Regulation of heart rate is a complex reflex mechanism caused by the work of several structures of the central and peripheral nervous system.
There are two main conditions when the heart rate changes: tachycardia (the actual acceleration of the rhythm above 90 beats per minute) and the reverse process: bradycardia. Both pose an immediate danger to the health, and sometimes even the life of the patient.
Tachycardia has nothing to do with low, high or normal blood pressure. Indicators of heart rate and blood pressure levels need to be considered separately, since they differ in the mechanism of development.
A high pulse with normal pressure is the most common, but it is difficult to determine the cause by eye: there are no visible changes in the cardiovascular system. A thorough diagnosis is required.
How dangerous is this condition? Very dangerous, especially if it lasts for a long time. Complications are possible.
What do you need to know about rapid heartbeat in different groups of patients?
Causes not related to pathologies
There are not many physiological factors for the development of tachycardia. But they exist and are detected in 30% of cases.
Among the stated reasons are:
- Use of certain drugs that have a hypertensive effect. Among them are Atropine, corticosteroids, including Prednisolone, Dexamethasone and others. Also, long-term use of diuretics, which, when used frequently, give the exact opposite effect.
- Unfavorable climatic factors. Particularly hot weather and stuffy air provokes a decrease in the concentration of oxygen in the blood and its thickening. Hence the need to more intensively pump hematological fluid throughout the body: otherwise hypoxia will occur. This is a well-thought-out mechanism, although dangerous for the person himself.
- Significant emotional stress. They are associated with the release of catecholamines and corticosteroid substances. Including cortisol. Both positive and negative emotions are equally dangerous. There is no big difference from a physiological point of view.
- Consumption of active substances with tonic properties: tea, coffee, energy drinks.
- Smoking. Causes generalized hemodynamic (blood flow) disturbances and stenosis (narrowing) of blood vessels. Tachycardia is often observed against the background of normal blood pressure or a slightly elevated level.
- Physical exercise. From minor ones, like climbing stairs, brisk walking, to significant ones, like working out in the gym. Everyone has their own norm for physical activity, their own limit.
- Substance use. First of all, alcoholic beverages (ethanol puts a lot of stress on the cardiovascular system). Especially narcotic drugs and their analogues. Cocaine is particularly active in this regard. It causes persistent and prolonged tachycardia, it is not controlled by classical drugs and is difficult to eliminate even in a hospital setting.
Physiological factors are limited to this. If the pressure is normal and the pulse is high, you also need to look at pathological causes, they are more likely and are diagnosed in 70% of cases.
Possible pathologies with increased heart rate in combination with other symptoms
In addition to strong pulsation, the patient may suffer from other manifestations of the disease. It all depends on the main reason that caused this violation. Tachycardia is a symptom of many diseases. Most often it manifests itself in heart defects, dysfunctions of nervous regulation and endocrine disorders.
Tachycardia with defects
In this situation, a rapid pulse causes attacks that have clear boundaries. The patient can know exactly the time of the onset and end of the attack. The heartbeat increases in a calm state or during stress and physical activity.
At the same time, the vital organ contracts with a frequency of more than two hundred beats. The person also suffers from other symptoms. Patients usually:
- dizzy;
- fainting conditions are observed;
- noise in the ears;
- the heart feels like it’s going to jump out of the chest or there’s a pressing sensation in the chest;
- sweating increases;
- in some cases nausea appears.
Also read: Sinus tachyarrhythmia: what is it, normal or pathology
Paroxysms are quite dangerous to health, as they can cause flutter or ventricular fibrillation. During an attack, the likelihood of developing cardiogenic shock and cardiac arrest increases.
This condition requires immediate treatment, which often involves surgery.
Disturbances in nervous regulation
Various types of dystonia are accompanied by an increase in contraction frequency.
In people suffering from vegetative-vascular dystonia, the pulse rises to 140 beats. In this case, the heart reacts poorly to physical activity. In some cases, the health deteriorates so much that the patient finds it difficult to climb stairs or walk.
Neurocirculatory dystonia is also characterized by an increase in pulse, which can be a constant concern or occurs in attacks.
