The difference between the upper and lower pressure, which normally does not exceed 50 units and does not fall below 30, is called the pulse pressure. This is a kind of marker of the preservation of the function of the heart and blood vessels. Let's take a closer look at what this bioindicator means, when it becomes dangerous for the patient, and how it is corrected.
Deviations in indicators
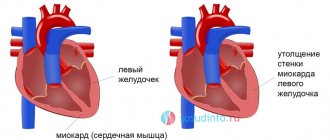
The heart is a four-chamber pump that pumps biological fluid enriched with oxygen to the periphery. Its work is recorded in several quantities. The upper one is a bioindicator of myocardial contractile potential. Bottom – components of the blood supply system.
Systolic pressure
Its ideal values are considered to be 120 units, the acceptable norm is 130, excess is 140, minimal hypertension is up to 170, high blood pressure is from 180. Any fluctuations in the indicator indicate an imbalance in the work of the myocardium.
Provoking moments of lowering the upper level are:
- overstrain: physical, mental;
- pregnancy;
- bradycardia of any origin;
- head bruises;
- insomnia;
- incorrect insulin production;
- imbalance of the heart valve apparatus.
Some triggers are physiological in nature. Indicators of the indicator of myocardial contractility are normalized without additional effort when the cause that caused their decrease is eliminated. An example is pregnancy, associated with a restructuring of the blood supply, when the upper level of pressure drops by approximately 10 units due to adaptation to the new conditions of the body’s existence. After childbirth, everything falls into place.
Athletes, through regular training, acquire the ability to work, saving energy during high loads, which automatically reduces the heart rate, causing a decrease in systolic blood pressure. The rest period normalizes myocardial contractions.
Pathological bradycardia or slow heart rate is characteristic of heart disease and atherosclerosis. It warns of the possible development of acute cerebrovascular accident - stroke or acute myocardial infarction - AMI.
Diabetes mellitus provokes blood hyperviscosity, which reduces the upper limit. Regardless of the reason that caused the decrease in pressure, the patient feels:
- apathy, drowsiness;
- hyperhidrosis;
- migraine pain;
- pre-fainting states;
- forgetfulness, irritability.
All this is a reason to seek medical advice. The question is extremely important, since often fluctuations in blood pressure occur with virtually no symptoms. AMI and stroke develop against the background of apparent well-being. Therefore, medical examinations or preventive examinations at least once a year are normal practice for patients who care about their health. Only a doctor can give a correct assessment of the condition of the heart and blood vessels; he also prescribes additional examinations if necessary and corrects the pathology.
Causes of increased systolic pressure:
- diseases of the cardiovascular system;
- nervous tension;
- alcohol abuse, nicotine addiction;
- physical inactivity, obesity;
- aortic defects;
- high cholesterol with the formation of atherosclerotic plaques;
- pathology of the kidneys, thyroid gland;
- age.
Clinically, a high upper bioindicator is manifested by nausea, nervousness, insomnia, ringing in the ears, constant palpitations, swelling of the legs, and loss of sensitivity in the fingers. Such symptoms should force the patient to seek medical help.
Diastolic pressure
The rest period of the myocardium is diastole. This is an indicator of capillary strength. Its optimal value is considered to be 80 units, the acceptable norm is 90, elevated is 95, mini-hypertension is 110, high is everything above 110.
A low diastolic limit requires diagnosing the functional integrity of the kidneys. In addition, it correlates with menstruation in women: blood loss leads to a minimization of its volume, that is, a decrease in the indicator. The following are considered triggers for low blood pressure: prolonged fasting, sensitization of the body, infection with Koch's bacillus, stressful situations, climate change.
Signs of low diastolic pressure:
- fainting;
- a sharp decrease in working capacity;
- dyspnea;
- chest pain;
- visual disturbances;
- cardiopalmus;
- vomiting - up to hypotonic crisis, coma.
An increase in the diastolic biomarker confirms the preservation of the tone of the peripheral capillaries due to the thickening of their membrane, narrowing of the lumen - the main trigger of hypertension. The diagnosis of the disease is made on the basis of long-term blood pressure values greater than 140/90. The causes of the pathology are recognized:
- heredity;
- alcoholism, nicotine addiction;
- gaining extra pounds;
- diuretics;
- osteochondrosis, other pathologies of the spinal column;
- depression.
Fluctuations in blood pressure are a sufficient reason for complete clinical and laboratory testing. Self-medication is unacceptable, as it can provoke complications leading to death.
