Increased blood viscosity can cause unfavorable pregnancy outcomes, premature birth and fetal death. What is thrombophilia during pregnancy? This is a pathological condition in which a blood clot can block the lumen of a vessel and impede blood flow. In the article we will look at the causes of blood clots, treatment and prevention of the disease during the period of planning conception and during gestation.
What is thrombophilia, the causes of increased thrombosis
Thrombophilia is an increased predisposition to the development of vascular thrombosis (mainly venous) of various locations due to genetic defects in the hemostatic system. The process of thrombus formation is a natural reaction of the body when blood vessels are damaged, aimed at stopping bleeding . In thrombophilia, the formation of a clot provokes a decrease in the inflow (in the arteries) or outflow (in the vein) of blood. If a blood clot detaches from the wall of an artery or vein, an embolus is formed - a particle that moves with the blood flow and can stick to the walls of other vessels.
The resulting blood clot is firmly attached to the site of endothelial damage, however, in some cases, the entire blood clot or its fragments can break off and enter other tissues and organs, leading to circulatory disorders
Blood clots often clog veins. In addition to the vessels of the lower extremities and the pulmonary artery, mesenteric veins, portal, hepatic, renal, and rarely veins of the upper extremities and brain are susceptible to thrombosis.
This pathology is widespread; up to 40% of the adult population suffers from its consequences, depending on the location of formation:
- blood clots in the legs: deep veins - thromboembolism or blockage of the pulmonary artery, chronic venous insufficiency;
The pulmonary artery will manifest itself as sharp chest pain, coughing up blood, difficulty breathing and a drop in pulse and pressure - main arteries - tissue necrosis and subsequent amputation.
Acute occlusion of mesenteric vessels is manifested by a sharp disturbance of blood circulation in the vascular areas proximal and distal to the site of obstruction, accompanied by severe vasospasm and additional thrombus formation, resulting in acute malnutrition and ischemic damage to the intestinal wall
Acute ischemia causes the death of some functional muscle cells (necrosis) and their subsequent replacement with connective tissue fibers, i.e. the formation of a post-infarction scar
The accumulation of peritoneal fluid during ascites is accompanied by an increase in intra-abdominal pressure, pushing the dome of the diaphragm into the chest cavity
Causes of increased thrombosis:
- thrombophilia in first-degree relatives;
- blood diseases: essential thrombocythemia - a tumor process accompanied by a violation of the formation of platelets in the bone marrow, as a result of which their excess enters the blood;
- erythermia is a tumor disease expressed by the proliferation of red blood cells due to disturbances in the regulation of blood formation;
It is worth noting that in 2/3 of cases, simultaneously with an increase in the level of red blood cells, platelets and leukocytes also increase - atherosclerosis is a chronic disease of the arteries that occurs as a result of impaired lipid metabolism (including fatty acids) and is accompanied by the formation of cholesterol growths in the inner lining of blood vessels;
According to statistics, the presence of atherosclerotic plaques and different stages of the disease are noted in every fourth person over 35 years of age - antiphospholipid syndrome is an autoimmune disease consisting of the formation of antibodies to the structural units of bilayer cell membranes of the lipid class - phospholipids;
- chronic circulatory failure - oxygen starvation of the body due to reduced functionality of the cardiovascular system both at rest and during exercise.
Varicose veins, or varicose veins, are pathological changes in the veins, accompanied by their saccular expansion, increase in length, formation of convolutions and knot-like tangles, which leads to valve failure and impaired blood flow
Preparing for pregnancy with a bleeding disorder
Planning pregnancy with thrombophilia requires consultation with a gynecologist, geneticist, hematologist, as well as a whole range of studies aimed at establishing the fact of hypercoagulation and clarifying the cause of this condition.
