Angioplasty technique
The angioplasty procedure involves passing a guidewire through a puncture in the patient's skin to the site of the stenosis, through which a catheter with a tiny balloon at the end is inserted.
Under pressure, the balloon inflates and “crushes” the atherosclerotic plaque.
Most often, this procedure uses access to stenotic vessels through the femoral artery in the groin area. This technique is technically simpler than through the radial artery at the wrist (radial approach). However, with radial access there is virtually no postoperative period and the patient can immediately lead an active lifestyle.
Currently, angioplasty with stenting is widely used. For this procedure, balloon catheters with a circular metal mesh, a stent, located around the balloon are used. The stent is in a collapsed state and when the balloon is inflated, it expands in the narrowed area. The lumen expands and blood flow is restored. The stent remains in the vessel as a supporting frame. The catheter is removed.
The procedure is carried out under constant X-ray monitoring, after the introduction of an X-ray contrast agent, which makes the vessel visible.
The intervention is performed by an x-ray endovascular surgeon in the cath lab.
The angioplasty procedure is painless and lasts from 1 to 3 hours.
Video: angioplasty with stenting - medical animation
Technique of the operation
Transluminal balloon angioplasty is considered a minimally invasive procedure and is therefore performed in a catheterization operating room. To perform it, general anesthesia is not required - the surgeon independently numbs the puncture point of the vessel with a local anesthetic. Despite this, an anesthesiologist is always present in the operating room in order to provide timely assistance to the patient in the event of an emergency.
The patient is placed on the operating table in a “supine” position. Next comes the connection of devices that measure blood pressure, blood oxygen saturation, and the patient’s pulse rate. The next stage will be puncture and catheterization of the peripheral vein to administer the necessary medications and infusion of solutions. The surgeon treats the skin at the puncture site with antiseptics and then covers it with sterile surgical linen. When the surgical field is prepared, the doctor administers local anesthesia.
Initially, the surgeon punctures the vessel and installs a guidewire into its lumen. Then the puncture needle is removed, and a balloon catheter is inserted through a soft guidewire. Controlling the progress of the catheter using x-rays, the surgeon guides it along the vessel to the place where the area of stenosis is supposed to be located. Once the target is reached, a contrast agent is injected into the bloodstream and an image is taken.
Once the site of stenosis is verified, the balloon catheter is advanced to it under X-ray guidance. Having reached the intended goal, the surgeon inflates and quickly deflates the cuff of the balloon. This achieves a vasodilation effect. There is a stent inside the balloon. It is a soft metal mesh folded in the shape of a tube. After inflating the cuff, the stent opens, tightly adjacent to the vascular wall. The device keeps the vascular lumen open and does not allow it to re-stenose.
After stent placement, the surgeon takes a control image to assess its position as well as the degree of revascularization. If the result is satisfactory, the balloon catheter is removed from the vascular lumen. A sterile pressure bandage is applied to the puncture site. The patient is transported on a gurney to the recovery room.
Laser angioplasty is performed using the same algorithm. Its difference is that fatty plaques are completely destroyed by laser. The expansion device is not installed.
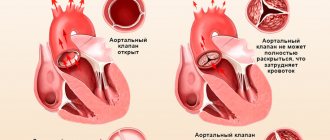
Coronary angioplasty of heart vessels
To restore blood circulation in the vasculature supplying the heart muscle, angioplasty of the coronary arteries (coronary angioplasty) is performed. This is an effective method of helping patients with coronary artery disease, especially complicated by a heart attack.
Coronary myocardial revascularization using stents significantly improves outcomes after stenosis or obstruction of the coronary arteries. When performing TLBAP, the dilatation device is most often installed in the LAD (anterior interventricular branch of the coronary artery that supplies blood to the heart). For this purpose, a standard balloon catheter for coronary angioplasty is used.
After surgery, patients are prescribed medications that improve blood flow and reduce the risk of blood clots. Transluminal balloon coronary angioplasty (TBCA) is considered successful if, after a control assessment of the result, the residual narrowing of the vascular lumen is no more than 18-20%. We can also speak of success when the patient, after recovery, notes a regression of symptoms indicating ischemia.
Indications for angioplasty
The most common application of angioplasty is for stenosing atherosclerosis of the heart vessels (coronary angioplasty); leg vessels; vessels involved in the blood supply to the brain and head tissues; renal artery stenosis.
Methods for detecting stenosing vascular atherosclerosis
- Duplex ultrasound examination of blood vessels
- CT scan
- Magnetic resonance imaging
If stenosing atherosclerosis is detected, angiography may be prescribed in some cases. When performing an angiography, it is possible to simultaneously perform an angioplasty procedure.
When is the choice made in favor of surgical treatment?
The choice in favor of surgical treatment of vessel narrowing is made when severe stenosis is detected, in which the diameter of the vessel decreases by more than 50% (hemodynamically significant stenosis). With such stenosis, oxygen starvation of tissues (ischemia) develops due to a pronounced decrease in blood flow.
Clinical manifestations of ischemia depend on the affected vessel:
- Coronary heart disease – with damage to the coronary arteries
- Pain in the calf muscles, ulcers and gangrene of the lower extremities - in case of atherosclerotic changes in the vessels of the legs
- Transient ischemic attacks, short-term loss of consciousness - with narrowing of the carotid arteries
- Increased blood pressure – with renal artery stenosis.
Indications and contraindications for use
Having recently become the most popular and effective treatment for myocardial infarction, being the best alternative to bypass surgery and drug therapy, its use is still limited by a number of strict indications.
This:
- Asymptomatic ischemia. This group includes patients with one or two affected coronary arteries and instrumentally and laboratory-confirmed ischemia of the heart muscle.
Attention! The asymptomatic course of myocardial ischemia and myocardial infarction, in particular, is most typical for patients with diabetes mellitus.
- Unstable angina or stable moderate angina. Stable angina, the symptoms of which classify it as class II-IV in severity, or unstable angina require not only angiography, but also angioplasty.