Upper and lower pressure
Taking blood pressure measurements during an examination by a doctor is a mandatory measure that makes it possible to determine the condition of the body. Two main indicators are taken into account:
- Systolic pressure - makes it possible to determine the force of blood expulsion during the contraction of the heart.
- Diastolic pressure - shows the strength of relaxation between heartbeats.
The upper threshold depends on the general condition of the myocardium and the strength of the heart, but the lower threshold is directly related to the tone of all blood vessels and the volume of circulating blood. The resulting difference between the two digital data is the pulse pressure.
A certain gap in values indicates the following:
- The functioning of blood vessels during heartbeats and its relaxation.
- Patency of the vascular system.
- Tone and elasticity.
- Presence of spasms.
- Possible inflammatory processes.
There are norms and deviations from them in any direction, due to which the doctor can determine the causes of the pathological condition, prescribe the necessary examination and correct treatment.
Little difference
The standard difference is 40 units. Over time, the systolic limit shows a tendency to increase. Therefore, after 50 years, the norm reaches 50 mm Hg. Art. Taking into account individual fluctuations, pulse pressure indicators range from 30 to 50 units. Anything below 30 indicates trouble in the condition of the heart and blood vessels, and warns of a possible heart attack or stroke.
A difference of 20 units indicates chronic fatigue or renal pathology. If the interval is smaller, this is a sign of renovascular hypertension due to narrowing of the lumen of the renal artery.
What to do if pulse pressure is low
First of all, you should not self-medicate. The pathology is serious enough to seek medical help as soon as possible to determine the cause.
If the examination results do not reveal any serious diseases that could cause low pulse pressure, the condition is corrected by changing lifestyle in a healthy direction. Such patients are advised to eat a balanced diet, give up bad habits, spend more time in the fresh air, get rid of physical inactivity, take a short break after every hour of work, monitor the condition of the cervical spine, and be sure to get enough sleep. The minimum duration of sleep should be 8 hours.
In the event that the cause of a small difference between systolic and diastolic pressure is determined, treatment consists of eliminating the causative factor.
So, with atherosclerotic damage to blood vessels, the patient needs to take drugs that reduce cholesterol levels in the blood; vitamin therapy and unsaturated fatty acids may be prescribed.
Low pulse pressure is manifested by deterioration of well-being
In the case of chronic inflammatory diseases of the urinary system, anti-inflammatory, antibacterial drugs, and physiotherapeutic procedures are prescribed.
For chronic left ventricular failure, angiotensin-converting enzyme inhibitors, diuretics, and cardiac glycosides are indicated. In some cases, surgery is required. In the acute form of the disease, diuretics, glycosides, and ganglion blockers are used.
Normally, the gap between systolic and diastolic pressure should be 40 mmHg. Art.
For coronary heart disease, surgical treatment may be required - bypass surgery, stenting, laser angioplasty, etc.
For aneurysms, surgical intervention is necessary.
For constrictive pericarditis, pericardiectomy is performed.
If the pathology is caused by aortic valve stenosis, it is replaced with an artificial one.
In case of severe heart rhythm disturbances, antiarrhythmic drugs are prescribed, and if they are ineffective, implantation of a cardioverter-defibrillator is indicated.
If the patient has neoplasms, both conservative and surgical treatment can be performed.
A big difference
A high difference is considered to be more than 50. It correlates with the upper limit, the diastolic remains unchanged. This condition is called isolated systolic hypertension. It is precisely this that is stopped by practicing cardiologists and therapists. ISH cannot be treated radically, but requires constant monitoring of blood pressure and stopping fluctuations. It raises concerns because it warns of the risk of stroke, AMI with a practically asymptomatic course.
A difference of 60, 70, 80 units a priori suggests medical assistance. This indicates a significant overstrain of the myocardium and blood vessels, and the risk of spontaneous failures.
Diastolic pressure: what is it and what is it responsible for?
Diastolic pressure
- Diastolic blood pressure (we call it lower) is the force of blood pressure on the walls of the arteries at the moment when the heart muscle completely relaxes after contracting. In addition, this indicator helps us find out with what force blood circulates through our veins and arteries. In a completely healthy person, this figure can range from 65 to 80 units. Such a large difference in indicators is due to the general condition of the body. If its vessels are sufficiently elastic and have good tone, then, as a rule, diastolic pressure indicators remain at around 75-80 units.
