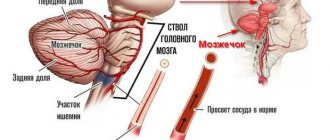
Brainstem stroke is a special case of cerebral stroke . With this pathology, problems with the blood supply to cells affect one of the most important parts of the brain - the brain stem. This structure is responsible for vital functions. And disruption of blood flow leads to their insufficiency.
A brainstem stroke is accompanied by the death of neurons in the main part of the brain—the brainstem. Tissue death occurs as a result of acute disruption of cerebral blood supply.
This type of stroke differs from others in that it poses an immediate threat to the life of the victim.
The blockage in the brain stem impairs vasomotor and respiratory function, disabling the person. In the absence of timely assistance, death is often recorded. The recovery prognosis does not exceed 3%.
What makes it special?
Ischemic brainstem stroke is the most dangerous type of brain damage, because all life-sustaining processes in the body occur under the control of its central brainstem. It is the connecting part of the brain and spinal cord. Its normal functioning affects a person's ability to move and process all instructions given to the body.
If the vascular structure in the trunk is damaged, other parts also suffer: the cerebellum, medulla oblongata and midbrain, and the pons. These departments are responsible for blood supply, breathing, swallowing and facial expressions.
As a result, this type of stroke has certain specifics:
- a person who has survived an attack loses the ability to swallow and speak;
- his function of regulating body temperature is impaired - it can deviate significantly both upward and downward;
- the heart rhythm is lost - the heart rate increases or slows down; when the rhythm slows down, the victim falls into a coma.
Diagnostic measures
To make a correct diagnosis, a detailed examination of the patient is required. The doctor can only assume the presence of a brain catastrophe based on the clinical picture.
Therefore, the victim undergoes a series of diagnostic procedures:
- Computed tomography, which provides three-dimensional visualization of the brain matter. The condition of the organ, the presence of damage, and ischemic phenomena are assessed.
- Magnetic resonance imaging, which allows you to study the organ in the smallest detail. The specialist evaluates the functioning of the brain and its blood circulation.
- Doppler ultrasound scan, which examines the carotid arteries.
- Angiography, which reveals the condition of the vascular channels and the presence of blood clots.
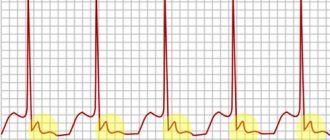
- An electrocardiogram that monitors the functioning of the heart muscle.
To obtain detailed information about the functioning of the heart, the victim is sent to an echocardiogram.
Types of pathology
According to the principle of action, stroke is divided into types:
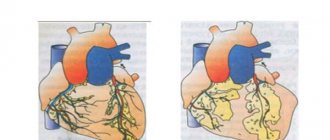
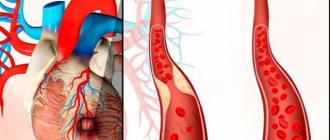
- Ischemic - is a vascular obstruction formed because the vessel is tightly blocked by a blood clot or cholesterol plaque. In this situation, the brain cells are no longer supplied with oxygen and die. Symptoms characteristic of an attack develop gradually.
- Hemorrhagic - characterized by hemorrhage into the brain structures due to rupture of the vascular walls. This type of stroke is characterized by a high rate of onset of symptoms: cerebral edema and increased intracranial pressure are formed, therefore, with the hemorrhagic type, the survival rate of patients is extremely low.
Before starting therapy, it is important to differentiate the types of this pathology from each other, since treatment plans are fundamentally different.
The main causes of strokes are blood clots and plaques in blood vessels, depletion of their walls, followed by rupture. But it is necessary to understand that such problems do not arise on their own; there are always prerequisites for their occurrence.
Most often, these are the consequences of specific diseases:
- stable hypertension and surges in blood pressure;
- vascular aneurysms;
- impaired blood clotting function;
- atherosclerosis of cerebral vessels;
- high cholesterol levels in the blood;
- cardiovascular diseases;
- fragility of vascular walls due to diabetes;
- disruption of the hormonal system due to incorrect use of oral contraceptives.
The presence of even one factor automatically places a person at risk of having a stroke. The majority of elderly people also fall into this group: due to age-related changes, cholesterol plaques form in their vessels.
What it is?
This type of stroke is a pathological condition in which cells in the brain stem gradually die. And this is the most important part of the organ, responsible for life support.
