The diagnosis of “microinfarction” sounds more reassuring than a regular myocardial infarction. However, it is too early to calm down: a microinfarction suffered on the legs, in which the patient does not receive the necessary treatment, is often complicated by extensive necrosis of the heart muscle. At the same time, it is impossible to predict the onset of large-focal, deep myocardial damage, and a critical situation in the vast majority of cases ends in death. To avoid a catastrophe, you should know the first signs of a microinfarction, symptoms after myocardial necrosis has occurred, and emergency measures if severe heart damage is suspected.
How does a microinfarction develop?
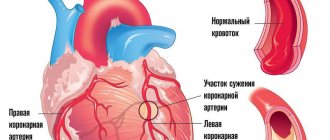
The myocardium is the heart muscle that contracts and releases portions of blood into the aorta. This blood is then distributed through the arteries, supplying the entire body with oxygen and removing carbon dioxide from the tissues. The myocardium itself also has arteries that supply it with blood, the so-called coronary arteries (from the Latin word cor - “heart”).
A heart attack is a dysfunction of a part of the heart muscle caused by the cessation of its blood supply. The most common cause of this is coronary heart disease, which is based on the formation of cholesterol plaques on the walls of the coronary arteries.
Sooner or later, such a plaque either completely blocks the lumen of the artery, or is damaged, and a blood clot forms on its surface. In both cases, blood flow through the artery stops, and part of the heart muscle experiences oxygen deficiency.
Under such conditions, heart cells can live for about 15 to 30 minutes, and then they die. Gradually, a scar forms in their place.
Depending on the size of the lesion, 3 forms of the disease were previously distinguished:
- Microinfarction, or small-focal, when only a small part of the heart cells died, and the functioning of the heart was practically not affected;
- Large-focal with preservation of part of the contracting myocardiocytes (heart cells) against the background of scarring;
- Transmural, after which there was almost end-to-end replacement of the myocardium with connective tissue (scar).
Microinfarction now has 2 official names:
- Myocardial infarction without Q wave.
- Non-Q-forming infarction.
The Q wave is formed at the site of scar changes. It is clear that with a small lesion, such as a microinfarction, the consequences are not so significant, and this wave does not appear on the ECG.
Thus, microinfarction is the form of the disease with the best prognosis for recovery. In many cases, heart function is completely restored after some time.
Why does a microinfarction occur?
The causes of microinfarction completely coincide with those of large-focal lesions. Doctors always name the main culprit of MI as atherosclerotic damage to the coronary arterial vessels and subsequent thrombosis of the coronary arteries, which supply this area with blood. A thrombus formed within a coronary artery is considered the main precursor to subsequent myocardial infarction. It itself is formed due to an atherosclerotic plaque that has arisen on the altered intima, or is the result of hemorrhage into the plaque itself.
occurrence of microinfarction/infarction
In addition, among the causes of microinfarction the following are noted:
- Local changes in blood vessels;
- Hypercholesterolemia;
- Diabetes;
- Increased adhesion and aggregation of the platelet component of blood cells;
- Arterial hypertension;
- Excessive stress of various kinds (physical and mental), which increases the need of the heart muscle for oxygen;
- Smoking;
- Spasm of unchanged (healthy) coronary arteries caused by fear, excitement or other circumstances.
The relationship between these reasons is obvious, with the exception of a sharp spasm of healthy blood vessels, all other factors interact and aggravate each other.
It should be noted that men are more prone to both microinfarction and infarction with deep lesions. For them, similar situations happen more often and earlier. As for women, hormones protect them for a long time, so a “young” heart attack is not typical for women.
Main reasons
The most common cause of a microinfarction is a blood clot in one of the small coronary arteries. It forms on the surface of a damaged atheromatous plaque. In about two-thirds of patients, it dissolves spontaneously within 24 hours, often accompanied by chest pain. However, in 30% of cases a small area of dead tissue forms.
In more rare cases, a microinfarction can be caused by:
- coronary artery embolism - blockage of a formation brought from outside, for example, with mitral or aortic stenosis, infective endocarditis;
- spasm of a coronary vessel under the influence of psychoactive substances or, for example, severe stress.
Consequences of “silent” small-focal infarction
A weak picture of a microinfarction is more of a minus than a plus. Patients come to the doctor with advanced heart pathologies that have arisen due to the failure to provide emergency medical care:
- swelling (fluid accumulation) in the lungs;
- irregular heartbeat;
- blood clot formation;
- severe damage to myocardial tissue.