- If the vessels are damaged, the blood flow is disrupted and the indicators begin to jump in one direction or another. Also, blood pressure indicators are greatly influenced by the frequency of contraction of the heart muscle and the amount of blood that the heart pumps. But even if you notice that your diastolic pressure has begun to drop or rise significantly, there is no need to sound the alarm right away. This indicator can be affected by stress, nervous disorders, hypothermia and even sudden temperature changes. Therefore, if they deviate from the norm by literally a few units, then just try to get more rest.
- If you see that your blood pressure readings have jumped or dropped by 10-15 units, then this is a reason to consult a specialist. As a rule, deviations in one direction or another occur due to the fact that the strength of the blood flow decreases or, conversely, increases. And if this process is not stabilized in the shortest possible time, then after some time the body will stop receiving the required amount of oxygen and, as a result, various health problems will begin.
Why is the pulse difference dangerous?
Deviations from generally accepted values are associated with somatic diseases. An incorrect difference between pressure indicators, in addition to AMI, stroke, provokes:
- heart failure of varying severity;
- pulmonary edema;
- risk of tuberculosis infection;
- pathology of the digestive tube;
- encephalopathy;
- musculoskeletal disorders;
- imbalance of visual function;
- myocardial damage;
- pathology of the kidneys and hearing organs.
The complications of dangerous pulse differences are difficult to manage. Sometimes they lead to death. Therefore, constant monitoring of blood pressure is an urgent need. It is especially difficult when the numbers of the systolic and diastolic indicators are the same. This prevents the circulation of biological fluid throughout the body, the myocardium stops contracting, shrinking beyond measure.
The only way out is to call an ambulance. Before her arrival, if the numbers of the lower - upper marker are high, you should take diuretics and drugs that slow down the rhythm. If your blood pressure is low, you need to take painkillers and drink a glass of strong sweet tea.
Symptoms
The clinical picture with a small difference between the upper and lower pressure is as follows:
- Headache.
- Attention disturbance.
- Failure to coordinate movements.
- General weakness.
- Blurred consciousness.
- Fainting.
- Trembling in hands.
Memory impairment is one of the signs of a small difference between pressure
With a large indicator, manifestations such as:
- Headache.
- Attacks of dizziness.
- Weakness.
- Irritability.
- Loss of consciousness.
- Pain in the chest area.
In addition to the symptoms that manifest themselves with low or high blood pressure, the patient may also be concerned about signs of pathologies that cause blood pressure deviations. For example, if a patient has kidney disease, symptoms such as pain in the lower back, urinary retention, nausea, and increased body temperature will be alarming.
What causes the pathological condition?
A decrease in the pulse difference is accompanied by an increase in the diastolic value or a decrease in the systolic value. Sometimes this occurs simultaneously. The triggers for this difference are the following somatic diseases:
- lipid metabolism disorders, pancreatic dysfunction;
- hypertension of any degree;
- cholesterolemia leading to vascular stenosis;
- imbalance of cerebral blood flow;
- kidney pathology;
- arrhythmias of various origins;
- aortic stenosis;
- myo-, pericarditis, myocardiopathy;
- left ventricular failure;
- tumors of the urinary system;
- neoplasms in the adrenal glands;
- Iron-deficiency anemia;
- aortic aneurysm;
- cardiogenic shock;
- hypocaloric diets, dehydration, hypothermia.
Age is a cause of isolated systolic hypertension or IHS. Over time, the layer of muscles in the vessels, which is responsible for their elasticity and lumen, becomes thinner. Against this background, plaques of calcium, blood clots, and cholesterol form. Arteries demonstrate fragility and respond inadequately to fluctuations in biomarkers. As kidney nephrons age, they lose their main function and stop regulating blood pressure.
The myocardial receptors that correct the response of the arteries to the systolic ejection of blood are subject to destruction. At the same time, the oxygen supply to the centers responsible for vascular tone deteriorates; they lose the ability to balance it. All this distinguishes patients over 60 suffering from age-related hypertension.
Reasons for deviations
The shift of the interval between the upper and lower values up or down depends on various factors. The following are the main reasons for deviations in the difference in systolic and diastolic pressure from the norm.
Low pulse pressure
In a healthy person, the impulse produced by contraction of the heart muscle meets adequate vascular resistance. A weak response may be due to their lack of elasticity, possible spasms, and various circulatory disorders.