- STEMI. Myocardial infarction with ST segment elevation above the baseline is a “red flag” that requires urgent treatment, the most effective of which is cardiac angioplasty. In this case, the individual characteristics of both the patient himself and his condition at the time of the infarction and the extent of necrosis play an important role in the choice of this method.
- Previous bypass surgery. Patients with a history of early bypass surgery who present to the hospital with symptoms of angina pectoris should be considered candidates for angioplasty.
Theoretically, repeat bypass surgery is possible, but it carries a high risk of adverse complications.
For chest pain, consultation with a cardiologist is required.
Contraindications for angioplasty
The main situations in which this type of therapy for myocardial ischemia is not used are the following:
- occlusion of a vessel whose diameter is reduced by less than 50% of the proper lumen;
- stenosis of the main trunk of the left coronary artery;
- clinically significant occlusion of three or more coronary arteries.
The last two factors are indications for referring the patient to open surgery - bypass surgery.
Other contraindications include certain health conditions of the patient, such as impaired blood clotting, congestive heart failure in the decompensation stage, renal failure, acute cerebrovascular accident, etc.
Coronary angioplasty
Coronary angioplasty is used to restore the patency of the coronary arteries and normal functioning of the heart, both in angina pectoris and in acute myocardial infarction.
The advent of stents has increased the number of patients who can undergo percutaneous coronary intervention. With the use of stents and modern drug therapy, rates of successful coronary angioplasty reach 90-95%.
We can speak of a successful angioplasty procedure if, according to angiography after the intervention, the residual stenosis in the affected vessel was 20% and blood flow in the artery was completely restored, the procedure was completed without serious complications, and the signs and symptoms of ischemia decreased after the patient recovered from the operation.
Complications of percutaneous coronary interventions
Serious complications are rare and are most often observed when patients are admitted in the acute period of myocardial infarction, in serious condition with cardiogenic shock, with multiple lesions of the coronary vessels and significant changes in the heart muscle, severe atherosclerosis of the peripheral arteries.
Minor complications include transient ischemic attack, access site complications, renal failure, and adverse reaction to contrast media.
Restenosis – what is it?
restenosis
After angioplasty, between the third and sixth months, a repeated narrowing of the vessel in the same place may occur - restenosis.
Restenosis is not considered a complication of angioplasty, but rather a response of the vascular wall to endovascular intervention.
A few words about stents
When performing coronary angioplasty, the following are used:
- Simple metal (without drug coating) stents;
- Drug-eluting stents are stents coated with a special polymer on the stent wall in contact with the vessel and releasing a dosed drug that prevents the development of restenosis;
- Bioabsorbable (self-absorbable) stents - when installed, they expand the lumen of the artery, and within three months they release a drug that prevents the process of restenosis. And after two years, bioabsorbable stents dissolve.
Each type of stent is selected individually, according to indications, taking into account the wishes of the patient and in accordance with all the features of the course of the disease.
With the advent of drug-eluting stents, the incidence of restonosis after coronary angioplasty is less than 10%.
Laser angioplasty is a technique used when it is technically impossible to perform balloon angioplasty.
The use of a laser has its own indications: in cases of severe calcification of atherosclerotic plaques, extended and located at the mouths of coronary vessels, as well as plaques that completely cover the lumen of the vessel. The principle of the technique is the same as balloon angioplasty, but a laser sensor is used rather than a catheter with a balloon. The laser hits the plaque with high temperature and the plaque evaporates. After this, a stent is inserted into the vessel.
Patient management after the procedure
Thanks to the recently widespread special devices that close the puncture in the artery, removal of the conductor sheath installed at the arterial access site is possible immediately after the end of the manipulation. After this, the patient remains in bed for an average of 18 to 24 hours without complications.
Percutaneous angioplasty is usually performed simultaneously by two cardiologists.
If a glycoprotein IIb/IIIa blocker was administered to the patient during the procedure, it continues to be given for another 18 hours after the end of the angioplasty.
Aspirin and Clopidogrel are also given to the patient after surgery, and the duration of treatment and dosage of the latter varies depending on the type of stent used. So, when installing a metal stent, taking Clopidogrel continues for up to 2-4 weeks, and if a drug-coated stent was installed, taking this drug is extended for a period of 3 to 6 months.
Important! The absence of symptoms of myocardial ischemia is expected immediately after stent placement.
Carotid angioplasty
Angioplasty with stenting of the carotid arteries is one of the most promising and complex areas in endovascular surgery to restore blood supply to the brain.
Surgery of the carotid arteries is indicated when the carotid arteries are narrowed by 60% or more in the presence of symptoms such as transient ischemic attacks, syncope, or a previous stroke. If the carotid arteries are narrowed by more than 70%, even in the absence of obvious symptoms, surgical treatment is indicated.
angioplasty of the carotid arteries with stenting
The choice of surgical treatment - open surgical treatment (endarterectomy) or angioplasty with stenting - is of paramount importance, as in patients with symptoms of the disease. as well as in “asymptomatic” patients.
A limiting factor for angioplasty with carotid artery stenting is the high risk of possible cerebral embolism during surgery. The invention of special occlusion balloons and filters located distal to the surgical site significantly reduces the incidence of embolism and stroke.
Currently, clear recommendations have been developed for the choice of surgical treatment method depending on the degree of stenosis, location and structure of the atherosclerotic plaque, as well as concomitant pathology.
Transluminal balloon angioplasty in patients with various forms of coronary artery disease (literature review).
