The term hypoxia comes from the Greek hypo- and Latin oxy [genium] (translated as oxygen). The term means oxygen starvation. Everyone knows that oxygen is critically important in the life of cellular organisms. Oxygen is especially important for brain cells, to which the nervous system is closed.
It is no coincidence that about 20% of all blood circulating in the human body is delivered to the brain tissue. Approximately 3.3 ml of oxygen is required for 100 g of tissue every minute. A decrease in this volume is called cerebral hypoxia.
Oxygen is delivered to brain cells using the blood, which takes it up in the lung tissues. There are many reasons for the deterioration of oxygen delivery. But the main thing is the consequences of this. Oxygen deficiency brings with it many problems. Up to and including death.
Causes
A common cause of oxygen starvation may be a lack of oxygen entering the body or a cessation of its absorption by body tissues. This is facilitated either by unfavorable external factors or certain diseases and conditions. If oxygen starvation develops as a result of a lack of oxygen in the inhaled air, then the form of pathology is called exogenous. Its reasons are:
- staying in wells, mines, submarines or other enclosed spaces that have no communication with the outside environment;
- smog in the city, severe gas pollution;
- poor ventilation;
- malfunction of anesthesia-respiratory equipment;
- being in a room where there are many people;
- thin atmosphere at altitude (pilot illness, mountain and altitude sickness).
If the pathology is the result of any disease or condition of the body, then it is called endogenous. The reasons for this type of oxygen starvation are:
- diseases of the respiratory system, such as asbestosis (deposition of asbestos dust in the lungs), pneumothorax, hemothorax (filling of the pleural cavity with air or blood), bronchospasm, bronchitis, pneumonia;
- the presence of foreign bodies in the bronchi, for example, after accidental ingestion;
- acquired or congenital heart defects;
- fractures and displacements of the chest bones;
- diseases or pathologies of the heart, such as heart attack, heart failure, pericardial obliteration, cardiosclerosis (replacement of the heart muscle with connective tissue);
- injuries, tumors and other brain diseases that damage the respiratory center of the central nervous system;
- venous hyperemia (plethora);
- congestion in the system of the superior or inferior vena cava;
- acute blood loss;
- asphyxia (suffocation) of any nature;
- a sharp narrowing of blood vessels in various organs.
Intrauterine fetal hypoxia
For an unborn baby, oxygen deficiency is very dangerous. It causes serious complications: in the early stages of pregnancy - slowdown or pathology of fetal development, in the late stages - damage to the central nervous system. Oxygen starvation of a child can be caused by some systemic diseases of a pregnant woman, including:
- pathologies of the cardiovascular system, which lead to vascular spasms and deterioration of blood supply to the fetus;
- diseases of internal organs, such as pyelonephritis and inflammation of the urinary system;
- iron deficiency anemia, which interferes with the supply of oxygen to tissues;
- chronic diseases of the respiratory organs, for example, bronchial asthma or asthmatic bronchitis;
- disturbances in the functioning of the endocrine system.
Hypoxia during pregnancy is often associated with a woman’s bad habits. A pregnant woman is strictly prohibited from smoking and drinking alcohol. All toxins enter the baby's bloodstream and lead to serious complications. Fetal hypoxia can also be associated with other disorders:
- abnormalities in the development of the placenta or umbilical cord;
- post-term pregnancy;
- increased uterine tone;
- premature placental abruption;
- infection of the fetus;
- incompatibility of fetal blood with maternal blood according to the Rh factor;
- prolonged compression of the head in the birth canal;
- entwining the umbilical cord around the neck;
- entry into the respiratory tract of mucus or amniotic fluid.
Risk factors for the development of cerebral hypoxia
The main risk factors contributing to the development of oxygen starvation in brain tissue include:
- smoking;
- alcohol abuse;
- high blood pressure;
- obesity;
- the patient has diseases of the cardiovascular system, diabetes mellitus, severe atherosclerosis, blood clotting disorders, autoimmune diseases, oncology;
- drug use;
- presence of severe anemia.
Risk factors for the development of intrauterine fetal hypoxia include the presence of anemia in the mother, smoking during pregnancy, multiple pregnancies, the presence of severe gestosis during pregnancy, fetoplacental insufficiency, entanglement of the umbilical cord during childbirth, and the presence of diabetes mellitus in the pregnant woman.