First, it is worth listing the physiological causes of low blood pressure.
1. Age factor. In older people, the volume of blood ejected by the heart decreases, at the same time, the walls of the blood vessels become rigid and cannot cope with the pressure of the blood flow.
2. Heredity. Low pulse pressure is often observed in those whose close relatives are susceptible to hypotension or suffer from neurocirculatory dystonia. Congenital low elasticity of vascular walls and their high tone can provoke the development of pathology.
3. Physiological factors. The difference between diastole and systole decreases as a result of sudden hypothermia or prolonged exposure to a stuffy environment. A decrease in pulse pressure is provoked by emotional stress, heavy physical labor, as well as improper treatment of hypertension (when the upper blood pressure “goes astray” and the lower one does not change). Another factor that reduces pulse pressure is pregnancy.
More dangerous and more difficult to eliminate are the pathological causes of a decrease in the gap between the upper and lower pressure. These are mainly serious diseases or traumatic lesions of the circulatory system.
- Anemia. The common name for this disease is anemia because it is characterized by low production of red blood cells (erythrocytes). Anemia often results from a decrease in hemoglobin levels. With anemia, the heart works overload to prevent hypoxia in tissues and organs, but the myocardium also suffers from a lack of oxygen and cannot support the volume of injected blood. As a result, the systolic reading decreases.
- Kidney pathologies. Regulatory functions to maintain normal blood pressure are performed by the hormone renin, which is produced by the glomeruli of the kidneys. When inflammation begins in the urinary system, renin production increases sharply, causing a rise in diastolic pressure and a decrease in pulse pressure. In this way, the lack of oxygen in the kidney tissue during acute inflammatory diseases is compensated.
- Cardiogenic shock. This is a pronounced heart failure that occurs during myocardial infarction, as a complication after poisoning or myocarditis (inflammation of the heart muscle). With cardiogenic shock, the muscle tissue of the left ventricle is affected - as a result, its contractility deteriorates. The upper pressure drops, but the lower pressure remains almost unchanged - therefore the difference between them decreases.
- Hypovolemic shock. An acute pathology characterized by a sharp decrease in the total amount of blood in the body. Most often, the process develops as a result of severe infections or poisoning (due to vomiting or diarrhea). Sometimes blood loss is associated with internal or external bleeding.
A fairly common cause of low blood pressure is vegetative-vascular (neurocirculatory) dystonia. This is a complex of symptoms, which include disturbances in the conduction of neurons or insufficient contractile function of the heart muscle. In this case, systole can simultaneously decrease and diastole increase, as a result of which they are separated from each other by only 10-25 units.
High pulse pressure
A large difference between the upper and lower blood pressure is usually explained by a drop in diastolic pressure for the following reasons:
- due to age-related decrease in the elasticity of the walls of blood vessels;
- sometimes vascular laxity develops with a lack of renin production due to tumor formations in the adrenal glands;
- with pathologies of the thyroid gland - if its hormones are produced less than normal, many organs and most systems suffer (including the heart and blood vessels);
- as a result of dysfunction of the gastrointestinal tract, gall bladder and ducts;
- for tuberculosis;
- with atherosclerosis.
Advice: In order not to miss the onset of pathological processes in the body, it is worth taking regular blood pressure measurements as a rule - at least twice a week. This should be done sitting or lying down, in a relaxed state, without talking or moving during the procedure.
Clinical manifestations
With a pathology of pulse difference, which is provoked by somatics, the patient complains of:
- fatigue;
- mood instability;
- forgetfulness, lack of concentration;
- constant pre-fainting state;
- bluishness of the skin.
In case of cardioshock, the symptoms are different:
- pale dermis, mucous membranes;
- profuse sweat;
- fainting;
- dyspnea.
Isolated systolic hypertension is sluggish, almost asymptomatic, but is characterized by:
- ringing in the ears;
- fainting;
- incoordination;
- emotional lability;
- arrhythmia.
The mild course of the disease spontaneously gives way to a crisis when physical inactivity, diabetes, myocardial dystrophy, kidney pathology, AMI, and a history of stroke predominate.
Stress and low pressure difference
The small gap between the two values can be explained by significant psycho-emotional stress. Under stress, changes in the functioning of the cardiovascular system are inevitable. If you experience it briefly, there is no danger. But chronic stress is a serious risk.