If the patient has VSD, then in addition to strong heartbeat:
- often feel dizzy and have ringing in the ears;
- worried about constant weakness and excessive fatigue;
- sweating increases;
- feeling worse in stuffy rooms;
- there is constant anxiety and suspiciousness;
- I want to sleep all the time;
- mood changes suddenly;
- hot and cold flashes bother you;
- sometimes panic attacks and obsessive states are observed.
In the case of pronounced symptoms, dystonia is difficult to distinguish from neurosis or psychosis.
Various manifestations indicate that neurocirculatory dystonia is developing:
- hands and feet are constantly cold;
- the skin turns pale;
- a person gets tired quickly;
- headache and dizziness;
- pressure in the arteries increases or decreases.
These pathologies are eliminated depending on the manifestations. The patient's condition should be monitored by a neurologist and cardiologist.
Endocrine disorders
Rapid pulse and heartbeat always accompany hyperthyroidism. In this condition, the thyroid gland produces more hormones than it should. In this case, tachycardia becomes permanent. The pulse reaches 120 beats. The heart rate does not slow down even when the person is sleeping. The pathological condition is recognized by:
- an increase in the size of the thyroid gland;
- large difference between systolic and diastolic blood pressure;
- painful sensations in the abdominal area;
- increased appetite due to sudden weight loss;
- increased sweating;
- irritability and fatigue;
- disruptions in the menstrual cycle, breast enlargement, potency problems in men;
- increased blood sugar;
- increase in liver size.
An endocrinologist should treat such problems.
In rare cases, a persistent increase in heart rate occurs with hypothyroidism.
Pathological causes of cardiac origin
More numerous and variable in character. Among the immediate pathologies that provoke the development of tachycardia are:
- Heart defects, both congenital and acquired. They are diverse in their manifestations and degree of danger. But, as a rule, pathology is eliminated only by surgical methods.
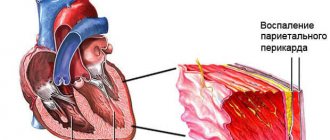
- Inflammatory diseases affecting the structures of the heart. Myocarditis, endocarditis and others.
They pose a colossal danger to life and health and can result in acute necrosis of anatomical structures or a sudden stop in the functioning of an organ with rapid death.
- Heart attack. Acute malnutrition of the myocardium with subsequent death of organ tissue. This is an extremely dangerous condition.
Even if help is provided in a timely manner, a person risks becoming disabled: functional muscle tissue is replaced by scar tissue that is not capable of contraction (post-infarction cardiosclerosis).
Hence, a decrease in the efficiency of the heart muscle, circulatory disorders of all organs and tissues, heart failure and the possibility of “going to the second round” with the development of a second heart attack. Lethal this time.
- Chronic congestive heart failure. Disease of old age. Is it always like this? No. In recent years, there has been a tendency towards rejuvenation of the pathological process.
Its essence lies in the development of a decrease in cardiac output. This ends in acute ischemia or, in other words, infarction. Without proper treatment, it's a matter of time.
Treatment Options
An increased heart rate is a treatable problem. Methods for eliminating the disorder depend on the underlying disease. Conservative and surgical treatment methods are used.
Depending on the problem, heart disease can be treated using:
- statins;
- antiplatelet agents and anticoagulants;
- nitrates;
- beta blockers;
- immunomodulators;
- antifungal, antiviral or antibacterial agents;
- cardiac glycosides;
- B vitamins;
- multivitamin complexes.
If a person is diagnosed with a heart defect, they resort to surgical treatment. For arrhythmias, radiofrequency ablation is used. The operation option is selected taking into account the disease, the patient’s age, and the individual characteristics of the body.
To avoid such violations, it is recommended to lead a healthy lifestyle, avoid the negative influence of provoking factors, undergo timely treatment for pathologies of internal organs, and regularly undergo preventive examinations.
Pathological noncardiac causes
- Dehydration. Large loss of fluid leads to thickening of the blood. The result is an increased load on the heart due to the need to pump it more actively. Hematological fluid is forced to overcome greater resistance. The entire load falls on the cardiovascular system. In such a situation, a pulse above 100 is possible with normal blood pressure.
- Infectious diseases. As fever develops, the pulse begins to increase. Why is that? It's all about toxic irritation of the heart structures and special centers of the brain, which causes a high pulse rate while maintaining normal blood pressure. The heart pumps blood faster to cleanse it of toxins that are abundantly produced by pathogenic flora.
