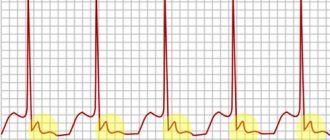
Heart and brain health are closely linked. Some heart diseases increase the risk of stroke. In turn, stroke is a risk factor for coronary heart disease.
In this article we will talk about how diseases of the cardiovascular system are associated with circulatory disorders in the brain, how you can reduce the risks, and what to do if your heart hurts after a stroke or other symptoms occur.
By the way, on our website there is a separate article about the relationship between high blood pressure and stroke.
Rehabilitation after craniotomy for stroke
A stroke is a serious disorder of cerebral circulation with rupture of a vessel, causing bleeding. This pathology leads to dangerous disorders of brain function, but the worst thing is the consequences of hemorrhage that forms a hematoma - possible disability and even death (if medical assistance was not provided within 6 hours).
Treatment with conservative methods is usually impossible, therefore, in order to help the patient and prevent the hematoma from enlarging, a decision is made to undergo surgery. In particular, if a person has a hemorrhagic stroke, then craniotomy is considered the only way to save him.
What are the indications?
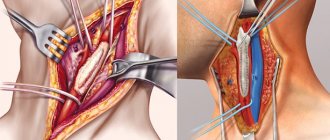
Craniotomy (French - trépanation, Latin - trepanatio) is an operation that involves opening the skull to provide access to hematomas in the brain area with their subsequent removal. Timely and correctly performed surgery reduces intracranial pressure. In 85%, the prognosis after trepanation is favorable.
Craniotomy is indicated for stroke in the following cases:
- infectious processes, inflammation in the brain;
- traumatic brain injuries;
- oncology;
- presence of blood clots;
- increased intracranial pressure;
- serious problems with blood vessels;
- the need to obtain brain tissue for biopsy.
Surgery for a cerebral stroke is performed by a neurosurgeon. Its success depends on the professionalism of the doctor and the availability of high-quality specialized equipment.
Preparation and stages of the operation
During the preoperative period, the patient is required to undergo a number of studies: chest x-ray, blood test, MRI, ECG. Also, the doctor should be aware of the patient’s allergies of various etiologies.
Non-steroidal anti-inflammatory drugs and blood thinners are not taken before surgery.
It is extremely important that at least 14 days before craniotomy, the patient completely gives up bad habits - smoking and alcohol.
What actions does the operation contain:
- Administration of anesthesia, insertion of lumbar drainage, removal of cerebrospinal fluid.
- An incision in the skin to gain access to the skull, scraping the skin from the bones of the skull. If this is not done, the remains of the dermis will fall into the open cranium.
- Treatment of the head with an antiseptic preparation along the hairline.
- Opening the skull: drilling several holes to gain access to the brain. The pieces of bone obtained by drilling are placed in a separate container - after the hematomas are removed, they are put in place.
- Removing blood stagnation, stitching together burst vessels, stopping bleeding. Screening monitors the patient's vital signs.
- Restoring the structure of the skull with missing parts.
- Completing the operation.
The surgical process takes 3-4 hours, but sometimes the operation can last up to 8 hours - it all depends on the stage of the pathology.
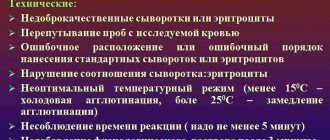
Risks of complications
Craniotomy is a complex operation that involves certain actions on the brain. It is impossible to guarantee a favorable outcome of a surgical intervention, since this is influenced by many factors: the individual characteristics of the body, the extent of the stroke, the patient’s age, and concomitant pathologies that occurred even before the operation.
The so-called risk group includes patients who have: diabetes mellitus, cardiovascular diseases, atherosclerotic formations, excessive accumulation of fatty deposits. Possible complications include general and surgical ones.
Experts include the second type of complications:
- infection of brain tissue;
- heavy internal bleeding or local hemorrhage;
- cerebral edema;
- mechanical trauma (damage to brain tissue, blood vessels with surgical instruments);
- epilepsy;
- paresis, paralysis;
- disorders of the central nervous system - memory impairment, absent-mindedness, slurred speech.