What function does the trunk perform?
The brain stem contains centers of the nervous system that regulate the vital functions of the body, namely respiratory and cardiovascular.
Therefore, due to the death of tissues in this area, their work is significantly disrupted, which leads to persistent disorders in the functioning of the body, even death.
Symptoms
The ability to identify the symptoms of a brainstem stroke greatly increases the victim’s chances of survival.
Since brainstem stroke also causes damage to other parts of the brain, the symptoms during an attack are quite extensive.
There are common signs of pathology, manifested by acute pain in the back of the head, dizziness, irregular heart rhythm, sudden changes in body temperature, loss of consciousness and paralysis.
Symptoms of ischemic stem stroke will be determined based on the area in which cell death occurred.
Symptoms may include:
- paralysis of the facial muscles from the damaged area of the trunk;
- paralysis extends to the muscles of the body;
- the tongue deviates to the affected side;
- loss of balance;
- drooping of the eyelid on the side where the stroke occurred;
- paralysis of the tissues of the soft palate;
- short, shallow breathing;
- difficulty swallowing;
- limb spasms.
Signs of brain hemorrhage appear suddenly and then increase very quickly.
The following symptoms indicate a hemorrhagic stroke:
- the muscles of the body are paralyzed;
- vision and synchronicity of movement of the eyeballs are impaired;
- speech function is impaired;
- nausea, vomiting;
- confusion;
- change in body temperature;
- coma.
Causes
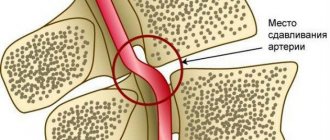
Trunk stroke is caused by the destruction or blockage of blood vessels.
Their rupture occurs with a sharp increase in blood pressure , in areas where the vascular walls are thinned or destructured.
Blood pressure increases with hypertension, significant physical and psychological stress, alcohol intake, and sudden climate changes.
However, destruction of blood vessels is possible only when the structure of their walls is weakened (loss of elasticity, appearance of defects, thinning).
Various diseases lead to this:
- atherosclerosis;
- diabetes;
- hypertonic disease;
- rheumatic type vasculitis;
- obesity, aneurysms;
- vascular malformations.
Particularly dangerous are bad habits - alcohol and smoking. Vascular weakness may be hereditary. The risk increases in older people (over 60 years of age), due to natural aging of tissues.
The ischemic process can be provoked by the following factors:
- atherothrombotic and atherosclerotic layers and narrowing of blood vessels in the neck and brain base;
- arterial and cardiogenic emboli;
- degenerative loss of tissue elasticity;
- hemorrhological disorders in terms of blood viscosity and clotting.
Cardiac problems such as atrial fibrillation, myocardial infarction, dilated cardiomyopathy and other heart defects can lead to serious problems.
First aid
Stroke damage to the brain after a few hours causes irreversible changes in brain structures - necrosis of a significant number of stem cells.
However, there is a time period for providing medical care to the victim, equal to 3-4 hours, during which the serious consequences of a stroke will be minimal.
Before the ambulance arrives, take the following measures:
- reassure the patient, do not create panic;
- Place the victim in bed so that the head is elevated 30 degrees;
- if the victim has lost consciousness, then turn his head to the side so that he does not choke on saliva, and if he vomits, he does not choke on vomit;
- unfasten belts, buttons, collars to increase oxygen access;
- If possible, measure your blood pressure: if it is high, give medicine to lower it;
- To ensure the outflow of blood from the brain, apply a heating pad to the patient’s feet.
Do not give the victim food, drink or drugs that dilate blood vessels. There is no need to try to deliver the patient to a medical facility on your own: to transport him, you need an ambulance with special medical equipment in order to begin measures to stabilize the patient’s condition even at the pre-hospital stage.
Diagnostics
If a stroke affects the brain stem, it immediately becomes noticeable due to characteristic signs. A specialist will be able to determine the deficiency of blood flow by conducting a series of standard neurological tests.
After examining the patient, the neurologist will issue a referral for general tests (blood test, cardiogram), as well as for computer (CT) and/or magnetic resonance imaging (MRI). Most often, these events are carried out bypassing the emergency department.
The use of MRI in the diagnosis of ischemic stroke is more effective than CT. This is explained by the fact that this device makes it possible to more carefully view longitudinal sections of the brain substance.