Signs
Hypoxia in a person can be determined by certain signs. There are symptoms common to all types of oxygen deprivation. They appear when the brain absorbs less than its fair share of oxygen. With this disorder, the following symptoms are observed:
- Nervous system inhibition. Has a pronounced character. The patient complains of nausea, headache and dizziness. Sometimes visual disturbances and even loss of consciousness are observed.
- Increased excitability. The person ceases to control speech and movements and feels in a state of euphoria.
- Change in skin tone. The person's face begins to turn pale and then turns blue or red. Cold sweat indicates that the brain is trying to cope with the condition on its own.
- Brain damage. Develops in severe oxygen deprivation and can lead to cerebral edema. This condition is accompanied by the loss of all reflexes and disruption of the functioning and structure of organs. The patient falls into a coma.
Acute hypoxia
The symptoms of oxygen deficiency are somewhat different for acute and chronic forms. In the case of fulminant oxygen starvation, not a single symptom has time to appear, because death occurs within 2-3 minutes. This condition is very dangerous and requires emergency help. The acute form of hypoxia develops within 2-3 hours and is characterized by the following symptoms:
- decrease in heart rate;
- drop in blood pressure;
- change in total blood volume;
- breathing becomes irregular;
- coma and agony followed by death if hypoxia was not eliminated at the initial stage.
Chronic
This form of hypoxia is manifested by hypoxic syndrome. In this case, symptoms from the central nervous system are observed. The brain is sensitive to oxygen starvation. Foci of hemorrhage, necrosis and other signs of cell destruction develop in the tissues of the organ. At an early stage, these changes cause a person to experience a state of euphoria and motor restlessness.
As hypoxia progresses, the cerebral cortex is depressed. Symptoms resemble those of alcohol intoxication. The patient experiences the following sensations:
- convulsions;
- drowsiness;
- nausea, vomiting;
- involuntary passage of urine and feces;
- disturbance of consciousness;
- noise in ears;
- lethargy;
- headache;
- dizziness;
- impaired coordination of movements;
- lethargy.
With convulsions, the development of opisthotonus is possible - a condition in which a person arches, his neck and back muscles straighten, his head throws back, and his arms bend at the elbows. The pose resembles a “bridge” figure. In addition to signs of depression of the cerebral cortex, during hypoxia the following are observed:
- pain in the heart area;
- a sharp decrease in vascular tone;
- tachycardia;
- low body temperature;
- dyspnea;
- depression;
- drop in blood pressure;
- cyanosis - blueness of the skin;
- irregular breathing;
- delirium – “delirium tremens”;
- Korsakov's syndrome - loss of orientation, amnesia, replacement of real events with fictitious ones.
Features of the course of brain hypoxia
The development of compensatory mechanisms is possible only with chronic, slowly progressive cerebral hypoxia. In acute cerebral hypoxia, the pathogenesis of oxygen starvation most often resembles the picture of ischemic stroke.
For reference. Restoration of the functions of brain neurons is possible within 6-8 minutes after the onset of acute total hypoxia. After this, the process of forming irreversible changes in the cerebral cortex begins.
With timely initiation of treatment, it is possible to restore brain tissue within an average of 3-6 hours (depending on the severity of acute hypoxia).
Types of hypoxia
According to the type of prevalence of oxygen starvation, hypoxia can be general or local. The broadest classification divides this condition into types depending on the etiology, i.e. reasons for occurrence. So, hypoxia happens:
- Exogenous. Also called hypoxic hypoxia, which is caused by environmental factors. Pathology develops due to insufficient oxygen supply to the body.
- Endogenous. Associated with third-party diseases or disorders.
Endogenous hypoxia is divided into several subtypes depending on the etiology. Each type has a specific cause:
- Respiratory (pulmonary, respiratory). It develops due to obstructions in the area of the pulmonary alveoli, which prevents hemoglobin from immediately contacting oxygen.
- Circulatory. Occurs due to a disorder of circulatory processes. According to the mechanism of development, it is divided into ischemic and stagnant.
- Hemic. It is observed with a rapid decrease in hemoglobin. Hemic hypoxia can be anemic or caused by a deterioration in the quality of hemoglobin.
- Fabric. Associated with the cessation of oxygen absorption due to suppression of enzyme activity. Tissue hypoxia is observed with radiation, poisoning with toxic substances of microbes, carbon monoxide or salts of heavy metals.