It is worth talking a little about the pathogenetic patterns of stress. The stressful situation (or stressor) itself is assessed by the GM cortex as a threat. Excitation along the neural circuit goes to the hypothalamus and pituitary gland. In response to this, pituitary cells synthesize adrenocorticotropic hormone. It, in turn, stimulates the adrenal cortex. And they already massively release adrenaline and cortisol into the biofluid, which should serve as adaptation structures. This, figuratively speaking, is done to adjust the body to stress.
But it’s one thing when hormones are present in the blood for a short time, and quite another thing if the body remains under their influence for a long time and often. He may be sensitive to these hormones, they may be produced in excess quantities, and this is already fraught with somatic pathologies.
Our emotions activate the autonomic nervous system, its sympathetic department. This is an important natural mechanism, the task of which is to make the body as resilient as possible for a certain short period.
That is, for example, if you are in danger and need to run, the reaction of the nervous system, the hormonal release makes us faster and stronger. Many people cannot even believe that, under stress, they covered a certain distance so quickly or were able to do something that required serious physical effort.
But if the autonomic nervous system is stimulated for a long time, it will cause vascular spasm, a failure in organs suffering from lack of blood circulation.
How to quickly normalize blood pressure
A gap in the pulse difference of 50 units upward requires contacting specialists. But the first steps to normalize blood pressure are usually taken independently. Recommend:
- take a horizontal position;
- restore breathing;
- open the window for oxygen access;
- if blood pressure is high, raise your head; if blood pressure is low, raise your legs;
- provide freedom to the neck;
- high blood pressure involves hot foot baths to improve blood flow from the brain;
- acupressure and breathing exercises are acceptable: hypotension requires rubbing the earlobes, hypertension requires circular movements from the ears to the back of the head.
How to treat
It is important to maintain a normal difference between the upper and lower pressure values. Its significant deviations to a lesser extent lead to oxygen starvation, tachycardia, atrophy of parts of the brain, blurred vision, paralysis of the respiratory muscles, cardiosclerosis, and cardiac arrest. A large pressure difference indicates wear and tear of the heart and may indicate a pre-stroke or pre-infarction condition.
Important: You should consult a doctor if the interval between tonometer readings is 20 units or lower - in addition to cardiovascular problems, the cause of this may be kidney disease. A patient with a pulse pressure over 60 units needs urgent help from a cardiologist.
Treatment depends on the causes of the pathological condition and always begins with diagnosis. If no serious diseases are identified, with a low difference in blood pressure, the therapist recommends taking the following measures:
- follow a daily routine, allocating at least 8 hours for sleep;
- engage in physical exercise in the fresh air - especially jogging or race walking, which stimulate the contractility of the heart;
- periodically ventilate the premises;
- try to avoid negative emotions and stressful situations;
- introduce into the diet foods containing vitamins A, E, and Omega-3 fatty acids.
In the presence of pathologies, therapy becomes more targeted, and treatment agents are prescribed by specialized specialists. Here are some recommendations to solve the problem of low pulse pressure.
- For vegetative-vascular dystonia - strengthening the heart muscle, improving the general condition with the help of Citramon, Aspirin, Askofen tablets. Water aerobics classes, contrast water procedures, and cardio exercises under the supervision of an instructor are useful. Folk remedies - tinctures of foxglove and lily of the valley - will not interfere.
- For anemia, take iron supplements and exercise.
- In case of acute pyelonephritis, renal colic - clarification of the diagnosis and treatment in a hospital.
- In case of cardiogenic shock - urgent resuscitation measures within 20-40 minutes. As first aid, the patient is laid horizontally, with his legs elevated using a pillow, his clothes are unbuttoned, and Nitroglycerin is given.
- With hypovolemic shock. If the reason for the decrease in systolic pressure is external bleeding, a tight bandage is applied before the doctor arrives: if a vein is damaged, on the affected area; if there is arterial bleeding, above the wound. In a hospital setting, plasma-substituting compounds are administered intravenously.
To combat high pulse pressure, folic acid is prescribed: this vitamin reduces cholesterol levels in the blood, thereby relieving the heart. If hypertension is noted at the same time, beta blockers are taken to reduce systolic pressure. Diuretics help reduce the load on the heart. The symptoms of atherosclerosis can be mitigated using anticholesterol drugs: nicotinic acid, statins, fibrates.
Did you like the article? Save it!
Still have questions? Ask them in the comments! Cardiologist Mariam Harutyunyan will answer them.
