Severe headaches that often turn into migraines.
- Nausea and vomiting.
- Severe dizziness.
Pain sensations may radiate to other parts of the body. The nature of the pain can be completely different. It increases with sharp turns of the head, shaking or fast driving, etc.
Consequences of vertebral artery stenosis
The most common consequence of advanced VA stenosis is stroke. The flow of blood to the brain is significantly blocked. There is a pronounced lack of oxygen.
Lack of timely medical care for a stroke or advanced vertebral artery stenosis can be fatal.
Femoral artery stenosis
The next type of stenosis is femoral artery stenosis. In this case, stenosis and occlusion of the lower extremities are interrelated and interchangeable concepts. Blood flow to the legs is significantly reduced, and swelling is observed. Swelling can lead to a point of no return, when the condition of the arteries and their tissues deteriorates so much that it is no longer possible to correct the situation.
Symptoms of femoral artery stenosis
The main symptoms of this disease include:
- Lameness.
- Severe pain in the lower extremities.
- Spasms.
- Complete cessation of hair growth in certain areas of the legs.
- Changes in color and shade of the skin of the lower extremities. Blueness or, conversely, redness may be observed.
- Changes in the temperature of the lower extremities, which indicates the development of inflammatory processes.
Consequences of femoral artery stenosis
Like all previous types of stenosis, this one requires immediate intervention. Otherwise, the patient will face negative consequences for his health.
In the absence of medical intervention, inflammatory processes will rapidly develop and increase. This will lead to the formation of gangrene.
In case of advanced inflammatory processes, swelling and tumors, immediate amputation of the limb is required. This is necessary to prevent the risk of increasing the affected area.
Iliac artery stenosis
The iliac artery is the second largest artery in the human body. Disturbances in the functioning of the iliac artery can lead to very serious consequences.
Symptoms of iliac artery stenosis
Among the main signs of ailments and lesions of the iliac artery are:
- Increased fatigue and inability to work.
- Drowsiness.
- Lameness.
- Loss of sensation in the limbs.
- Blueness or redness of the skin.
- Swelling of the lower extremities.
- Impotence syndrome, etc.
Consequences of the disease
With iliac artery stenosis, tissue metabolism slows down significantly. The removal of unnecessary substances from the body worsens.
They begin to accumulate in large quantities in the plasma. This inevitably leads to an increase in its thickness and viscosity. Such changes in the composition of the blood always result in the formation of blood clots in the walls of blood vessels. This interferes with normal blood circulation and oxygen supply to the internal organs of the human body.
Critical stenosis
The acute form of stenosis is critical. It begins to develop if the thickness of the vessels increases by more than 70 percent.
This form requires immediate surgical intervention. This is the only method of treating this form of the disease.
Critical stenosis increases the risk of complete cardiac arrest or myocardial infarction in the patient. This can happen at any time, which is why if the condition worsens, you should immediately contact a specialist.
Source: //CardioPlanet.ru/zabolevaniya/sosudy/stenoz-arterij
Clinical manifestations
With coronary stenosis, no symptoms are observed for a long time. The first sign is a deterioration in health during physical activity.
Shortness of breath appears, the heart rate increases, chest discomfort may be felt, and as the stenosis progresses, pain occurs. Often patients note swelling of the lower extremities without any reason for this.
Chest pain and shortness of breath are the first signs of the disease
If the disease is not identified at this stage and treatment is not started, the symptoms will intensify and occur even with the slightest load due to insufficient nutrition of the heart muscle.
Clinically, this will be manifested by the symptoms of AHF:
- feeling of lack of air;
- pain behind the sternum;
- tachycardia;
- cold sweat;
- paleness of the skin;
- heart rhythm disturbances;
- cyanosis of the lips and nose;
- weakness, etc.
Without adequate treatment, coronary artery stenosis leads to myocardial infarction. In such situations, the patient’s condition sharply worsens, the pain behind the sternum intensifies and spreads to the left arm, it becomes difficult to breathe, blood pressure drops, and the patient may lose consciousness.
Emergency hospitalization to the intensive care unit or cardiology department is required. The price of delay in this matter is death in almost 100% of cases.
Carefully! The pathology is dangerous because it may not manifest itself in any way before the development of myocardial infarction.
Cardiac stenosis
Diseases
According to medical statistics, cardiac vascular stenosis is diagnosed in almost 30-40% of cases when visiting a cardiologist. This dangerous pathological condition causes deterioration of blood circulation due to narrowing of the lumen of the artery.
The most common diagnosis is aortic stenosis. This disease can lead to serious complications, such as stroke, and can also lead to death.