Introduction: Coronary heart disease still occupies a leading position in the structure of morbidity and mortality in the population of developed industrial countries, despite the impressive successes achieved over the past decade in the prevention and treatment of coronary artery disease. IHD, as is known, is based on stenotic atherosclerosis of the coronary arteries, which occurs in approximately 98% of patients. In this regard, one of the promising areas of treatment for coronary artery disease is reperfusion therapy. Restoring blood flow through the heart artery affected by atherosclerosis is the ultimate goal of 3 principal directions of reperfusion therapy: systemic thrombolysis, coronary angioplasty and CABG. Restoration of blood flow in a syndrome-related artery using coronary angioplasty is achieved without surgical trauma and quickly, as with thrombolysis, and at the same time fully, as with surgical revascularization (Spencer B. King, 1996). Coronary angioplasty is a method that allows you to combine the positive aspects of other treatment methods. It increasingly acts as a method of choice in the treatment of patients with acute forms of coronary artery disease and is more economically profitable (Grinmes S. et al., 1996; Zjilstra F., 1995). Current state of the problem of transluminal balloon angioplasty in patients with different forms of coronary artery disease One of the effective and most frequently used methods of endovascular myocardial revascularization in interventional cardiology is currently transluminal balloon coronary angioplasty. The method was developed and introduced into clinical practice by A. Gruentzig in 1977. Initially, TLAP was used in patients with chronic stable angina, then it increasingly began to be used for unstable angina and in the acute period of myocardial infarction (Ioseliani D.G., 1982, 1992; O. Kamp 1989). The technical success of coronary angioplasty for unstable angina does not differ from that in the treatment of patients with stable angina, however, the incidence of severe complications increases significantly (Holmes DR, 1985; Bentvoglio LG, 1991). The effectiveness of PTPA in AMI remains controversial. A number of authors (Ioseliani D.G., 1993, 1995, Dzhorgova-Lu, 1995) consider the method of direct myocardial revascularization in the acute stage of myocardial infarction to be effective, other researchers (Topol E., 1980; Rainzer AE, 1985) do not find positive results . There are even reports (Reimer KA, 1981) that this procedure may have an adverse effect on the course of AMI due to the expansion of the necrosis zone. Traditionally, it was believed that PTPA was primarily indicated for patients with isolated lesions of the proximal or middle segments of one (less often two) branches of the coronary artery of the heart (Ioseliani D.G., 1993; Yambe T., 1991). However, constant technical improvement has made it possible to perform PTPA in patients with damage to several segments of all 3 main arteries. Currently, the indication for PTPA is myocardial ischemia associated with coronary artery stenosis. Any patient with symptoms of angina pectoris and objective confirmation of severe myocardial ischemia, without any special age restrictions, can be a candidate for balloon angioplasty (Echo Ya.E. et al., 1984; Cheng GS et al, 1993; Joel K. Kahn 1993). Factors influencing the long-term survival of patients after balloon angioplasty of the coronary arteries. When assessing the effectiveness of PTLA in the long term, it is traditional to use several criteria: survival, absence of angina attacks, prevention of AMI and the need for additional procedures. Most foreign researchers (Joel K. Kahn, 1990; Gregg W. Ston, 1995; Kotaro Sumii, 1993) have found that TLAP has a beneficial effect on long-term survival of patients, noting a high survival rate: 95%, 87% and 82% after 1 year, 4 years, and 7 years, respectively, compared with 80%, 69%, and 65% survival rates for unsuccessful PLAT. The question of the effect of the number of affected arteries on long-term survival remains controversial. Long-term survival in patients with multivessel coronary disease is lower than in patients with single-vessel coronary disease. (K. Detre et al., Toraxcenter, 1986). No significant difference was found in the survival of patients after PTAP performed for various forms of coronary artery disease: stable and unstable angina, AMI. (Toraxcenter 1986; SM Scott et al., 1994; O. Kamr et al., 1989; M. Naqui Sabri, 1992 ; David W. M. Muller, 1990). In patients with multiple lesions of the coronary arteries, balloon angioplasty is a more labor-intensive and time-consuming procedure, and they also have a greater likelihood of restenosis and reocclusion. According to a number of authors (Ioseliani D.G et al., 1997), when planning angioplasty in patients with multiple lesions of the coronary vessels, it is necessary to identify the stenoses responsible for the occurrence of angina symptoms, and they should be dilated first. It is also necessary to identify vessels whose role in the occurrence of ischemia and angina symptoms is insignificant and, accordingly, the dilatation of which will not play a significant role in this patient. Determining the sequence of vascular dilatation and the possibility of step-by-step PTAP is also of great importance. Table No. 1 presents summary indicators of long-term survival of patients after successful transluminal balloon angioplasty. Analysis of the literature showed a significant dependence of long-term survival on the state of LV contractile function. As can be seen from the data below, more favorable survival rates are observed in the group of patients with LV FEV * 50%. T. Sterens (1991) studied long-term survival when performing PTPA in patients with LV dysfunction (LV FEV < 40% according to VH). At 1 and 4 years, long-term survival was 87% and 69%, respectively. Hochbert Y. et al. (1996) compared long-term survival of patients with LV FEV * 20% and with LV FEV * 20%. After 3 years it was 60% and 15%, respectively. A group of researchers from the Toraxcenter (1986) published a paper presenting data on the overall survival of patients after LTAP depending on the functional state of the LV. After 5 and 10 years, it was 91% and 80%, respectively, for patients with LV FEV * 50%, and 79% and 57% for patients with LV FEV * 50% (p * 0.0005). Many authors emphasize that mortality during angioplasty is lower than with drug treatment in patients of comparable severity. E. Berger (1992) compared mortality in PTAP after 18 months. and it was 1%, with CABG - 4% and with conservative treatment - 6% after 27 months. A less significant difference in mortality rates between LTAP and CABG was observed in studies by T. Hamaguchi et al. (1995). After 3 years it was 3% and 5%, respectively. High long-term mortality was observed in the CASS studies, where the 15-year mortality rate after CABG was 22%, and with conservative treatment - 15%. Thus, the success