General complications, expressed in deterioration of health (vomiting, intestinal upset, critical weight loss, dizziness), develop after surgery, when the patient recovers from anesthesia and gradually returns to normal life. Patients who have had to undergo craniotomy, which is a serious operation, often experience a stressful state.
Who should not undergo surgery?
After an attack, a person needs a lot of time for rehabilitation. At this time, the body is still very weak, and surgery after a stroke doubles the load on it, which can lead to a relapse. For example, cataract removal should be carried out no earlier than six months after the end of a stroke; preference should be given to laser surgery rather than ultrasound.
Despite the effectiveness of craniotomy proven by medical practice, there are a number of contraindications that do not allow this operation to be performed. These include:
- hypertension;
- the time interval between heart attack and stroke is less than 6 months;
- congestive heart failure;
- progressive brain diseases;
- poor blood clotting;
- renal and liver failure;
- old age - after 70 years (not in all cases a reason for refusal to undergo surgery);
- malignant tumor;
- acute phase of inflammation accompanied by the formation of pus;
- neurological deficit.
Trepanation is prohibited if the patient is in a coma.
Rehabilitation
After the operation, trepanned patients are transferred to intensive care, where medical personnel monitor the functions of vital organs.
Particular importance is attached to the condition of the discharge through the drainage and the holes of the resection trepanation.
The appearance of a postoperative hematoma and increased cerebral edema may be indicated by swollen facial tissue, bruises and bruising around the eyes.
If the postoperative period is successful, the patient can be transferred to the neurosurgery department on the second day, where he will remain for up to 2 weeks.
After craniotomy, deformation of the skull and the formation of a colloidal scar may be observed (if tissue regeneration processes are disrupted). These phenomena are eliminated by surgical correction.
Recovery after surgery should include adequate drug treatment, elimination of neurological disorders, social and occupational therapy of the patient. Physical therapy classes (kinesitherapy) are required.
To improve the healing of sutures, you need to provide high-quality wound care every day and promptly change the dressing. Hair can be washed no earlier than 2 weeks after surgery, depending on the condition of the stitches.
If different parts of the brain are affected, patients often have to be re-taught to speak, walk, and help with memory restoration. Close people play a huge role. It is they who, in the first time after surgery, will help the patient cope with some inconveniences in everyday life, for example, taking water procedures, preparing and eating food.
Physical activity is excluded during the rehabilitation period; the patient must be provided with complete peace in psycho-emotional terms.
Disability after surgery is not always assigned, since craniotomy is not a reason for this.
If a person feels well and recovers quickly, then after a while he may well return to his usual lifestyle, going to work.
If he has complications, for example, in the form of neurological pathologies that limit life activity, then the issue of disability can be considered by a special commission consisting of different specialists.
source
Stroke and trepanation - what to expect in the end
Stroke is an acute cerebrovascular accident (CVA), leading to severe consequences. There is even such a thing as a “therapeutic window,” which means that the patient can be helped as fully as possible only in the first 6 hours.
One of the most severe types of stroke is hemorrhagic, the consequences of which are often unpredictable. It is accompanied by a cerebral hemorrhage resulting from a ruptured blood vessel.
The size of the hematoma can vary, and the same differences are observed in symptoms - from moderate to extremely severe.
If the size of the hematoma is above average and conservative treatment is ineffective, surgical treatment is often resorted to.
Sometimes the patient’s condition is so severe that surgery is the only option.
Surgical treatment of stroke - is there an alternative?
Since the consequences of a stroke are often irreversible, sometimes only surgery can save the patient's life.
One of the most common methods of surgical treatment of stroke, helping to stop bleeding or restore blood supply (in severe ischemic strokes) is craniotomy, or craniotomy, a complex operation that requires special equipment and experienced doctors.
It is craniotomy that is often the only way to give a person a chance to recover and return to normal life.
Before surgery, the following mandatory studies are carried out:
- duplex ultrasound scanning;
- computer or magnetic resonance imaging of the brain;
- angiography.