Therefore, it is very important not to delay treatment of the disease, but when it is identified, immediately begin to fight it.
Symptoms
The danger of this disease is that it does not immediately manifest itself. Stenosis develops quite slowly and over a long period of time, but the symptoms in the early stages of the disease are quite vague. Signs of stenosis can only occur during physical activity. In this case, the patient feels:
- shortness of breath;
- cardiopalmus;
- weakness;
- chest pain.
During intense physical activity, people with stenosis may experience dizziness and fainting. In addition, in the early stages of the development of the disease, a person may also be bothered by swelling of the lower extremities and face, headaches and hoarseness of voice.
Over time, coronary artery stenosis causes symptoms to worsen. Chest pain becomes more intense, causing serious discomfort. They can radiate to the arm, scapula and interscapular area.
Such symptoms can be regarded as signs of many other diseases of the cardiovascular system. At the same time, people begin to treat themselves on their own, only worsening their condition.
As a result, such incorrect actions can quickly provoke the emergence of complications that are difficult to treat.
Cardiac vascular stenosis can be either congenital or acquired. In the first case, we are talking about a defect that occurs even at the stage of intrauterine development. This disease has a hereditary predisposition.
Therefore, if one of the relatives had vascular stenosis, then other family members need to closely monitor their health. The most common cause of the acquired form of the disease is considered to be atherosclerosis.
This disease occurs due to:
- poor nutrition;
- sedentary lifestyle;
- increased blood clotting;
- diabetes mellitus;
- hormonal disorders.
Atherosclerosis causes the accumulation of cholesterol plaques on the walls of the arteries, which narrow their lumen, causing stenosis of the heart vessels.
As a result, blood flow is disrupted and may stop completely if they are blocked by a blood clot or a detached plaque.
People who are overweight, eat a lot of fatty foods, and abuse tobacco smoking are at risk of encountering atherosclerosis and stenosis of heart vessels.
Stenosis can also appear in a person after suffering a severe streptococcal infection, namely tonsillitis. In this case, the disease develops as a complication of this disease. Sore throat can provoke the growth of fibrous tissue on the aortic valves, which causes the development of stenosis.
When the first symptoms indicating the development of stenosis appear, you should immediately seek medical help. The following specialists can cope with such a complex disease:
At the first appointment, the doctor will carefully examine the patient’s complaints. An examination will help determine the cause of a person’s poor health. The doctor will feel your pulse, measure your blood pressure and listen to your heart sounds. After this, the doctor will ask the patient to answer a few simple questions:
The survey helps the specialist understand what could trigger the development of stenosis. But only a full examination can confirm the doctor’s suspicions.
The patient is referred for an electrocardiogram, ultrasound examination of the heart, computed tomography or magnetic resonance imaging.
To confirm atherosclerosis, the patient will also have to donate blood to determine cholesterol levels.
Based on the examination results, the doctor develops a therapy program for the patient. Depending on the severity of the patient's condition, medical or surgical treatment is carried out. If the disease is at an early stage of development, then conservative therapy is prescribed. The patient will need to take:
- vasodilators;
- cholesterol-lowering agents;
- blood thinning medications.
In order for the therapy to be effective, the doctor asks the patient to adhere to proper nutrition. He will need to give up all foods. Which are rich in fats. It is also very important to try to overcome bad habits.
If the disease is diagnosed at a late stage of development, the patient is prescribed surgery. Surgical intervention is resorted to in extreme cases, when no conservative treatment methods can improve the patient's condition.
Heart attacks are younger, but they can be prevented
In recent years, heart attacks have become significantly younger. If earlier they threatened the main...
Sports for the heart: shown to everyone
At one time, Churchill explained the secret of his longevity something like this: when it is possible...
Smokers are hired less often
Smoking is harmful not only to your health, but also to your pocket. Numerous studies have shown...
Pressure in the chest
According to statistics from the World Health Organization, heart disease...
Source: https://bolezni.zdorov.online/terapevticheskie-uslugi/stenoz/stenoz-sosudov-serdtsa/
How to make a correct diagnosis
At the first signs of heart failure described above, you should contact a cardiologist for consultation and examination.
After collecting complaints and anamnesis to examine the condition of the heart vessels, the doctor will refer you to:
- ECG;
- Ultrasound of the heart and blood vessels;
- angiography of the coronary arteries;
- computed tomography.
In addition, he will perform percussion and auscultation to confirm the suspected diagnosis.
Instrumental research methods help confirm the diagnosis
Treatment
Depending on the degree of narrowing of the lumen and the cause that caused it, treatment of stenosis of the heart vessels is carried out using conservative therapy or surgical intervention.