of the procedure and long-term results of myocardial revascularization are influenced by the nature of the lesion of the coronary artery undergoing PTPA, the functional state of the myocardium and the chosen treatment method. Transluminal balloon angioplasty is currently the safest method of treating coronary artery disease, as it has lower long-term mortality compared to CABG and conservative treatment. Various aspects of the quality of life of patients in the long-term period after balloon angioplasty. Of particular interest are studies that examine the problems of angina pectoris and the development of non-fatal AMI in or outside the dilated artery in patients undergoing PTAP. Although balloon angioplasty helps open the vessel and preserve LV function, it remains controversial whether it leads to a more favorable clinical course of the disease compared with other treatment methods. Quality of life means a person’s satisfaction with his physical, mental and social well-being (Gladkov A.P. et al., 1982, Levy L., Anderson A. 1979, G.F. Mukhamedzhanova et al., 1996). One of the constituent aspects of quality of life is the clinical condition (survival, absence of angina episodes, increased exercise tolerance) of the patient in the long-term period after PTAP. Most of the authors (Babunashvili V.M., Rabkin I.Kh., Ivanov V.I. 1996; Saakyan Yu.M., 1996; J. D. Talley et al., 1988; Toraxcenter, 1986; M. G Bouzassa, 1998) believe that the return of angina in the long-term period depends on the degree of myocardial revascularization, but does not depend on the clinical form of coronary artery disease for which PTAP was performed. A. Rodrigues et al. 1995, W. Weintraub et al. 1995 revealed the dependence of the return of angina on the method of treatment of coronary artery disease. Patients undergoing LTPA have a higher incidence of recurrent angina than patients undergoing CABG. And here it should be taken into account that angioplasty can be repeated until angiographic and clinical success is achieved without a time limit, which cannot be said about CABG. And the results obtained after repeated TLAP are much better. The risk of developing recurrent AMI in the long-term period after PTAP is higher in patients with multivessel coronary lesions and incomplete myocardial revascularization (Detre et al., 1988; Brien O. Murchu, 1993; Saakyan Yu.M., 1996; Toraxcenter, 1986). Condition of the coronary bed and dilated vessel in the long term after PTAP. To date, there is no clear definition of restenosis after LTAP. Various diagnostic criteria for restenosis have been proposed, in particular, such as: 1) a decrease in diameter by 30% or more compared to its diameter achieved with TLAP; 2) the presence of stenosis of at least 70% with stenosis immediately after PTLA of less than 50%; 3) an increase in the severity of stenosis by more than 10% compared to the diameter of the stenosis before PTLA; 4) a decrease of 50% or more in the diameter of the lumen of the vessel from that achieved with TLAP; 5) reduction in the diameter of stenosis (less than 50% after TLAP) to 50% or more; 6) a decrease in the minimum diameter of the vessel lumen by 0.7 mm compared to the lumen achieved with angioplasty (A.A. Alekseevsky, D.V. Drozdov, A.L. Syrkin, A.E. Moreyra, A. Wajnberg, 1994). The frequency of restenosis, according to numerous researchers, performed in various institutions in many countries, ranges from 17-40%. As a rule, restenosis developed within 1–6 months. after successful TLAP. In earlier periods, the resumption of coronary insufficiency is often caused by thrombosis of the dilated area, and the appearance of angina pectoris after more than 6 months. Usually, damage to intact or slightly stenotic areas of the artery at the time of LPAP is determined. It is noteworthy that in approximately 1/3 of cases, restenosis occurs without adequate clinical symptoms. According to R. Hernander et al., out of 277 patients with restenosis in a period of 6 to 9 months. in 48%, restenosis was not accompanied by clinical symptoms of angina. At the same time, in 30−50% of patients, angina pectoris is not caused by the development of restenosis. These observations indicate that it is insufficient to take into account only the anginal syndrome for monitoring the patient after PTAP. The pathophysiological mechanisms of restenosis are currently not well understood. The main morphological substrate of restenosis is fibromuscular intimal hyperplasia (Waller Bf et al. 1987, Glagov S. 1994.,). The formation of thrombotic layers also plays a certain role. Coronary angiospasm also accelerates fibromuscular hyperplasia. According to R. Schwartz et al. (1996) the formation of a blood clot on the surface of the plaque plays the role of a kind of matrix that facilitates the proliferation of smooth muscle cells. Each of the described processes takes a certain time, thus, true restenosis can form only by the end of 1 month or later after PTAP. The literature considers a number of factors that increase the risk of restenosis. Clinical, morphological and “technical” factors can be distinguished. The incidence of restenosis is influenced by the clinical course and nature of coronary artery disease, and the presence of aggravating risk factors. The morphological (angiographic) characteristics of stenosis are significant: localization, extent, severity, multiplicity of lesions. “Technical” factors include all the characteristic features of the TLAP procedure itself and its immediate results (Leimgruber PP et al. 1985, Bourassa MG et al. 1990,1991, Hermans WR et al., 1992). The purpose of many studies (Tohma H., 1991, Terres W. 1992, Garlek-A 1995) was to study the angiographic and anatomical state of the coronary bed in the long term after endovascular treatment procedures. They determined the influence of such factors as smoking, diabetes, hypertension, dyslipopreidemia, the volume of coronary lesions (damage to one, two or three vessels) on restenosis and reocclusion of dilated vessels. A number of publications report repeat angioplasty for restenosis, and the authors consider this tactic to be natural and justified, considering restenosis an inevitable consequence in a certain percentage of cases (B. Meier et al., 1984, Williams DO et al., 1984, O. Keefe et al., 1984). al., 1989). A number of authors (R. Muler, 1982, G. Austin, 1987, E. Fleck, 1988, Cregg J. Reis, 1991, Gurlek-A, 1995) believe that patients with hyperlipidemia, multivessel disease, hypertension have a higher risk of developing restenosis. It was noted that gender, smoking, and previous myocardial infarctions do not affect the process of restenosis. Other authors (Terres W., 1992), on the contrary, highlight female gender, older age, and patients with diabetes mellitus at risk of late complications and believe that smoking and hypercholesterolemia do not affect the further course of the disease. Most authors, Simonton CA1988; Starc C., 1988; Hiasa Y., 1994; O. Kamp et al. 