If you do not pay attention to the cardiac signs that have arisen for a long time, more dangerous complications will begin to develop:
- severe arrhythmias that can only be controlled with medication;
- gradual thinning of the myocardial layer;
- reducing the intensity of contractions;
- blockage of blood vessels by blood clots;
- cardiosclerosis, causing valve deformation.
A heart attack suffered on the legs has a negative impact on current pathological processes (inflammation of the pericardium, heart failure, arrhythmia). They get significantly worse, which also leads to certain complications.
Ignoring a small-focal heart attack will increase the likelihood of its recurrence several times. Each time the patient’s condition will become worse due to an increase in areas of necrosis. Microinfarctions occur without consequences only in rare cases.
Symptoms and first signs
The signs of this disease are very similar to the symptoms of other acute coronary conditions (unstable angina, Q-wave myocardial infarction), so it is impossible to immediately differentiate these diseases based on the clinical picture.
At the very beginning of the process, they are combined into the concept of “acute coronary syndrome”. Depending on how events develop further, whether tissue necrosis will occur, what its size will be, and the final diagnosis will be established.
Difference between men and women
The symptoms and first signs of a microinfarction are similar in men and women. The difference lies in the age at which the disease most often occurs.
For men, this is 45–50 years; in women, microinfarction occurs more often after 55–60 years, since previously their blood vessels are under the “protection” of female sex hormones.
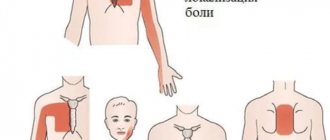
Symptoms that suggest a microinfarction are the same for both men and women:
- pain, pressure, tightness or burning behind the sternum that does not go away after taking 3 nitroglycerin tablets taken at intervals of 5 minutes each;
- pain radiating to the shoulder, collarbone, upper abdomen, back, neck, jaw;
- nausea or vomiting;
- sudden shortness of breath, feeling of lack of air;
- sudden heavy sweating and severe weakness;
- dizziness or loss of consciousness;
- feeling of anxiety, fear for your life.
Chest pain or discomfort that does not go away after taking nitroglycerin is the most common sign of a microinfarction. However, it is not observed in everyone. Some patients do not feel any particular unpleasant signs and do not notice the disease they have had. This is more common in women, older people and people with diabetes.
For example, a 65-year-old woman with diabetes may experience several of these infarcts in her legs, which together can significantly weaken the contractility of her heart muscle and cause heart failure.
The main thing is not to miss
The first signs of a so-called microinfarction in other cases are really scanty. People suffering from angina pectoris and accustomed to frequent heart pain may not pay attention and perceive the manifestations of small focal myocardial infarction as another attack of an old disease. In addition, it should be borne in mind that sometimes such a condition may not produce any symptoms or may occur in an atypical manner. In such cases, it is indeed difficult for the patient and his relatives to immediately suspect the presence of a microinfarction.
Meanwhile, it is probably worth recalling once again what can be expected from this pathology and how an attack called a mini- or micro-infarction can manifest itself:
- Pain of varying intensity. Sharp “dagger” pains are considered not only a sign of a large-focal infarction, but also a symptom of a microinfarction, but they are not always present. Typical pains are unbearable, burning, pressing, they can make their way from the chest between the shoulder blades to the stomach, radiate to the arm, neck, reach the face and linger in the lower jaw. With an atypical version of mini-myocardial infarction, the severity of pain is not so great or may be absent altogether. In addition, sometimes a completely asymptomatic course of an attack is possible, and the experienced heart attack is recorded on the ECG after some time, then the patient is informed that he suffered an MI on his legs.
- A nitroglycerin tablet taken urgently under the tongue and not having the desired effect is also, to some extent, a symptom of a micro-infarction or a heart attack in general.
- Cold sweat breaking through the body, weakness throughout the body, the patient feels bad, he understands that something serious has happened in the body.
- An increase in temperature (usually no higher than 38°C), which indicates that zones of necrosis (necrosis) have appeared in the myocardium, indicate a later period of myocardial infarction.
- A person is overcome by fear of death, anxiety, which is very reminiscent of a panic attack, but this is not her case. Here the disorder is due to objective reasons, the patient does not think that he is having a heart attack, he is really in a lot of pain, and the body gives a signal about the trouble that has happened.
The first signs and their variants, in principle, may not differ from those with deeper lesions, however, in other cases, atypical manifestations are more typical for small-focal infarction compared to large-focal myocardial infarction.