Ivan Grekhov
Graduated from the Ural State Medical University with a degree in General Medicine. General practitioner
Diagnostics
After a conversation with the patient, the doctor prescribes a full clinical and laboratory examination, taking into account the direction in which the tonometer deviation occurred. Mandatory for everyone - an ECG, as well as an EchoCG, assessing the electrical activity of the myocardium, the condition of the heart chambers, and the large arteries adjacent to them. Additionally prescribed:
- UAC, OAM;
- blood chemistry;
- Ultrasound of the urinary system;
- MRI of the aorta;
- angiography of the renal arteries.
The ISH study algorithm is simple: 24-hour monitoring of blood pressure over time. In addition, they prescribe: blood sugar tests, lipid and coagulograms, ultrasound of cerebral vessels. If necessary, the patient is consulted with an angiosurgeon, neurologist, diabetologist, nutritionist, and psychotherapist.
What is blood pressure?
Arterial pressure
- Blood pressure is the natural process of blood pressure on the walls of blood vessels, capillaries, veins and arteries. If a person is completely healthy, then he generally does not notice how the blood circulates inside his body. But if something is wrong with the body, then depending on whether it is high or low, a person may feel a headache, pulsation in the back of the head, nausea and dizziness.
- Now let's figure out why this happens. If you were a diligent student at school, then you probably remember that the blood in the human body is always in motion. Even when a person is resting, it continues to circulate through his arteries and veins. As soon as it reaches the ventricles of the heart, a spasm of the heart muscle occurs and blood under pressure is released into the vessels and begins to fill them quite quickly, putting pressure on their walls. If at this stage there is more or less pressure on the vessels than necessary, then the person begins to feel all those unpleasant symptoms that we introduced you to above.
- From all this we can draw only one conclusion: our blood pressure directly depends on how often and with what force the heart muscle contracts. Therefore, if you notice a deviation in one direction or another, then be sure to check if you have heart problems. If the examination shows that it is working correctly, begin to look for other reasons for the malfunction of the vascular system.
Features of treatment
A set of measures to relieve a pathological condition is aimed at eliminating the cause.
- Atherosclerosis requires drug therapy or surgery. Among the medications used are: statins and fibrates, which reduce the concentration of blood cholesterol (Rosuvastatin, Fenofibrate); unsaturated fatty acids that stimulate the removal of toxic fats from the body (Linetol); vitamins that nourish the endothelium and block the formation of atherosclerotic plaques. Among the surgical methods that deserve attention are laser angioplasty, vascular stenting, bypass surgery - creating a bypass blood flow, endarterectomy - excision of part of the inner layer of an artery with an atherosclerotic plaque.
- Aneurysms are treated only with surgery.
- Pericarditis involves pericardiectomy of the affected area with recovery in 60% of cases.
- Aortic stenosis requires replacement of the valve with an artificial one, which lasts from 8 to 25 years, taking into account the properties of the selected material.
- Heart rhythm disturbances are treated with antiarrhythmic drugs, sometimes with the help of a defibrillator or the installation of a pacemaker.
- Chronic kidney pathology is treated with anti-inflammatory therapy, antibiotics, anticoagulants, and physiotherapy.
- Tumors are corrected with cytostatics and other antitumor drugs. Failure requires a decision on the operation.
- Left ventricular failure requires either surgery or a combination of medications:
- ACE inhibitors – reduce diastolic pressure;
- cardiac glycosides improve myocardial contractility;
- nitrates to improve oxygen supply to the heart;
- diuretics to relieve swelling.
Acute left ventricular failure requires emergency hospitalization in a specialized hospital.
ISH therapy is prescribed by a cardiologist or therapist after a full clinical and laboratory examination and requires compliance with several rules: the force of the blood hitting the vascular wall is gradually reduced so that adaptation to new conditions occurs and ischemia does not develop; medications are required to affect only the upper blood pressure reading; There should be no negative impact on the kidneys or brain. For this purpose the following are appointed:
- antihypertensive drugs: calcium antagonists, beta blockers, ACE inhibitors, angiotensin blockers;
- diuretics: a small blood volume reduces the upper limit, cardiac output;
- drugs that stimulate blood flow in the kidneys, brain, heart;
- neuro-, cerebroprotectors – improve the nutrition of nerve cells, prevent stroke.
To increase efficiency, various combinations of drugs are used under medical supervision.