Tests are required in the following situations:
- in case of antenatal fetal death;
- when repeated episodes of preeclampsia and eclampsia are detected in a pregnant woman;
- against the background of habitual miscarriage, if other causes of this condition are excluded - endocrine pathologies (disorders of the thyroid gland, pituitary gland, adrenal glands), intrauterine infections, genetic pathologies, gynecological diseases;
- when thrombosis is detected in a woman, including those that occurred before pregnancy;
- for thrombosis that occurred during contraception, for which COCs (combined oral contraceptives) were prescribed;
- when identifying in a pregnant woman before conception any conditions that are suspicious of hypercoagulation (thrombophlebitis of any localization, arterial and venous thrombosis);
- if visible manifestations of varicose veins are detected in the patient (during examination during consultation);
- with an unfavorable family history - the presence of thrombosis, thromboembolism, heart attacks and ischemic strokes in close relatives, especially in cases where these diseases developed at a relatively young age (up to 40 years).
Livedo reticularis and telangiectasia are symptoms of thrombophilia, noticeable upon examination during consultation
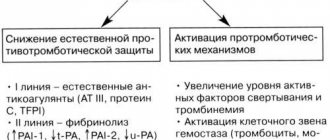
To confirm hypercoagulation, it is recommended to take a coagulogram with the obligatory determination of D-dimer (a product that is formed when a blood clot is destroyed). If changes in indicators are detected in these tests, diagnostics are prescribed aimed at identifying polymorphism of genes of the hemostatic system.
Both studies are carried out in modern laboratories, but if the price of a coagulogram is affordable for all pregnant women, the cost of genetic diagnostics is quite high. Thrombophilia is detected in approximately 10-12% of the population, so such tests are prescribed strictly according to indications.
Before genetic testing, the doctor may recommend tests that confirm or refute the presence of acquired thrombophilia.
For this purpose the following is prescribed:
- identification of lupus coagulant - this specific protein is synthesized in the body during autoimmune pathologies;
- determination of antibodies to antiphospholipids - these proteins damage the inner lining of blood cells and the walls of blood vessels;
- a quantitative study aimed at clarifying the level of homocysteine - an amino acid, the concentration of which decreases with insufficient intake of B vitamins from food, physical inactivity, and smoking.
Interpretation of the results of genetic studies allows us to determine the type of carriage of the altered gene. In homozygotes, the manifestations of thrombophilia are more pronounced, and treatment requires more effort, while in heterozygotes, half of the genes are normal, so the pathology is easier and the prognosis for pregnancy is better.
To clarify the causes of hypercoagulation, 10 markers are used, the most important of which are considered:
- genes responsible for folate metabolism;
- genes responsible for homocysteine metabolism;
- genes that determine platelet integrin;
- genes affecting prothrombin mutations;
- Leiden mutation (factor V of the blood coagulation system).
One patient may have a combination of several altered hemostasiogram factors, which worsens the pregnancy prognosis.
Blood tests – tests to detect clotting disorders
In addition, depending on the result, a thrombophilia treatment program is selected during the period of pregnancy planning and childbearing. Positive tests do not mean mandatory and immediate prescription of drug therapy - treatment is necessary if signs of hypercoagulation are detected.
If there are no such changes, then monitoring the coagulogram is necessary - the analysis is repeated at least once a month in the absence of complaints, and immediately if any changes in well-being or signs indicating possible thrombosis appear.
How does pregnancy affect thrombophilia?
Genetically determined thrombophilia affects generation after generation, but does not reveal itself for a long time. But with the onset of pregnancy and a change in blood viscosity, this tendency to form blood clots begins to become excessively active.
Pregnancy increases the formation of blood clots by 4-5 times, because the blood changes its viscosity under the influence of hormones.
Video: researcher, obstetrician-gynecologist, author of books on women’s health E. Berezovskaya on thrombophilia and pregnancy
Types of thrombophilias
The types of these violations are presented in the table
| Type of disease | Causes |
| Acquired | Concomitant diseases - polycythemia, heart disease, taking hormonal drugs, past infections |
| Gennaya | Hereditary pathologies and mutations affecting blood clotting. It occurs at the gene level and is expressed by a congenital increase in blood clotting factors. Often found in close relatives |
| Immune | Autoimmune disorders, in which the mother’s body produces antibodies to her own tissues, and alloimmune, manifested by the production of antibodies to fetal tissues |
| Vascular | Atherosclerosis, vasculitis, varicose veins, diabetic vascular lesions |
| Hemodynamic | Disruption of blood flow through vessels caused by decreased blood pressure and increased blood viscosity |
| Hematogenous | Acquired disorders of the hematocoagulant, anticoagulant and fibrinolytic systems |
Severe cases of thrombophilia are caused by several factors. For example, impaired blood flow is combined with congenital increased thrombus formation.