Drug treatment can have good effects only in the early stages of the development of heart failure. If symptoms are severe, surgery is required.
Table. Degrees of heart failure.
| Degree | Symptoms |
| Lightweight | The patient does not experience any symptoms with normal physical activity. Increased loads cause slight shortness of breath, weakness, palpitations, chest discomfort |
| Average | Prolonged physical activity causes shortness of breath, tachycardia, chest pain |
| Heavy | At rest, the patient does not show any complaints. But with normal physical activity, symptoms of heart failure occur |
| Very heavy | Symptoms of heart failure appear even at rest and gradually increase |
Drug treatment
In order to improve blood supply to the heart, reduce symptoms of heart failure and prevent the development of myocardial infarction during drug treatment of aa stenosis. coronaria is used:
- vasodilators;
- anticoagulants;
- diuretics.
If the cause of the disease is atherosclerosis, additional medications are prescribed to help dissolve cholesterol plaques and prevent the formation of new ones.
The degree of narrowing of the arteries determines treatment options
Vasodilator therapy
Vasodilators promote vasodilation, therefore they are used for coronary artery stenosis.
From this group the following are most often prescribed:
- Nitroglycerine;
- Molsidomine;
- Isosorbide mononitrate.
These drugs cannot be used in all clinical situations, so only a doctor should prescribe them.
Improving the rheological properties of blood
To prevent the formation of blood clots in the coronary vessels, anticoagulants and antiplatelet agents are used. These drugs help thin the blood and prevent its increased coagulability and viscosity.
Among the anticoagulants for stenosis, heparin and its derivatives (Warfarin, Enoxaparin, Nadroparin and others) are prescribed.
Among antiplatelet agents, the following have gained popularity:
- Aspirin;
- Cardiomagnyl;
- Dipyridamole;
- Ticlopidine;
- Clopidogrel et al.
Blood thinning drugs should be used with caution during surgery due to the increased risk of bleeding as a result of their action.
Diuretics
Diuretics (water medications) reduce high blood pressure and reduce the workload on the heart. For this purpose, use:
- Furosemide;
- Torasemide;
- Ethacrynic acid;
- Indapamide;
- Spironolactone, etc.
Depending on the severity of heart failure, they are prescribed in the form of tablets or injections. Uncontrolled use of diuretics may lead to disturbances in water-electrolyte balance, hormonal or metabolic disturbances, so they should be taken only as prescribed by a doctor and following his dosage recommendations.
Stenosis of the main trunk of the left coronary artery
Performing CABG is traditionally considered as a standard procedure in providing care to patients with severe stenosis of the main trunk of the left artery, for whom surgical intervention is not contraindicated. The CASS registry reported that 912 patients who underwent CABG had an average survival of 7 years longer than those who used medical therapy [54]. Despite the fact that the ESC recommendations for PCI indicate that “the possibility of stenting a stenosis of the main trunk of the left coronary artery should be considered only in situations where there is no access to other interventions for myocardial revascularization” [55], recent data that have appeared will discussed below, indicate that at the 2nd year of follow-up in patients with mild stenosis of the main trunk of the left coronary artery, PCI is accompanied by at least comparable, if not better, results compared to CABG. Such new data could somewhat ease the list of restrictions on performing PCI. However, studies are needed in which the validity of the findings can be verified over a longer (at least 5 years) observation period.
Despite the fact that stenosis of the main trunk of the left coronary artery is a fairly attractive option for PCI due to the large diameter of this artery and the proximal location of the stenosis in the coronary bloodstream, there are two pathophysiological features that can neutralize the effectiveness of PCI:
– up to 80% of stenoses located in the main trunk of the LMCA can spread to the bifurcation area, in which, as is known, the risk of restenosis is much higher;
– 80% of patients with stenosis of the main trunk of the LMCA have multivessel disease, in which, as noted earlier, CABG can improve patient survival.
To date, the most complete and accurate answer to the question regarding the advisability of using CABG or PCI in people with stenosis of the main trunk of the left coronary artery is provided by the SYNTAX study, which analyzed indicators in subgroups specifically created to test one or another hypothesis. In a total population of 705 patients diagnosed with main LMCA stenosis who were randomized, the event rates at the end of 1 year of follow-up were:
– death: in the CABG group – 4.4%, in the PCI group – 4.2% (P=0.88);
– serious cerebrovascular events: in the CABG group – 2.7%, in the PCI group – 0.3% (P=0.009);
– MI: in the CABG group – 4.1%, in the PCI group – 4.3% (P=0.97);
– the need for repeated intervention for myocardial revascularization: in the CABG group – 6.7%, in the PCI group – 12.0% (P=0.02);
– major cardiac and cerebrovascular events: in the CABG group – 13.6%, in the PCI group – 15.8% (P=0.44).
