Features of the pathology
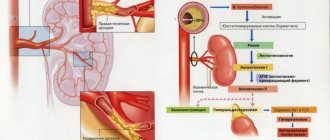
In most cases, cholesterol plaques are deposited near the mouth of the artery, or directly in it, which leads to the rapid development of complications associated with the functioning of the kidneys.
A potential concern for patients with renal artery atherosclerosis is that there is a high risk of progression to hypertension.
The larger the plaques in the kidneys, the worse the patient’s health will be and the higher the risk of complications.
Also, if a person who develops atherosclerosis of the renal arteries has severe heredity, diabetes mellitus or other concomitant blood or vascular diseases, then the risk of developing kidney failure increases significantly.
This pathology is chronic and develops over a long period of time, during which cholesterol deposits gradually accumulate on the vascular walls, which lead to degenerative changes in the structure of the artery walls and narrowing of the lumen for blood flow.
In advanced forms of atherosclerosis, plaques can calcify, increasing the risk of blood clot formation.
Fibromuscular dysplasia of the renal artery
Diet and nutrition
Maintaining a healthy diet is especially important. You will have to reduce the amount of fat you consume per day. However, it is impossible to completely stop their intake into the body, so many harmful animal fats are replaced with vegetable ones.
The diet must have a sufficient amount of minerals and vitamins, especially C and group B. Otherwise, you should adhere to all the principles inherent in a balanced diet. Diet is especially important for obese people, since they are faced with the task of losing weight. Normalizing its level will significantly help in the treatment of atherosclerosis of the renal arteries.
Stages
It is important to realize that this disease does not occur suddenly. The patient's condition worsens as the lumen of the vessel becomes more blocked. In some it may develop more slowly, while in others it may develop more quickly, depending on various factors.
However, for each of the people suffering from atherosclerosis, the pathology develops in several stages, shown in the table below.
| Stage | Description |
| 1 | The initial stage of disease development. The appearance of lipid stains is noted, but no symptoms appear at this stage. If there are several reasons that provoke atherosclerotic deposits, then the disease develops at a faster rate. |
| 2 | The number of lipid stains increases significantly, which leads to the formation of a fibrous plaque. First, the spots that appear become inflamed, accumulating many immune complexes around them. Reacting with the inflammatory process, they disintegrate and decompose into fats, which begin to become overgrown with connective tissue. This process leads to thickening of the plaque and significant disruption of blood flow. |
| 3 | The extreme and most severe stage, characterized by the progression of serious complications caused by atherosclerosis. Quite often, this stage is called atherocalcinosis, since deposits of calcium salts begin in the cholesterol plaque. The blood flow is severely disrupted, up to the complete closure of the lumen of the vessel. As a result of severe circulatory impairment, gradual tissue death develops, which can lead to death. |
Causes of atherosclerosis of the renal arteries
Age plays an important role in the progression of the disease. Thus, people over 45 years of age are more susceptible to the formation of atherosclerotic deposits in the arteries of the kidneys.
According to statistics, men are more at risk of developing pathology than women of the same age.
The main factor provoking the development of this disease is a violation of lipid metabolism.
In a healthy body, cholesterol and lipoproteins are balanced, but with atherosclerosis, the amount of cholesterol exceeds the norm, which provokes their deposits on the walls of blood vessels.
Renal atherosclerosis develops after cholesterol plaques from the aorta enter the renal arteries.