- Neurotic diseases. They are fraught with the development of tachycardia due to the release of large amounts of stress hormones: cortisol, norepinephrine and adrenaline. Also catecholamines in different concentrations. Cause characteristic symptoms. The pressure often rises, but normal tonometer readings are also possible.
- Heavy bleeding. For example, during the menstrual cycle in the fairer sex or after childbirth. The main development factor is a violation of the volume of circulating blood. To provide the tissues with the necessary amount of substances and oxygen, this requires increasing the number of beats per minute.
- Anemia. Iron deficiency in 90% of cases is less common - hemolytic, B12 deficient, aplastic is accompanied by a constantly rapid heartbeat.
The reason for a high heart rate with normal blood pressure may lie in a disruption of the hormonal system.
Including damage to the adrenal glands of a tumor or other nature, changes in the functioning of the thyroid gland (hyperthyroidism, when there are so many hormones that they begin to poison the body).
Possible tumors of the pituitary gland with the development of characteristic phenomena from the entire endocrine system.
The reasons need to be considered separately. The diagnosis is made by exclusion, after a thorough examination.
The causes of increased heart rate do not depend on age and gender. Everyone suffers equally, so the factors described are subject to assessment.
Symptoms of tachycardia
If the heart muscle contracts intensely under emotional stress, then there is no need to worry. The condition stabilizes on its own. With painful throbbing, the following symptoms are usually present and should not be ignored:
- increased sweating;
- dizziness;
- dark spots before the eyes;
- presyncope, often ending in fainting;
- difficulty breathing, a feeling of lack of air, shortness of breath, you can feel your heart beating, you are very thirsty. Breathing problems also occur in a calm state;
- severe weakness that comes on suddenly;
- feeling of stiffness, squeezing in the sternum.
If a tumor grows inside, then tremors of the limbs, headaches, increased dryness of the skin, and irritability are added to the listed symptoms.
How dangerous is tachycardia and what consequences can be expected?
Ideally, you should not expect consequences dangerous to health and life. It is better to consult a doctor at the first suspicion.
Among the possible complications of tachycardia, especially over a long period of time:
- Possibility of cardiac arrest. It always exists with tachycardia, since the process is often chaotic. The complication ends with the patient's imminent death.
- Generalized disorders of metabolic processes in the body with the formation of immunodeficiency and other consequences. Happens frequently.
- Fainting on a regular basis. They determine the danger of injury, even fatal, because they take a person by surprise, sometimes at the most unfortunate moment.
- The development of a sharp decrease in blood pressure or so-called cardiogenic shock. Threatens the imminent death of the patient.
- Increased likelihood of myocardial infarction. The reason lies in the disturbance of trophism (nutrition) of the heart muscle itself; the phenomenon increases as the process develops.
- The risk of thromboembolism and blockage of blood vessels due to blood clots.
To prevent complications, you need to promptly contact a cardiologist for diagnosis and treatment.
Diagnostics
To determine the causes of increased heart rate, you need to conduct a number of diagnostic studies:
- Consultation of narrow specialists. At this stage, you may need the help of a cardiologist, narcologist, psychiatrist, or neurologist. A referral to these doctors is issued by a therapist after a preliminary examination and interview of the patient.
- Blood tests - general and biochemical. A study may also be performed to determine the level of thyroid hormones.
- Complete cardiac examination. To do this, they do an electrocardiogram, a study of the state of the heart with a load, ultrasound diagnostics, etc.
What to do at home
You can try to lower your heart rate at home, but only with caution: complications of the condition are possible. How this can end has already been said.
Attention:
Indicators of 90-120 beats per minute are acceptable; anything higher requires an urgent call to the ambulance.
The algorithm is as follows:
- Make the patient sit down. Place a soft cushion of blankets or a pillow under your back. The main thing is not to lie down, otherwise blood circulation will be uneven. On the one hand, this will cause an even greater acceleration of the heart rate, on the other hand, breathing will be impaired, and the risk of pulmonary edema will increase. It can all end in the death of the patient.
- Breathe slowly and evenly, holding your breath as you exhale. This will not only normalize your heart rate, but also bring your blood pressure into order if the numbers creep up.