First aid
Treatment at home for microinfarction is not carried out, as this disease is deadly. If you suspect this pathology, you must call an ambulance, and in the meantime do the following:
- give the patient a semi-sitting position;
- give him a nitroglycerin tablet under the tongue and chew a quarter of an aspirin tablet, after 5 minutes you can repeat taking nitroglycerin, and after the next 5 minutes take another tablet;
- unfasten the tight belt, collar, open the window;
- reassure the patient, say that help is close, do not leave him alone;
- collect a few things - underwear, pajamas or robe, slippers, socks, personal hygiene items, passport, medical insurance and SNILS card;
- organize an ambulance meeting, open the door to the entrance, take the dog (if you have one) to the neighbors or at least to another room, if the patient needs to be transferred - think about who can help (the team may not include orderlies) , find out if access to the entrance is free.
Diet after microcardiac infarction
After suffering a micro-heart attack, it is recommended to follow a diet that includes the inclusion in the diet of fruits, vegetables, nuts, bread products made from wholemeal flour, pasta made from durum wheat, brown rice, seafood, and lean boiled meat. Dairy products consumed should have no more than 5-10% fat content, and should be consumed in moderation. To season salads and other foods, it is recommended to use only olive or vegetable oil. A little wine is also recommended, which is pre-diluted with water. In addition, it is advisable to limit salt intake, since if it is included in the diet in excess, blood pressure may increase.
How to recognize a microinfarction?
Recognition of a microinfarction consists of 4 main components:
- Clinical picture, symptoms and complaints of the patient.
- External inspection data.
- ECG picture.
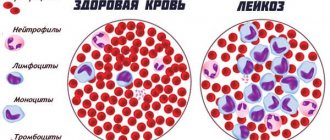
- The results of blood tests for troponins are substances that reflect the necrosis and destruction of myocardial cells that have occurred.
It is quite difficult to diagnose a microinfarction on an ECG. Usually, but not necessarily, in the first hours of an attack, an elevation of the ST segment is noted on the cardiogram. Subsequently, this segment returns to the isoline and a negative T wave is formed. This occurs during the first week of the disease. After about a month, the T wave may change from negative to positive again, and then in the future there will be no traces of the previous microinfarction on the ECG.
The same can be said about other research methods. With a microinfarction, there is no deep necrosis, and the heart muscle contracts almost normally. Therefore, on EchoCG there will be no zones of hypo- or akinesia (that is, scars).
With emergency coronary angiography performed in a hospital, doctors can detect a thrombosed artery. Treatment tactics will depend on its size and the time that has passed since the onset of the attack. Also, with a microinfarction, an increase in the level of troponins in the blood will be observed.
Literature
- Aravdeep Jhand, MBBS, Harish C. Devineni, MD, Gene Pershwitz, MD. Acute Coronary Syndromes: NSTE-ACS (Unstable Angina and NSTEMI)
- Galyavich A.S., Kamalov G.M. Galeeva Z.M., Baleeva L.V. Non-ST segment elevation myocardial infarction, 2017
- Syrkin A.L. , Dobrovolsky A.V. Acute coronary syndrome without ST segment elevation on ECG, 2011
- Natalie Olsen. NSTEMI: What You Need to Know, 2017
- Gilles Montalescot Jean Dallongeville Eric Van Belle Stephanie Rouanet Cathrine BaulacAlexia Degrandsart Eric Vicaut for the OPERA Investigators.
- STEMI and NSTEMI: are they so different? 1 year outcomes in acute myocardial infarction as defined by the ESC/ACC definition (the OPERA registry), 2007
Irina Kostyleva
Higher medical education. Kirov State Medical Academy (KSMA). Local therapist. More about the author
All articles by the author
What to take for treatment
The immediate goals of treatment are to relieve pain and improve circulation and heart function. Long-term goals of microinfarction treatment: prevention of complications, management of risk factors, reduction of the likelihood of recurrent heart attacks. A combination of medications and surgical procedures is used to achieve these goals.
Depending on the patient's condition, medications for acute and/or long-term therapy may include:
- thrombolytics, which dissolve a blood clot that has blocked an artery;
- analgesics, including narcotics, to relieve pain;
- nitroglycerin, which temporarily dilates the coronary arteries;
- antiplatelet drugs to prevent future blood clots;
- beta blockers, which slow down the pulse, reduce blood pressure and stress on the heart;
- ACEIs that improve blood circulation;
- angiotensin receptor blockers that control blood pressure;
- statins, which reduce the amount of cholesterol in the blood and stabilize atherosclerotic plaques.