The main reasons that cause atherosclerotic processes are:
- Congenital kidney pathologies;
- Hypodynamics - a sedentary lifestyle and lack of mobility slows down blood flow and increases the amount of cholesterol in the blood;
- Poor nutrition – consumption of more fatty and smoked foods, fast food, sweet carbonated water, etc.;
- Cigarette smokers have an increased risk of high blood pressure, which can directly affect the development of atherosclerotic disease. In addition, smoking leads to oxygen deficiency in the blood, which can lead to hypoxia of organs and tissues;
- Inflammatory processes developing in the kidney area;
- Hypertension - vascular walls are intensively saturated with fats at high blood pressure. However, quite a lot of atherosclerosis provokes the appearance of hypertension;
- Nephrotic syndrome;
- Diabetes mellitus significantly disrupts the body’s metabolic processes, increasing the risk of atherosclerotic deposits by 7 times;
- Obesity - with this condition of the body, there is a significant concentration of cholesterol in the blood, which leads to its accelerated accumulation on the walls of blood vessels;
- Infectious diseases - the most dangerous are chlamydia and cytomegalovirus;
- Endocrinological diseases that provoke a decrease in the production of sex hormones;
- Impaired fat metabolism - can be provoked by various diseases or causes, but significantly increases the risk of atherosclerosis of the renal arteries and other vessels;
- Hereditary predisposition;
- Cholelithiasis.
Cholelithiasis
Symptoms
At the first stage, it is practically impossible to determine the disease by the patient’s well-being, since there are no symptoms. However, the formation of lipid stains can be detected during examination.
Active manifestation of signs of damage to the renal arteries by cholesterol plaques occurs in the second stage of the disease.
The following symptoms are typical:
- Increased blood pressure, which is provoked by narrowing of the vessel by atherosclerotic deposits, disruption of blood flow, oxygen starvation of organs and tissues, as well as increased production of renin (a hormone responsible for the speed of blood circulation);
- The appearance of protein in the urine and its darkening;
- Feeling of constant weakness;
- Nausea and gag reflexes;
- Itching of the skin surface;
- Pain in the abdominal cavity and back. The main difference between such pains and renal colic is that they do not radiate to the groin area;
- Possible increased body temperature;
- The appearance of edema;
- Decreased vision;
- Sharp pain in the chest caused by insufficient blood supply to the heart;
- Severe headaches;
- Violation of the functional functioning of the kidneys with the subsequent development of kidney failure;
- Disorders in sleep patterns.
The development of atherosclerosis of the renal arteries can be accompanied by one of the above symptoms, or several at once. It all depends on the individual indicators of the body and the presence of additional diseases that are stored in the patient’s medical history.
If one of the above symptoms is detected, you must go to the hospital for examination.
Previously detected diseases will allow you to avoid surgical intervention and eliminate cholesterol plaques much faster and easier.
Sleep disorders
Diagnosis and treatment of bradycardia during pregnancy
Bradycardia is one of the types of arrhythmia, which is characterized by a decrease in heart rate. Normally, heart rate varies from 60-80 beats per minute at rest to 120-140 with significant physical activity. Conditions in which the heart rate is below 60 beats per minute are classified as different degrees of bradycardia.
During sleep or when the ambient temperature drops, the heart works in an economical mode, and physiological bradycardia is observed. A reduced heart rate, which is recorded in athletes and people with heavy physical labor, is also physiologically determined and does not pose a health hazard. Pathological bradycardia is said to occur if changes in heart rate are caused by other diseases, perhaps not accompanied by direct damage to the cardiovascular system. In such cases, abnormal heart rhythm is one of the nonspecific symptoms of the pathological condition. Bradycardia in pregnant women is relatively rare.
In cardiological practice, there are three degrees of heart rate slowing. At a heart rate of 50-60 beats per minute, a mild degree of bradycardia is stated, 40-50 beats per minute are classified as moderate bradycardia. A decrease in heart rate to less than 40 beats per minute is called severe bradycardia, which is potentially dangerous.
Bradycardia of any degree in a single case can be considered as a variant of the individual norm, if the abnormal heart rhythm is not accompanied by hemodynamic disturbances and does not affect the patient’s well-being.
Bradycardia during pregnancy
During pregnancy, the load on the cardiovascular system of the expectant mother increases greatly and differs from usual. Blood flow is hampered due to the occurrence of a fetoplacental circulation, an increase in blood volume and due to mechanical compression of some vessels. As a rule, the heart rate during pregnancy accelerates somewhat, and compensatory tachycardia develops. A slowdown in heart rate during pregnancy indirectly indicates possible disturbances in the functioning of the body.