- Before the doctors arrive, no unnecessary movements, just rest and measured breathing. You should not take drugs like Bravadin. It is not known what the origin of the pathological process is. You can only make things worse if you act on your own.
- If your pulse is high, you can take one tablet of the beta blocker Anaprilin, 50 mg, no more. With a slightly pronounced heartbeat (up to 110 beats per minute), half is enough.
- Additionally, you can drink motherwort (1 tablet) or valerian (1 tablet).
- The following composition of folk remedies is allowed: yarrow herb, calendula, anise and peppermint are mixed in equal proportions and poured with boiling water (500 ml). You can drink in any quantity.
If after 20 minutes the heart rate has not decreased, you need to call an ambulance. There is no point in hesitating or hesitating; your health and maybe your life are at stake.
When the team arrives, the issue of assistance on site and transportation of the patient to the cardiology hospital is decided.
If hospitalization is not possible, it is recommended to consult a cardiologist as soon as possible.
In the long term, it is possible to reduce a high pulse without lowering blood pressure only by using a certain combination of drugs. The selection of medications and dosages is the prerogative of the doctor.
What you should not do: drink medications other than those described, douse yourself with cold or warm water, eat, turn to other folk recipes. Many are downright dangerous.
Factors causing tachycardia
Certain habits, lifestyle, and monotonous food increase your heart rate. Provoking factors that can increase performance include:
- excessive consumption of coffee, chocolate, strong tea;
- uncontrolled use of drugs from the group of tranquilizers and antidepressants;
- long-term use of certain medications;
- lack of physical activity;
- excess weight;
- severe fatigue;
- stressful situations;
- lack of magnesium and calcium in the body.
Tachycardia is often a concern in old age. In older people, the pulse may increase due to any, even minor, experience. You should not delay your medical appointment. It is necessary to relieve the symptoms and treat the diagnosed disease.
When is it necessary to call an ambulance?
The answer is simple: in the presence of tachycardia lasting more than 20 minutes. The following symptoms should especially alert the patient:
- A sharp headache for no apparent reason. May indicate increased hypertension, that is, increased blood pressure.
- Dizziness. The nutrition of the cerebellum, which regulates the entire vestibular apparatus, is disrupted. Orientation in space must be present.
- Disturbances in the functioning of the heart. If an arrhythmia such as fibrillation or extrasystole occurs, it is deadly. Calling an ambulance is necessary. Subjectively, it feels like missing a beat, slowing down and speeding up activity, and tying a knot.
- Chest pain of any nature and any degree of intensity. Perhaps we are talking about developing acute myocardial ischemia.
- Shortness of breath, suffocation. In a word - breathing problems.
- Nausea.
- Vomit.
- Sweating.
- Cyanosis of the nasolabial triangle (blue discoloration of the skin around the mouth).
All these are reasons for urgent qualified help. You should consult a doctor as soon as possible, discarding false attitudes and doubts. Health is more valuable.
When is palpitations a reason to see a doctor?
A rapid heartbeat is a reason to see a doctor if it:
- too intense;
- is protracted (does not go away for a long time);
- occurs with less and less exposure to the above factors;
- occurs independently of the above factors;
- is uneven in nature (arrhythmia can be assumed - a violation of the heart rhythm).
In these cases, rapid heartbeat may be a manifestation of serious disorders and diseases, such as:
- avitaminosis;
- anemia (low hemoglobin and iron in the blood);
- tetany (a condition caused by a lack of calcium);
- endocrine diseases;
- heart pathologies.
However, as a rule, in the case of myocarditis, other heart diseases, and hyperthyroidism, palpitations are not the main complaint. With such diseases, first of all, they complain of pain in the heart and shortness of breath.
It is necessary to react promptly if, against the background of increased heartbeat, dizziness, shortness of breath, pale skin, and sweating are observed. In this case, you should call an ambulance.
Diagnostic measures
Diagnosis is carried out by a specialized cardiology specialist. At the discretion of the doctor, assistance from other specialized specialists may be required: a cardiologist and a neurologist.
The examination scheme for patients with tachycardia has been worked out and is clear:
- Questioning the patient. To identify characteristic complaints, and therefore symptoms of a possible pathological condition.