1989; Inigues A., 1994., did not reveal the influence of clinical forms of coronary artery disease on the development of restenosis in the long-term period after PTAP. According to the observations of Ioseliani D.G. et al., (1997), L. Mata (1985), P. P. Leimbrube et al. (1986), Sinisa M. Ketik (1995), Stone GM (1996) showed a more likely occurrence of reocclusion with damage to the LAD LCA with simultaneous dysfunction of the corresponding area of the LV, leading to low blood flow in the dilated vessel after PTAP. These patients are prone to developing thrombosis and restenosis. The influence of factors such as inflation pressure, inflation time, and number of balloon inflations on the incidence of restenosis remains poorly understood. B. Meier et al. (1984) noted a high rate of immediate success with the use of high balloon pressure at the time of dilatation. However, the reduction in restenosis rates was not statistically significant. Meier B. 1989, Hermans WR 1992, Banka VS et al. 1993 They suggest using prolonged inflation with a gradual increase in pressure in the balloon. In their opinion, this promotes gradual remodeling of the vessel without deep damage to its wall and leads to a decrease in the incidence of restenosis. R. Uebis 1989 compared the rate of restenosis in the group with a single dilation (14.7%) and in the group with a 3-fold dilation (34%). Rubin GS et al. (1987) reported that multiple balloon inflations had a high rate of restenosis (53%) compared with fewer balloon inflations (26%). CJ Botman (1989) found that choosing a larger balloon for repeat PTAP procedures reduced restenosis rates from 60% to 25%. Having studied the condition of the coronary bed in the long-term period after PTAP, the authors raised the question of repeated procedures that a patient needs after balloon angioplasty with the progression of atherosclerosis, the appearance of angina pectoris and the detection of restenosis or reocclusion on CAG. Almost all researchers (A. Rodrigues et al. 1995, JJ Goy et al. 1995, K. Detre et al. 1986, JD Talley 1988, E. Berger et al. 1986, G. Kober et al. 1989) , W. M. Muller 1990, H. Bonnier et al. 1989, P. Guiteras 1990) came to the conclusion that patients undergoing PTAP require repeated revascularization procedures in the long-term period. Thus, the development of restenosis and reocclusion in the long term after LTAP is an inevitable process in a certain percentage of cases, and additional procedures (repeat LTAP, stenting and CABG) are in some cases an integral part of treatment. The influence of many risk factors (age, gender, smoking, hypercholesterolemia, diabetes, hypertension, nature of the lesion, location of the lesion) on the development of restenosis remains controversial and has not been fully studied.
The effect of PTPA on the contractile function of the LV myocardium. LV contractile function is one of the most important predictors of the “quality” and life expectancy of patients with various forms of coronary artery disease (Sanz G. 1982, De Feyter PJ 1982, Kander NH 1989). Currently, the question remains open about the effect of balloon angioplasty on LV contractile function in patients with coronary artery disease. T. Linder et al. (1992) reported that PTPA performed in both stable and unstable angina normalizes reduced LV function. Since the contractile function of the LV changes dramatically during AMI, patients who underwent PTPA in the acute stage of myocardial infarction were subjected to the greatest study. The main mechanism by which thrombolytic therapy improves long-term survival is the preservation of LV function through early restoration and preservation of ICA patency (Stadius ML 1986, Sheehan FH1988, Feifenbrumm AJ1992, Brodie BR 1996). According to El Khatib Mohammed 1994, Ioseliani D.G. 1996, D. Rothbaum 1989, Fiefenbrumm AJ 1992, the earliest reperfusion of ischemic myocardium promotes maximum salvage of ischemic myocardium, reduced LV dilatation and lower mortality. At the same time, Voqt A. (1988) believes that only restoration of blood flow in full in the ICA leads to improved LV function and long-term survival. Particularly noteworthy is the fact that restenosis has virtually no negative effect on the clinical course of the disease and on the process of restoration of LV function (Savchenko A.P. 1991, Christophe Bauters 1995). A possible explanation may be the functional adaptation of the coronary blood supply system, which manages to be realized during the gradual restenosis of ICA. Sheehan FH 1988, Feifebrumm AJ 1992, Leunq WH 1992 It is believed that residual stenosis of ICA is accompanied by LV dilatation and interferes with the improvement of LV FEV. In this case, the degree of LV dilatation is determined by the degree of residual stenosis of the ICA at discharge from the hospital (Dalen JE 1986, Stadius ML1986). James H. O'Keefe (1992) believes that already at the hospital stage, the segmental ejection fraction in the infarction zone increases by 30% and increases most significantly in patients with an initial LV FEV < 40% (on average from 28% to 42%) . However, the question of the time frame for performing ICA reperfusion, within which this procedure can still be effective, remains controversial. It is believed that PTPA, performed even 48 hours after the onset of an anginal attack, improves clinical outcome, but does not improve LV function (Ellis SG 1989). S. Miketik et al. (1995) believes that successful restoration of optimal perfusion in the late period (2-8 weeks) in patients with persistent ischemia after AMI can improve LV FEV by improving the segmental function of the LV wall in the infarct zone, and not due to compensatory hyperkinesia of the non-infarct zone. Garot G. et al. (1996) notes a significant increase in LV FEV at the long-term stage after PTAP of ICA, 3-4 weeks after the development of AMI, and at the same time indicates the reverse development of the aneurysm if the open state of ICA persists. Ioseliani D.G. et al., (1997) showed that, regardless of the method of treatment (TLAP or conservative treatment), during a control examination after 12+1.4 months. LV function improved. However, a more significant improvement was observed in the group with successful reperfusion. The positive dynamics depended on the number of affected arteries: with a single-vessel lesion, LV FEV increased by 9.4 + 3.2%, and with a multi-vessel lesion by 5.5 + 2.4%. In the group with detected reocclusion and restenosis, LV FEV remained virtually unchanged. In a small percentage of cases (mainly in patients with unstable angina and recurrent AMI), a decrease in LV FEV was observed. Thus, from all of the above, we can conclude that questions about the effect of PTPA on the contractile function of the LV in patients with stable and unstable angina, as well as in acute myocardial infarction, remain controversial. The question of the timing of ICA reperfusion, when this procedure can still be effective, is also discussed.