Based on the location of disturbances in the conduction system of the heart, sinus bradycardia and bradycardia due to sinoatrial or atrioventricular heart block are distinguished.
Pathological bradycardia often accompanies various diseases. Depending on the characteristics of the underlying disease, cardiac and non-cardiac causes of heart rhythm disturbances are distinguished. The group of cardiac causes includes:
Among the non-cardiac causes of bradycardia during pregnancy, the following should be noted:
- Some types of injuries;
- Hypothyroidism;
- Infectious diseases of various etiologies;
- Disturbances in the electrolyte composition of the blood;
- Diseases of the digestive system, in particular peptic ulcers and tumor processes;
- Severe poisoning;
- Some kidney pathologies.
Clinical manifestations of bradycardia
Mild and moderate bradycardia in pregnant women is often asymptomatic. Since bradycardia, like tachycardia, in most cases is part of symptom complexes characteristic of the course of diseases of other organs and systems, its manifestations depend on the specifics of the underlying pathology. An abnormally low heart rate may be indicated by:
- Increased fatigue and chronic fatigue;
- Difficulty breathing;
- Increased sweating;
- Disorders of memory and attention processes;
- Short-term visual impairment;
- Feeling of vague discomfort or pressure in the chest;
- Dizziness, fainting, loss of consciousness.
- "Floaters" before the eyes.
Being a nonspecific symptom of a number of diseases, bradycardia provokes the same nonspecific changes in condition, some of which can be taken as a consequence of hormonal changes in the body.
The danger is posed by cases of severe bradycardia, when the heart rate is less than 40 beats per minute. A sudden decrease in heart rate can be accompanied by the development of a potentially fatal condition known as Morgagni-Adams-Stokes syndrome. It is characterized by the following symptoms:
- Severe anxiety, panic attack;
- Hyperemia of the facial skin;
- Breathing disorders;
- Dizziness, deep fainting;
- Swelling of the neck veins;
- Cyanosis of lips;
- Pupil dilation;
- Involuntary muscle contractions, severe cramps;
- Urinary incontinence.
The heart rate may recover after a few seconds; when the woman comes to, she does not remember what happened. However, an attack of bradycardia, accompanied by convulsions and prolonged (more than a minute) fainting, is potentially life-threatening for the mother. In such cases, you must immediately call an ambulance. Morgagni-Adams-Stokes syndrome is an emergency condition, the patient must be immediately hospitalized in the intensive care unit.
Sinus forms of bradycardia
In cases of congenital reduced automatism of the sinus node, bradycardia is a common condition for women and does not in any way affect the course of pregnancy. As a variant of the norm, cases of bradycardia are considered in women who, before pregnancy, were actively involved in sports or heavy physical labor.
If bradycardia is a symptom of concomitant pathologies, the pregnant woman should be under the supervision of a cardiologist. Sometimes a specific type of bradycardia occurs, provoked by fetal growth. A slow heart rate can be caused by constant irritation or compression of the branches of the vagus nerve by the enlarging uterus. Sinus forms of bradycardia, as a rule, are not dangerous for either the mother or the fetus, and are not grounds for termination of pregnancy.
Heart block as a cause of bradycardia
In some cases, bradycardia during pregnancy is a consequence of dysfunction of the cardiac conduction system. In case of conduction disturbances between the sinus node and the atrium, sinoauricular block is detected. Sinoauricular block occurs against the background of cardiac pathologies of various origins. The easiest way to relieve an attack of weakness or dizziness caused by a decrease in heart rate is by drinking a cup of fresh leaf tea, preferably with a small piece of dark chocolate.
Another type of heart block is atrioventricular, when the transmission of impulses between the atrium and ventricles is disrupted. With bradycardia of atrioventricular origin, the pulse is rare, the rhythm of contractions of the atria and ventricles is uncoordinated. The attacks are accompanied by general weakness, dizziness, and fainting. Oxygen starvation of the brain can provoke a Morgagni-Adams-Stokes attack.