Thus, the advantage of performing CABG was only in its ability to reduce the need for repeated interventions for myocardial revascularization. However, it was associated with a higher risk of adverse cerebrovascular events.
When studying indicators in subgroups of patients, identified depending on the score (in points) on the SYNTAX scale, the following results were obtained. The incidence of major adverse cardiac and cerebrovascular events was: in persons with a low score (0–22 points) – 13.0% in the CABG group and 7.7% in the PCI group (P=0.19); in persons with an average score (23–32 points) – 15.5% in the CABG group and 12.6% in the PCI group (P=0.54); in those with a high score (≥ 33 points) – 12.9% in the CABG group and 25.3% in the PCI group (P=0.08).
Unpublished study results obtained at the end of 2 years of follow-up show that in the subgroup of people with a low SYNTAX score, mortality in the CABG group was 7.9% and in the PCI group it was 2.7% (P=0.02). ); the incidence of repeat intervention for myocardial revascularization in the CABG group was 11.4%, and in the PCI group – 14.3% (P=0.44).
These data suggest that in longer follow-up periods, the effectiveness of PCI may be slightly higher than that of CABG. By the way, out of 1212 patients with stenosis of the main trunk of the left coronary artery included in a parallel registry or in the observation groups of randomized controlled trials, 65% of individuals had a SYNTAX score of ≥ 33 points.
Evidence that PCI is effective in the treatment of low-risk main trunk lesions has been obtained from a number of other sources. The meta-analysis, covering the results of 10 studies, including two randomized controlled trials and the MAIN-COMPARE registry, analyzed data on 3773 patients diagnosed with lesions of the main trunk of the LCA. N. Naik et al. [56] reported that in the CABG and PCI groups there were no differences in mortality, as well as in the incidence of achieving the primary combined endpoint of the study (the latter included the incidence of deaths, MI and adverse cerebrovascular events at the end of the 3-year period observations). However, in the PCI group, the need for repeat revascularization was 4 times higher. These results were confirmed by data obtained from the MAIN-COMPARE registry over a 5-year follow-up period [57].
6.7. Recommendations
There are two points to consider:
— to what extent revascularization is indicated in a particular clinical situation (Table 8);
- which of the interventions - CABG or PCI - would be preferable to undertake with the corresponding variant of the course of coronary artery disease (Table 9).
The current database, based on the principles of evidence-based medicine, indicates that the need for myocardial revascularization can be quite easily justified:
· clinically – in patients with persistent symptoms (angina or its equivalents) that continue to be recorded despite OMT, and/or
· based on an assessment of the prognosis - when the patient is identified with corresponding prognostically unfavorable variants of the course of the disease or the presence of sufficiently extensive foci of ischemia is confirmed by objective methods (even against the background of the absence of symptoms of the disease). For example, severe stenoses of the main trunk of the LMCA or the proximal part of the anterior descending branch of the LMCA (especially occurring against the background of the presence of multivessel lesions) are direct indications for revascularization. In very severe cases of coronary artery disease, it turned out that performing CABG improves survival rates, and also significantly reduces the need for repeated intervention for myocardial revascularization, although it increases the risk of adverse cerebrovascular events (especially when this intervention is performed for stenosis of the main trunk of the LCA).
Considering that attempts to visually assess the severity of stenosis on angiograms are accompanied by its underestimation or overestimation, the increasingly widespread introduction of the indicator of relative (partial) coronary reserve to identify functionally significant stenoses is undoubtedly great progress in resolving this issue (see section 5.4).
In general, it is not possible to formulate any single recommendations regarding the preferred use of a particular method of myocardial revascularization for every possible clinical situation. However, it has been estimated that there are over 4000 possible clinical and anatomical variants of the disease. However, based on a comparison of clinical outcomes accompanying PCI and CABG and presented in Table. 8 and 9, the cardiac team can formulate their basic recommendations, which they will use in the process of informing the patient and obtaining informed consent for a particular intervention. However, all these recommendations should be interpreted taking into account the individual preferences of the patient, as well as the specific clinical situation. For example, if, as a result of a prognostic assessment, a patient has indications for CABG, they can be revised taking into account the individual clinical characteristics of the disease (for example, advanced age and severe concomitant pathology).