Conclusions: Based on literature data, it has been established that PTPA of the coronary arteries is a highly effective, safest and most economical method of treating patients with various forms of coronary artery disease. According to modern researchers, there is conflicting information about the survival of patients after PTAP with single and multi-vessel lesions of the coronary arteries, with low and normal contractile function of the LV. Researchers have divergent opinions about the importance of risk factors for the development of restenosis in the long-term period after PTAP. The issue of the effectiveness of balloon angioplasty, its impact on various aspects of the quality of life of patients in the long-term period, the prevention of recurrent AMI, and the need for repeated procedures in the long-term period remains controversial. The issue of using PTPA in patients with multiple coronary lesions is being debated.
Bibliography. 1. Anderson HV Restenosis after coronary angioplasty. Dis Mon.1993; 39: 613−670. 2. Bates E. Bell DEGrill et. al. Long-Term outcome of women Compared with men after Succesfull Coronary angioplasty. Circulation. 1995; 91:2876−2881. 3. Bentivoglio LG, Holubkov R., Kelsey SF et al. Short and long term outcome of percutaneous transluminal coronary angioplasty in unstable versus stable angina pectoris a report of the 1985−1986 NHLBI PTCA registry. Cathet Cardiovasc Diag. 1991; 23: 227−38. 4. Berger, M. R. Bell et. al. Effect of restenosis after an Earlier Angioplasty at another coronary site on the Frequency of Restenosis after a subseguent coronary angioplasty. Am. J Cardiol 1992; 69:1086−1088. 5. H. Bonnier, P. Bronzwaer., R. Michels and M. El. Gamal. Long term follow up of 100 patients with left anterior descending artery lesions treated with Percutaneous Transluminal coronary angioplasty. European Heart Journal. 1989; 10: 49−51. 6. C. J. Botman., M. El. Gamal., F.El. Deeb. et. al. Percutaneous transluminal coronary angioplasty more than twice for the same coronary lesson. European Heart J.1989; 10: 112−116. 7. Bourassa MG, Feldman B., Brower RW Strategy for complete revascularization in patients with multivessel coronary disease. Am. J. Cardiology.1992; 70: 2:174−178. 8. Brodie BR Grines CL Ivanchoe R. Six-month clinical and angiographic follow up after direct angioplasty for acute myocardial infarction. Final results from Primary Angioplasty Registry. Circulation. 1994; 90(1). 9.Mc. Bride W., Lange RA, Hillis LD Restenosis after succesful coronary angioplasty. N.Engl. J. Med. 1988; 318:1734−7. 10. Dangoisse V., Guiteras P., David PR, Lesperanse J. et al. Reccurens of stenosis after succesful percutaneous transluminal coronary angioplasty. Circulation.1982; 66:2−331. 11. De Feyter PJCoronary angioplasty for unstable angina. Am Heart J 1989; 860. 12. De Feyter HJPTCA in patients with stable angina pectoris and multivessel disease: is incomplete revascularization acceptable? Clin. Cardiol.1992;15:317−322. 13. K. Detre., R. Holubkov, Sh. Kelsey et. al. One—year follow—up results of the 1985 -1986 National Heart, Lung and Blood Inst. PTCA Registry. N engl J Med. 1988; 318:265−270. 14. Galan KM, Deligonul U, Kern MJ, Chaitman BR et al. Incresed frequency of restenosis in patients continuing to smoke cigarettes after percutaneous transluminal coronary angioplasty.Am. J. Cardiol. 1988; 61: 260−263. 15. Gruintzig AR, King SB 3, Schlumpf M., Siegenthaler W. Long-term follow-up after PTCA: the early experience. // N Engl. J. Med.- 1987.-Vol.316.-P.1127−1132. 16. Guiteras V.P., Bourassa M.G., David R.R., Bonan R., Grepeau J. et al. Restenosis after succesful percutaneous transluminal coronary angioplasty. The Montreal Heart Institute experience. Am.J.Cardiol. 1987; 60: 50B –55B. 17. P. Guiteras., L. Tomas., C. Varas and et.al. Five years of angiographic and clinical coronary angioplasty. European Heart J. 1989; 10: 42−48. 18. Harts AG, Mabin TA, Holmes DR Mortality after PTCA and coronary bypass surgery. Am. J Cardiol 1992; 70:179−185. 19. Hiasa Y., Furinaga H., Wada T. Restenosis after successfull emergency coronary angioplasty for acute miocardial infarction Comparison with elective angioplasty. Int-J-Cardiol.1994; 47: 49−54. 20. Yolmes DR, Holubkov R., Vlietstra RE et al. Comparison of complications during PTCA from 1977 to 1981 and from 1985 to 1986. J. Am. Coll Cardiol. 1988; 12: 1149−1155. 21. Kadel C., Vallbracht C., Buss F., Kober G., Kaltenbach M. Long-term follow up after percutaneous transluminal coronary angioplasty in patients with single-vessel disease. Am. Heart J 1992; 124: 1159−69. 22. Kamp O., Beatt KJ, De Feyter P. Short, medium and long term follow up after PTCA for stable and unstable angina pectoris. Am. Heart J 1989:117: 1:991−996. 23. Kander NH, O Neil W, Topol EJ et al. Long-Term follow up of patients hearted with PTCA for acute myocardial infarction. Am. Heart J 1989; 118:2: 228−233. 24. Kent KM, Bentivoglio LG, Block PC, Bourassa MG et al. Long-term efficacy of PTCA: Report from the NHLBI PTCA Registry. Am. J. Cardiol. 1984; 53: 27C−31C. 25. Kohli RS, DiSciascio G, Cowley MJ, Nath A, King SB 3 et al. Coronary angioplasty in patients with seven very left ventricular dysfunctions. J Am/Cardiol.1990;16:807−811. 26. Leimgruber PP, Roubin GS, Hollman J, Cotsonis GA, Meier B et al. Restenosis after succesful coronary angioplasty in patients with single vessel disease. Circulations.1986; 73: 710−717. 27. Meyer J., Bocker B., Erbel R. et al. Treatment of unstable angina with PTCA. Circulation.1990; 60:3−160. 28. David W. M. Muller, Eric J. Topol, Barry S. George et. al. Two-year outcome after angiographically Documented Miocardial Reperfusion for Acute Coronary occlusion. Am. J Cardiol 1990; 60; 796−801. 29. Myler RK, Topol EJ, Shaw re, Stertzer SN et al. Multiple vessel coronary angioplasty: classification, results and patterns of restenosis in 494 consesutive patients. Cathet & Cardiovascular Diagn.1987;13:1−15. 