- Substrate. Against the background of normal oxygen transportation, there is a lack of nutrients. More often observed with diabetes mellitus or prolonged fasting.
- Reloading. Occurs after heavy physical exertion.
- Mixed. It is the most serious type and is observed in cases of serious life-threatening pathologies, for example, coma or poisoning.
The following classification divides hypoxia into types, taking into account the rate of development of oxygen starvation. The most dangerous is the one that manifests itself very quickly, because it often leads to death. In general, there are the following types of hypoxia:
- chronic – lasts from several weeks to a couple of years;
- subacute – develops within 5 hours;
- acute – lasts no more than 2 hours;
- lightning fast - lasts 2-3 minutes.
Definition
Hypoxia is a condition in which the body is deprived of oxygen supply at the tissue level. Hypoxia is classified as generalized, affecting the entire body, or local, affecting specific organs. Although hypoxia is a pathological disease, different levels of arterial oxygen concentration are acceptable in the case of certain physical conditions, for example, during training in hypoventilation or vigorous exercise.
Exogenous or hypoxic hypoxia is associated with ascents to high altitudes, and this causes altitude sickness even in healthy people, leading to fatal consequences: pulmonary edema and acute cerebral edema of the brain. Hypoxia also occurs in healthy people when inhaling gas mixtures with low oxygen concentrations, such as when diving while using closed rebreather systems that control the oxygen content of the supplied air. An artificially induced moderate state of hypoxia is used specifically during training at high altitudes to develop adaptations at both the systemic and cellular levels.
Hypoxia is a common complication in newborns resulting from premature birth. Because the fetus's lungs develop toward the end of the third trimester, premature babies are often born with underdeveloped lungs. Infants at risk of hypoxia are placed in incubators, which provide small organisms with oxygen and positive airway pressure.
Degrees
Hypoxia is classified according to the severity of its symptoms and the severity of oxygen deficiency. Taking these factors into account, oxygen deficiency has the following degrees:
- Critical. Hypoxic syndrome leads to coma or shock and can result in agony and death.
- Heavy. The lack of oxygen is severe, and the risk of developing a coma is high.
- Moderate. Clinical signs of hypoxia appear at rest.
- Easy. Oxygen starvation occurs only during physical activity.
Consequences
Oxygen deficiency affects the functioning of all organs and systems. The consequences depend on the period in which the pathology was eliminated and how long it lasted. If the compensatory mechanisms have not yet been exhausted, and the oxygen deficiency has been eliminated, then no negative consequences will arise. When the pathology appears during the period of decompensation, complications are determined by the duration of oxygen starvation.
The brain suffers more from this condition, because without oxygen it can only withstand 3-4 minutes. The cells may then die. The liver, kidneys and heart are kept for about 30-40 minutes. The main consequences of oxygen deficiency:
- depletion of adaptation reserves;
- weakening of antitumor protection;
- decreased immunity;
- deterioration of memory and reaction speed;
- neuropsychiatric syndrome;
- psychosis;
- dementia;
- parkinsonism (shaking palsy);
- exercise intolerance;
- fatty degeneration of muscle cells, myocardium, and liver.
Consequences for the child
Oxygen deficiency is one of the common causes of not only fetal mortality, but also the appearance of developmental defects. The consequences depend on the trimester of pregnancy and the degree of oxygen deficiency:
- First trimester. During this period, the laying of organs occurs, therefore, due to oxygen deficiency, a slowdown in the development of the embryo and the formation of anomalies are possible.
- Second trimester. At this stage, problems arise with the baby’s adaptation and pathologies of the central nervous system. In the chronic form, the death of the child is possible.
- Third trimester. Lack of oxygen provokes developmental delays during pregnancy. Serious damage to the baby's nervous system is also possible. During childbirth, oxygen deprivation causes asphyxia.
Consequences of fetal hypoxia in a child after birth
Experiencing oxygen deprivation after the birth of a baby seriously affects his health. The child becomes restless, easily excitable, and suffers from high muscle tone. The latter is expressed in frequent twitching of the legs or arms, convulsions, and trembling of the chin. Other symptoms include lethargy, frequent regurgitation and reluctance to latch on to the breast. A list of more serious consequences includes:
- stillbirth;
- death in the early postpartum period;
- impairment or delay of psychomotor and intellectual development;
- damage to blood vessels and heart;
- diseases of the nervous system;
- problems with the urinary organs;
- severe eye diseases.