Table 8. Indications for revascularization in patients with stable angina and silent ischemia
| Variant of the course of IHD | Class of clinical recommendations | Level of evidence | Source | |
| Based on forecast | Stenosis of the main trunk of the left artery > 50%1 | I | A | 30, 31, 54 |
| Any proximal stenosis of the anterior descending branch of the LCA1 | I | A | 30–37 | |
| Simultaneous damage to two or three arteries + LV dysfunction1 | I | B | 30–37 | |
| Extensive area of ischemia confirmed by additional imaging methods (> 10% of the LV wall) | I | B | 13, 14, 38 | |
| Stenosis of the only remaining patent vessel > 50%1 | I | C | – | |
| Single vessel lesion without involvement of the proximal anterior descending branch of the LMCA and without extensive areas of ischemia (> 10% of the LV wall) | III | A | 39, 40, 53 | |
| Based on existing symptoms of the disease | Stenosis of any localization > 50%, occurring with limited anginal syndrome (or its equivalents), which does not respond to OMT. | I | A | 30, 31, 39–43 |
| Dyspnea/CHF + extensive area of ischemia (> 10% of the LV wall)/proven by additional research methods the viability of myocardial areas that are supplied with blood by an artery in the lumen of which there is stenosis (> 50%) | IIa | B | — | |
| The effectiveness of OMT in eliminating anginal syndrome | III | C | — |
1 With ischemia confirmed by additional research methods or partial coronary reserve <0.80 (for confirmed angiographic stenoses > 50–90% of the vessel lumen). CHF – chronic heart failure.
Table 9. The choice between performing CABG or PCI in patients with stable disease and low predicted operative mortality, in whom the nature of the existing injuries allows performing any of the compared surgical interventions
| Anatomical variant of the course of ischemic heart disease | Preferably CABG | PCI preferred | Source |
| Damage to one or two vessels (without involving the proximal anterior descending branch of the LCA) | IIb C | IC | – |
| Damage to one or two vessels (involving the proximal part of the anterior descending branch of the LCA) | I.A. | IIa B | 30, 31, 50, 51 |
| Simple damage to three vessels at the same time; complete functional revascularization after PCI SYNTAX score ≤ 22 points | I.A. | IIa B | 4, 30–37, 53 |
| Complex damage to three vessels simultaneously; incomplete functional revascularization after PCI SYNTAX score > 22 points | I.A. | III A | 4, 30–37, 53 |
| Lesion of the main trunk of the left artery (isolated or in combination with damage to another artery) - with a lesion in the lumen or from the outside | I.A. | IIa B | 4, 54 |
| Lesion of the main trunk of the left artery (isolated or in combination with damage to another artery) - with a lesion in the distal bifurcation | I.A. | IIb B | 4, 54 |
| Damage to the main trunk of the left artery + simultaneous lesions of two or three vessels Score on the SYNTAX scale ≤ 32 points | I.A. | IIb B | 4, 54 |
| Damage to the main trunk of the left artery + simultaneous lesions of two or three vessels SYNTAX score ≥ 33 points | I.A. | III B | 4, 54 |
7. Carrying out myocardial revascularization in acute coronary syndrome without ST segment elevation
Non-ST segment elevation ACS is the most common form of acute coronary syndrome. Patients with non-ST segment ACS make up the majority of those undergoing PCI. Despite all the advances in drug therapy and interventional interventions, mortality and morbidity rates are still quite high, almost comparable to those recorded in patients with STEMI after the first month of the disease. However, individuals who experience ST-segment elevation ACS represent a heterogeneous group of patients with a highly variable prognosis. Therefore, early risk stratification is extremely important in the choice of both drug therapy and intervention. The main goals of coronary angiography and subsequent intervention for myocardial revascularization should be recognized as the following: complete elimination of symptoms of the disease, as well as improvement of short- and long-term prognosis. In addition, in the process of choosing treatment tactics, it is also necessary to take into account other factors that are inextricably linked with the use of invasive interventions and pharmacotherapy, namely: quality of life, length of hospital stay and the potential risks of the technical implementation of a particular intervention.
7.1. The choice of an invasive or conservative approach in the early period of the disease
Randomized controlled trials have shown that early use of an invasive approach reduces the incidence of adverse clinical outcomes associated with recurrent severe ischemia, namely, reduces the need for re-hospitalization and myocardial revascularization interventions. These studies also showed that early use of an invasive approach leads to a marked reduction in mortality and the incidence of MI in the intermediate term. However, the reduction in mortality during the long-term follow-up period was moderate, and the incidence of MI during the initial hospitalization even increased (an early complication) [58]. A recent meta-analysis confirmed that the use of an invasive approach early in the disease was associated with a reduction in the incidence of cardiovascular deaths and incident myocardial infarction throughout the 5-year follow-up period [59].