All types of thrombophilias are much more complicated in women over 35 years of age who have given birth a lot or, conversely, are expecting their first child at this age. Abortions, recurrent miscarriages and severe concomitant illnesses affect the course of pregnancy.
What is the most dangerous period of pregnancy?
The most dangerous period is up to 10 weeks, when the risk of miscarriage is especially high due to the formation of a blood clot in the vessels of the placenta during its increased nutrition to ensure the vital activity of the fetus. If this milestone was successfully overcome, you should remember that in the 3rd trimester of pregnancy the risk of developing thrombosis will increase again. After 30 weeks, a pregnant woman’s body intensively prepares for childbirth and blood clotting increases noticeably. When preparing for childbirth, the levels of the following estimated coagulation indicators are additionally checked:
- prothrombin or coagulation protein, normal - 8–142%;
- thrombin time or aPTT, during which blood clotting occurs. Normal - 11–17.8 seconds;
- Fibrinogen is a plasma protein responsible for the formation of a blood clot. Its normal content is 2.00 - 4.00 g/l;
- atithrombin is a specific protein that ensures the resorption of a blood clot, normally 75–125%.
Bottom line
Thrombophilia during pregnancy is not a death sentence. The disease can be defeated if treatment is started on time. To successfully carry a fetus, you should not only take blood thinning medications on time, but also lead an active lifestyle with the right diet. You need to undergo regular examinations and tests - this will help prevent the formation of a blood clot. There is no need to be afraid of death: timely blood thinning will prevent blood clots from forming and causing harm to the body. These comprehensive measures will help you maintain your health, carry your baby to term, and give birth without a cesarean section. When diagnosed with thrombophilia, the birth of a child at 37 weeks is the norm, not a deviation.
What hormonal medications did you take to stimulate ovulation?
- Gonal 33%, 4091 votes
4091 votes 33%4091 votes - 33% of all votes
- Clostilbegit 25%, 3038 votes
3038 votes 25%
3038 votes - 25% of all votes
- Menopur 16%, 1990 votes
1990 votes 16%
1990 votes - 16% of all votes
- Puregon 14%, 1737 votes
1737 votes 14%
1737 votes - 14% of all votes
- Decayed 8%, 998 votes
998 votes 8%
998 votes - 8% of all votes
- Menogon 3%, 374 votes
374 votes 3%
374 votes - 3% of all votes
Total votes: 12228
Voted: 8996
January 17, 2018
×
You or from your IP have already voted.
Possible consequences and complications of recurrent thrombophilia
Hereditary or acquired thrombophilia is considered the most likely cause of such obstetric complications as:
- miscarriage;
- IUGR or fetal growth retardation, when its growth and development parameters do not correspond to the obstetric gestational age;
- death of the fetus in the womb or stillbirth;
- placental insufficiency with delayed fetal development and oxygen starvation (hypoxia);
- premature detachment of a normally located placenta - early separation of the placenta from the walls of the uterus that occurs before the birth of the fetus;
- gestosis is a deviation from the normal course of pregnancy, characterized by a set of main symptoms: edema, protein in urine tests, increased pressure;
- eclampsia is the most severe, critical form of gestosis, occurring with convulsive syndrome, loss of consciousness, and the development of post-eclamptic coma;
- fetoplacental insufficiency.
How is diagnosis carried out?
Women prone to thrombophilia are registered in the pathology department from the first months of pregnancy, where the condition will be monitored until delivery. Throughout the entire period of bearing a child, the pregnant woman will need to undergo tests, ultrasound, and caulogram. To monitor the condition, a general and specific blood test is taken. The results of a general analysis for thrombophilia show an increase in red blood cells, D-dimer and blood clotting rate.
Specific diagnosis for thrombophilia markers gives the following results:
- lack of proteins C and S, antithrombin III,
- Leiden mutation.