Oxygen starvation: symptoms
Symptoms of oxygen starvation are shortness of breath, tachycardia (fast pulse), dizziness, loss of consciousness, convulsions. In the acute form, death occurs without treatment. Chronic hypoxia occurs over a long period of time with impaired brain function (depression, poor memory), constant fatigue, and insomnia.
Stages of development
There are five stages of hypoxia. They manifest themselves most clearly with a sudden (acute) cessation of oxygen supply, and in chronic forms they are extended over time.
First
It occurs hidden, as the body turns on defense mechanisms. The state of health is normal, the mood improves, the pace of movements increases, criticism of the condition disappears, coordination of movements and stability are impaired.
Second
Compensation is still possible, the following processes occur:
- activation of brain centers;
- the frequency of breathing and heart contractions increases;
- the level of red blood cells, hemoglobin, and oxygen uptake by cells from the blood increases;
- nutrition of organs increases (primarily the brain and heart due to blood redistribution).
Signs of the compensatory stage:
- rapid pulse;
- heaviness in the head;
- general weakness;
- decreased performance;
- slow movements and speech;
- mental and physical activity are difficult.
Third
Compensatory possibilities have been exhausted; the organs have nothing to obtain additional nutrition from. The balance of sodium and potassium ions is disrupted, and the level of toxic metabolic products (under-oxidized) increases. Symptoms of decompensation:
- headache and heart pain;
- nausea, vomiting;
- convulsive muscle twitching;
- performance decreases significantly;
- pale skin;
- darkening of the eyes;
- dizziness.
Fourth
Severe oxygen starvation, the level of oxygen in the blood drops, the concentration of toxins and acids increases, cell membranes are destroyed. Manifestations:
- rare breathing;
- slow and weak pulse;
- drop in blood pressure;
- convulsions;
- lack of consciousness;
- involuntary bowel and bladder emptying.
Fifth
The final stage is an excess of toxins in the blood and a critical drop in oxygen, active destruction of cells, accumulation of water inside the tissues, irreversible damage. Breathing in the form of irregular single deep breaths, drop in pressure, rare heart contractions, death.
Signs of acute hypoxia
Acute hypoxia manifests itself with rapidly increasing symptoms:
- frequent, then rare breathing;
- rapid contraction rhythm, interruptions, then a weak and rare pulse, an increase with a drop in pressure;
- decreased criticism of well-being, excitement turning into drowsiness; lethargy, lightheadedness, loss of consciousness, convulsions;
- decreased volume of urine excreted;
- loss of appetite, nausea, vomiting.
Symptoms of chronic
The main signs of chronic oxygen starvation include:
- headaches, heart pain;
- constant fatigue;
- low mood, depression;
- deterioration of hearing and vision;
- sleep disorders – daytime sleepiness, insomnia at night;
- shortness of breath and rapid pulse with little physical activity;
- difficulty learning new information, concentrating, memory loss.
How to determine fetal hypoxia
You can suspect a lack of oxygen in your baby based on high physical activity. It is a reflex by which the child tries to restore normal blood flow and increase blood supply. A pregnant woman feels the following:
- violent movement of the baby;
- sudden strong shocks that cause pain and discomfort;
- with increasing oxygen deficiency, a gradual weakening of the tremors, which may disappear completely.
At the last sign, a woman should be wary. In general, fetal activity in the antenatal clinic is observed from the 28th week of pregnancy. When determining intrauterine oxygen deficiency, doctors use the following methods:
- Listening to heart sounds. For this purpose, a stethoscope is used - a special obstetric device. It allows you to evaluate the tone, rhythm and heart rate, and notice extraneous noise.
- Cardiotocography. It is a recording of the heart rhythm on paper using a special ultrasonic sensor.
- Doppler. It consists of studying abnormalities in blood flow between the fetus and the woman. The method helps determine the severity of oxygen starvation.
In addition to the basic methods, laboratory blood tests are used to determine hormone levels and biochemical composition. To confirm hypoxia, amniotic fluid is examined for the presence of original feces - meconium. It indicates relaxation of the baby's rectal muscles due to lack of oxygen. This diagnostic method plays an important role in the progression of labor. The entire birth process will depend on it.