Treatment options
If there is a difference between the upper and lower pressure, which is a deviation, it is necessary to urgently take measures to combat blood pressure disorders. The following is recommended for patients:
- Set up a daily routine. You need to allocate at least 8 hours for sleep; you should not agree to work night shifts.
- Do not overload the body with physical labor.
- Eat properly. It is necessary to remove all harmful foods from the menu, especially those that affect blood pressure.
- Exercise. If pulse pressure is abnormal, it is recommended to run, swim, and perform therapeutic exercises.
- Spend more time outdoors.
- Ventilate the room more often.
- Quit smoking and drinking alcohol.
- Avoid stressful situations and unnecessary worries.
- Monitor your body weight.
A balanced diet, adequate sleep and exercise are the first steps on the path to recovery.
If the deviations are significant, then you cannot do without taking medications. Medications should only be prescribed by a doctor; choosing your own medication is strictly prohibited.
If deviations in pressure are caused by a specific disease, then it is necessary to direct all efforts to treat it. Without eliminating the cause, it will be impossible to normalize the pulse rate.
Prevention
The patient’s lifestyle is important: giving up bad habits, diet, dosed exercise, walking, proper rest. It is necessary to calculate the daily drinking ration together with your doctor, at least 2 liters of clean water daily. Instead of saunas and hot baths, take a contrast shower. The diet should consist of vegetables, fruits, and foods containing iron: liver, tomatoes, fish, apples. A healthy lifestyle is especially relevant for those who have crossed the forty-year mark.
Treatment regimens
The method of therapy depends on the nature of the process. For endocrine pathologies, a replacement technique or surgical intervention is indicated.
Cardiac causes are corrected surgically or by taking medications: ACE inhibitors, tonics and diuretics in strictly defined dosages.
Nephrogenic factors are eliminated through radical (surgical) measures, less often through conservative means.
Specific symptomatic therapy is even more difficult. It is necessary to select means to normalize both indicators in the hospital.
A significant role is played by lifestyle changes. A calm, measured regimen with proper nutrition and proper rest will help put the body in order and mitigate the negative manifestations of the disease.
Pressure and overwork
The upper pressure is high, the lower pressure is also high - this is what a complaint from a patient with overwork may look like. The upper pressure is high and the lower pressure is low - and such indicators can be recorded in a patient with suspected fatigue. What is overwork, and why can it affect all blood pressure indicators, including the pulse difference?
The causes of overwork are numerous:
- Constant intellectual overstrain at work - it affects workaholics and perfectionists; in Japan, for example, there have been cases of death right at work due to critical overwork;
- Poor nutrition, lack of valuable vitamins and microelements;
- Poor quality rest, when the body simply does not have enough time to recover after exhausting work;
- Severe stress;
- Serious physical activity, excessive for the physical fitness of a particular person;
- Taking medications that cause fatigue - including cold and cough medications, antihistamines, as well as medications that affect the central nervous system.
Long-term illnesses also lead to fatigue - from depression to heart failure, obesity, long-lasting ARVI, oncology (the list can be continued for a long time).
Symptoms of overwork include: sleep disturbances, pale skin and bruises under the eyes, nausea and vomiting that occurs for no reason, headaches with red eyes, emotional instability, pressure surges, heart pain, problems with appetite.
An increase in blood pressure in different variations during fatigue is associated with physical and mental stress. A patient who is in a state of prolonged overexertion cannot organize the necessary rest for his body. His cerebral circulation inevitably changes, blood vessels narrow, headaches appear, and blood pressure rises.
How to cope with stress?
Psychologists identify three general reactions to stress.
They are:
- Rabbit. As you might guess, this is a passive response. In this case, the stress factor itself deprives a person of the opportunity to think sensibly and logically. He simply hides from problems, since he does not have his own resources to solve them.
- A lion. In this case, stress activates all the body’s reserves, but for a short period of time. The person makes a leap towards the problem. But this strategy is far from ideal - actions are often thoughtless, they contain a lot of emotions and little logic. And if the situation is not resolved quickly, then strength is depleted, weakness, apathy, and anxiety set in.
- Vol. This reaction implies that a person uses his psychic and mental resources with maximum rationality, so he can continue his normal life without allowing the stressor to knock him down. From the point of view of neurophysiology, this strategy is the most competent.
Any cardiologist who mentions the risks associated with cardiovascular disease always mentions stress.
Stress, along with excess weight, bad habits, and physical inactivity, can accelerate diseases that were previously considered age-related.