7.2. Risk stratification
Taking into account the large number and heterogeneity of patients with ST-segment elevation ACS, early risk assessment (stratification) is extremely important, as it allows us to identify those patients who have a high risk of death and adverse cardiovascular events in the intermediate and long term, and in whom early use of an invasive approach in combination with drug therapy is able to reduce their risk. In addition, it is equally important to identify low-risk groups of people in whom the use of potentially dangerous and costly invasive interventions and drug therapy may be ineffective or even harmful.
Risk assessment should be made taking into account various clinical characteristics, ECG changes, and biochemical markers. Various scoring scales have been developed for risk stratification. The “Recommendations for the management of patients with ST-segment elevation ACS” developed by the ESC suggest using the GRACE scale (https://www.outcomes-umassmed.org/grace). This scale is recommended for use in everyday clinical practice and should be used at the time of admission and discharge of the patient from the hospital [61]. Initially, the GRACE scale was intended to predict the risk of death in a hospital, and then began to be widely used in a fairly large population of patients with ACS to predict the nature of clinical outcomes in the long-term follow-up period, as well as to assess the feasibility of invasive intervention [61].
Significant benefit from an early invasive approach has only been demonstrated for high-risk patients. Recently published meta-analysis [59] and the results of the FRISC II [62], ICTUS [63] and RITA III [64] studies demonstrated a direct relationship between the patient’s risk, calculated taking into account various factors (age, presence of diabetes mellitus, hypotension, segment depression ST; as well as body mass index), and the effectiveness of early use of an invasive approach.
The initial increase in troponin concentrations and ST segment depression turned out to be the most reliable individual prognostic factors indicating the effectiveness of the upcoming invasive intervention. The reasons for the high prognostic significance of such a factor as troponin concentration have not yet been established.
7.3. Duration of period between diagnostic angiography and invasive intervention
The length of the period between diagnostic angiography and invasive intervention has been the subject of much debate. Five prospective randomized controlled trials compared the effectiveness of early and late invasive interventions (Table 10).
There is extensive evidence regarding the preferable use of an invasive approach in the early period of the disease compared to a conservative one. To date, there is no reliable evidence that any specific delay period before invasive intervention, during which only pharmacological therapy (including potent antithrombotic drugs) would be used, has any advantages over adequate drug therapy in combination with both it is possible to perform angiography earlier [65]. The incidence of ischemic events, as well as hemorrhagic complications, is reduced, and the duration of patient hospitalization is shortened with the early (but not delayed) use of invasive intervention. In high-risk patients (GRACE score > 140), angiography should be performed as soon as possible, within the next 24 hours [66].
Patients with extremely high risk were excluded from the observation groups of the above randomized controlled trials, therefore invasive interventions were not performed for life-saving reasons. Therefore, patients with ongoing symptoms and significant ST segment depression in the anterior leads (especially in combination with elevated troponin concentrations) appear to be suffering from transmural posterior wall ischemia and should undergo coronary angiography urgently (Table 1). eleven). Moreover, patients at high risk of thrombotic complications or progression of ACS to MI should be urgently (immediately) evaluated using angiography.
In low-risk patients with non-ST-segment elevation ACS, angiography and subsequent myocardial revascularization can safely be delayed but should be performed during the same hospitalization, preferably within the first 72 hours of admission.