Diagnosis of cerebral hypoxia
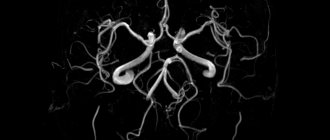
To diagnose oxygen starvation of the brain, the following can be used:
- electroencephalogram;
- angiography of neck and brain vessels;
- MRI and CT scan of the neck and brain;
- X-ray of the cervical spine;
- complete blood count + iron level;
- coagulogram;
- assessment of blood oxygen saturation;
- ECG and ultrasound of the heart;
- fundus examination;
- blood pressure monitoring;
- control blood sugar levels.
An examination by a neurologist and cardiologist is also required.
Treatment
In most cases, a mixed form of oxygen deficiency is noted. For this reason, the treatment approach must be comprehensive. To maintain the supply of oxygen to cells, hyperbaric oxygenation is used - a procedure for pumping this gas into the lungs under pressure. It provides:
- dissolution of oxygen directly in the blood without binding to red blood cells;
- delivery of oxygen to all tissues and organs;
- dilation of blood vessels in the heart and brain;
- organs work at full capacity.
For the circulatory form, taking heart medications and medications that increase blood pressure is indicated. In case of blood loss incompatible with life, a blood transfusion is required. Hemic hypoxia, in addition to hyperbaric oxygen therapy, is treated using the following procedures:
- blood or red blood cell transfusions;
- administration of drugs that perform the functions of enzymes;
- plasmapheresis and hemosorption (blood purification);
- administration of oxygen carriers, glucose or steroid hormones.
During pregnancy, treatment of oxygen deficiency is aimed at normalizing blood circulation in the placenta. This helps ensure that nutrients and oxygen reach the fetus. Preparations and methods used:
- relax the myometrium;
- improve rheological blood parameters;
- dilate the uteroplacental vessels;
- stimulate metabolism in the placenta and myometrium.
Every day a woman needs to breathe a mixture of oxygen and air. Medicines are prescribed only by a doctor. A specialist may prescribe the following medications:
- Szigetin;
- Trental;
- Methionine;
- Heparin;
- Chime;
- Vitamins E and C;
- glutamic acid;
- Haloscarbine;
- Lipostabil.
In case of oxygen starvation at 28-32 weeks, emergency delivery is necessary. The same applies to the deterioration of biochemical blood parameters, the appearance of meconium in the amniotic fluid, and oligohydramnios. As preparation for obstetric or surgical resolution of childbirth, the following is used:
- breathing with humidified oxygen;
- intravenous administration of glucose;
- introduction of Sigetin, Cocarboxylase and ascorbic acid, Euphyllin.
If oxygen deficiency is suspected at birth, the baby is immediately provided with medical assistance. Mucus and fluid are removed from the respiratory tract, the child is warmed, and, if necessary, resuscitation measures are carried out to ensure that the threat to life is eliminated. When the newborn's condition has stabilized, he is placed in a pressure chamber. There he obtains nutrient solutions. As you grow older, excitability, convulsions, twitching of arms and legs gradually stop, but at 5-6 months a relapse of the pathology is possible.
Oxygen deficiency in a newborn
Fetal hypoxia is a lack of oxygen in the blood or tissues. Mechanisms responsible for child hypoxia include:
- abnormal oxygen flow across the placenta;
- improper gas exchange through the placenta;
- other diseases in women.
Sometimes, during or immediately after birth, the baby's brain is hypoxic. Then the so-called perinatal hypoxia appears. This can occur, for example, as a result of umbilical cord pressure or improper oxygenation of the fetus.
Prevention of hypoxia
Measures to prevent oxygen starvation are aimed at preventing conditions that lead to this. A person should lead an active lifestyle, walk more often, play sports and eat right. Chronic diseases need to be treated on time. When working in stuffy rooms, they must be regularly ventilated. Prevention during pregnancy is as follows:
- drinking oxygen cocktails;
- swimming;
- singing (develops proper breathing);
- doing normal household chores (a regimen with minor physical activity supplies the muscles with oxygen);
- ensuring a calm environment;
- walks in the open air;
- full healthy sleep;
- a balanced diet with foods rich in potassium, iron, iodine;
- tracking fetal movements (normally, the baby moves about 10 times a day);
- regular visits to the doctor.