They allow you to accurately determine the location of the hematoma, its size, and the presence of plaques. And also assess the current state of blood flow, which ultimately helps the neurosurgeon determine the scope of the operation. It is worth understanding that a large hematoma will not resolve on its own, and if it is not promptly removed by craniotomy, the outcome will most likely be fatal.
Progress of craniotomy surgery
The entire operation, depending on the initial condition of the patient and the size of the pathological focus, can last up to 5 hours or more. There are several main stages of this surgical intervention.
Patient preparation
Anesthesia is administered intravenously and endotracheally, and the patient is placed on the operating table. A special device is rigidly fixed on the table, fixing the human head in a vertical position at three points. This ensures complete immobility during the manipulations (fixation occurs after the onset of sleep).
Sometimes a lumbar drain is installed in the lower part of the spine to drain cerebrospinal fluid - this helps reduce the pressure of the cerebrospinal fluid. If necessary, this effect is enhanced by medication.
After this, surgeons cut the skin, usually along the hairline - they try to minimize the cosmetic consequences of the operation.
Discovery of the skull
The skin is separated from the skull to the bone. One or more holes are made with a special drill, after which a pedicle bone flap is formed using a medical saw. As long as the craniotomy operation is ongoing, the flap is securely stored so that it can be put back in place later.
Autopsy of the brain and correction of the problem
Armed with special glasses with an operating microscope, the dura mater is opened. The brain itself is very tightly enclosed in the cranial cavity, so its soft tissues cannot move to the side.
Surgeons use very fine instruments to carefully work deep within the brain tissue. During the operation, constant monitoring of the condition of the cranial nerves and the general condition of the patient is carried out, this helps to avoid the negative consequences of the intervention.
Once the situation is corrected, the cranial cavity is closed.
Is there a high risk of brain surgery?
Sometimes the consequences of surgical interventions can be postoperative complications, not to mention brain surgery.
Craniotomy, which is often necessary for stroke, is a complex operation, the consequences of which can be unpredictable.
They largely depend on the severity of the stroke itself, the promptness of first aid and delivery to the operating table. All consequences of trepanation can be divided into surgical and non-surgical.
Surgical consequences
After surgery, complications that fall into the “category” of surgical complications may occur:
- intracranial bleeding;
- cerebral edema;
- infection;
- damage to brain tissue or blood vessels;
- epilepsy.
Surgery may cause swelling of the brain
Depending on the degree of the stroke itself, craniotomy is occasionally complicated by partial or complete paralysis. Separately, it is worth noting the symptoms of neurological deficits - problems with memory or perception, difficulties with pronunciation. Almost all patients after craniotomy complain of nausea and headaches (at first they can be relieved with narcotic analgesics).
Source: https://tepcontrol.ru/reabilitatsiya-posle-trepanatsii-cherepa-pri-insulte/
Complications
Complications after surgery occur when the patient’s condition is serious, when the body is not able to recover. The main negative consequences that can occur even after a successful operation are:
- Bleeding. It may appear when the vascular walls are highly fragile. In this case, within 2 days after the intervention, a violation of their integrity may occur and bleeding may develop.
- Infection. Such a complication is often the fault of medical personnel who, to one degree or another, violated sanitation rules during the operation.
- Damage to the brain tissue surrounding the affected area. In the case of intervention in a hard-to-reach area of the brain, when the patient’s life depends on it, doctors may disrupt the condition of the surrounding tissues, due to which certain functions of the body may suffer. Most often observed when a hemorrhagic stroke occurs in the cerebellum.
- Brain swelling.
- Coma.
Craniotomy for stroke: consequences
Sometimes craniotomy is necessary for a stroke. The stroke itself leads to disruption of blood flow in the vessels of the brain.
With a hemorrhagic stroke, a cerebral hemorrhage occurs: it is impossible to predict the patient’s condition. Therefore, if a very large hematoma is detected, surgery may be necessary.
This method of treatment is chosen when drug treatment is unable to produce positive results.
Stroke surgery
If the consequences of a stroke are difficult for the patient’s health, only surgery can correct the situation. Surgery of this level is very complex and is carried out using special equipment.