Spinal puncture, which involves taking fluid, is strictly contraindicated for this diagnosis. It can lead to the development of edema and provoke a shift in brain structures, which can lead to death. The use of hardware diagnostics helps to exclude other neurological diseases. For example, traumatic brain injury, tumor and alcoholic coma.
Contrast studies, such as angiography, are used to identify vascular formations - aneurysms, malformations. For example, atherosclerosis or thrombosis. Changes in heart rate, and therefore the intensity of blood flow, are detected using cardiography.
All these examinations will allow the specialist to obtain a complete picture of pathological changes. And based on the results, the degree of development of foci of tissue necrosis is determined and their adequate correction is carried out.
Treatment and rehabilitation
Treatment of stroke patients is a complex, lengthy process involving several stages. First of all, the patient is admitted to the intensive care unit, where doctors literally save his life.
Without fail, the patient undergoes a magnetic resonance or computed tomography to identify the location of areas of damage and their size, an ECG, and a blood test.
Next, the patient is transferred to a 24-hour neurological department of the hospital, where the therapeutic process is reduced to restoring damaged cells and parts of the brain and enhancing their nutrition. For this, Ceraxon, Piracetam, Thiocetam, Cavinton, Neurobion, Cortexin are prescribed. To eliminate cerebral edema, Furosemide, Mannitol, and L-lysine are used.
Monitoring of blood pressure, blood counts, and body temperature is mandatory. To normalize high blood pressure, the drugs Enap, Magnesium sulfate, Metoprolol, Captopril are used, and for low blood pressure - Atropine, Dexamethasone. Paracetamol and Ibuprofen are used to reduce body temperature.
There is a fundamental difference in the prescription of drugs, depending on the type of stroke. In case of ischemic injury, thrombolytics (Actilyse) or anticoagulants (Heparin, Clexane) are required; in case of hemorrhagic stroke, hemostatic agents are required.
If the patient is unable to swallow, nutrients are administered through a tube.
A very important stage is the rehabilitation period after discharge from a medical institution. Dead brain cells are no longer able to recover, so rehabilitation measures are simply necessary in order to make the patient’s life easier and teach him lost skills using the neurons that remain unharmed.
An individual recovery plan is created by the attending physician for each individual patient.
It includes:
- Physiotherapeutic methods (magnetic therapy, laser therapy) aimed at improving blood circulation and restoring brain functions.
- Occupational therapy is a set of activities designed to teach patients simple household skills and restore fine motor skills (open a door, type on a keyboard, hold cutlery).
- Classes with a speech therapist to restore speech functions.
- Therapeutic exercise and massage techniques to prevent muscle fiber atrophy and strengthen muscles.
- Psychotherapeutic consultations to help the patient recover from shock after an attack.
Relatives and loved ones play a huge role in the patient’s recovery, since patients need round-the-clock care and moral support. The patient’s immediate circle needs to be prepared for the fact that recovery may take a long time, and the results may differ from those expected.
Classification
There are two types of such stroke: ischemic and hemorrhagic.
Ischemic
This is the most dangerous type of brain stem stroke. It most often becomes the cause of death of the patient (in second place among the causes of death). Ischemic stroke is also known as “cerebral infarction”. It develops due to the formation of a blood clot in a vessel in the brain stem.
It causes extensive damage to brain tissue , because ischemia disrupts the normal flow of blood and its formation.
Nutrients cannot reach parts of the brain, which causes tissue necrosis in the affected area. Typically, this type of stroke occurs due to advanced atherosclerosis. In addition, diabetes, rheumatism and hypertension may be the cause. Ischemic stroke can “not show up” for quite a long time and is characterized by slow development. If a person experiences weakness, there is a lack of coordination, and dizziness is accompanied by nausea, then this is the first sign of the development of ischemia.
There are the following stages of ischemic brainstem stroke:
- The acute period lasts up to 3 weeks. Cell death occurs within 3-5 days. Perifocal edema develops (fluid accumulation in the intercellular space of the brain due to the expansion of this space), and the cytoplasm and karyoplasm of cells shrink.
- The early recovery period lasts up to 6 months. Paranecrosis (protective reaction to damage) of cellular elements, proliferation (growth) of small vessels occurs. There is regression of neurological deficit (consequences of stroke in the form of impaired motor function, etc.).
- The late recovery period lasts from 6 to 12 months. The development of glial scars (replacement of areas of necrosis with connective tissue) and cystic defects of brain tissue occurs.