Clinical manifestations of thrombophilia
Depending on where the clot has formed, the symptoms are different:
- For hepatic vein thrombophilia and ascites:
- increase in abdominal volume;
- increased gas formation;
- heaviness;
- feeling of fullness;
- abdominal pain;
- dyspnea;
- lack of appetite;
- swelling of the ankles;
- portal hypertension, or increased pressure in the blood supplying the liver.
- For thrombophilia of cerebral vessels and stroke:
- headache;
- loss of consciousness;
- increased heart rate;
- neurological manifestations.
- For pulmonary artery or pulmonary infarction:
- feeling of fullness in the chest;
- suffocation;
- cough with bloody sputum;
- chest pain;
- shortness of breath appears;
- breathing is difficult.
- For thrombophilia of the lower extremities and varicose veins:
- heaviness in the legs;
- pain in the lower leg when walking;
- swelling of the legs.
- For thrombophilia of the intestinal mesenteric vessels:
- nausea;
- vomit;
- diarrhea;
- sharp cutting pain in the abdomen;
- tissue necrosis;
- gangrene;
- hemorrhagic diathesis - disorders of platelet, vascular, plasma synthesis.
Common to all hemorrhagic diathesis, regardless of their origin, are the syndrome of increased bleeding (recurrent, prolonged, intense bleeding, hemorrhages of various locations) and post-hemorrhagic anemic syndrome
When thromboembolism recurs, both genetic and acquired, pregnant women often turn not to a hematologist, but to their gynecologist with the confidence that they are suffering from late obstetric complications of pregnancy, namely those expected in the later stages of gestosis or VSD - vegetative-vascular dystonia:
- headache;
- hypertension;
- general weakness;
- loss of consciousness;
- increased fatigue;
- dyspnea;
- swelling of the upper and lower extremities;
- leg cramps;
- bluishness or redness of the skin;
- pain in the lower abdomen;
- uterine bleeding;
- toxicosis with vomiting.
What treatment is prescribed?
If the pathology is caused by genetic mutations, it is impossible to completely get rid of it. Therefore, the doctor selects individual replacement therapy, which includes drugs that replenish the missing blood clotting factors. Blood transfusions are also required periodically. If thrombophilia is acquired, in this case anticoagulants are prescribed, which are often used for drug therapy of thrombosis. These are medications such as:
- "Wafarin"
- "Courantil"
- "Pradaxa"
- "Heparin"
- "Dalteparin"
- "Enoxaparin"
- "Fraxiparin".
In addition to drug treatment, to prevent blood clots, you must regularly wear compression garments, which are selected together with your doctor. Thanks to constant compression of the limbs, it will be possible to unload the blood vessels and control intravenous pressure. In addition, it is recommended to attend massage courses, exercise, and walk in the fresh air.
Methods for diagnosing thrombophilia
First of all, it is necessary to donate blood to study hemostasis - this is a biological system in the body, the function of which is to maintain the liquid state of the blood, stop bleeding in case of damage to the walls of blood vessels and dissolve blood clots that have fulfilled their function. The main blood clotting factors are:
- F5—accelerin gene, Leiden mutation;
- F2 - prothrombin.
These genes are the most studied and it is known that their violation can lead to severe complications of pregnancy, for example, placental abruption at 25–26 weeks of pregnancy. Based on them, the hetero- or homozygosity of a woman is revealed, i.e. how damaged her genes are. Tests for these two markers are carried out first; you can donate blood for this even after a light breakfast. The turnaround time for analyzes is only two days. Such tests for gene polymorphism are taken only once in a lifetime; there is no need to retake them after treatment.
If necessary, additionally prescribed:
- study of the plasminogen activator gene - fibrin in the diagnosis of PAI-1 and blood coagulation factor XIII. It is known that inhibition of fibrinolysis often leads to disruption of the fetal implantation process. In this regard, a decrease in the fibrinolytic activity of this system is one of the reasons for early termination of pregnancy;
- platelet receptor genes; the presence of mutations in these genes leads to increased platelet aggregation and adhesion. Platelets are the first to appear at the site of the defect. They stick (adhere) to damaged endothelial cells, swell and form processes. Parallel to adhesion, the process of platelet aggregation occurs, swelling and gluing them together with the formation of processes and the imposition of aggregates on the site of vessel damage, as a result of which the hemostatic plug or thrombus quickly grows. Diagnosis of the following factors is necessary: FBG - fibrinogen gene;
- ITG A2—platelet integrin gene;
- ITG B3. Such patients are insensitive to aspirin and need chimes;
- F7—proconvertin gene;
- F13 - fibrin stabilizing factor gene.