In this case, two methods are used:
- trepanation - drilling into the skull;
- Craniotomy - an incision into the skull.
This can help save the patient's life. But no specialist will make predictions in advance for a complete recovery.
Sometimes craniotomy is the patient’s only chance of recovery.
Before establishing the possibility and necessity of surgical intervention, you need to:
- Complete examination of blood vessels. To do this, a special scan is done using ultrasound.
- Be sure to conduct a full examination of the brain using a computer and a magnetic field.
- X-ray examination of blood vessels, which checks their function, blood flow and the development of pathology.
Only after examination can the size of the hematoma formed be determined. Afterwards, you can decide on the type of surgical intervention. It will be performed by a neurosurgeon.
If the hematoma is not removed, patients have virtually no chance of further life.
.
Stages of craniotomy
The progress of the operation directly depends on the patient’s condition. The development of a hematoma occurs within several hours.
There are several stages of this treatment method.
Preparatory stage:
- An anesthetic drug is administered using the chosen method, and the patient is transferred to the operating room.
Be sure to fix the body so that the patient does not have the opportunity to make unconscious movements. If necessary, a drainage is installed to drain cerebrospinal fluid. This helps reduce blood pressure. Sometimes medications are used for this. The skin incision is made so that even cosmetic seams are almost invisible. - The skull is opened after the skin is separated.
For trepanation, special drills are used and several holes are made with them. Then the skull bone is filed down to gain access to the brain. After the operation is completed, this part of the bone is put in place. - Direct brain surgery is performed using very fine instruments.
This is necessary because the brain is very tightly closed by the bones of the skull. A microscope will be used to monitor the patient’s condition at the time of surgery. At the end of the entire process, the skull is closed.
Any brain surgery is a complex procedure that requires extensive experience from the doctor and the use of special equipment
.
Percentage of risk and possible consequences
When there are medical indications for craniotomy, the unpredictability of the consequences must be considered. But sometimes refusal to perform such an operation will mean the patient’s recovery is impossible in principle. A positive prognosis can be made with timely assistance.
The ability to perform craniotomy may be complicated. This occurs when the patient is completely or partially paralyzed. Consciousness may be unclear, and the person partially loses memory. Speech may be unclear.
After craniotomy surgery, the patient may experience:
- nausea;
- headaches;
- difficult perception of reality.
Painkillers will help you get rid of pain, but you shouldn’t get too carried away with them.
Possible consequences:
- bleeding inside the skull;
- swelling of the brain;
- penetration of infection;
- mechanical damage to tissues or blood vessels;
- development of nervous diseases.
These complications are usually called surgical consequences. But there is another group - non-surgical.
These conditions appear after the patient begins to feel an improvement in their general health. His life is no longer in danger, and the person begins to worry about his appearance. After trepanation, he will experience a change in the skull, namely, in its shape. During the operation, trepanned bones may be removed.
To correct the situation, special plastic surgery must be performed.
The patient may also experience:
- sudden weight loss;
- memory impairment;
- short-term loss of consciousness;
- symptomatic epilepsy;
- disruption of the digestive system.
The cause of such symptoms may not only be the trepanation. These manifestations can be caused by medications or improper first aid for hemorrhage.
Restoration activities
Craniotomy for stroke is necessary to prevent the development of complex pathologies and brain diseases. The recovery period should help the patient return to normal life.
Restoration measures allow:
- eliminate the consequences of craniotomy;
- prevent the development of any complications;
- restore all vital functions of the body as quickly as possible.
The recovery process must proceed according to a certain pattern: the actions will depend on the type of trepanation. The sutures are removed after about 10 days, and the patient can be sent home.
But in the hospital the patient’s recovery is already beginning:
- Medicines are used to relieve pain. Therapy will also be needed to prevent any infection from developing.
- The functioning of all brain functions must be checked.
- Wounds are treated with antiseptics and dressings are performed regularly.
- And the prevention of various diseases is also important.