- The last stage begins after a year. Residual effects occur and consequences appear.
There are also several degrees of severity:
- Average. There are no clinical signs of cerebral edema and no disturbances of consciousness. The clinical picture is of local lesions.
- Heavy. It is characterized by depression of consciousness, signs of tissue swelling, trophic and vegetative gross focal symptoms are noticeable.
If you notice an ischemic stroke in time and recognize it at an early stage, then there is a chance to prevent the disease.
Hemorrhagic
When such a lesion occurs in the brain stem, the symptoms are characterized by immediate manifestation .
It appears due to increased permeability of the vascular walls and damage to the walls. It causes blood cells to leak into the brain tissue: red blood cells, plasma, leukocytes and platelets. Divided into subspecies:
- Subarachnoid . It differs in that the blood penetrates the soft meninges.
- Parenchymatous . Brain tissue comes into contact with blood due to its penetration through the walls of blood vessels.
- Epidural and subdural . Blood enters the cavity between the skull and the lining of the blood vessels. These two subtypes are more common due to injury.
To save a person, immediate assistance from surgeons is required to eliminate the hematoma and bleeding . In addition to the open method (craniotomy during surgery), there is also an invasive method (elimination of the hematoma through a small hole in the skull using special medications and instruments). The latter type of operation is possible only for hemorrhagic hemorrhage due to hypertension. It is contraindicated for aneurysm and vascular pathologies.
Possible consequences
More than half of stroke cases end in the death of the victim; in other cases, the patient is doomed to disability.
Subsequently, after a stroke, the following complications may occur:
- slurred, incoherent speech if the speech center in the brain is affected;
- loss of ability to swallow food;
- paralysis of the limbs, inability to walk, sit, or chaotic involuntary movements of the arms and legs;
- pneumonia;
- vein thrombosis;
- internal bleeding;
- myocardial infarction;
- bedsores in bedridden patients;
- mental disorders.
The occurrence of a repeated episode of stroke is especially dangerous; the patient’s body will no longer cope with such a load, and the result will be death.
Rehabilitation period
Is recovery possible after a brain stem stroke? A person can partially recover, but even if the changes in the brain are small, it is not possible to fully restore the lost functions.
The patient must undergo a course of rehabilitation procedures. Physical therapy exercises significantly speed up the recovery process. At first, classes are conducted in a lying position. They are designed to normalize the motor activity of the legs and arms.
Next, special gymnastics are prescribed to develop facial expressions and exercises to rehabilitate speech function. The patient is also recommended to have a massage, undergo sessions of manual therapy, reflexology, and hirudotherapy.
Patients who have impaired swallowing or breathing, as well as patients in a coma, require longer rehabilitation. Recovery takes about 2 years, and many functions cannot be normalized at all.
Recovery prognosis
Statistics show that approximately 80% of brainstem stroke survivors die within 3 days after the attack. For the remaining 20%, the prognosis is disappointing: they become severely disabled, some of them are forever bedridden.
About 18% of patients are able to live more than 5 years; it was possible to fully recover and recover for only 2-3%.
The prognosis for recovery depends on the symptoms of the stroke and is considered unfavorable if the patient has deterioration in motor and speech abilities, breathing problems, heart failure, and inability to thermoregulate.
Doctors’ prognosis is also influenced by the patient’s physical condition and the presence of concomitant pathologies before the attack and his age: the younger and healthier he is, the greater the chance of a full recovery; it is much more difficult for an elderly person to cope with the consequences of the disease.
Author of the article: Yulia Dmitrieva (Sych) - In 2014, she graduated with honors from Saratov State Medical University named after V. I. Razumovsky. Currently working as a cardiologist at the 8th City Clinical Hospital in the 1st clinic.
Prevention measures
The main methods of preventing stroke include:
- Treatment of existing chronic diseases.
- Normalization of weight.
- Quitting alcohol and smoking.
- Sufficient physical activity.
- Drug correction of blood pressure and dyslipidemia.
- Low cholesterol diet.
At the first signs of an acute cerebral circulatory disorder, it is necessary to call an ambulance and hospitalize the patient in the neurological department. Early diagnosis and timely treatment for brainstem stroke contributes to a favorable prognosis and recovery. The rehabilitation period is also important for recovery. If it is carried out adequately, life after a brain stem stroke will be full and long.
content