Diagnosis and treatment
Persistent bradycardia, accompanied by attacks of weakness or other clinical manifestations, is a reason for a more thorough examination of the pregnant woman’s health. As a rule, heart rhythm disturbances resulting from diseases of the cardiovascular system are potentially dangerous. In such cases, a plan for managing pregnancy and childbirth is developed individually; the expectant mother will visit the doctor more often for a routine examination. Monitoring by a cardiologist is required, and, if necessary, additional hardware and laboratory tests to make a diagnosis.
The fetal heartbeat is monitored at every visit to the antenatal clinic. If a pregnant woman shows signs of arrhythmia of any type, monitoring is carried out more carefully. If signs of bradycardia are detected on fetal CTG, the doctor refers the pregnant woman to a Doppler study. After the examination, treatment is prescribed to correct the identified problems.
In most cases, bradycardia during pregnancy does not require treatment.
Source: holesterin-lechenie.ru
Complications
Failure to see a doctor in a timely manner or ineffective treatment can lead to the progression of serious complications, which are listed in the table below.
| Name | Description |
| Vasorenal hypertension | A secondary form of the disease, which developed due to ischemia of the kidney with a large amount of secreted renin. This form of hypertension is difficult to treat, even with the most modern medications. The disease progresses rapidly and can lead to the death of heart muscle tissue or a stroke. |
| Renal artery aneurysm | An enlargement of a separate section of the vessel, provoked by cholesterol deposits and inflammatory processes, which disrupts the structure of the wall. When an aneurysm ruptures, sharp pain occurs in the side or back, pale skin appears, the number of heartbeats increases, blood pressure decreases, and the victim loses consciousness. |
| There is internal bleeding, which in 70% of cases leads to death before hospitalization. Salvation lies only in urgent surgery. | |
| Kidney failure | Narrowing of the artery lumen, which impairs blood circulation, can lead to the development of kidney failure. This pathology leads to loss of kidney functionality - stopping urine output, which disrupts the water-salt balance. Kidney failure without immediate medical intervention can be fatal. |
Diagnosis of atherosclerosis of the renal arteries
Initially, the doctor admits the patient, conducts an initial examination, examines the medical history and prescribes various tests. It is important to realize that indicators from laboratory tests alone will not be enough to make a diagnosis.
To make a final decision on the disease, you will need to undergo some hardware tests, the main ones of which are shown in the table below.
| Variety | Description |
| Ultrasound examination (ultrasound) | It is the most common method for examining the kidneys, adjacent arteries and vessels. Its main advantage is that it does not irradiate the body and has no contraindications. Allows you to determine the degree of blockage of the artery lumen, as well as structural disorders of the kidneys and vessel walls. |
| Magnetic resonance imaging (MRI) | It is the most accurate and expensive research method. Determines the speed of blood flow in the artery, the degree of its damage, the nature of the formation, etc. |
| Echocardiography (EchoCG) | Used to determine functional disorders in the heart and adjacent vessels. |
| Angiography | The patient is injected with a contrast agent and an MRI or X-ray is taken to determine abnormalities in the blood vessels. |
| Dopplerography | A type of ultrasound examination that determines the speed of blood flow in the vessels. |
The final diagnosis is made only by the attending physician based on the studies performed.
Diagnostic methods
Confirmation or refutation of the diagnosis is done after a series of procedures, including urine and blood tests.
Renal atherosclerosis can be suspected based on the clinical signs present in the patient and after a general examination.
To confirm this diagnosis, an ultrasound with Doppler ultrasound of the vessels is performed. Using this method, atherosclerotic plaques and impaired blood flow can be visualized. MRI with angiography is also performed, which is the illumination of blood vessels. OAM and UAC, determination of cholesterol content are indicated.
Treatment
To achieve maximum effect, complex treatment is used, which requires not only the use of effectively selected therapy, but also adherence to a low-cholesterol diet, as well as an active lifestyle.
The main goals of therapeutic treatment are:
- Reducing the total cholesterol level in the patient’s body;
- Improving metabolic processes for accelerated removal from the body;
- Reducing the risk of progression of thrombosis and embolism;
- Improving the elasticity and tone of the walls of blood vessels;
- Restoring kidney function and urine excretion from the body.