After discharge, the patient needs specific care and activities:
- mandatory hygiene of the wound and scars remaining after surgery;
- physiotherapy;
- classes with a speech therapist;
- massage and therapeutic exercises;
- being in the fresh air;
- proper nutrition;
- restoration of psycho-emotional background.
In this case, medications must be prescribed that can improve bleeding through the vessels. All medications are prescribed only by a doctor. He also recommends carrying out all restoration measures.
Craniotomy is a very complex operation. How a patient recovers completely depends on many factors. Restoring mental activity will be especially difficult. Therefore, it is better to take preventive measures to prevent stroke and lead a healthy lifestyle.
Source: https://BolezniKrovi.com/serdce/insult/trepanatsiya-cherepa-pri-insulte.html
Stroke and trepanation - what to expect in the end
Stroke is an acute cerebrovascular accident (CVA), leading to severe consequences. There is even such a thing as a “therapeutic window,” which means that the patient can be helped as fully as possible only in the first 6 hours.
One of the most severe types of stroke is hemorrhagic, the consequences of which are often unpredictable. It is accompanied by a cerebral hemorrhage resulting from a ruptured blood vessel.
The size of the hematoma can vary, and the same differences are observed in symptoms - from moderate to extremely severe.
If the size of the hematoma is above average and conservative treatment is ineffective, surgical treatment is often resorted to.
Sometimes the patient’s condition is so severe that surgery is the only option.
Non-surgical consequences
Once the postoperative period has passed and the danger caused by the stroke has receded, other difficulties come to the fore. The patient first begins to worry about the defect of the skull bones, since part of the bone is sometimes removed. Cranioplasty is a way out of the situation and prevention of trephine syndrome.
There are frequent cases of sudden weight loss by the patient, memory impairment, constant weakness, short-term disturbances of consciousness, episyndrome, and indigestion.
But it is impossible to say unequivocally that it is trepanation that causes such symptoms, since in the postoperative period a lot of potent drugs are prescribed; some of the symptoms can be caused by the stroke itself, especially if help is not provided in a timely manner.
Source: https://GolovaLab.ru/insulto/kak-lechit/trepanaciya-cherepa-pri-insulte.html
Long-term complications
After a stroke, the treatment of which required surgery, long-term negative consequences may also occur. It is not always possible to say for sure whether they are related to the primary disorder (stroke) or surgery. If the patient strictly followed all medical recommendations during the rehabilitation period, then the risk of long-term complications is significantly reduced.
Long-term complications of stroke treated surgically are:
- memory impairment;
- short-term disturbance of consciousness;
- increased fatigue;
- mental disorders that cause depression or attacks of aggression;
- a change in the functioning of the digestive system, due to which the patient loses weight in a short time to the point of exhaustion.
In most cases, long-term consequences occur when the patient’s condition is initially severe.
Craniotomy for stroke: indications, preparation, rehabilitation
A stroke is a serious disorder of cerebral circulation with rupture of a vessel, causing bleeding. This pathology leads to dangerous disorders of brain function, but the worst thing is the consequences of hemorrhage that forms a hematoma - possible disability and even death (if medical assistance was not provided within 6 hours).
Treatment with conservative methods is usually impossible, therefore, in order to help the patient and prevent the hematoma from enlarging, a decision is made to undergo surgery. In particular, if a person has a hemorrhagic stroke, then craniotomy is considered the only way to save him.
Contraindications to intervention
Surgery is not recommended for patients over 75 years of age, since often after surgery there is a deterioration in the patient’s health, as well as progression of neurological disorders and relapses of pathology.
This contraindication is not absolute, but most doctors consider surgery in old age to be futile.
Surgery is also recommended for:
- pulmonary, renal or heart failure in advanced forms;
- liver diseases;
- diabetes (decompensated form);
- blood pathologies;
- oncology.
Craniotomy for stroke
A stroke is a serious disorder of cerebral circulation with rupture of a vessel, causing bleeding. This pathology leads to dangerous disorders of brain function, but the worst thing is the consequences of hemorrhage that forms a hematoma - possible disability and even death (if medical assistance was not provided within 6 hours).