- MTR—gene encoding the enzyme methionine synthase;
Based on the results of the analysis, the severity of the possible manifestation of thrombophilia is determined and recommendations for treatment are given, and sometimes the condition of the pregnant woman is simply monitored.
Table: diagnosis of thrombophilia based on laboratory diagnostic results
| Analysis name | What determines |
| General blood analysis |
|
| Coagulogram |
|
| Genetic markers of congenital thrombophilia: |
|
| Homocysteine |
|
How to monitor the condition of the fetus if there is an identified tendency to thrombosis
If thrombophilia is diagnosed in a pregnant woman, there will be more monitoring of the condition of the fetus and tests will be prescribed more often.
To monitor the development of the fetus and the safety of the placenta, it is necessary:
- In the first trimester:
- at 8–10 obstetric weeks - three-dimensional echography of uteroplacental blood flow;
- later ultrasound with Doppler, which reveals areas of reduced blood flow in the placenta.
- In the II and III trimesters:
- When checking ultrasound screening, the following is performed: Doppler ultrasound to measure the nature and speed of blood flow in the vessels;
- fetometry or measurements of the child in utero;
- cardiotocography to record fetal heart rate and uterine tone.
Does treatment lead to thrombosis?
The side effects of many medications manifest themselves in the development of a tendency in the blood to increase the formation of blood clots. For example, estrogen contraceptives and certain groups of cytostatics have similar qualities. Paradoxically, this list can be supplemented with heparin, which in some patients stimulates spontaneous adhesion of blood platelets (heparin thrombophilia with rebound thrombosis), and thrombolytics (in large doses), which deplete the plasmin system and enhance thrombus formation due to aggregation.
Thrombocytopenia that occurs on days 2-3 of heparin treatment is called early thrombocytopenia. The late one appears after approximately 1-1.5 weeks and is characterized by more pronounced symptoms (bleeding and thrombosis at the same time), reminiscent of thrombotic thrombocytopenic purpura.
To avoid undesirable consequences of such therapy, one should remember about prevention and the use of heparin and thrombolytics should be combined with antiplatelet agents (acetylsalicylic acid, ticlide, etc.). It is important to remember that when combining these drugs you cannot act blindly, so monitoring the aggregation and coagulogram must be mandatory.
Who needs to undergo genetic testing for a hereditary form of thrombophilia?
Genetic tests to diagnose hereditary thrombophilia identify genetic mutations that are important for thrombophilia.
First of all, such studies are prescribed:
- Women who are expected to use hormonal drugs for treatment, and those who are preparing for planned cesarean section operations;
- For women who have a burdened personal history in the past, when chromosomal, hormonal, infectious and uterine causes of miscarriage are excluded:
- with habitual miscarriage during various periods of pregnancy;
- with repeated complications of pregnancy: preeclampsia;
- abruptions of a normally located placenta;
- fetal growth retardation syndrome.
- unsuccessful IVF experience;
- tendency to minor bleeding (nasal, cervical).
- Women with a complicated family history of thrombosis:
- unclear causeless (idiopathic) thrombosis;
- in the family, close relatives have cases of early stroke, myocardial infarction, pulmonary embolism, sudden death before the age of 50;
- repeated episodes, especially in women under 50 years of age;
- thrombosis of rare localization (in the mesenteric vessels of the intestine, in the cerebral veins);
- complications from the use of oral contraceptives or hormone therapy;
- birth of children with chromosomal abnormalities.
Video: geneticist Z. Bayanovna about thrombophilia genes
Consequences
In order to assess the risks of pathology and select the right treatment, it is important to correctly understand what the consequences of hypercoagulation may be for the woman and the fetus.
For a child
Genetic thrombophilia during pregnancy poses a serious threat to the fetus - in this condition, blood clots appear in the initially intact vessels of the placenta, disrupting normal blood flow. The pathological process affects both arteries and veins, which significantly disrupts normal blood flow - what the changes look like is shown in the photo.