It is important to understand that if atherosclerosis of the renal arteries is seriously neglected, medications cannot be used; prompt surgical intervention will be required.
The main methods of treating this disease are given in the table below.
| Medication | Surgical |
| · Statins – lower blood cholesterol levels; | · Endovascular method - a special needle is inserted through the femoral artery, which, reaching the point where the vessel is blocked, expands, leaving a special stent at the site of narrowing; |
| · Fibrates – reduce the synthesis of cholesterol by the body; | · Endarterectomy is an open surgical procedure in which the cholesterol plaque is simply removed and the incision site is stitched; |
| · Nicotinic acid – reduces the level of triglycerides, low-density lipoproteins (LDL) and cholesterol; | · Bypass surgery is an operation performed under general anesthesia, in which a bypass path is built from artificial materials, bypassing the cholesterol plaque. |
| · Sequestrants – required to accelerate the processes of removing cholesterol and bile acids; | |
| · Antihypertensive drugs – lower blood pressure, which relieves stress on the walls of blood vessels and reduces the risk of further development of atherosclerosis of the renal arteries. |
Self-medication, especially with folk remedies, can lead to serious complications.
Consult a qualified physician for diagnosis and treatment options.
Diagnostic procedures
To establish a diagnosis, it is necessary to visit a therapist, who, first of all, visually examines the patient, measures his blood pressure and BMI, and collects an anamnesis. Then the patient is sent for laboratory tests:
- Complete blood count (OAK);
- Blood chemistry;
- Urinalysis (OAM).
To identify atherosclerosis of the kidneys, the following examination methods are used:
- Dopplerography;
- Ultrasound examination (ultrasound) of the kidneys;
- Magnetic resonance imaging (MRT);
- Renal angiography and scintigraphy.
A complete diagnosis will help the attending physician establish an accurate diagnosis and prescribe appropriate treatment.
Prevention
Precautionary measures that will help avoid this disease are similar to the general prevention of atherosclerosis.
The main goal of such measures is to maintain a normal balance of cholesterol in the blood, as well as normalize metabolic processes.
It is recommended to adhere to the following lifestyle:
- Balanced diet (with acceptable cholesterol levels);
- Maintaining water balance (drink at least 1.5 liters of clean water per day);
- Avoid alcohol and nicotine;
- Moderate physical activity - it is recommended to walk at least 3 km a day, as well as engage in active sports (swimming, football, running, athletics, etc.).
What is your life prognosis?
With timely treatment of the pathology in the early stages, the outcome will be favorable, since this disease responds well to treatment if it is selected correctly.
If the vessel is seriously blocked, urgent surgical intervention will be required, which will help avoid complications and even save lives.
Self-medication or failure to see a doctor in a timely manner will lead to the progression of additional diseases that can lead to death or disability.
What are the risks of kidney atherosclerosis?
If cholesterol deposits form on the walls of the renal arteries, blood flow is disrupted and causes the development of hypertension, more precisely, symptomatic vasorenal hypertension. This pathology is difficult to treat, despite the qualifications of modern doctors and the availability of effective remedies of the latest generations. Long-term high blood pressure can lead to heart attack or stroke. And prolonged ischemia (insufficient blood circulation) leads to renal failure and ultimately complete kidney failure.
Considering all the complications listed above, it is necessary to treat atherosclerosis of the kidneys only in a comprehensive manner. If you start treatment in the early stages of the disease, you can protect your kidneys without surgery, and also prevent a heart attack or stroke.
Complex therapy of atherosclerosis consists of the following measures:
- Adjusting the patient’s diet and lifestyle.
- Taking medications to help lower cholesterol.
- If vasorenal hypertension is detected, then a decrease in blood pressure.
- In severe forms of the disease, surgery is performed to restore blood flow in the vessels of the kidneys.
Whether conservative methods of treating atherosclerosis will be sufficient or whether there is a need for surgery can only be determined by a doctor after examining the patient, studying the medical history and test results.