- Taking an anamnesis to determine etiological factors that can lead to the formation of tachycardia.
- Blood pressure measurement.
- Electrocardiography. The most valuable research method, especially for complex patients. But it is important to have sufficient qualifications to decipher.
- Invasive electrocardiography. Rarely used due to complexity. However, it allows you to assess the degree of cardiac conduction.
- 24-hour blood pressure monitoring using an automatic tonometer. Allows you to evaluate not only your heart rate, but also your blood pressure level. Also the dynamics and behavior of cardiac activity.
- Angiography in some cases.
Usually this is enough. If necessary, the neurological status and levels of hormones in the bloodstream are checked.
Methods for lowering heart rate
You can get rid of an attack of increased heartbeat by coughing, pinching, or blowing your nose. It is also useful to wash your face with cold water. There are other methods to solve the problem:
- Take a deep breath and hold your breath for a few seconds, then exhale slowly.
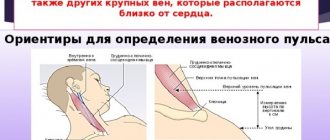
- You can easily massage the carotid artery.
- Some medications help. In such situations, Valocordin or Corvalol. 20-30 drops are enough.
Medical assistance for a rapid pulse is necessary if these methods do not help improve the condition and the patient’s well-being quickly deteriorates.
Treatment methods
Diverse. The main goal of therapy is to eliminate the underlying pathological process causing tachycardia.
Everything else is symptomatic measures designed to combat the effect without affecting the cause.
Among the treatment methods:
- Use of specialized medications such as beta blockers, calcium channel blockers, and heart rate normalizers. Only the doctor selects the specific names of the drugs.
- Surgical interventions on the heart to install an artificial pacemaker, defibrillator or correct a defect. These methods are resorted to in extreme cases, due to their complexity.
It is also recommended to normalize your lifestyle. Avoid intense physical activity, only prescribed sets of therapeutic exercises.
No alcohol or tobacco products, as they will worsen the patient’s health condition. Also tidy up your diet: as little salt as possible, as much healthy plant foods and protein as possible.
Together, these methods will give the desired effect in the shortest possible time. It is important to follow all the recommendations of the treating specialist and not engage in amateur activities.
What examinations are recommended?
A visit to a cardiologist is indicated on a planned or urgent basis. An approximate list of diagnostic measures:
- Oral questioning of the patient. Interested in complaints, as well as the frequency of tachycardia attacks. How long ago did the process begin, how much does it interfere?
- Anamnesis collection. Interested in lifestyle, family history, past pathological processes, current diseases.
- Measurement of blood pressure, heart rate. Both are outside the normal range. Blood pressure is below adequate levels, heart rate is higher.
- Daily monitoring. Using a special automatic tonometer. To assess the condition
- health over time. Electrocardiography. Functional features are subject to research. This is a specialized technique for identifying arrhythmias of various types, including combined ones.
- Echocardiography. Ultrasonic method of tissue visualization.
- General blood test, hormones and biochemical.
Basically this is enough. An MRI may be ordered as needed.
Help with palpitations
Quick help with a strong heartbeat and a subsequent decrease in the pulse rate consists of the following actions that effectively reduce the pulse rate and relieve pain:
- open the window;
- remove clothes that interfere with air access, unfasten the buttons on the neck;
- wash with cold water;
- It’s better to lie down, or at least take a sitting position, but not stay on your feet;
- you need to give a person to drink 30 drops of tincture of valerian, motherwort, Corvalol. A Validol tablet under the tongue is suitable;
- lying with your eyes closed, press your fingertips on your eyeballs and remain in this position for 10 seconds. Release, and after 10 seconds repeat the procedure until a feeling of relief occurs.
If your pulse quickens, you can stretch a mint or lemon balm leaf with your fingers, then smell the plant.
When attacks recur too often, you cannot prescribe treatment for yourself and draw independent conclusions about the diagnosis. It is necessary to visit a doctor, sign up for all prescribed diagnostic tests, and find out why the problem arose.
A rapid heart rate may be a symptom of a serious illness. Seizures cannot be ignored, even if they go away on their own. It is necessary to treat the pathology and do everything possible to reduce the pulsation.