Thrombosis of placental vessels - consequences of thrombophilia for the fetus
The outcome of hypercoagulation is:
- spontaneous abortion (two or more episodes) - this condition is called recurrent miscarriage;
- frozen pregnancy;
- intrauterine hypoxia, manifested by delayed fetal development;
- discrepancy between the actual gestational age and the results of additional studies - the gestational age is determined incorrectly due to its small size;
- change in the volume of amniotic fluid - both oligohydramnios and polyhydramnios are detected;
- multiple fetal malformations;
- placental abruption (retroplacental hematoma);
- premature onset of labor.
In each case, the doctor must assess the risk of developing thrombophilia in such pathologies individually, and a set of examinations is prescribed to confirm the diagnosis. In this case, it is necessary to exclude the influence of other factors that cause these pathologies (STDs, TORCH infections, intrauterine infection of the fetus).
For woman
Pregnancy with thrombophilia has its own characteristics, because this condition has virtually no effect on conception, but interferes with pregnancy. The pathology most often manifests itself after the 8th week of pregnancy - it is at this period that the formation of the baby’s place and the placental circulation begins.
An imbalance of the blood coagulation and anticoagulation systems provokes conditions that affect both the course of pregnancy itself and the somatic status of the woman.
The first type of pathology includes gestosis in the second half of pregnancy (preeclampsia and eclampsia), manifested by:
- a sharp increase in blood pressure;
- proteinuria - protein excretion in the urine;
- pronounced swelling of the lower extremities, anterior abdominal wall, and face.
These changes can progress until the onset of labor, during labor, and in the early postpartum period. Symptoms disappear a few days after delivery, and a condition that did not cause serious disorders (cerebral hemorrhages, swelling, convulsions) disappears almost without a trace.
The second type of pathology includes diseases of internal organs that arise during pregnancy. These conditions may persist after delivery, requiring patients to continue treatment throughout their lives.
A striking example is thrombophlebitis of the legs during pregnancy, which causes the expectant mother great discomfort due to severe bursting pain and swelling in the legs.
In addition, inflammation of the veins is almost always accompanied by the formation of blood clots, and they can break away from the site of primary localization and migrate through the circulatory system, which can trigger the development of ischemic stroke, myocardial infarction (very rare), pulmonary embolism (pulmonary embolism), renal embolism, hepatic embolism , mesenteric veins.
Thrombophlebitis and childbirth during pregnancy pose a certain danger for a woman - during childbirth (during contractions), blood clots can break off and be transferred to other blood vessels. If the disease is detected in the late stages of pregnancy, a consultation with a vascular surgeon is necessary, based on the results of which the doctor must recommend the optimal delivery tactics.
In each case, the recommendations will be individual, but one piece of advice remains unchanged - both during vaginal delivery and during caesarean section, compression stockings are required (the limbs are bandaged with elastic bandages. Such preventive measures reduce the risk of thromboembolism many times over.
Treatment of thrombophilia during pregnancy
Detection of thrombophilia is not at all a sign that a woman will not be able to give birth. If you undergo all examinations on time and plan your pregnancy, there is every chance that the expectant mother will have healthy children.
Treatment started on time will contribute to successful placentation and reliable attachment of the embryo to the wall of the uterus. Compliance with anticoagulant treatment is indicated throughout pregnancy and for 6 weeks after delivery.
If therapy is started late in pregnancy, the woman has little chance of carrying the fetus to term without significant complications.
After conducting all the necessary studies, the doctor will prescribe the following to the woman:
- If the level of homocysteine is normal, then folic acid (vitamin B9) is prescribed in an increased dose throughout pregnancy and is not canceled when the term reaches 12 obstetric weeks:
- Folacin;
- Folio;
- Folic acid 9 months;
- Metafolin is an accessible form of folic acid that is absorbed by almost everyone, since its absorption does not require a long chemical process involving enzymes (as in the metabolism of regular folic acid). The ratio of those who absorb this vitamin and those whose bodies are insensitive to it is approximately the same. To check this, expensive and hard-to-find tests are needed.