If technically possible, angioplasty can be performed, during which a thin tube, a stent, is inserted into the affected coronary artery. If a patient has suffered many microinfarctions and constantly has angina attacks, he may be offered coronary artery bypass surgery.
Painful form
In essence, this is classic necrosis of cardiac structures. Symptoms of a microinfarction increase gradually and may be absent in some cases.
Treatment is carried out in a hospital; additional examinations are necessary to avoid complications. At a minimum, ECG, ECHO, measure blood pressure.
It is generally accepted that the first sign of a microinfarction is pain. This is not always fair. It all depends on the form. The assessment is carried out in a hospital setting.
Cardiac pathologies are assumed first of all. If a condition of this kind is excluded, other studies are prescribed (spirography, ultrasound, and others).
Consequences and prevention
With timely treatment, the consequences of a microinfarction for both men and women are usually favorable. Severe complications for this disease are not as typical as for larger necrosis of the heart muscle.
Having suffered a microinfarction on the legs can be accompanied by such consequences for women and men as:
- heart rhythm disturbances, blockades, extrasystole, rare pulse or attacks of rapid heartbeat;
- attacks of chest pain during exercise;
- with a large number of such microinfarctions, there is a gradual increase in shortness of breath and a decrease in exercise tolerance.
Prevention of microinfarction consists of eliminating risk factors for this disease:
- do not smoke, avoid passive smoking;
- eat more fruits, vegetables, whole grains, moderate amounts of low-fat dairy products and lean meats;
- exercise regularly or at least maintain possible, albeit small, but constant physical activity;
- Check your cholesterol levels regularly, avoid high-fat meat and dairy products, and take statins as prescribed by your doctor;
- monitor blood pressure and, if necessary, take medications daily to lower it;
- maintain a healthy weight;
- find a way to cope with stress, review your routine, perhaps move to calmer working conditions;
- give up alcohol.
Video from the “Health” program about the symptoms and methods of identifying a microinfarction:
We wish you to maintain a strong heart throughout your life, we hope our recommendations will be useful.
Symptoms that make you wary
As already noted, along with the typical manifestation of myocardial infarction, accompanied by the above symptoms, sometimes an attack occurs that no one mistakes for MI. This is not surprising, because weakness, fatigue, slight dizziness, slightly rapid heartbeat, decreased blood pressure and a short-term increase in temperature are more likely to look like a slight malaise and have nothing to do with the terrible diagnosis.
Even more errors occur due to the asymptomatic course of myocardial infarction. Usually this option is what patients have in mind when talking about a microinfarction that they suffered on their legs and accidentally found out about it after receiving a transcript of the electrocardiogram with the consequences recorded there (scars in the heart muscle).
In addition, an atypical variant of the disease is possible, which often misleads the patient, his relatives, and medical staff. Symptoms of a microinfarction in such cases may resemble another, sometimes unrelated, pathology:
- Asthmatic form
, more typical for elderly patients who already have ischemic heart disease (coronary heart disease), arterial hypertension, and signs of heart failure.
In most cases, this option does not cause pain, but is accompanied by shortness of breath, signs of cardiac asthma or pulmonary edema. Of course, in such a situation, where the main symptom of a microinfarction is suffocation
, it is difficult to consider damage to the heart muscle. - Abdominal or gastralgic form
, as a rule, occurs with diaphragmatic infarction. It all starts with intense pain in the epigastrium, accompanied by severe dyspeptic symptoms: nausea, vomiting, flatulence, which are confusing, simulating the clinic of an “acute abdomen”. The worst thing is that in such cases the patient is intensively treated for diseases of the digestive system: they wash the stomach, prepare for surgery, and sometimes even perform it. Of course, an error in diagnosis can be costly for a poor patient. - The arrhythmic variant
is characterized by moderate pain, sometimes there is no pain at all. Objective data reflect signs of obvious rhythm disturbance. Any of the arrhythmias can be suspected, which often happens during diagnosis. - The cerebral (apoplectiform), cerebrovascular form,
with its manifestations, is very similar to the symptoms of a dynamic (transient) cerebrovascular accident or transient ischemic attack. The first signs of trouble are headache, dizziness, motor and sensory disturbances, as well as mnestic disorders.
Atypical forms of MI include variants of the disease that occur with pain in unusual places (back, arms, right half of the body, etc.), but they can also be symptoms of a microinfarction.