Table 10. Randomized clinical trials comparing different invasive strategies
| Early invasive intervention/conservative approach | Early/late invasive intervention | ||||||||||
| Study | FRISC | TRUCKS | TIMI I 8 | VINO | RITA-3 | ICTUS | ELISA | ISAR-COOL | OPTIMA | TIMACS | ABOARD |
| Number of patients | |||||||||||
| Period | 1996–1998 | 1997–1998 | 1997–1999 | 1998–2000 | 1997–2002 | 2001–2003 | 2000–2001 | 2000–2002 | 2004–2007 | 2003–2008 | 2006–2008 |
| Period before angiography1, h | 96/408 | 48/120 | 22/79 | 6,2/1464 | 48/1020 | 23/283 | 6/50 | 2.4/86 | 0.5/25 | 14/50 | 1.2/21 |
| Average age, years | |||||||||||
| Women, % | |||||||||||
| Diabetes, % | |||||||||||
| ↑ troponins at the time of inclusion, % | No data | ||||||||||
| Patient ratio1.2, % | 78/45 | 100/61 | 64/45 | 73/39 | 57/28 | 79/54 | 74/77 | 78/72 | 100/99 | 74/69 | 91/81 |
| Performing PCI/CABG1, % | 30/27 | 43/16 | 36/19 | 50/27 | 26/17 | 51/10 | 54/15 | 68/8 | 99/0 | 57/28 | 63/2 |
| Main indicators studied | S/MI 6 months | S/IM/P | S/MI/G 6 months | S/MI 6 months | S/MI 12 months | S/MI/G 12 months | MI area, LDH level | S/MI 1 month | S/MI/HR 30 days | S/IM/I 6 months | Troponi-nov level |
| Achievement of primary endpoint | + | — | + | + | + | — | + | + | — | — | — |
| 1 At the time of achievement of the primary endpoint of the study. 2 Proportion of patients treated with early invasive intervention/conservative approach or early/late invasive intervention, respectively. C – incidence of death, P – duration of hospital treatment; D – frequency of re-hospitalization; I is the incidence of strokes; VR – unplanned revascularization |
Table 11. Main prognostic factors indicating a high risk of developing thrombotic complications and disease progression (with the occurrence of MI), and therefore the need for emergency coronary angiography
| Ongoing or recurrent ischemia |
| Spontaneous dynamic changes in the ST segment (depression > 0.1 mV or transient elevation) |
| Deep ST segment depression in the anterior leads (V2–V4), indicating ongoing transmural ischemia of the posterior wall |
| Instability of hemodynamic parameters |
| Development of severe ventricular arrhythmias |
7.4. Coronary angiography, percutaneous coronary intervention and coronary artery bypass grafting
The invasive approach always begins with angiography. Only after a thorough study of the anatomical structure of the coronary vessels and lesions and the risks associated with them can a decision be made regarding the use of one or another type of invasive intervention. Angiography, in combination with recording changes on the ECG, in almost all cases makes it possible to identify the damage that causes the development of the disease. The detection on angiograms of an eccentrically located formation with uneven contours, ulcerations or filling defects allows us to suspect the presence of blood clots in the lumen of the vessel. When clinically significant lesions located on the surface of the vessel are detected, as well as in patients with multivessel disease, the calculation of partial coronary reserve provides additional important information for making decisions regarding the choice of management tactics for such patients [28]. Angiography should be performed for diagnostic purposes urgently in patients at high risk, as well as in those individuals who require differential diagnosis to clarify the nature of the acute clinical situation. Particularly in patients with ongoing symptoms and significantly elevated troponin levels in the absence of diagnostic changes on the ECG, identification of acute thrombotic occlusion (especially in the lumen of the circumflex coronary artery) is extremely important.
In all studies that compared the effectiveness of early versus late invasive intervention, as well as invasive versus medical approaches, patients who had undergone either CABG or PCI were included in the observation groups at the discretion of the investigators. To date, no specific prospective RCTs have been conducted to study the preferred choice of one intervention or another in patients with non-ST segment elevation ACS. In patients with stable general condition after ACS, there is apparently no need to interpret the results of RCTs differently, which compared the effectiveness of two interventions for myocardial revascularization in patients with stable coronary artery disease. The choice of the type of intervention for myocardial revascularization should be determined by the severity and extent of coronary artery disease.
If in a particular clinical situation it is preferable to perform PCI, it is recommended to use angiography and ECG to identify the lesion that caused the development of the disease and focus primarily on it. If an angiographic study revealed numerous clinically insignificant stenoses or lesions, the severity and significance of which are generally difficult to assess, routine determination of the partial coronary reserve index is recommended to resolve the issue of further treatment tactics for such a patient [28]. Until now, there have been no RCTs that compared the effectiveness of stenting several vessels simultaneously or stenting a single lesion that caused the development of the disease. The optimal timing of invasive intervention differs between PCI and CABG. Thus, in patients with non-ST segment elevation ACS, the best results and clinical outcomes were observed when this intervention was performed as early as possible. The best results of CABG were observed in situations where this intervention was carried out in a slightly delayed period, a few days after complete stabilization of the patient’s condition.
7.5. Selected patient populations
Although certain subgroups of patients, such as women or older people, are at increased risk for bleeding complications, there is no data to support the assumption that patients in these groups should be treated differently than patients included in the observation groups of RCTs. A meta-analysis summarizing the results of 8 RCTs demonstrated that an early invasive approach in biomarker-positive women was as effective as in men [67]. However, biomarker-negative women tended to experience more adverse events when they had an early invasive procedure. Therefore, early invasive procedures should be avoided in low-risk troponin-negative women.
Age is one of the most significant risk factors; however, early invasive interventions in elderly patients turned out to be the same or even more effective than in people of other age categories [59]. When choosing management tactics for elderly patients, priority should be given to the following goals and objectives: complete elimination of symptoms of the disease and prevention hemorrhagic complications.