30. RITA Trial Participants Coronary angioplasty versus coronary artery bypass surgery the Randomized Intervention Treatment of Angina (RITA) trial. Lancet 1993; 341:573−80. 31. Roubin GS, Douglas JS, King SB3 et al. Influence of balloon size on initial succes, acute complications and restenosis after PTCA. Circulation.1988; 78: 916−927. 32. Sabri, G. Di Siascio, M. J. Cowley et. al. Immediate and Long Term Result of Pelayed Recanalization of occluded Acute Miocardial infarction- Related arteries using Coronary angioplasty.Am.J. Cardiol. 1992; 69; 575−578. 33. Talley, JW Hurst, S. B, King 3 et. al. Clinical outcome 5 years after attempted PTCA in 427 patients. Circulation. 1988;77:4: 820. 34. Vandormael MG, Deligonul U, Kern MJ et al. Multilesion coronary angioplasty: Clinical and angiographic follow-up. J.Am.Coll Cardiol. 1987; 10: 246−252. 35. WSWeintraub., AS Kosinski Brown CL et al. Can restenosis after coronary angioplasty be predicted from clinical variables? J. Am. Coll Cardiol.1993; 21: 6−14.
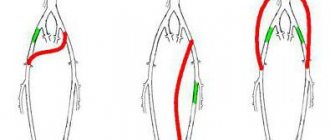
Angioplasty of vessels of the lower extremities
Angioplasty of vessels of the lower extremities is indicated for severe clinical manifestations of ischemia, as well as ulcerative-necrotic changes in the lower extremities. The choice of surgical intervention in favor of percutaneous intervention depends on the type of stenosis and its extent. There is a high immediate success of angioplasty - about 90%, with preservation of vessel patency after 5 years of observation of about 80%.
angioplasty of vessels of the lower extremities
Transluminal administration technique
The access site is usually the femoral artery. The length of the incision does not exceed 2 mm, through which the trocar is advanced along the vessel. Contrast is injected through this tube to visualize the area of narrowing. The location of the stenosis is revealed on the monitor, and a wire is applied to it to determine where it is best to destroy the plaque.
After this, the catheter passes to the desired area, and a saline solution is pumped into the balloon to restore the patency of the vessel and destroy the plaque. Then a control examination is carried out and the catheter and wire are removed. The final stage is the application of a bandage and observation throughout the day to prevent postoperative complications.
If percutaneous transluminal artery plasty is combined with the installation of a stent, then, when inflated with a balloon, this metal structure is straightened inside the lumen of the vessel. The stent can also be self-expanding, in which case there will be no balloon expansion stage. The stent material may be coated to prevent re-occlusion.
Angioplasty performed
The entire period of manipulation takes about 2 hours. At this time, there are unpleasant sensations associated with the expansion of the artery in the form of pain or burning in the chest.
Advantages of angioplasty compared to traditional surgery
- Minimal physical and mental trauma for the patient. The operation is performed without an incision, under local anesthesia and is practically painless.
- The time spent in the hospital is reduced to one to two days. The patient quickly returns to his normal lifestyle after discharge.
- High efficiency of endovascular interventions.
- The procedure can be performed on patients with severe illnesses when traditional surgery is not feasible.
- Contraindications are minor: severe allergy to contrast agents, bleeding disorders, acute renal failure.
- Lower cost compared to open surgeries.
What to do after angioplasty
After the operation, the patient is transferred to the ward and is monitored by ECG equipment for 24 hours. Medical personnel provide constant monitoring of the patient’s condition, the dynamics of blood counts and the puncture site.
To remove the contrast agent from the body, the patient must drink enough fluid.
After discharge from the hospital, any exercise is contraindicated. The patient must independently monitor the puncture. At the first signs of bleeding from the artery, you must clamp the bleeding area and urgently call an ambulance.
After surgery, the patient should be prescribed medications that prevent the formation of blood clots.
How to choose the right hospital for angioplasty?
The main requirement when choosing a medical institution is the number of percutaneous vascular interventions performed in the clinic and the presence of a specialized surgical department for possible extended vascular surgery if complications arise during angioplasty.
Clear recommendations have been developed for choosing a clinic for performing percutaneous interventions on the coronary vessels - at least 400 interventions per year, as well as the presence of a cardiac surgery department in the clinic.
Questions to ask your doctor
- Discuss in detail with your doctor the risks and benefits of percutaneous intervention compared to traditional surgery and drug therapy. It is important to be sure that you are consulting with a highly qualified specialist with extensive experience in percutaneous interventions. Since only the doctor makes decisions on all issues related to your treatment.
- Decide on the choice of stent. Drug-eluting stents are significantly more expensive than simple metal stents. Their advantage in reducing the number of restenoses after coronary angioplasty with stenting has been proven.
There is not a single study that has demonstrated the superiority of one type of stent over another (coated or conventional metal) in terms of reducing the number of neurological complications during angioplasty with carotid stenting.
It should be remembered that drug-eluting stents will require long-term use of serious antiplatelet therapy:
- Decide for yourself whether you can strictly follow all the recommendations for taking antiplatelet therapy and assess your financial capabilities;
- If you are planning any invasive procedures or surgery in the next 12 months that will require you to stop taking antiplatelet drugs due to the risk of bleeding, a standard metal stent should be implanted in preference.