- Vitamin complexes are prescribed:
- which contain polyunsaturated fatty acids: Femibion natalcare I;
- Angiovitis;
- Vitrum cardio omega - 3;
- Omegamama 9 months;
- Wessel due f.
- magnesium and B6 preparations, 1 tablet 2 times a day for 1 month:
- Magne B6 - forte;
- Magnelis B6.
- In some cases, the use of low molecular weight heparin (LMWH) - Clexane and its derivatives Dalteparin, Enoxaparin, Fraxiparin - is indicated as antithrombotic therapy:
- in the second trimester - doha increases to 60–80 mg/day due to a state of increased activity of the blood coagulation system with monitoring of the hemostasiogram and markers of thrombosis;
- heparin withdrawal is prescribed 4–5 days before the date of delivery. A fetal echocardiogram is monitored every three days. Three days after discontinuation, a hemostasiogram and fetal markers are also checked. With very intensive growth, urgent delivery is necessary to prevent the death of the mother. After all, thrombophilia — No. 1 cause of maternal mortality in the postpartum period.
Clexane (enoxparin sodium) is a low molecular weight heparin preparation for subcutaneous administration, which is available in disposable syringes of 0.2, 04, 0.6, 0.8 and 1 ml - Progesterone preparations:
- dydrogesterone - Duphaston;
Dydrogesterone in the composition of Duphaston is very close in its molecular structure, chemical and pharmacological properties to natural progesterone - natural progesterone - Utrozhestan or Prajisan.
The drugs Utrozhestan and Pradzhistan are analogues of Duphaston - Additionally, anticoagulants are prescribed to slow down blood clotting processes:
- Warfarin, which blocks the synthesis of vitamin K-dependent blood coagulation factors (II, VII, IX, X) in the liver, reduces their concentration in plasma;
- Pradaxa or thrombin inhibitor, which in turn is responsible for the process of converting fibrinogen into fibrin and the formation of a blood clot.
Video: obstetrician-gynecologist I. I. Tyan about congenital thrombophilia and pregnancy management tactics
Additional treatment options
Dietary nutrition is of particular importance for women after an accurate diagnosis is established - changing the diet cannot completely eliminate hypercoagulation, but helps reduce the dose of necessary medications.
Features of the diet for thrombophilia:
- The expectant mother should receive at least two liters of fluid per day. Correction of the drinking regime is required only in cases of severe preeclampsia and eclampsia.
- It is recommended to increase the amount of foods in your diet that are rich in folic acid and its metabolites - you need fresh greens, vegetables and fruits, seafood, cabbage, lettuce.
- Ginger and dried fruits (dried apricots, dried apples and pears, prunes) help thin the blood - they can be consumed independently or used to make tea, compotes, jelly.
- Chocolate of any kind, tea and coffee in any form, grapes are excluded from the diet - these products accelerate the excretion of folates from the body of a pregnant woman.
- Limit the consumption of foods that increase the concentration of homocysteine in the blood serum - eggs in any form, nuts regardless of type, dairy products (fresh milk, cheeses, cottage cheese).
Of course, thrombophilia, regardless of the type of pathology and its severity, significantly aggravates the prognosis of pregnancy. Timely comprehensive diagnosis and implementation of all doctor’s recommendations will help a woman suffering from hemostasis disorders to bear a fetus and give birth to a healthy baby.
Diet
All patients with an increased risk of thrombosis are prescribed an antithrombotic diet according to (J. Casper, 1973), food should be rich in folates and B vitamins:
- The proportion of such products that increase blood clotting is increasing:
- seafood;
- roots;
- berries - cranberries, lingonberries, grapes, viburnum, chokeberries, cherries, raspberries;
- dried fruits - figs, dates, prunes, dried apricots, raisins;
- seaweed;
- ginger;
- fresh grape juice;
- cranberry tea;
- natural tomato juice;
- lean meats and fish;
- whole wheat bread.
- Fatty and fried foods are excluded, since the lipids in their composition thicken the blood:
- fat meat;
- salo;
- legumes;
- hard varieties of cheese;
- full fat whole milk;
- leafy vegetables - spinach, celery, parsley.