Treatment with conservative methods is usually impossible, therefore, in order to help the patient and prevent the hematoma from enlarging, a decision is made to undergo surgery. In particular, if a person has a hemorrhagic stroke, then craniotomy is considered the only way to save him.
What are the indications?
Craniotomy (French - trépanation, Latin - trepanatio) is an operation that involves opening the skull to provide access to hematomas in the brain area with their subsequent removal. Timely and correctly performed surgery reduces intracranial pressure. In 85%, the prognosis after trepanation is favorable.
Craniotomy is indicated for stroke in the following cases:
- infectious processes, inflammation in the brain;
- traumatic brain injuries;
- oncology;
- presence of blood clots;
- increased intracranial pressure;
- serious problems with blood vessels;
- the need to obtain brain tissue for biopsy.
Surgery for a cerebral stroke is performed by a neurosurgeon. Its success depends on the professionalism of the doctor and the availability of high-quality specialized equipment.
Preparation and stages of the operation
During the preoperative period, the patient is required to undergo a number of studies: chest x-ray, blood test, MRI, ECG. Also, the doctor should be aware of the patient’s allergies of various etiologies.
Non-steroidal anti-inflammatory drugs and blood thinners are not taken before surgery.
It is extremely important that at least 14 days before craniotomy, the patient completely gives up bad habits - smoking and alcohol.
What actions does the operation contain:
- Administration of anesthesia, insertion of lumbar drainage, removal of cerebrospinal fluid.
- An incision in the skin to gain access to the skull, scraping the skin from the bones of the skull. If this is not done, the remains of the dermis will fall into the open cranium.
- Treatment of the head with an antiseptic preparation along the hairline.
- Opening the skull: drilling several holes to gain access to the brain. The pieces of bone obtained by drilling are placed in a separate container - after the hematomas are removed, they are put in place.
- Removing blood stagnation, stitching together burst vessels, stopping bleeding. Screening monitors the patient's vital signs.
- Restoring the structure of the skull with missing parts.
- Completing the operation.
The surgical process takes 3-4 hours, but sometimes the operation can last up to 8 hours - it all depends on the stage of the pathology.
Risks of complications
Craniotomy is a complex operation that involves certain actions on the brain. It is impossible to guarantee a favorable outcome of a surgical intervention, since this is influenced by many factors: the individual characteristics of the body, the extent of the stroke, the patient’s age, and concomitant pathologies that occurred even before the operation.
The so-called risk group includes patients who have: diabetes mellitus, cardiovascular diseases, atherosclerotic formations, excessive accumulation of fatty deposits. Possible complications include general and surgical ones.
Experts include the second type of complications:
- infection of brain tissue;
- heavy internal bleeding or local hemorrhage;
- cerebral edema;
- mechanical trauma (damage to brain tissue, blood vessels with surgical instruments);
- epilepsy;
- paresis, paralysis;
- disorders of the central nervous system - memory impairment, absent-mindedness, slurred speech.
General complications, expressed in deterioration of health (vomiting, intestinal upset, critical weight loss, dizziness), develop after surgery, when the patient recovers from anesthesia and gradually returns to normal life. Patients who have had to undergo craniotomy, which is a serious operation, often experience a stressful state.
Who should not undergo surgery?
After an attack, a person needs a lot of time for rehabilitation. At this time, the body is still very weak, and surgery after a stroke doubles the load on it, which can lead to a relapse. For example, cataract removal should be carried out no earlier than six months after the end of a stroke; preference should be given to laser surgery rather than ultrasound.
Despite the effectiveness of craniotomy proven by medical practice, there are a number of contraindications that do not allow this operation to be performed. These include:
- hypertension;
- the time interval between heart attack and stroke is less than 6 months;
- congestive heart failure;
- progressive brain diseases;
- poor blood clotting;
- renal and liver failure;
- old age - after 70 years (not in all cases a reason for refusal to undergo surgery);
- malignant tumor;
- acute phase of inflammation accompanied by the formation of pus;
- neurological deficit.
Trepanation is prohibited if the patient is in a coma.