This must be taken into account, since interruption of antiplatelet therapy after percutaneous intervention on the coronary arteries is an independent risk factor for the development of thrombosis - blockage of the stent with a blood clot.
If the doctor insists on using a stent that releases drugs due to the characteristics of atherosclerotic lesions of the vessel or concomitant diseases, then this must be heeded. However, the choice is yours.
Percutaneous intervention equipment
Although this method is minimally invasive, since there is no open surgical wound, it is carried out exclusively in special operating rooms. The following minimum set of diagnostic instruments and consumables is required:
- X-ray machine with a monitor to visualize the progress of the operation;
- balloon catheter - a tube of sufficient length to pass the affected vessel, at its end there is a balloon that is filled with saline solution for expansion;
- guidewire - a flexible wire that guides the catheter to the target;
- stent - a metal frame for placement in a narrowing zone, before insertion it is a compressed tube, it is inflated by a balloon to the desired size;
- trocar - a tube for inserting a catheter into an artery.
Life after stenting
It is important to remember that percutaneous intervention is about eliminating the consequences of the disease, not the disease itself.
In order to prevent the progression of atherosclerosis and the development of thrombosis:
- Strictly follow your doctor's recommendations for taking antiplatelet medications for the first 3 months to a year after stenting. The choice of antiplatelet treatment regimen is individual for each patient.
- Follow a lipid-lowering diet and take cholesterol-lowering medications to reduce low-density lipoprotein cholesterol below 100 mg/dL.
- Monitor your blood pressure regularly. It is recommended to achieve a reduction in blood pressure by changing lifestyle and prescribing individual drug treatment. Particular attention should be paid to limiting the consumption of table salt.
- Elimination of risk factors for the progression of atherosclerosis: reducing excess body weight by reducing calorie intake, quitting smoking and alcohol abuse, dosed physical training.
Risks of Angioplasty
- In very rare cases, it is still possible to have an allergic reaction to the X-ray contrast agent or local anesthesia.
- Sometimes the artery can be damaged by the guidewire, in which case urgent open surgery may be necessary.
- There is a risk of stroke.
- A hematoma may develop at the site of puncture of the vessel.
- Possible displacement of the atherosclerotic plaque.
Angioplasty, like any procedure, can have its complications. To obtain information about the essence of the process being performed and its possible unpleasant consequences, you should consult a doctor.
Cost of angioplasty with stenting procedure
The cost of the procedure will depend on which clinic and in which country the operation will be performed, the degree and complexity of the lesion and the specific artery, the number of stenotic vessels, and the technical features of the procedure. But the main component of the price is the cost of the stent.
The cost of an angioplasty procedure in Russia ranges from 80,000 rubles to 180,000 rubles. This includes manipulation, hospital stay, medications and nutrition. The cost of the stents themselves ranges from 40,000 to 130,000 rubles.
Coronary stenting for patients with acute myocardial infarction or unstable angina who are brought to the clinic by ambulance on an emergency basis is provided free of charge under the compulsory health insurance policy.
Angioplasty with stenting for coronary heart disease with stenosis of 1-3 coronary arteries is included in the basic compulsory health insurance program and can be provided free of charge.
Prognosis after treatment
Coronary angioplasty significantly increases blood flow through a previously narrowed or blocked coronary artery. In this case, chest pain (angina) should usually decrease, and the physical capabilities of the body, on the contrary, should increase.
You need to understand that angioplasty and stenting do not cure coronary heart disease, but only eliminate specific circulatory disorders of the heart muscle. To achieve a stable result, you must lead a healthy lifestyle and take medications prescribed by your doctor.
If the symptoms of angina return, then you need to contact your doctor again, and if you have chest pain at rest that does not respond to nitroglycerin, then call an ambulance.
After coronary angioplasty and stenting, the quality of life improves in 95% of patients, with many of them maintaining the effect for more than 5 years.
Patient reviews
Reviews from people who have undergone stenting are mostly positive and describe the sensations they experienced before, during and after the operation.
Many note the painlessness of the operation and a significant improvement in well-being almost immediately after the intervention. Everyone writes about the need to constantly take medications, see a doctor, and monitor certain blood clotting parameters.
Some people changed their lifestyle after the operation: they decided to quit smoking, lost excess weight, and began to lead an active lifestyle.
They also write that it is still necessary to decide on surgery in a timely manner, not to prolong the illness, and to have a positive attitude toward recovery. And also that the support of loved ones and relatives is important.
Preparation for angioplasty
- The attending physician must determine a list of medications that must be taken before surgery. Among them should be drugs that will prevent blood clots from forming during the procedure.
- We need to think about how to return home after the intervention.
- It is necessary to inform your doctor if you have kidney problems or allergies to foods containing iodine, such as seafood, or to radiocontrast agents.
- Before the procedure, you will need to sign a consent both for the angioplasty itself and for x-ray examination of blood vessels using a radiocontrast agent - angiography (coronography).
- You must not eat or drink for at least 4 hours before surgery.
- It is necessary to take preliminary blood tests, do an ECG and, according to indications, do other studies.
- On the eve of the operation, you should shave and wash the puncture area (groin, wrist or elbow area) to avoid infection.
How to prepare
Preparation for the operation is as follows:
- The patient undergoes a number of mandatory tests: ECG, general blood test, biochemical composition, ultrasound diagnostics and radiography. The preanalytical stage is important to confirm the extent of the pathological process and a clear location for determining the narrowing. Some clinics require consultation with an ophthalmologist and endocrinologist.
- Afterwards, the patient is admitted to the hospital, where the anamnesis is re-collected and the clinical picture of the disease is restored. Doctors repeat x-rays, but in several projections, to accurately determine the minimally invasive intervention.
- Angiography or duplex scanning of veins and arteries is prescribed. After receiving basic and auxiliary data on the patient’s condition, the day for the operation is scheduled.
- On the day of surgery, you should not eat for 2 days - you must stop taking medications and alcohol. If the patient cannot note taking medications, then he must inform the doctor about this fact.