In table 12 lists recommendations for performing myocardial revascularization in patients with non-ST segment elevation ACS.
Table 12. Recommendations for revascularization in patients with acute coronary syndrome without ST-segment elevation
| Recommendations | Class of clinical recommendations | Level of evidence | Source |
| The use of an invasive approach is indicated in patients: · with a GRACE score > 140 or with at least one very high risk criterion; · presence of recurrent symptoms of the disease; · presence of latent myocardial ischemia, which was identified using stress tests | I | A | 64, 68–70 |
| Early (<24 hours) invasive approach is indicated in patients with a GRACE score >140 or multiple very high risk factors | I | A | 63, 64, 66, 70–72 |
| A late invasive approach (within the first 72 hours) is indicated in patients with a GRACE score < 140 who do not have multiple very high risk factors but have recurrent disease symptoms or occult myocardial ischemia that has been identified by stress testing | I | A | 59, 66, 68 |
| In patients with an extremely high risk of developing ischemic complications (with refractory angina, concomitant heart failure, cardiac arrhythmias, or hemodynamic instability), urgent (< 2 hours) coronary angiography is indicated | IIa | C | – |
| The invasive approach should not be used in patients: · at low overall risk; with an extremely high risk of performing invasive diagnostic and therapeutic procedures | III | A | 59 ,68 |
8. Carrying out myocardial revascularization in myocardial infarction with ST segment elevation
8.1. Selection of approaches to ensure myocardial reperfusion
Treatment of atherosclerosis
HMG-CoA reductase inhibitors (statins) are used to treat atherosclerosis. They influence cholesterol metabolism, helping to dissolve existing plaques and reduce cholesterol and lipids in the blood, and also prevent the formation of new atherosclerotic deposits.
Treatment of atherosclerosis often eliminates pathological narrowing
In clinical studies, the use of atorvastatin and rosuvastatin showed significant clearance of aa. coronaria from cholesterol plaques. Which leads to a decrease in cardiovascular failure and a decrease in the risk of myocardial infarction.
Surgery
Modern surgery has in its arsenal three types of operations for narrowing of the coronary vessels:
- Endarterectomy (removal of blood clot);
- Vascular bypass surgery;
- Vascular stenting.
Endarterectomy
This operation involves surgical removal of a blood clot from the lumen of a coronary vessel. One of its varieties is atherectomy (removal of cholesterol plaque due to atherosclerosis).
Both of these interventions are now almost never used, since their implementation is not only associated with high risks, but also often leads to recurrent thrombus formation. Therefore, doctors prefer other types of operations.
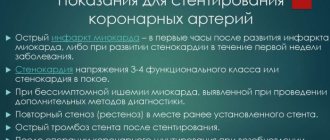
Stenting
This operation can be performed either planned to prevent myocardial infarction, or urgently when it develops to eliminate ischemia and restore blood supply to the heart muscle.
This surgical intervention consists of installing a stent in the affected vessel. This is done through the femoral artery, so stenting is a minimally invasive procedure that does not require large incisions and general anesthesia. With the help of a guide, the stent is delivered to its destination - the affected artery.
It is installed in it and then straightened out. The design of this device allows the vessel to be maintained in a dilated state to its normal diameter, which ensures adequate blood flow.
Stenting mechanism
The entire course of the procedure and the correct positioning of the stent are controlled by X-ray equipment, so the operation requires special equipment in the operating room.
You can learn more about this type of surgery from the video in this article.
Bypass surgery
Coronary artery bypass surgery involves providing a bypass path for blood flow and disconnecting the affected artery from it. A shunt is created using the patient's own vein or artery, which allows blood flow to the heart muscle to be restored, bypassing the blocked vessel.
The operation diagram is shown in the photo below:
CABG
This operation is very traumatic, as it requires the use of a heart-lung machine and opening the chest. The rehabilitation period is usually long and difficult, and complications often arise.
Prevention
Prevention of this disease is aimed primarily at preventing heart and vascular diseases and includes:
- proper nutrition with a low fat content (see Foods that are good for the heart and blood vessels: what to eat to keep our “engine” healthy for many years);
- daily drinking regime;
- active lifestyle (sports, walks, active entertainment);
- timely treatment of chronic diseases;
- annual medical examination.
This instruction will not completely protect against the risk of developing pathology, but will reduce it to a minimum.
The prognosis for life and recovery directly depends on how early the stenosis was detected. Therefore, at the first signs of the development of heart failure, it is recommended to consult a cardiologist for examination. Timely treatment will allow you to avoid the development of serious complications and surgical interventions, limiting yourself to conservative therapy.